Abstract
Background
acquired exotropia mostly manifests as an intermittent form, and very few cases show constant exotrpia. However, the differences in the clinical features of the constant and intermittent exotropia patients has not been clear yet.
Methods
We retrospectively evaluated 6159 patients with exotropia from 2012 to 2022 in Farabi Eye Hospital, Tehran, Iran. The preoperative data collected were best corrected distance visual acuity (BCVA), spherical equivalent refractive error, amount and laterality of exotropia, presence of amblyopia and anisometropia.
Results
The mean age at the time of surgery was 21.9 ± 13.8 (range, 2–77) years and 3104 (50.4%) cases were male. Constant and intermittent exotropia were observed in 4244 (68.9%) and 1915 (31.1%) cases, respectively. BCVA was significantly worse in the constant than in the intermittent group (P < .05). In cases with dominancy, the non-dominant eye in intermittent exotropia patients showed significantly more minus spherical equivalent (-1.28 ± 3.03 diopter) compared to the constant group (-0.63 ± 4.41 diopter) (P < .001). Moreover, the mean angle of horizontal and vertical deviation at distance and near in patients with constant exotropia was significantly higher than in the intermittent cases, either when there was a dominance in one eye or in cases with no dominance (P < .001). Amblyopia was found in 38.3% of cases with constant and 13.1% with intermittent exotropia (P < .001). Anisometropia was observed in 821 (19.34%) with constant and 88 (4.6%) with intermittent exotropia (P < .001).
Conclusion
Constant exotropic patients had worse BCVA, larger angle of deviation, and higher prevalence of amblyopia and anisometropia compared to the intermittent cases.
Keywords: Intermittent Exotropia, Constant Exotropia, Amblyopia, Ansiometropia, Strabismus Surgery
Introduction
Exotropia usually starts with an exophoria and then evolves to an intermittent form and in only a small portion of patients, it becomes constant [1]. More than 90% of exo deviations are reported as intermittent [2]. Parents usually observe intermittent exotropia in early childhood while the child looks at distance, mainly when he/she is frustrated, inattentive or daydreaming [2–4]. Previous studies have reported varying results regarding the development of childhood intermittent exotropia, with no change over three years [5] or a higher percentage of improvement than deterioration over three years [6] to equal chance of deterioration or improvement over five years [7]. Therefore, the management of intermittent exotropia requires careful investigation.
Several different treatment modalities have been suggested for managing patients with intermittent exotropia; however, there is no evidence-based consensus regarding the best treatment time and the most effective method [8]. Common procedures include minus over-correction, part-time occlusion, base-in prism, and vision therapy. Surgery is usually recommended for constant and deteriorating intermittent exotropia patients [9]. Surgical intervention is considered in intermittent exotropia cases whose (1) exotropia could not be controlled with the conventional methods of treatment, (2) there is a large angle of deviation, and (3) control of deviation has gotten worse over time. It has been shown that patients with constant exotropia and a previous history of intermittent exotropia attain better post-operative sensory outcomes in gross stereopsis in comparison to those without a history of intermittent exotropia [10]. A randomized clinical trial study showed that strabismus surgery significantly improved health-related quality of life in patients with intermittent exotropia and their parents [11]. Determining the optimum timing for surgery is crucial for achieving the best sensory and motor outcomes. However, early surgery may result in consecutive esotropia [12]. Most surgeons prefer to postpone the surgical intervention in order for the child to get older. However, a recent randomized clinical trial suggested that in children with intermittent exotropia, younger age at surgery (3 to < 5 years in comparison to 5 to < 11 years) was associated with better surgical outcomes; although, they did not consider other baseline factors such as duration of intermittent exotropia and presence and severity of suppression which may have differed between age groups [13]. In cases with constant exotropia, the following protocols has been recommended before surgery: first, any significant refractive error should be corrected, and then major sensory anomalies, including amblyopia, should be treated. After that, basic ocular motilities and gross convergence should be trained, and a combination of prism and added lenses can be tried for sensory alignment of the eyes. At last, strabismus surgery can be performed to reduce the angle of deviation to within the range of fusional vergence [14].
So far, there is not much data in the literature to investigate whether or not patients with intermittent and constant exotropia are different in their clinical features, including visual acuity, refractive errors, frequency of amblyopia and anisometropia, and amount of deviation. The current study aims to compare the clinical features of cases with acquired intermittent and constant exotropia who underwent surgery in a large sample of participants.
Subjects and methods
This cross-sectional and retrospective study was performed on preoperative hospital records of 6159 Iranian patients with acquired constant and intermittent exotropia who underwent surgery. These records were derived from cases examined at Farabi Eye Hospital, Tehran, Iran over a period of 10 years, from January 1, 2012, through March 1, 2022. The Ethics Committee of Tehran University of Medical Sciences approved the protocols of this study (IR.TUMS.FNM.REC.1401.038) and the tenets of the Declaration of Helsinki were followed.
This study was conducted at Farabi Eye Hospital, which is the nation’s ophthalmology hospital and major ophthalmic-academic center. Inclusion criteria were confirmed acquired intermittent and constant exotropia based upon a unilateral cover test, and absence of other disabilities, such as motor and mental disabilities, plagiocephalic syndromes, cerebral palsy, craniofacial anomalies, and other skeletal and muscular abnormalities. All patients with a history of ocular surgery and other types of exotropia such as congenital exotropia (exotropia that started before 12 months of age) [15], Duane retraction syndrome, and fourth nerve palsies were excluded from this study. The exam findings immediately preceding surgery were used as the source of data for both intermittent and constant exotropia patients in this study.
Examinations
Routine ophthalmic examinations were performed, including dry and cycloplegic refraction, distance visual acuity measurement, slit lamp evaluation and fundus examination. Visual acuity was tested at distance using the Snellen E chart and the results were converted to logMAR; however, visual acuity was not assessed for children under 4 years old given the challenges of measuring acuity accurately and interpreting norms in that age group. The measurement of refractive error was performed using an autorefractor (Topcon KR-8900 and KR-800, Topcon Corporation, Tokyo, Japan), and the results were confirmed by the Heine beta 200 retinoscope (Heine Optotechnik, Herrsching, Germany). Then, the angle of deviation was measured by an alternate prism-cover test at distance and near. At distance, patient looked at the letters on the visual acuity chart one line bigger than their best-corrected distance visual acuity (BCVA) and at 33 cm, they fixated on a small detailed accommodative target while performing the cover test [12]. Exotropia was defined as an outward misalignment of the eyes’ visual axes, which was confirmed using the unilateral prism cover test [16]. Also, all intermittent or constant exotropia cases were divided into two groups according to the dominance: 1- patients with dominance of one eye and 2- patients without dominance of one eye. Patients were asked to fix an accommodative target at distance; first, the right eye and then the left eye were occluded for 3 to 5 s, and the recovery speed of ocular alignment from an exotropic state in the occluded eye after removal of the occluder was checked and compared. If the recovery rate after removing the occluder was not different, the patient was put into patients without dominance group. If the recovery rate differed, the eye with a better recovery rate was considered dominant. Afterwards, eye movements were tested by the motility test. Throughout the examinations, the best distance refractive correction, attained based on cycloplegic refraction results, was worn by all patients. Amblyopia was defined as an interocular difference of two lines or more in visual acuity or visual acuity equal or worse than 20/30 (0.2 logMAR) with the best optical correction in presence of an amblyogenic factor [17]. The amblyogenic factors were defined as the presence of (1) an anisometropia (difference in myopia, hyperopia, and astigmatism equal or more than 3.00 D, 1.00 D and 1.50 D, respectively), or (2) constant unilateral heterotropia at distance and/or near fixation and (3) combined anisometropia and strabismus. Amblyopic patients were divided into three severities, mild (best corrected visual acuity in the amblyopic eye 0.2 logMAR), moderate (best corrected visual acuity in the amblyopic eye 0.7 − 0.3 logMAR) and severe (0.8 logMAR or worse) [18, 19]. In the final stage, patients who were candidates for surgical treatment in Farabi Eye Hospital were divided into intermittent and constant groups.
In the intermittent exotropia group, the included patients were those who were followed up several times and because of deterioration in exotropia control, they were referred for surgery. The criteria for surgery were considered as documented serial deterioration in exotropia control assessed by both home and office control scales [20]. For instance, if exotropia occurred at least 50% of the time, or if any increase in the magnitude of deviation was observed after several follow-ups or if a progressive inability to control the exotropia, when the deviation was in manifest phase was observed, they were considered as the manifestation of poor control [20]. In the constant exotropia group, if a patient was younger than three years old and the magnitude of deviation was ≥ 40 prism diopters in two consecutive follow-ups, the patient was referred for surgery. However, in patients older than three years old with constant exotropia, surgery was performed if there was no improvement following nonsurgical treatments and the deviation remained constant in two consecutive follow-ups. In these cases, correction of any significant refractive error, amblyopia therapy, active vision therapy, and prisms prescription if required, were done before surgery.
Statistical analysis
The data was analyzed using the SPSS-26 software (IBM Inc., Chicago, USA). To describe quantitative data, statistical indices such as mean, standard deviation, and statistical tables were used. The normality tests were conducted using the Shapiro–Wilk test. Based on the distribution pattern of each parameter, independent samples t-test or Mann-Whitney U test were used to examine significant differences between the patients with intermittent and constant exotropia. The analysis of covariance was performed in order to remove the effect of the age as a covariate factor. Statistical tests were performed at a level of 5% error.
Results
All patients with exotropia
Among 6159 cases who met the criteria for surgical management, 4244 (68.9%) patients showed constant and 1915 (31.1%) showed intermittent exotropia. The mean age at the time of surgery was 21.9 ± 13.8 (range, 2–77) years, and 3104 (50.4%) of cases were male. The mean age at the time of the surgery in intermittent patients (15.2 ± 11.7 years) was significantly lower than the constant patients (24.9 ± 13.6 years) (P < .001). In terms of laterality, 3598 (58.4%) cases showed exotropia without dominance, and in 2561 (41.6%) patients, dominance was observed in one eye [1307 (21.20%) right exotropia and 1254 (20.40%) left exotropia].
Visual acuity was measured in 5187 (84.2%) cases (3643 constant exotropia and 1544 intermittent exotropia), as the remaining did not cooperate to measure their visual acuity. Among them, 1596 (30.8%) cases had amblyopia [1394 (26.9%) constant exotropia vs. 202 (3.9%) intermittent exotropia, P < .001]. The mean angle of horizontal deviation was 31.9 ± 14.6 (range 4-110) prism diopters at distance and 32.33 ± 15.40 (range 4-123) prism diopters at near. Also, the mean vertical deviation at distance and near was 1.1 ± 4.2 (range, 0–45) and 1.1 ± 4.1 (range, 0–45) prism diopters, respectively. In exotropic patients with amblyopia, the mean angles of horizontal deviation at distance and near were 33.66 ± 15.10 and 33.19 ± 14.78, respectively.
Constant exotropia
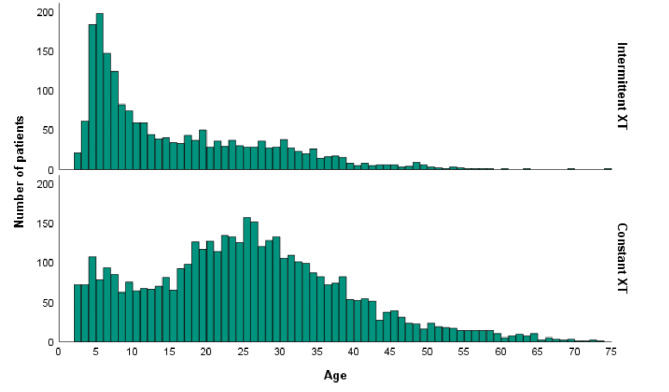
Constant exotropia was found in 4244 cases. The mean age was 24.9 ± 13.6 (range 2–77) years, and 2303 (54.3%) cases were male. Figure 1 illustrates the age distribution of patients with constant exotropia.
Fig. 1.
The age distribution (years) at the time of surgery for patients with constant and intermittent exotropia who underwent surgery
XT; exotropia
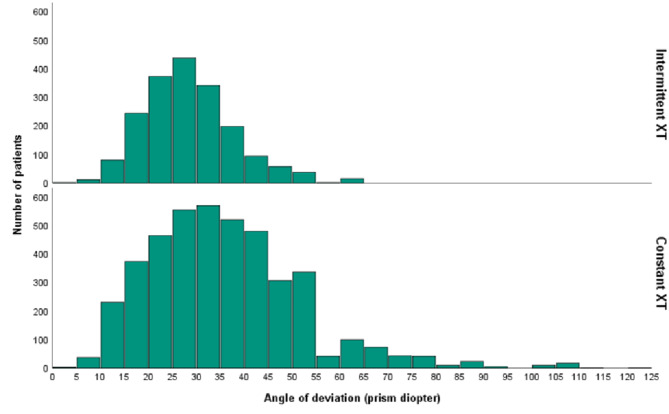
In terms of laterality of exotropia, 2100 (49.4%) cases had no dominance; however, 2144 (50.6%) cases had dominant eye [1068 (49.8%) right eye and 1076 (50.2%) left eye]. In constant exotropia cases, the mean angle of exotropia at distance and near was 34.1 ± 15.8 (range, 5-110) and 34.9 ± 16.9 (range, 4-123) prism diopters, respectively. Also, the mean vertical deviation at distance and near was 1.5 ± 4.9 (range, 0–45) and 1.5 ± 4.8 (range, 0–45) prism diopters, respectively. The distribution of magnitude of exotropia in these patients is shown in Fig. 2.
Fig. 2.
The distribution of the magnitude of exotropia in patients with constant and intermittent exotropia who underwent surgery
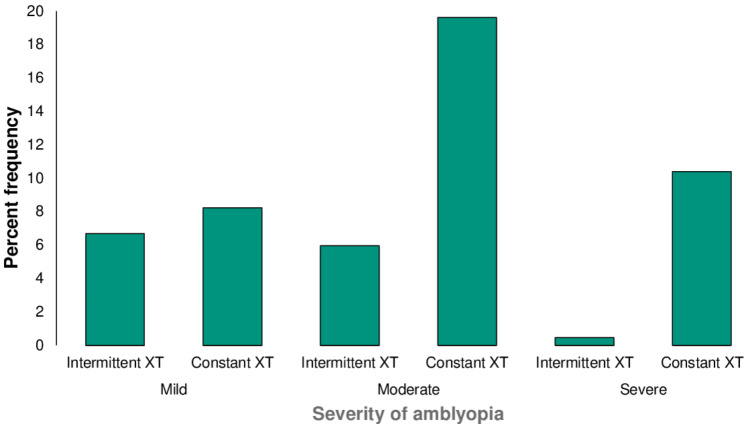
Among 3643 cases whose visual acuity was measured in this group, amblyopia was found in 1394 (38.3%) cases. The frequency of mild, moderate, and severe amblyopia was 300 (21.5%), 715 (51.3%), and 379 (27.2%) cases, respectively (Fig. 3). Regarding the amblyopia type, strabismic and combined-mechanism amblyopia were observed in 984 (70.6%) and 410 (29.4%) cases, respectively. In cases with combined-mechanism amblyopia, 76 (18.5%) cases were anisohyperopic amblyopia; whereas, 92 (22.5%) and 242 (59.0%) cases showed anisomyopic and aniso-astigmatism, respectively.
Fig. 3.
Percent frequency of different severities of unilateral amblyopia among patients with constant and intermittent exotropia who underwent surgery
XT; exotropia
Anisometropia was observed in 821 (19.34%) cases, consisting of 186 (22.6%) anisohyperopic, 200 (24.4%) anisomyopic and 435 (53%) aniso-astigmatism.
Intermittent exotropia
Intermittent exotropia was found in 1915 cases. The mean age was 15.2 ± 11.6 (range 2–74) years and 801 (41.8%) cases were male. The age distribution of these patients is shown in Fig. 1. Regarding the deviation laterality, 1501 (78.4%) cases showed exotropia without any dominance, whereas the remaining 414 (21.6%) patients had dominant eye [195 (47.1%) right eye and 219 (52.9%) left eye]. In intermittent exotropia cases, the mean angle of distance and near exotropia were 27.3 ± 10.1 (range, 4–60) and 26.5 ± 10.3 (range, 5–60) prism diopters, respectively. Accordingly, the angle of vertical deviation in this group at distance and near was 0.2 ± 1.6 prism diopters (range, 0–5) and 0.2 ± 1.5 (range, 0–5) prism diopters, respectively. The distribution of the magnitude of exotropia is shown in Fig. 2.
Among 1544 cases whose visual acuity was measured, amblyopia was found in 202 (13.1%) patients. The frequency of mild, moderate and severe amblyopia were 103 (51%), 92 (45.5%) and 7 (3.5%) cases, respectively (Fig. 3). In terms of the amblyopia types, 13 (6.4%) cases showed anisometropic amblyopia; whereas, strabismic and combined-mechanism amblyopia were observed in 166 (82.2%) and 23 (11.4%) cases, respectively. In this group, the majority of cases with anisometropic amblyopia showed aniso-astigmatism (29 patients), then anisomyopia was observed in 7 cases, and no cases showed anisohyperopic amblyopia. Anisometropia was found in 88 (4.6%) cases in this group, with 14 (15.9%) patients showing anisomyopia, 9 (10.3%) patients showing anisohyperopia and 65 (73.8%) cases showing aniso-astigmatism.
To better compare clinical features in patients with intermittent and constant exotropia, patients were patients with dominance in one eye and patients without dominant eye were compared (Tables 1, 2 and supplementary 2).
Table 1.
Best corrected distance visual acuity (BCVA), refractive status, and horizontal and vertical deviation angle in intermittent or constant exotropia patients with dominance in one eye
| Deviation types | N | Mean ± SD | Minimum | Maximum | P-value* | |||
|---|---|---|---|---|---|---|---|---|
| Age | Intermittent XT | 414 | 20.2 ± 13.0 | 2.0 | 69.0 | < 0.001 | ||
| Constant XT | 2147 | 27.6 ± 13.1 | 2.0 | 77.0 | ||||
| BCVA(logMAR) | Non-dominant eye | Intermittent XT | 407 | 0.22 ± 0.22 | 0.00 | 1.22 | < 0.001 | |
| Constant XT | 1953 | 0.68 ± 0.86 | 0.00 | 2.90 | ||||
| Dominant eye | Intermittent XT | 407 | 0.08 ± 0.13 | 0.00 | 0.70 | 0.833 | ||
| Constant XT | 1953 | 0.09 ± 0.18 | 0.00 | 2.60 | ||||
| Refraction (diopter) | Non-dominant eye | Sphere | Intermittent XT | 414 | -0.60 ± 2.92 | -23.00 | 7.25 | < 0.001 |
| Constant XT | 2147 | 0.11 ± 4.33 | -28.00 | 23.50 | ||||
| Cylinder | Intermittent XT | 414 | 1.36 ± 1.27 | 0.00 | 7.50 | 0.090 | ||
| Constant XT | 2147 | 1.47 ± 1.58 | 0.00 | 10.00 | ||||
| SE | Intermittent XT | 414 | -1.28 ± 3.03 | -24.00 | 7.25 | < 0.001 | ||
| Constant XT | 2147 | -0.63 ± 4.41 | -28.00 | 23.50 | ||||
| Dominant eye | Sphere | Intermittent XT | 414 | -0.35 ± 2.13 | -16.50 | 6.50 | < 0.001 | |
| Constant XT | 2147 | -0.08 ± 1.81 | -17.50 | 9.00 | ||||
| Cylinder | Intermittent XT | 414 | 0.86 ± 0.97 | 0.00 | 5.00 | 0.491 | ||
| Constant XT | 2147 | 0.81 ± 1.06 | 0.00 | 8.00 | ||||
| SE | Intermittent XT | 414 | -1.20 ± 2.47 | -19.00 | 6.50 | < 0.001 | ||
| Constant XT | 2147 | -0.89 ± 2.17 | -19.00 | 6.50 | ||||
| Angle of deviation (prism diopter) | Near | Horizontal | Intermittent XT | 414 | 28.0 ± 11.2 | 7 | 60 | < 0.001 |
| Constant XT | 2147 | 35.5 ± 16.6 | 4 | 123 | ||||
| Vertical | Intermittent XT | 414 | 0.2 ± 1.6 | 0 | 5 | < 0.001 | ||
| Constant XT | 2147 | 1.4 ± 4.9 | 0 | 45 | ||||
| Far | Horizontal | Intermittent XT | 414 | 28.2 ± 10.9 | 8 | 60 | < 0.001 | |
| Constant XT | 2147 | 34.8 ± 16.0 | 5 | 110 | ||||
| Vertical | Intermittent XT | 414 | 0.2 ± 1.6 | 0 | 5 | < 0.001 | ||
| Constant XT | 2147 | 1.4 ± 4.9 | 0 | 45 | ||||
The mean difference is significant at the 0.05 level. BCVA less than 20/400 was considered as follows: finger count: 2.0 logMAR; hand motion: 2.3 logMAR; light perception: 2.6 logMAR; and no light perception (NLP) = 2.9 logMAR. N, number of cases; XT, Exotropia; BCVA, corrected distance visual acuity; SE, spherical equivalent
Table 2.
Best corrected distance visual acuity (BCVA), refractive status, and angle of horizontal and vertical deviation in intermittent or constant exotropia patients without dominance in one eye
| Deviation types | Number | Mean ± SD | Minimum | Maximum | P-value* | |||
|---|---|---|---|---|---|---|---|---|
| Age (year) | Intermittent XT | 1501 | 13.9 ± 11.2 | 2.0 | 74.0 | < 0.001 | ||
| Constant XT | 2097 | 22.2 ± 13.5 | 2.0 | 76.0 | ||||
| BCVA (logMAR) | Right eye | Intermittent XT | 1137 | 0.03 ± 0.11 | 0.00 | 2.30 | 0.012 | |
| Constant XT | 1690 | 0.04 ± 0.17 | 0.00 | 2.30 | ||||
| Left eye | Intermittent XT | 1137 | 0.03 ± 0.11 | 0.00 | 2.30 | 0.041 | ||
| Constant XT | 1690 | 0.04 ± 0.13 | 0.00 | 1.30 | ||||
| Refraction (diopter) | Right eye | Sphere | Intermittent XT | 1501 | 0.36 ± 1.23 | -9.00 | 8.50 | 0.008 |
| Constant XT | 2097 | 0.28 ± 1.52 | -14.50 | 17.00 | ||||
| Cylinder | Intermittent XT | 1501 | 0.43 ± 0.67 | 0.00 | 4.50 | 0.003 | ||
| Constant XT | 2097 | 0.50 ± 0.80 | 0.00 | 7.25 | ||||
| SE | Intermittent XT | 1501 | 0.15 ± 1.31 | -10.62 | 7.00 | 0.075 | ||
| Constant XT | 2097 | 0.03 ± 1.56 | -15.00 | 16.50 | ||||
| Left eye | Sphere | Intermittent XT | 1501 | 0.38 ± 1.25 | -10.00 | 8.25 | < 0.001 | |
| Constant XT | 2097 | 0.39 ± 1.77 | -13.50 | 17.00 | ||||
| Cylinder | Intermittent XT | 1501 | 0.43 ± 0.68 | 0.00 | 5.50 | 0.003 | ||
| Constant XT | 2097 | 0.51 ± 0.81 | 0.00 | 6.50 | ||||
| SE | Intermittent XT | 1501 | 0.17 ± 1.33 | -11.62 | 6.50 | 0.003 | ||
| Constant XT | 2097 | 0.13 ± 1.80 | -14.12 | 17.00 | ||||
| Angle of deviation (prism diopter) | Near | Horizontal | Intermittent XT | 1501 | 26.1 ± 10.0 | 5 | 60 | < 0.001 |
| Constant XT | 2097 | 34.4 ± 16.5 | 4 | 80 | ||||
| Vertical | Intermittent XT | 1501 | 0.2 ± 1.5 | 0 | 5 | < 0.001 | ||
| Constant XT | 2097 | 1.5 ± 4.8 | 0 | 40 | ||||
| Far | Horizontal | Intermittent XT | 1501 | 27.1 ± 9.8 | 4 | 60 | < 0.001 | |
| Constant XT | 2097 | 33.3 ± 15.6 | 4 | 80 | ||||
| Vertical | Intermittent XT | 1501 | 0.2 ± 1.6 | 0 | 5 | < 0.001 | ||
| Constant XT | 2097 | 1.6 ± 4.9 | 0 | 40 | ||||
* The mean difference is significant at the 0.05 level. BCVA less than 20/400 was considered as follows: finger count: 2.0 logMAR; hand motion: 2.3 logMAR; light perception: 2.6 logMAR; and no light perception (NLP) = 2.9 logMAR. N, number of cases; XT, Exotropia; BCVA, corrected distance visual acuity; SE, spherical equivalent
Discussion
The present study investigated the clinical features of patients with intermittent and constant exotropia who underwent surgery. Among them, 3598 (58.4%) showed no dominance and 2561 (41.6%) cases showed dominance in one eye. The mean BCVA in patients with constant exotropia was significantly worse than the intermittent cases; in both cases with dominance in one eye and no dominance cases. In terms of the refractive error and in cases with dominance in one eye, the spherical equivalent was significantly different between the intermittent and constant exotropia groups. Intermittent patients showed more minus results (-1.28 ± 3.03 diopter) than the constant ones (-0.63 ± 4.41 diopter) in the non-dominant eye. The same scenario happened in the dominant eye (P < .001); however, in the dominant eye, the difference between intermittent (-1.20 ± 2.47 diopter) and constant groups (-0.89 ± 2.17 diopter) was 0.31 diopter which may not be clinically significant. Moreover, the mean angle of horizontal and vertical deviation at distance and near in patients with constant exotropia was significantly higher than the intermittent cases either when there was a dominance in one eye or in cases with no dominance (both P < .001).
The leading treatment strategy in patients with constant exotropia is surgical intervention. The main reason is the presence of large angle constant deviation, the danger of amblyopia in young children and loss of normal binocular function. In a retrospective consecutive case series, Keenan and Willshaw reviewed documents of 42 non-paralytic patients with exotropia who underwent surgery over five years. Eleven out of 42 patients (26.2%) had constant exotropia, 17 (40.5%) had pseudo divergence excess, and 14 (33.3%) had true divergence excess exotropia. The median age at the time of surgery for constant exotropia, true divergence excess and pseudo divergence excess was 50, 66.5 and 68 months, respectively. Our sample size (6159) was remarkably bigger than them and we found 4244 (68.9%) of patients with constant exotropia with age at time of surgery being 24.9 ± 13.6 years. They found that in cases with constant exotropia, the median refractive error before surgery was + 2.25 diopter and 3 out of 11 patients with constant exotropia had anisometropia. The median refractive error for pseudo divergence excess and true divergence excess groups were + 2.50 diopter and + 2.00 diopter, respectively [21]. In contrast, we found minus spherical equivalent refractive error in the non-dominant (-0.63 ± 4.41 diopter) and dominant eye (-0.89 ± 2.17 diopter) in the constant strabismus cases, when there was dominance in one eye and less hyperopic amounts in the right (0.03 ± 1.56 diopter) and left (0.13 ± 1.80 diopter) eyes in patients with no dominance. The different values between our study and Keenan and Willshaw study can be mainly attributed to the considerably different sample size and inclusion criteria of patients with different types of exotropia as well as different age distribution. In another retrospective study, Smith et al. investigated the visual acuity of 600 patients with primary intermittent exotropia to report the incidence rate of amblyopia in these patients. They reported that 412 (68.7%) patients had almost the same visual acuity between the two eyes, 111 (18.5%) patients had unequal visual acuity of one line difference between the two eyes and 77 (12.8%) patients had amblyopia. The authors reported a higher prevalence of amblyopia in constant exotropia (21%) compared to the intermittent exotropia (9.3%) [22], which is in line with our findings with 26.9% amblyopia in the constant and 3.9% in the intermittent group. As expected, strabismic amblyopia was the most prevalent amblyopia type in our study with 70.6% in the constant exotropia and 82.2% in the intermittent group. We found the high frequency of strabismic amblyopia in the intermittent exotropia group. The point that needs to be considered is that these patients were those whose exotropia became worse over time in terms of constancy and frequency, so that they became amblyopic. In Yang et al. study, prevalence of amblyopia was 4.2% which is in accordance with our findings in the intermittent exotropia group (3.9%).9
In cases with anisometropic amblyopia, aniso-astigmatism was the most common type in both groups (242 constant cases and 29 intermittent patients). In a retrospective study in 471 children with intermittent exotropia between 3 and 15 years, those with cylindrical hyperopic anisometropia showed a higher possibility of developing amblyopia [23].
Regardless of amblyopia in anisometropic cases, anisometropia was observed in 821 (19.34%) cases in the constant and 88 (4.6%) patients in the intermittent group, with aniso-astigmatism being the most prevalent type in both constant (435 patients) and intermittent (64 patients) groups. In other words, the prevalence of anisometropia in the constant group was about 4 times more than in the intermittent group. To the best of our knowledge, this study is the first to report anisometropia prevalence in cases with constant exotropia. The current evidence in the literature is mostly attributed to the intermittent exotropia and not much data on the clinical profile of the constant group has been provided yet.
As our data demonstrated, the most common type of spherical equivalent refractive error was myopia in cases with dominance in one eye in both study groups, and emmetropia in cases with no dominance. This is in accordance with previous findings that myopia has been related to the occurrence of exotropia [24–26]. Although the underlying reason for this association has not been clarified, one potential explanation is that the presence of exotropia might increase the accommodation demand which might lead to myopic shift [27]. Therefore, exotropia can be a risk factor for the development of myopia. In a retrospective study, Yang et al. reported the clinical characteristics of 1228 patients with intermittent exotropia who received surgery in China from 2009 to 2013. The mean age of onset was 6.77 ± 6.43 years and the mean age at surgery was 13.7 ± 8.8 years. The authors reported that the mean refractive error of these patients in the right and left eyes were − 0.84 ± 2.69 diopter and − 0.72 ± 2.58 diopter, respectively. Their finding of myopia in intermittent exotropia patients is in agreement with our findings [9].
Another finding in our study was that intermittent exotropia cases underwent surgery at a younger age than constant cases. A retrospective study on 184 pediatric patients (< 19 years old) with intermittent exotropia that spanned over 20 years showed that the angle of deviation increased by 10 prism diopters or more in approximately half of the patients; however, the deviation resolved spontaneously only in 4%[28]. Another study that followed intermittent exotropia cases (mean age 8.6 ± 3.6 years old) for three years, reported that 34% of patients deteriorated in exotropia control over time, while 66% had improvement or had no deterioration. Comparing their baseline parameters showed that patients with no deterioration had significantly smaller angle of deviation, larger fusional reserve and larger fusional recovery [6]. Another study showed equal chance of improvement or deterioration in distance deviation after 5 years in participants between 5 and 25 years [7]. Cotter et al. also did not show any deterioration in children between 3 and 10 years with intermittent exotropia who were received no treatment over 3 years [5].
The current study had several limitations. The most important one is that the study was retrospective and performed in only one center; however, Farabi Eye Hospital is the biggest academic and educational ophthalmology center in Iran. Moreover, we did not record postoperative data of patients who underwent surgical intervention to determine the favorable and unfavorable predictors of surgery success in exotropia. Also, no data was collected regarding the binocular status, such as stereopsis, before surgery. In addition, visual acuity was measured using a Snellen E chart. Using a pediatric visual acuity test for younger age instead could have increased the response rates.
Conclusions
The constant exotropia group showed worse BCVA and a higher magnitude of deviation compared to the intermittent cases. Myopia was the most common type of refractive error in both groups. Amblyopia and anisometropia were more prevalent in the constant group than in the intermittent group. In both groups, the most common type of amblyopia was strabismic amblyopia, and aniso-astigmatism was the most common type of anisometropia. It should be noted that the obtained data in the intermittent group cannot be generalized to all intermittent exotropia patients, as the patients in this study represented a subset of intermittent exotropia patients who required surgery due to deterioration in alignment control over time.
Acknowledgements
Not applicable.
Abbreviations
- BCVA
best corrected distance visual acuity
Author contributions
MR.A, B. M. and M. Kh contributed to the design of the research and providing the facilities. (A) H. and Y. A.Sh. collected the data. M. Kh and E. A analyzed the results and wrote the original draft. (B) M. and MR.A revised the manuscript.
Funding
There was no special funder for this study and no financial disclosure for the authors.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The ethical committee of Tehran university of medical sciences approved the protocol of this study (IR.TUMS.FNM.REC.1401.038) and the study adhered to the tenets of the Declaration of Helsinki and HIPAA. Informed written consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jampolsky A. Ocular deviations. Int Ophthalmol Clin. 1964;4:567–627. [Google Scholar]
- 2.Wright KW. Exotropia. In. Pediatric ophthalmology and strabismus. Springer; 2003. pp. 224–31.
- 3.Pan CW, Zhu H, Yu JJ, et al. Epidemiology of intermittent exotropia in preschool children in China. Optom Vis Sci. 2016;93:57–62. [DOI] [PubMed] [Google Scholar]
- 4.Mohney BG, Cotter SA, Chandler DL, et al. Three-year observation of children 3 to 10 years of age with untreated intermittent exotropia. Ophthalmology. 2019;126:1249–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cotter SA, Mohney BG, Chandler DL et al. Natural history of childhood intermittent exotropia over a 3-year period. Invest Ophthalmol Vis Sci 2016;57.
- 6.Kwok JJ, Chong GS, Ko ST, et al. The natural course of intermittent exotropia over a 3-year period and the factors predicting the control deterioration. Sci Rep. 2016;6:27113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romanchuk KG, Dotchin SA, Zurevinsky J. The natural history of surgically untreated intermittent exotropia—looking into the distant future. J AAPOS. 2006;10:225–31. [DOI] [PubMed] [Google Scholar]
- 8.Holmes JM, Hatt S, Leske D. Is intermittent exotropia a curable. condition? Eye. 2015;29:171–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang M, Chen J, Shen T, et al. Clinical characteristics and surgical outcomes in patients with intermittent exotropia: a large sample study in South China. Medicine. 2016;95:e2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu H, Sun J, Xia X, et al. Binocular status after surgery for constant and intermittent exotropia. Am J Ophthalmol. 2006;142:822–6. [DOI] [PubMed] [Google Scholar]
- 11.Wang X, Gao X, Xiao M, et al. Effectiveness of strabismus surgery on the health-related quality of life assessment of children with intermittent exotropia and their parents: a randomized clinical trial. J AAPOS. 2015;19:298–303. [DOI] [PubMed] [Google Scholar]
- 12.Scheiman M, Wick B. Clinical management of binocular vision: heterophoric, accommodative, and eye movement disorders. Lippincott Williams & Wilkins; 2008.
- 13.Repka MX, Chandler DL, Holmes JM, et al. The relationship of age and other baseline factors to outcome of initial surgery for intermittent exotropia. Am J Ophthalmol. 2020;212:153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Griffin JR, Grisham JD. Binocular anomalies: diagnosis and vision therapy; 2002.
- 15.Kraft S. Selected exotropia entities and principles of management. Clinical strabismus management: Principles and surgical techniques. Philadelphia: WB Saunders; 1999. pp. 193–9. [Google Scholar]
- 16.Evans BJ. Pickwell’s binocular vision anomalies. Elsevier Health Sciences; 2021.
- 17.Zagui RMB. Amblyopia: types, diagnosis, treatment, and new perspectives. In: American Academy of Opthalmology; 2019.
- 18.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–78. [DOI] [PubMed] [Google Scholar]
- 19.Rajavi Z, Moghadasifar H, Feizi M, et al. Macular thickness amblyopia JOVR. 2014;9:478–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenbaum AL, Santiago AP. Clinical strabismus management: principles and surgical techniques. David Hunter; 1999.
- 21.Keenan J, Willshaw H. The outcome of strabismus surgery in childhood exotropia. Eye. 1994;8:632–7. [DOI] [PubMed] [Google Scholar]
- 22.Smith K, Kaban TJ, Orton R. Incidence of amblyopia in intermittent exotropia. Am Orthopt J. 1995;45:90–6. [Google Scholar]
- 23.Ku M, Paik HJ. The association between amblyopia and anisometropia in intermittent exotropia. J Korean Ophthalmol Soc. 2009;50:1686–91. [Google Scholar]
- 24.Zhu H, Yu JJ, Yu RB, et al. Association between childhood strabismus and refractive error in Chinese preschool children. PLoS ONE. 2015;10:e0120720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weakley DR Jr. The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001;108:163–71. [DOI] [PubMed] [Google Scholar]
- 26.Ekdawi NS, Nusz KJ, Diehl NN, et al. The development of myopia among children with intermittent exotropia. Am J Ophthalmol. 2010;149:503–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huynh S, Wang X, Ip J, et al. Prevalence and associations of anisometropia and aniso-astigmatism in a population based sample of 6 year old children. Br J Ophthalmol. 2006;90:597–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nusz KJ, Mohney BG, Diehl NN. The course of intermittent exotropia in a population-based cohort. Ophthalmology. 2006;113:1154–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.