Abstract
Objectives:
Yearly rolling aggregate trends or rates are commonly used to analyze trends in overdose deaths, but focusing on long-term trends can obscure short-term fluctuations (eg, daily spikes). We analyzed data on spikes in daily fatal overdoses and how various spike detection thresholds influence the identification of spikes.
Materials and Methods:
We used a spike detection algorithm to identify spikes among 16 660 drug-related overdose deaths (from any drug) reported in Massachusetts’ vital statistics from 2017 through 2023. We adjusted the parameters of the algorithm to define spikes in 3 distinct scenarios: deaths exceeding 2 adjusted moving SDs above the 7-, 30-, and 90-day adjusted moving average.
Results:
Our results confirmed the on-the-ground observation that there are days when many more people die of overdoses than would be expected based on fluctuations due to differences among people alone. We identified spikes on 5.8% to 20.6% of the days across the 3 scenarios, annually, constituting 11.1% to 31.6% of all overdose deaths. The absolute difference in percentage points of days identified as spikes varied from 5.2 to 11.5 between 7- and 30-day lags and from 0 to 4.6 between 30- and 90-day lags across years. When compared with the adjusted moving average across the 3 scenarios, in 2017 an average of 3.9 to 5.5 additional deaths occurred on spike days, while in 2023 the range was 3.7 to 6.0.
Practice Implications:
A substantial percentage of deaths occurred annually on spike days, highlighting the need for effectively monitoring short-term overdose trends. Moreover, our study serves as a foundational analysis for future research into exogenous events that may contribute to spikes in overdose deaths, aiming to prevent future deaths.
Keywords: drug overdose, mortality, surveillance
During the past 2 decades, the United States has experienced an increase in drug overdose deaths. 1 To analyze trends in overdose deaths, yearly rolling aggregate trends or rates are commonly used.2,3 These methods are particularly useful to provide a broad view of trends over time. 3 Public health policy and decision makers may use these data to identify long-term patterns, evaluate the effectiveness of ongoing interventions, and strategize resource allocation.
While these aggregate trends are invaluable for understanding long-term changes, focusing solely on these general trends can obscure short-term fluctuations (eg, daily spikes). 2 Such fluctuations are crucial to assess because the risk of an overdose death may change substantially during a short period (eg, a few days or a week). For instance, emergency responders often report that periods of calm are followed by a sudden rise, or spike, in overdoses. 4 Similarly, law enforcement officers report waves of overdose service calls, responding to several calls in a single week after periods of quiet. 5 These spikes could be linked to multiple factors, such as changes in the drug supply and in access to pain medications and mental health services, among others. 6 Thus, neglecting to investigate overdose death data at a more granular level to identify any spikes may result in missed opportunities for interventions that could prevent future deaths.
Many jurisdictions have engaged with key partners—including public health, law enforcement, emergency medical services, and people who use drugs—to respond effectively to overdose spikes. 7 However, the definition of an overdose spike lacks universal consensus. 8 It may be characterized by a sudden increase in deaths, even if they are not the highest recorded, or by more conspicuous rises. Differences across jurisdictions may be influenced by factors such as differences in partner perspectives, the data used, and unique trends in local drugs (eg, frequency of fentanyl-laced heroin). 7 For example, the Rhode Island Department of Public Health historically defined spikes as the number of suspected nonfatal opioid overdoses in a week that surpassed 2 SDs above the weekly average in the past year’s data. 9 Meanwhile, many counties have identified spikes based on the number of deaths within a 24-hour period that exceed a set absolute count10-12 or 2 SDs above a 90-day moving average. 13 Furthermore, to anticipate overdose trends, researchers have, for example, developed predictive models to analyze drug overdose deaths in the upcoming week by using a 7-day lag period and setting a threshold at 1 SD above the mean for simplicity and interpretability. 14 Although different mechanisms are used to identify spikes, the rationale for the thresholds that define these spikes is often undocumented. Consequently, a need exists to examine how differing thresholds may affect the identification of spikes.
In this analysis, we used a robust spike detection algorithm to investigate the frequency, volume, and characteristics of spikes in daily fatal overdose data. We analyzed state-level mortality data from Massachusetts to identify spikes. Additionally, we demonstrated how varying the parameters of our algorithm affects the detection of spikes, underscoring the need for careful consideration when choosing spike-detection strategies. The findings illustrate the critical share of spike days in overall overdose data and may guide public health partners in understanding the nuances of spike detection to assist them in making informed decisions for monitoring overdose trends.
Materials and Methods
We obtained individual-level mortality data from January 1, 2017, through December 31, 2023, from the Massachusetts Registry of Vital Records and Statistics. The causes of death are coded per the International Classification of Diseases, 10th Revision. 15 Accordingly, we extracted data for all fatal drug overdoses defined by underlying cause-of-death codes for poisoning by drugs, medicaments, and biological substances through any intent (not inclusive to poisoning by or exposure to alcohol), aligning with the methods used in reports by the Centers for Disease Control and Prevention16,17 and previous studies on drug overdose deaths18,19: X40-X44 (unintentional), X60-X64 (suicide), X85 (homicide), and Y10-Y14 (undetermined). Then, we aggregated the data to obtain daily counts of overdose deaths. The Mass General Brigham Institutional Review Board (protocol 2021P003355) exempted the study from review and waived informed consent because no human subjects were involved; data were not obtained through participant interaction.
To identify days with spikes in overdose deaths, we leveraged a spike detection algorithm based on z scores that functions as a data-monitoring tool, designed to identify signals or, in other words, deviations from the established patterns within a dataset. 20 Researchers have used this algorithm for various applications, such as identifying peaks in steps and heartbeat data 21 and pinpointing key moments in a person’s walking pattern. 22 The algorithm’s robustness lies in its ability to dynamically construct moving averages and SDs, ensuring that the detection threshold is not unduly affected by previously detected signals. The involved parameters that define the identification of spikes, including the lag, SD, and influence, may be selected heuristically.
Namely, the lag is the moving window where the algorithm calculates the rolling average and SD of historical data (eg, the number of periods considered). A longer window encompasses a more extensive set of historical data, providing a broader perspective. In contrast, a shorter window offers greater sensitivity, enabling quicker adaptation to new trends or information shifts. The SD parameter, defined as the z score, is used to signal when the distance between a data point and the rolling average exceeds this parameter multiplied by the rolling SD. Lastly, the influence parameter, ranging from 0 to 1, regulates the effect of signals on the calculation of subsequent rolling averages and SDs: a value of 0 excludes signals from these calculations, while a value of 1 treats all data points equally, fully integrating signals into rolling calculations. We did not want dips to heavily influence the detection of subsequent spikes, so we treated spikes and dips as signals with an influence value <1; ultimately, however, our focus was solely on identifying spikes. Additionally, we modified the original algorithm so that the lagged variable at any given day was calculated by the values from the days leading up to, but not including, the current date.
All 3 parameters of the algorithm can alter the detection of spikes. In the primary analysis, we focused on 3 scenarios with varying lag values of 7, 30, and 90 days with a fixed SD of 2 as illustrative examples, which covers the commonly used lag periods reported in existing reports and literature.9,13,14 We set the influence parameter at 0.3 based on visual analysis. After the spike detection, we quantified the characteristics of the spikes by analyzing the percentage of days identified as spikes, the percentage of deaths occurring in spikes, and the average difference in deaths occurring in spikes and the corresponding adjusted moving average, yearly.
For a sensitivity analysis, we assessed a wider parameter range of lags (7-180 d) and SDs (2-3). Additionally, we evaluated how spike identification varied across influence values (range, 0.1-0.9), maintaining a lag of 30 days and an SD of 2. We used RStudio from R version 4.3.1 (R Core Team) to analyze the data, and the code for analysis and visualization is available in the Supplement.
Results
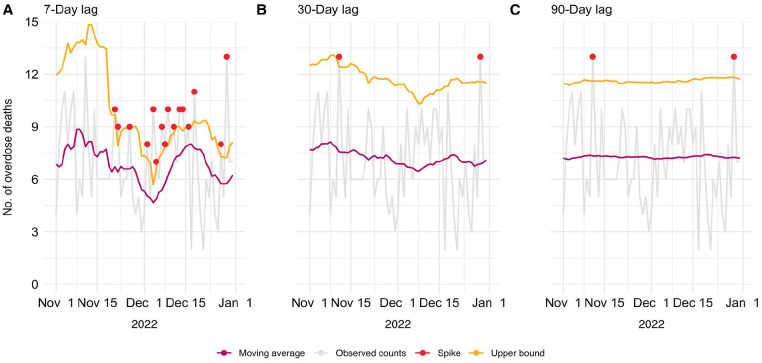
We analyzed data on 16 660 overdose deaths, with the average number of daily deaths ranging from 6.1 in 2017 to 6.5 in 2023. Among these deaths, 71.6% were male, and the median (IQR) age was 42 (33-54) years. A shorter lag value was associated with higher fluctuations in the moving average and SD, therefore affecting the number and timing of the detected spikes. However, the frequency of spikes and the lag value did not necessarily follow a monotonic trend. The spikes differed across the 3 scenarios for the last 2 months of 2022 in Massachusetts (Figure). In this period, we identified 16 spikes in the first scenario (7-day lag). The second scenario (30-day lag) and the third (90-day lag) had 2 consistent spikes, with one of the spikes not being identified in the first scenario.
Figure.
Time-series daily overdose death data and detected spikes in Massachusetts for the last 2 months of 2022 with the adjusted moving average and a detection threshold of 2 adjusted SDs above the adjusted moving average across varying lags.
Across the 3 scenarios, we identified 5.8% to 20.6% of days as spikes in deaths annually, constituting 11.1% to 31.6% of all overdose deaths (Table 1). Spike identification generally varied more noticeably between shorter and longer lag periods (eg, 7-day lag vs 30- or 90-day lag), with this variability being less apparent between increasing lag durations (eg, 30- and 90-day lags). For example, the absolute difference in the percentage points of total days identified as spikes between the 7- and 30-day lags ranged from 5.2 (in 2017) to 11.5 (in 2022) across the years. In contrast, the absolute difference between the 30- and 90-day lags ranged from 0 (in 2021) to 4.6 (in 2023). When examining the trends during the study period, we did not observe a clear pattern in the first and second scenarios for the percentage of days identified as spikes or the percentage of deaths occurring on spikes. However, in the third scenario, we observed lower percentages in 2023 as compared with the earlier years in our study period, with 5.8% of days as spikes and 11.1% total overdose deaths. Furthermore, when examining the average excess number of deaths on spike days, we observed a general increasing trend with longer lag periods. For example, in 2023, an average of 3.7 more deaths occurred on spike days with a 7-day lag as compared with 6.0 more deaths with a 90-day lag.
Table 1.
Comparison of annual spikes in drug overdose deaths in Massachusetts across lag values, 2017 through 2023
| Year | |||||||
|---|---|---|---|---|---|---|---|
| Lag: statistic | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 |
| 7 d | |||||||
| Total days identified as spikes, % | 17.0 | 20.6 | 18.1 | 18.0 | 18.4 | 19.2 | 18.1 |
| Total deaths occurring on spikes, % | 28.0 | 31.6 | 28.1 | 27.9 | 28.1 | 28.7 | 28.3 |
| No. of excess deaths on spikes, average | 3.9 | 3.8 | 3.5 | 3.7 | 4.2 | 3.9 | 3.7 |
| 30 d | |||||||
| Total days identified as spikes, % | 11.8 | 9.6 | 8.0 | 10.1 | 7.7 | 7.7 | 10.4 |
| Total deaths occurring on spikes, % | 20.4 | 17.0 | 13.8 | 17.7 | 13.7 | 13.5 | 17.9 |
| No. of excess deaths on spikes, average | 4.9 | 5.2 | 4.6 | 4.7 | 5.9 | 5.7 | 5.1 |
| 90 d | |||||||
| Total days identified as spikes, % | 9.6 | 8.0 | 6.8 | 7.1 | 7.7 | 8.8 | 5.8 |
| Total deaths occurring on spikes, % | 17.4 | 14.5 | 12.1 | 13.0 | 13.9 | 15.3 | 11.1 |
| No. of excess deaths on spikes, average | 5.5 | 5.3 | 4.9 | 5.3 | 6.2 | 5.7 | 6.0 |
The results of the sensitivity analysis were similar overall to the findings of our 3 scenarios. The comparison of lower parameter values (the lag, SD, or influence) resulted in different identification of spikes. However, as the parameter value increased, the differences in the identified spikes became progressively less pronounced (Table 2 and eTables 1 and 2 in the Supplement). Specifically, when 2 and 3 SDs were compared, the absolute difference in days identified as spikes was 14.7 percentage points for a 7-day lag, as opposed to 6.3 percentage points for a 180-day lag (Table 2).
Table 2.
Sensitivity analysis across varying lag and SD parameters of the percentage of days identified as spikes in drug overdose deaths in Massachusetts, 2017 through 2023
| Total days identified as spikes by lag, % | ||||||||
|---|---|---|---|---|---|---|---|---|
| SD | 7 d | 15 d | 30 d | 60 d | 90 d | 120 d | 150 d | 180 d |
| 2.0 | 18.4 | 11.4 | 9.1 | 6.9 | 7.0 | 6.4 | 6.3 | 6.8 |
| 2.1 | 15.9 | 9.2 | 6.9 | 5.5 | 5.8 | 5.5 | 5.6 | 5.6 |
| 2.2 | 12.8 | 7.7 | 5.9 | 4.5 | 4.6 | 4.2 | 4.6 | 4.2 |
| 2.3 | 10.5 | 6.3 | 4.5 | 4.0 | 3.4 | 3.1 | 2.9 | 3.0 |
| 2.4 | 8.8 | 5.5 | 4.1 | 2.9 | 2.5 | 2.5 | 2.5 | 2.5 |
| 2.5 | 6.7 | 4.9 | 2.5 | 2.4 | 2.2 | 2.1 | 2.0 | 2.3 |
| 2.6 | 5.8 | 3.8 | 2.0 | 2.0 | 1.8 | 1.6 | 1.4 | 1.4 |
| 2.7 | 4.5 | 3.3 | 1.5 | 1.8 | 1.5 | 1.4 | 1.2 | 1.1 |
| 2.8 | 4.2 | 2.7 | 1.2 | 1.2 | 1.3 | 1.1 | 1.1 | 1.0 |
| 2.9 | 4.1 | 1.8 | 0.9 | 0.7 | 0.9 | 0.8 | 0.7 | 0.7 |
| 3.0 | 3.7 | 1.3 | 0.8 | 0.7 | 0.5 | 0.6 | 0.6 | 0.5 |
Discussion
We assessed fatal overdose data to identify daily spikes in deaths and to characterize their frequency and the number of excess deaths in Massachusetts. Using a spike detection algorithm, we found that varying the parameters that define a spike greatly changes its identification. Greater lag values primarily led to the detection of spikes in days with conspicuously high death counts, whereas lower lag values identified these spikes in addition to more abrupt increases in deaths that were not as immediately obvious in the time-series data. As the values of the parameters (ie, the lag, threshold, or influence) increased, the variations between the identified spikes became less apparent.
Regardless of the parameters used, the identification of spikes in Massachusetts indicates that on certain days, the number of overdose deaths substantially exceeds what would be expected solely from day-to-day fluctuations due to variations among people. This finding suggests the broader presence of factors affecting the entire population of people who use drugs, such as changes in the drug supply, particularly if illicit substances were involved in the deaths that constitute spikes. 6 Our findings suggest that the magnitude of spikes generally increased during the study period, regardless of the chosen parameters. Additionally, a notable percentage of deaths occurred annually on the days identified as spikes.
This study contributes to the literature by analyzing variations in spike identification, using an algorithm with a wide range of commonly used parameter values. Our findings may help public health partners make informed decisions when analyzing trends in overdose deaths, as rapid responses to spikes are crucial. In Rhode Island, relevant proactive measures include the implementation of a spike detection strategy based on rapidly collected nonfatal overdose data to respond to spike alerts with resources such as naloxone and recovery services, and these may have contributed to the 8.3% reduction in opioid overdose deaths from 2016 to 2019. 9 Furthermore, considering that we identified spikes in up to one-fifth of all days annually in Massachusetts (20.6%; year 2018 with a 7-day lag), our findings may help adjust the method of spike detection to align response capabilities with the frequency of spike alerts. Using spike alerts selectively can prevent communities from becoming desensitized to warnings, avoiding the pitfalls of constant emergency alerts such as burnout and reduced engagement with outreach staff. Such a selective approach ensures effective mobilization for response when truly necessary. Lastly, our analysis may guide future research into the factors driving these spikes, thereby assisting policy makers in more efficacious resource allocation. 23
This study had several limitations. First, it relied exclusively on state-level data from Massachusetts only, limiting the generalizability of our findings about spikes to other regions, including localized regions in the state. Detailed analysis at the county or town level would be beneficial, as state-level data offer limited utility in enhancing public health practices or the intervention capabilities of community organizations. Second, our focus on fatal overdose data excluded other relevant datasets, such as those with data on nonfatal overdoses or naloxone administration, which could provide additional insights into spikes. The delay in finalizing fatal overdose data, ranging from 3 or 4 months in Massachusetts to often longer in other states, 18 renders these data impractical for timely responses to spikes, unlike near–real-time overdose surveillance data as used by states such as Rhode Island. 9 A third limitation was the inclusion of all fatal overdoses, regardless of intent—whether unintentional, suicide, homicide, or undetermined—which will require different intervention strategies. For example, harm reduction efforts aiming to reduce unintentional overdoses could be different from those addressing overdoses resulting from suicide or homicide. Future analyses that distinguish overdoses by intent could help guide more tailored interventions. Fourth, our analysis did not differentiate among the various substances involved in the overdoses, which restricts our understanding of the contributing factors to spikes. However, studying patterns in drug-related fatal overdoses (from any drug) remains crucial for public health professionals and policy makers, as it confirms the existence of spikes and underscores the need for strategic resource allocation to prevent future deaths. Finally, the absence of a clear definition of a spike prevented us from claiming that the occurrences that we identified met the criteria of true spikes. Therefore, we cannot conclusively assess whether the algorithm that we used represents a superior alternative to other methods. Nonetheless, our approach has effectively narrowed the pool of potential spikes, providing a focused dataset for further analysis.
Practice Implications
Our findings may provide insights for public health partners in defining and monitoring spikes in fatal overdose data. We underscore the urgent need to investigate overdose death data at the granular level to uncover potential factors contributing to spikes in drug overdose deaths. Identifying these factors may reduce deaths, given their disproportionate occurrence on days identified as spikes. Future research should investigate exogenous events that may contribute to these sudden increases in overdose deaths. For example, changes in the drug supply may suggest supply-targeted prevention efforts. Any geographic patterns or drug involvement should also be examined. Such investigations can help public health decision makers and policy makers effectively allocate resources and prevent future overdose deaths.
Supplemental Material
Supplemental material, sj-docx-1-phr-10.1177_00333549241299613 for Uncovering Patterns in Overdose Deaths: An Analysis of Spike Identification in Fatal Drug Overdose Data in Massachusetts, 2017-2023 by Hannah Lee, Daniel Otero-Leon, Huiru Dong, Erin J. Stringfellow and Mohammad S. Jalali in Public Health Reports®
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by grant R01CE003358 from the Centers for Disease Control and Prevention (CDC). This article reflects the views of the authors and does not represent the views or policies of CDC or the US Department of Health and Human Services.
ORCID iDs: Hannah Lee, BS  https://orcid.org/0009-0006-8803-0694
https://orcid.org/0009-0006-8803-0694
Daniel Otero-Leon, PhD  https://orcid.org/0000-0003-2404-1635
https://orcid.org/0000-0003-2404-1635
Mohammad S. Jalali, PhD  https://orcid.org/0000-0001-6769-2732
https://orcid.org/0000-0001-6769-2732
Supplemental Material: Supplemental material for this article is available online. The authors have provided these supplemental materials to give readers additional information about their work. These materials have not been edited or formatted by Public Health Reports’s scientific editors and, thus, may not conform to the guidelines of the AMA Manual of Style, 11th Edition.
References
- 1. Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States, 2001-2021. NCHS Data Brief. 2022;457:1-8. doi: 10.15620/cdc:122556 [DOI] [PubMed] [Google Scholar]
- 2. Friedman J, Akre S. COVID-19 and the drug overdose crisis: uncovering the deadliest months in the United States, January‒July 2020. Am J Public Health. 2021;111(7):1284-1291. doi: 10.2105/AJPH.2021.306256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fujita-Imazu S, Xie J, Dhungel B, et al. Evolving trends in drug overdose mortality in the USA from 2000 to 2020: an age-period-cohort analysis. EClinicalMedicine. 2023;61:102079. doi: 10.1016/j.eclinm.2023.102079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cuda A. Emergency responders fighting hard against overdose deaths. Stratford Emergency Medical Service. February 7, 2016. Accessed May 28, 2024. https://www.stratfordems.org/2016/02/07/emergency-responders-fighting-hard-overdose-deaths [Google Scholar]
- 5. Smiley-McDonald HM, Attaway PR, Richardson NJ, Davidson PJ, Kral AH. Perspectives from law enforcement officers who respond to overdose calls for service and administer naloxone. Health Justice. 2022;10(1):9. doi: 10.1186/s40352-022-00172-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Association of County & City Health Officials. Overdose spike response framework for communities and local health departments. June 2021. Accessed April 27, 2024. https://www.naccho.org/uploads/full-width-images/overdose-spike-response-framework-for-communities-lhds-1.pdf
- 7. Washington/Baltimore High Intensity Drug Trafficking Areas. Overdose spike response framework. 2018. Accessed April 27, 2024. https://www.hidta.org/wp-content/uploads/2018/04/ODMap-Overdose-Response-Framework-2018-3.29.18.pdf
- 8. Association of State and Territorial Health Officials. Responding to an overdose spike: a guide for state health departments. June 2020. Accessed May 26, 2024. https://www.astho.org/globalassets/pdf/overdose-spike-guide.pdf
- 9. Hallowell BD, Lasher L, Chambers LC, et al. Using timely overdose data to address a spike in nonfatal overdoses and inform a coordinated community-level response in Rhode Island, 2019. Public Health Rep. 2021;136(1):24S-30S. doi: 10.1177/00333549211012407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ocean County Health Department. Ocean County overdose response plan 2021-2022. 2021. Accessed April 28, 2024. https://www.ochd.org/wp-content/uploads/2021/12/Ocean-County-Overdose-Response-Plan.pdf
- 11. Connecticut Department of Public Health, Office of Emergency Medical Services. Statewide Opioid Reporting Directive (SWORD) 2020 annual report: June 2019–May 2020. 2020. Accessed April 28, 2024. https://portal.ct.gov/-/media/departments-and-agencies/dph/dph/ems/pdf/sword/sword-newsletters/2020/20200812-sword-annual-reportfinal.pdf
- 12. Oneida County Opioid Task Force. A brief: putting data to action. October 2022. Accessed April 27, 2024. https://www.cossup.org/Content/Documents/Publications/Oneida_County_Opioid_Task_Force_Data_to_Action_Brief.pdf
- 13. Alter A, Yeager C. The consequences of COVID-19 on the epidemic: overdoses are increasing. Washington/Baltimore high intensity drug trafficking areas. May 13, 2020. Accessed April 29, 2024. https://www.odmap.org:4443/Content/docs/news/2020/ODMAP-Report-May-2020.pdf [Google Scholar]
- 14. Mukherjee S, Becker N, Weeks W, Ferres JL. Using internet search trends to forecast short term drug overdose deaths: a case study on Connecticut. Paper presented at: 19th IEEE International Conference on Machine Learning and Applications; December 14-17, 2020; online. doi: 10.1109/ICMLA51294.2020.00208 [DOI] [Google Scholar]
- 15. World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). 5th ed. World Health Organization; 2016. [Google Scholar]
- 16. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013-2019. MMWR Morb Mortal Wkly Rep. 2023;70(6):202-207. doi: 10.15585/MMWR.MM7006A4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ahmad FB, Cisewski JA, Rossen LM, Sutton P. Provisional Drug Overdose Death Counts. National Center for Health Statistics; 2024. [Google Scholar]
- 18. DiGennaro C, Garcia G-GP, Stringfellow EJ, Wakeman S, Jalali MS. Changes in characteristics of drug overdose death trends during the COVID-19 pandemic. Int J Drug Policy. 2021;98:103392. doi: 10.1016/J.DRUGPO.2021.103392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Friedman J, Shover CL. Charting the fourth wave: geographic, temporal, race/ethnicity and demographic trends in polysubstance fentanyl overdose deaths in the United States, 2010-2021. Addiction. 2023;118(12):2477-2485. doi: 10.1111/ADD.16318 [DOI] [PubMed] [Google Scholar]
- 20. van Brakel JPG. Robust Peak Detection Algorithm Using Z-Scores. Stack Overflow; 2014. Accessed December 14, 2023. https://stackoverflow.com/questions/22583391/peak-signal-detection-in-realtime-timeseries-data [Google Scholar]
- 21. Rykov Y, Thach T-Q, Bojic I, Christopoulos G, Car J. Digital biomarkers for depression screening with wearable devices: cross-sectional study with machine learning modeling. JMIR Mhealth Uhealth. 2021;9(10):e24872. doi: 10.2196/24872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim M, Hargrove LJ. A gait phase prediction model trained on benchmark datasets for evaluating a controller for prosthetic legs. Front Neurorobot. 2023;16:1064313. doi: 10.3389/fnbot.2022.1064313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Williams KE, Freeman MD, Mirigian L. Drug overdose surveillance and information sharing via a public database: the role of the medical examiner/coroner. Acad Forensic Pathol. 2017;7(1):60-72. doi: 10.23907/2017.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-phr-10.1177_00333549241299613 for Uncovering Patterns in Overdose Deaths: An Analysis of Spike Identification in Fatal Drug Overdose Data in Massachusetts, 2017-2023 by Hannah Lee, Daniel Otero-Leon, Huiru Dong, Erin J. Stringfellow and Mohammad S. Jalali in Public Health Reports®