ABSTRACT
Background:
Thalassemia is a hemoglobinopathy-associated genetic disease resulting due to defective synthesis of globin chains, causing defects in the skeletal and oral structures.
Aim:
This cross-sectional study was designed to analyze the prevalence of dental caries, oral health status, malocclusion status, and dental treatment needs in thalassemic children.
Materials and Methods:
Institutional Ethical committee clearance was obtained before starting the study. The study sample comprised 100 thalassemic and 100 normal children in which oral disease markers like dmft/DMFT index, plaque index, gingival index, and Angle’s classification for malocclusion were used. The statistical tool used was ‘one-way ANOVA’ with the probability set at 0.05.
Results and Observations:
Statistically significant differences in prevalence of dental caries, periodontal disease, malocclusion, and treatment needs were noted in thalassemic individuals when compared to normal subjects.
Conclusion:
The present study has given an insight into the various oral and dentomaxillofacial manifestations of thalassemia, thus considering the importance of routine oral examination for the prevention of dental caries and periodontal diseases.
Keywords: Dental caries, periodontal, plaque, thalessemia
Introduction
Hemoglobinopathies are mainly constituted by thalassaemia and sickle-cell anemia and have underlying genetic defects. These have global prevalence (approximately 5% of the total world population).[1] Individuals carrying hemoglobin E/beta-thalassemia comprise nearly 50% of the subjects afflicted with severe form of beta thalassemia. The highest prevalence has been observed in India, Bangladesh, and southeastern Asian countries, especially Thailand, Laos, and Cambodia.[2,3,4,5]
Beta thalassemia major is the severest form of hereditary hemolytic anemia (also known as Cooley’s anemia). The underlying pathogenesis of beta thalessemia is the unusual synthesis of β-chain hemoglobin that starts appearing early in the prenatal period between 4 and 6 months due to switching of HbF into HbA. Children diagnosed with this disease demonstrate a hematocrit value of 20% and suffer from chronic anemia-associated complications such as retardation or stunted growth.[6,7]
In thalessemia, there is reduction in the synthesis rate of one globin chain in the hemoglobin molecule, which is responsible for anemia due to either deficient or no synthesis of normal adult hemoglobin chains combined with the oxygen carrying capacity of red blood cells. Oral structural alterations in thalassemic subjects include enlargement of maxilla, which results in protrusion of anterior teeth, an increase of interdental spacing, overbite, open bite, and malocclusion that increases the chances of development of dental caries.[8]
The subjects suffering from the beta form of thalassemia have high caries experience compared with normal children. Since these patients have a preoccupation with this life-threatening condition, neglecting basic preventive oral health care is a common feature.[9]
There are very few studies that have explored the prevalence of dental caries, oral health, malocclusions, and dental treatment needs among thalassemic children in India. Hence, this study was designed to ascertain the overall prevalence of dental caries, malocclusion, oral health status, and need for dental treatment in children diagnosed with thalessemia in India.
Materials and Methods
Study design and setting
This cross-sectional study analysis was conducted on 100 thalassesmic children registered with thalassemic society. Hospital centers equipped with management of thalassemic patients were selected for the study. Institutional ethical committee clearance was taken before starting the study project (IEC/GMCHK23-24M).
Study participants and sampling
The study sample comprised two categories: a) Group A: This group comprised 100 thalassemic pediatric patients; b) Group B: This group comprised 100 normal children. There were 55 male and 45 female afflicted children in group A and 35 male and 65 female children in group B. The age range of studied population was between 1 and 17 years.
The inclusion criteria for the study were a) children diagnosed with thalessemia and b) those receiving regular blood transfusions. The exclusion criteria included a) any systemic diseases that might result in dental and oral disease and b) those children whose parents or caregivers refused to participate in the study.
Statistical analysis: The entire observational data were entered in Microsoft Excel Worksheets and analyzed using the SPSS statistical tool (version 27.0). The statistical tests used included one-way ANOVA, and the significance of the test was set at a probability of 0.05.
Methods of oral examination
Decayed and filled teeth (dft) and decayed missing filled teeth (DMFT) indices were used for determining prevalence of dental caries in deciduous and permanent dentitions Oral hygiene status was analyzed by debris index (DI), calculus index (CI), and Simplified Oral Hygiene Index (OHI-S), whereas malocclusion status was assessed using Angle’s and Baume’s classifications.
Results and Observations
Maxillofacial characteristics
The maxillofacial features that were observed in studied thalassemic patients included frontal bossing, prominent malar bones, saddled nose, protrusion of maxilla, flaring of maxillary anteriors, and incompetence of lips. These features contributed to distinct “chipmunk facies”.
Of all the thalassemic patients who were examined, 39% had normal facial appearance, 31.1% exhibited little nasal depression, 12.0% demonstrated puffiness of eyelids with the absence of overgrowth of maxilla, 10% subjects showed mild maxillary proclination and bulging of frontal and zygomatic bones, and 18% of patients exhibited typical “chipmunk” resembling facies [Table 1, Graph 1].
Table 1.
Table demonstrating maxillofacial characteristics in thalassemia
| Maxillofacial features | Percentages |
|---|---|
| Normal appearance | 39 |
| Slight nasal depression | 31.1 |
| Puffiness of eyelids (no maxillary protrusion) | 12 |
| Mild maxillary proclination, bulging of frontal and zygomatic bones | 10 |
| Chipmunk facies | 18 |
Graph 1.
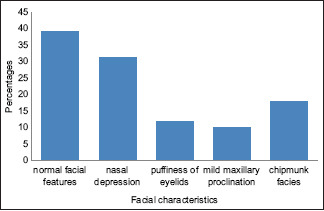
Graph showing facial characteristics
Dental caries
The mean ± S.D. dmft values were 4.92 ± 1.9 in 6 to 9 years old, 6.89 ± 0.23 in 12–14 years, and 5.14 ± 0.12 in 15–18 years age range in thalassemic patients. It was noted that the caries prevalence among thalassemic subjects was significantly greater when compared with controls. The mean ± S.D. dmft/DMFT index scores in control group subjects were found to be 2.01 ± 1.04 in 6–9 years age group, 4.23 ± 0.78 in 12 to 14 years, and 1.23 ± 0.01 in 15 to 18 years age group. This difference in mean ± S.D. dmft/DMFT index scores was calculated to have statistical significance (P < 0.001) [Table 2, Graph 2].
Table 2.
Table demonstrating mean±S.D. dmft/DMFT index scores in thalassemic and normal subjects
| Age group | Mean±S.D. dmft/DMFT index (thalessemia group) | Mean±S.D. dmft/DMFT index (control group) |
|---|---|---|
| 6-9 years | 4.92±1.9 | 2.01±1.04 |
| 12-14 years | 6.89±0.23 | 4.23±0.78 |
| 15-18 years | 5.14±0.12 | 1.23±0.01 |
Graph 2.
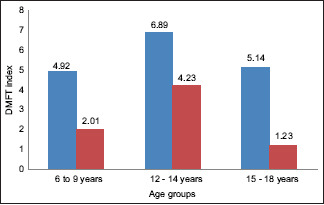
Graph showing mean dmft/DMFT indices
Periodontal and oral hygiene status
It was noted that thalassemic patients demonstrated high plaque and gingival indices scores when compared with control subjects. The mean ± S.D. plaque index value in children with thalassemia was found to be 2.76 ± 0.23 when compared to control group subjects, where it was found to be 1.09 ± 0.21 [Graph 3]. 50.2% of thalassemic children were found to have had a mild form of gingivitis, 24.9% suffered from a moderate level of gingivitis, and 15.9% suffered from a severe form of gingivitis. This difference was found to be statistically significant (P < 0.05).
Graph 3.
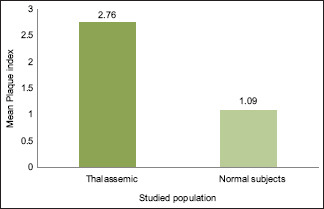
Graph showing mean plaque index
Approximately two-thirds of thalassemic children had a poor status of oral hygiene. 23.7% of thalassemic children had supragingival and subgingival calculus deposition, whereas only 9% of normal children had calculus deposits.
Malocclusion
Almost 95% of studied thalassemic children were found to have class II skeletal relation. A protrusive premaxillary region was responsible for an increase in overjet, interdental spacing, and forward pathological drifting of maxillary anterior. This was found to have extremely statistical significance (P < 0.001).
Treatment needs
It was found that nearly all studied study subjects suffering from thalassemia required dental treatment and good oral hygiene practices. Hence, adequate training programs must be held at frequent intervals for the patients and their parents or caregivers.
Discussion
Thalassemia results from defective synthesis of single or greater number of globin chains in hemoglobin. This is a genetic disorder and has autosomal recessive inheritance. It was first identified in 1925 by Dr. Thomas Cooley as syndrome associated with anemia that had small-sized red blood cells. Thalassemia is characterized by different grades of anemia with a wide range and can also be threatening to one’s life. This hereditary form of anemia occurs due to the mutations localized on chromosome 16, which is responsible for encoding of α-globin, and also over chromosome 11, which encodes for γ, δ, and β-globin chains.
Hence, depending upon the affected globin chain (s), thalessemia is classified into a) αthalassemia and b) β-thalassemia. Depending upon clinical and genetic variations, thalassemias are categorized into a) homozygous, b) heterozygous, and c) compound heterozygous.[10]
The heterozygous or thalassemia minor type of β-thalassemia has mild manifestations with minimal clinical expression, while homozygous or thalassemia major exhibits the severest form of clinical manifestations with distinct oral and facial deformities. There is also a lesser severe type known as the ‘Thalassemia intermedia’, which is very rare in occurrence.[11]
Thalassemia significantly affects the quality of life in affected children. Hence, both clinicians and dentists must possess sound knowledge of oral and maxillofacial features in thalassemic individuals. These patients require greater psychological and social and family supportiveness that may be helpful in causing improvement in outcome of treatment. The patients with thalassemia demonstrate clinical variations in signs and symptoms of the disease. Due to severity of anemia in the early childhood phase, changes in bony structures, growth retardation, and splenomegaly are seen.[12] The present study attempts to record the prevalence of intraoral and extraoral findings in children and adolescents affected with thalassemia.
Demographic data of present study demonstrated an age range from 1 to 17 years with slight male predilection. In the present study, the maxillofacial features most commonly found in the studied population included frontal bossing, prominently placed malar bones, saddle nose, maxillary protrusion, maxillary anterior teeth flaring, and incompetent lips altogether contributing to “chipmunk facial features”. 39% children were having normal facies, 31.1% had slight nasal bridge depression 12.0% showed puffiness of eyelids, 10% showed mild maxilla proclination along with bulging of frontal and zygomatic bones, and 18% exhibited “chipmunk” facies. The prevalence of dental caries was found to have a statistically significant difference (P < 0.01) greater on comparing with control subjects. The periodontal status and oral hygiene status were found to have a statistically significant difference (P < 0.05) on comparing with normal children. 95% of studied thalassemic children were found to have class II malocclusion and were statistically significant (P < 0.001). All thalassemic children had a need for the dental treatment.
Elangovan et al.[13] (2013) found that 59.7% of thalassemic patients had class I malocclusion, 23.6% had class II malocclusion, and none of the patients had class III type of malocclusion.
Our study findings are supported by Singh et al.[14] (2013) reported significantly high prevalence of dental caries and periodontal diseases in beta thalassemia patients in comparison with normal subjects (mean DMFT = 13.33 ± 6.813 and 3.51 ± 1.131, respectively), mean plaque index (mean PI = 3.66 ± 2.115 and 2.83 ± 1.407, respectively), and gingival index (mean GI = 2.83 ± 1.152 and 2.04 ± 1.410, respectively).
Also, Kaur et al.[8] (2012) concluded beta thalassemic patients have higher prevalence of dental caries (mean DMFT = 3.45 ± 4.20) than controls (mean DMFT = 1.82 ± 2.51).
Fatemeh Abbasi et al.[15] (2023) in their findings concluded that the mean OHIP-14 score was 13.20 (±7.01), and the mean DMFT score was 9.54 (±5.72). DMFT and OHIP-14 scores were found to be statically higher in females.
Pedullà et al.[16] (2015) concluded from their study findings that younger thalassemic populations had higher dental caries prevalence and a poor status of oral hygiene when compared older thalassemic populations. However, in contrasting findings, Jahangirnezhad et al.[17] (2014) observed that there was no statistically significant difference in dental caries prevalence in thalassemia patients when compared with controls. Also, Rajajee et al.[18] (2017) found no statistically significant difference in malocclusion in thalessemia patients and controls.
Hence, there are contrasting studies which reflect the diversity in findings pertaining to oral and maxillofacial structures in thalassemic patients.
Thalassemic patients are at high risk of dental caries and susceptible to periodontal disease. Thus, effective preventive measures must be implemented to minimize the need for extensive dental procedures.
Limitations
A larger sample size from diverse populations is required to reflect upon the extent of signs and symptoms in thalessemia patients.
Conclusion
According to present study findings, there is significant prevalence of dental caries, periodontal disease, malocclusion, and poor oral hygiene among children suffering from thalessemia. However, there are studies that reflect in lesser disease manifestations in oral and maxillofacial structures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: An increasing global health problem. Bull World Health Organ. 2001;79:704–12. [PMC free article] [PubMed] [Google Scholar]
- 2.Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86:480–7. doi: 10.2471/BLT.06.036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen S, Eldor A, Barshtein G, Zhang S, Goldfarb A, Rachmilewitz E, et al. Enhanced aggregability of red blood cells of beta-thalassemia major patients. Am J Physiol. 1996;270:H1951–6. doi: 10.1152/ajpheart.1996.270.6.H1951. [DOI] [PubMed] [Google Scholar]
- 4.De Silva S, Fisher CA, Premawardhena A, Lamabadusuriya SP, Peto TE, Perera G, et al. Thalassaemia in Sri Lanka: Implications for the future health burden of Asian populations. Sri Lanka Thalassaemia Study Group. Lancet. 2000;355:786–91. doi: 10.1016/s0140-6736(99)08246-x. [DOI] [PubMed] [Google Scholar]
- 5.Olivieri NF, Pakbaz Z, Vichinsky E. Hb E/beta-thalassaemia: A common and clinically diverse disorder. Indian J Med Res. 2011;134:522–31. [PMC free article] [PubMed] [Google Scholar]
- 6.Kazazian HJ., Jr The thalassemia syndromes: Molecular basis and prenatal diagnosis. Semin Hematol. 1990;27:209–28. [PubMed] [Google Scholar]
- 7.Forget BG. The patho physiology and molecular genetics of beta thalassemia. Mt Sinai J Med. 1993;60:95–103. [PubMed] [Google Scholar]
- 8.Kaur N, Hiremath SS. Dental caries and gingival status of 3-14 year old beta thalassemia major patients attending paediatric OPD of vanivilas hospital, Bangalore. Arch Oral Sci Res. 2012;2:67–70. [Google Scholar]
- 9.Kataria SK, Arora M, Dadhich A, Kataria KR. Orodental complications and orofacial menifestation in children and adolescents with thalassaemia major of western Rajasthan population: A comparative study. Int J Biol Med Res. 2012;3:1816–9. [Google Scholar]
- 10.Guzeldemir E, Toygar HU, Boga C, Cilasun U. Dental and periodontal health status of subjects with sickle cell disease. J Dent Sci. 2011;6:227–34. [Google Scholar]
- 11.Abu Alhaija ES, Hattab FN, AlOmari MA. Cephalometric measurement and facial deformity in subjects with Thalassemia major. Eur J Orthod. 2002;24:9–19. doi: 10.1093/ejo/24.1.9. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan RI, Werther R, Castano FA. Dental and oral findings in cooley's anemia: A study of fifty cases. Ann N Y Acad Sci. 1964;119:664–6. doi: 10.1111/j.1749-6632.1965.tb54066.x. [DOI] [PubMed] [Google Scholar]
- 13.Elangovan A, Mungara J, Joseph E, Guptha V. Prevalence of dentofacial abnormalities in children and adolescents with β-thalassaemia major. Indian J Dent Res. 2013;24:406–10. doi: 10.4103/0970-9290.118360. [DOI] [PubMed] [Google Scholar]
- 14.Singh J, Singh N, Kumar A, Kedia NB, Agarwal A. Dental and periodontal health status of beta thalassemia major and sickle cell anemic patients: A comparative study. J Int Oral Health. 2013;5:53–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Abbas F, Tabesh A, Yavari A, Makaremi R, Bizhani O, Mahmood M. Evaluation and relation of oral healthrelated quality of life and oral health status in Thalassemia Major patients, a crosssectional study. BMC Oral Health. 2023;23:493. doi: 10.1186/s12903-023-03202-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pedullà E, Scibilia M, Saladdino G, Colletta G, Rapisarda S. Dental and periodontal condition in patients affected by β-thalassemia major and β-thalassemia intermedia: A study among adults in Sicily, Italy. J Dent Health Oral Disord Ther. 2015;3:00081. [Google Scholar]
- 17.Jahangirnezhad M, Keikhahi B, Robati M, Yousefimanesh H, Karimifar A, Abdevand MZ. Evaluation oral and dental health status in major thalassemia patients referred to Ahvaz Shafa Hospital. Jundishapur Sci Med J. 2014:1–8. [Google Scholar]
- 18.Rajajee KTSV, Jampanapalli SR, Govada J, Erugula SR, Sudheer KA, Krishna MM, et al. Prevalence of dental caries, oral hygiene status, malocclusion status and dental treatment needs in thalassemic children –A cross sectional study. Sch Acad J Biosci. 2017;5:41–6. [Google Scholar]


