ABSTRACT
Ectodermal dysplasia (ED) is a spectrum of inherited disorders that compromise the development and function of ectodermal structures, like hair, nails, and teeth. This case report describes a 17-year-old male with sparse hair and cognitive difficulties who was diagnosed with ED in childhood. A multidisciplinary evaluation with dermatology, neurology, and dentistry revealed characteristic clinical features, and the histopathological diagnosis was confirmed via punch biopsy. Also, ED poses challenges beyond dermatologic manifestations, affecting cognitive function, psychological well-being, and nutrition. Multidisciplinary management, early diagnosis, and awareness are crucial for optimizing patient outcomes and exploring potential therapies.
Keywords: Ectoderm, ectodermal dysplasia, genetic diseases, patient care team
Introduction
During embryogenesis, the ectoderm forms various structures including the epidermis, mammary glands, sweat glands, olfactory epithelium, and teeth.[1] Proper development requires interaction between mesoderm and ectoderm, primarily mediated by ectodysplasin A protein, associated with TNF-alpha ligand family genes (EDA, EDAR, EDARADD). The Wnt signaling pathway also plays a crucial role, alongside Hedgehog, NF-kB, TNF, P63, and retinoic acid pathways.[2]
Ectodermal dysplasia (ED) has a prevalence of approximately 7 per 10,000 newborns. However, data for Peru is lacking. ED can be inherited through Mendelian patterns, affecting ectoderm-derived tissues like skin, sweat glands, hair, nails, and teeth, leading to diverse symptoms.[3] Complications may include cleft lip/palate, immune deficiencies, and sensory impairments.[4]
The 2019 classification system focuses on molecular pathways [Table 1]. EDA mutations aren’t the sole cause; WNT, BMP, FGF, TP63, and NFKB mutations are also implicated, affecting ectoderm-mesenchyme interaction. This classification links clinical characteristics to affected pathways or molecules.[5]
Table 1.
Summary of classification of ectodermal dysplasia
| Affected Gene (s) | Disease (s)/Syndrome (s) - Previously suggested nomenclature | OMIM number | Distinguishing Features | |
|---|---|---|---|---|
| P63 pathway | DLX3 | Tricho-dento-osseous syndrome (TDO) | 190320 | Hair and nail phenotypic. |
| RIPK4 | Curly hair ankyloblepharon-nail dysplasia syndrome (CHANDS); complex lethal subtype known as Bartsocas-Papas syndrome 1 (BPS1) | 214350, 263650 | Hair and nail phenotypic, additional symptoms. | |
| Structure group | KRT74 | Ectodermal dysplasia 7, hair/nail type (ECTD7) | 614929 | Hair and nail phenotypic |
| KRT85 | Ectodermal dysplasia 4, hair/nail type (ECTD4) | 602032 | Hair and nail phenotypic | |
| GJB2 | Keratitis-ichthyosis-deafness syndrome, AD (KID) | 148210 | Hair, nail phenotypic and additional symptoms | |
| GJB6 | Clouston syndrome or ectodermal dysplasia 2, Clouston type (ECTD2) | 129500 | Hair and nail phenotypic | |
| Others | HOXC13 | Ectodermal dysplasia 9, hai/nail type (ECTD9) | 614931 | Hair and nail phenotypic |
This study presents a case report of a 17-year-old male from Arequipa, Peru, diagnosed with Ectodermal Dysplasia. It will delve into the clinical characteristics of the case and explore its impact on daily life. Given that no cases have been reported in our country thus far, we believe it is crucial to raise awareness about this condition not only for educational purposes but also to assess potential forms of multidisciplinary intervention that should be pursued.
Case History
A 17-year-old male patient visited the primary care clinic with complaints of sparse hair on the scalp, eyelashes, eyebrows, deformed nails, and poor academic performance. He reported difficulties with short-term memory but denied skin dryness, inability to sweat, dry mouth, and recurrent respiratory infections. His mother reported similar issues with hair and nails, and her sister has a significant intellectual disability. No other family members have skin complaints or cognitive impairments, and there has been no previous genetic testing in the family [Graphic 1].
Graphic 1.
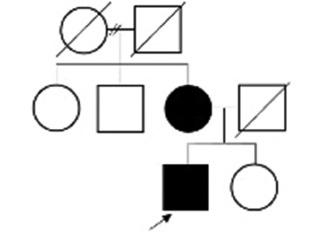
Patient’s family pedigree. Three generations are evident; only the patient and his mother are affected. There is no evidence of a sex-linked pattern
Clinical examination revealed diminished and thin hair on the scalp, eyebrows, eyelashes, upper lip, and chin, without evidence of eczematous rash or dry skin. The patient had complete teeth without obvious malformations. Examination of his fingers showed normally shaped fingers with thick structure, slow-growing, discolored, brittle, and incomplete nails in the distal third [Figure 1]. A punch biopsy showed normal epidermal thickness, normal eccrine and sebaceous glands, and follicular structures with a rudimentary aspect, compatible with congenital ectodermal dysplasia.
Figure 1.

(a and b): Hands and feet showing thickened skin, brittle and incomplete nails. (c): Scalp with visibly diminished hair density. (d): Teeth with normal structure
The initial focus was on addressing his hair and nail concerns, leading to a referral to a dermatologist. The patient established a skincare routine using neutral soaps and moisturizing creams daily, applying sunscreen every morning, reapplying every 4 hours, and avoiding prolonged sun exposure during peak hours. A neurocognitive assessment by a neuropsychologist was conducted using Kaufman’s Assessment Battery for Children (KABC-II), the Wechsler Intelligence Scale for Children (WISC-V), and Raven’s Progressive Matrices test. These tests measure various cognitive abilities, including verbal and non-verbal reasoning. The patient was categorized as having a moderate intellectual disability. A referral to neurology for further evaluation and management was recommended, alongside therapy sessions focusing on attention, learning strategies, memory enhancement, and concentration skills. Regarding ophthalmology, the patient had decreased visual acuity for distance vision, with measurements of −0.25 in the right eye and −0.5 in the left eye, necessitating corrective lenses. Sparse upper and lower eyelashes caused a preliminary reaction in the papillary area due to constant exposure to dust and external agents, leading to a recommendation of 1% sodium carboxymethylcellulose and 0.2% olopatadine [Figure 2]. The patient’s teeth were clean, free of decay, and well-aligned, with healthy gums. The importance of regular follow-up with specialists was emphasized. The patient was assessed monthly, with no reported adverse effects. Emphasis is placed on the daily use of body creams and artificial tears to prevent complications.
Figure 2.
(a): Pupil and iris show no alterations. (b): scant superior and lower eyelashes. (c): reactive papilla from environmental exposure
Finally, the primary limitation is the patient’s residence in a remote rural area. However, the patient was able to access specialists via telemedicine for follow-up.
Discussion
There are various types of ectodermal dysplasia, with the most common being anhidrotic/hypohidrotic and hidrotic. The case described presents a patient with the hidrotic type, also known as Clouston syndrome, primarily affecting hair and nails while sparing teeth and sweat glands.[6] Typical manifestations include hair loss, nail dystrophy, and palmoplantar keratoderma, with hyperpyrexia usually absent. Hair abnormalities include atrichia, hypotrichosis, and slow, weak growth, with males often exhibiting diffuse patches of weak hair growth and facial or axillary hair. Nail alterations such as micronychia, anonychia, slow growth, thickening, or weakness are common.[7,8]
Non-cutaneous manifestations are rare but may include bone abnormalities. A study by Pietrzak et al.[9] reported thickened cranial bones, increased bone density, cortical layer thickening, and periosteal proliferation of proximal phalanges, similar to our case. Additionally, mutations in GJB6 and GJB2 genes can contribute to sensorineural deafness or photophobia, as seen in another case report by Duzkale et al.[10] Clouston syndrome has also been linked to eccrine syringo-fibroadenoma—a rare neoplasm originating from eccrine glands. Regular follow-up is crucial to monitor for potential complications.
Moreover, a study involving 35 individuals with signs of ectodermal dysplasia found that 51% experienced poor mental health and anxiety compared to controls.[9] In our case, the patient was diagnosed with intellectual disability. Patients with this condition may also face an increased risk of food allergies due to epithelial barrier disruptions. A reported case included allergies to egg, milk, dust, and ovomucoid.[11] Therefore, assessment by an allergist and nutritionist is relevant for addressing both mechanical and allergic issues in nutrition.
Declaration of patient consent
The author certifies that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that their name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hu MS, Borrelli MR, Hong WX, Malhotra S, Cheung ATM, Ransom RC, et al. Embryonic skin development and repair. Organogenesis. 2018;14:46–63. doi: 10.1080/15476278.2017.1421882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Majmundar VD, Baxi K. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [[Last accessed on 2023 Jul 24]]. Ectodermal dysplasia. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563130/ [PubMed] [Google Scholar]
- 3.Yapijakis C, Douka A, Gintoni I, Agiannitopoulos K, Vlachakis D, Chrousos GP. Clinical and molecular genetic analysis of cases with ectodermal dysplasia. In: Vlamos P, editor. GeNeDis 2022. Cham: Springer International Publishing; 2023. [[Last accessed on 2024 Jul 26]]. pp. 181–6. (Advances in Experimental Medicine and Biology;vol. 1423) Available from: https://link.springer.com/10.1007/978-3-031-31978-5_15 . [DOI] [PubMed] [Google Scholar]
- 4.Ectodermal Dysplasia. National Institute of Dental and Craniofacial Research [Internet] 2024. Aug, Available from: https://www.nidcr.nih.gov/health-info/ectodermal-dysplasia .
- 5.Wright JT, Fete M, Schneider H, Zinser M, Koster MI, Clarke AJ, et al. Ectodermal dysplasias: Classification and organization by phenotype, genotype and molecular pathway. Am J Med Genet A. 2019;179:442–7. doi: 10.1002/ajmg.a.61045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saltnes SS, Jensen JL, Sæves R, Nordgarden H, Geirdal AØ. Associations between ectodermal dysplasia, psychological distress and quality of life in a group of adults with oligodontia. Acta Odontologica Scandinavica. 2017;75:564–72. doi: 10.1080/00016357.2017.1357189. [DOI] [PubMed] [Google Scholar]
- 7.Dev A, Malhi K, Mahajan R. Ectodermal dysplasia –An overview and update. Indian Dermatol Online J. 2024;15:405–14. doi: 10.4103/idoj.idoj_599_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anbouba GM, Carmany EP, Natoli JL. The characterization of hypodontia, hypohidrosis, and hypotrichosis associated with X-linked hypohidrotic ectodermal dysplasia: A systematic review. Am J Med Genetics Pt A. 2020;182:831–41. doi: 10.1002/ajmg.a.61493. [DOI] [PubMed] [Google Scholar]
- 9.Pietrzak A, Grywalska E, Gerkowicz A, Krasowska D, Chodorowska G, Michalska-Jakubus M, et al. Immune system disturbances in Clouston syndrome. Int J Dermatol. 2016;55(5):e241–9. doi: 10.1111/ijd.13152. [DOI] [PubMed] [Google Scholar]
- 10.Duzkale N, Aygar GT, Keseroglu K, Mutlu M, Ugur MB. Causal variants of the GJB6 gene are associated with hearing loss and skin manifestations: A case report from Turkey. Int J Dermatol Venereol. 2022;5:166–8. [Google Scholar]
- 11.Suzuki T, Tajima H, Migita M, Pawankar R, Yanagihara T, Fujita A, et al. A case of anhidrotic ectodermal dysplasia presenting with pyrexia, atopic eczema, and food allergy. Asia Pac Allergy. 2019;9:e3. doi: 10.5415/apallergy.2019.9.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]



