Abstract
Patient: Male, 13-year-old
Final Diagnosis: Sublingual dermoid cyst
Symptoms: Difficulties in food intake • elevation of the floor of the mouth and tongue • growing mass • speech disorders
Clinical Procedure: Surgical excision
Specialty: Otolaryngology • Surgery
Objective:
Rare disease
Background:
Ranulas are typical causes of sublingual cysts in children. However, our case was histopathologically confirmed to be a dermoid cyst. Epidermoid and dermoid cysts of the floor of the mouth account for <0.01% of all oral cavity lesions and 0.29% of head and neck tumors in children. Salivary congestive cysts (ranulas) involve the sublingual salivary glands or the common duct of the sublingual and submandibular salivary glands. This report describes a 13-year-old boy presenting with a sublingual cyst, diagnosed by histopathology as a dermoid cyst. Treatment is based on surgical removal of the cyst, sometimes along with the altered salivary gland.
Case Report:
A 13-year-old boy was admitted to the Department of Otolaryngology with the Subdivision of Maxillofacial Surgery for the diagnosis of a tumor localized under the tongue. A significant growth of the tumor during a 3-month period was noticed, with appearance of a mass effect, speech disorders, and difficulties in eating. Significant elevation of the floor of the mouth and tongue was shown. The presence a ranula was indicated. Surgical excision was performed using intra-oral excision. Histopathological examination revealed a diagnosis of dermatoid cyst.
Conclusions:
This case highlights the importance of detailed histopathological diagnosis of lesions and the usefulness of imaging methods like magnetic resonance imaging (MRI), ultrasound (US) or computed tomography (CT). Our patient had a dermoid cyst, which appears rarely among children in the floor of the mouth. This shows the significance of their proper differentiation, as some may be misdiagnosed as ranula.
Key words: Child, Dermoid Cyst, Epidermal Cyst, Mouth Floor, Ranula
Introduction
A common lesion in the sublingual area is an inflammatory pseudocyst (ranula) [1,2]. Ranulas account for approximately 6% of all cystic lesions in the oral cavity [3]. The form through mucus escape from the sublingual gland, causing mylohyoid muscle herniation in a submandibular space and surrounding area [4]. Differential diagnosis may include an infection, cystic masses of salivary gland origin, lymphatic malformation, branchial cleft remnant, and thyroglossal duct cyst [2]. Epidermoid and dermoid cysts of the floor of the mouth account for <0.01% of all oral cavity lesions, with dermoid being twice as common as epidermoid [5]. Cysts are classified as epidermoid if the lining consists solely of epithelium, as dermoid if they contain skin appendages, and as teratoid if they include other tissues like muscle, cartilage, or bone [2]. Those lesions are derived from entrapped midline endodermal and ectodermal remnants appearing during the third and fourth embryonic weeks. They appear as a result of fusion of the first and second branchial arches [2]. The development of midline cysts in the floor of the mouth is not clearly understood, with proposed theories including dysontogenic, traumatic, and thyroglossal anomaly origins [6]. We report the case of a 13-year-old boy with a sublingual cyst, diagnosed by histopathology as dermoid. We highlight the similarities and differences between 2 previously published cases involving dermoid cysts on the floor of the mouth, and discuss the size, symptoms, and surgical procedures used to treat these masses.
Case Report
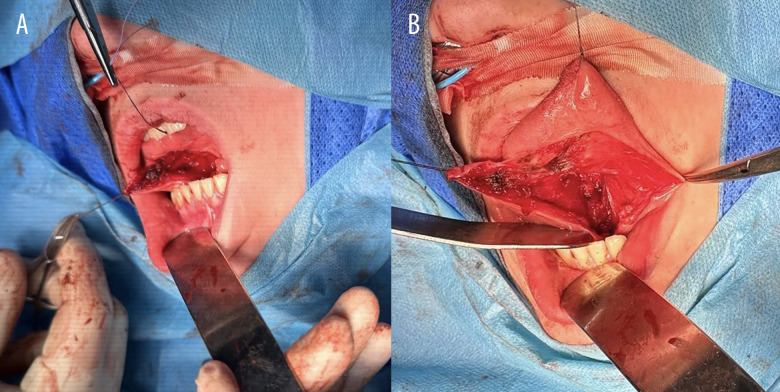
A 13-year-old boy with autism spectrum disorder was admitted to the Otolaryngology Department with a Maxillofacial Surgery Subdivision for diagnosis of a tumor located under the tongue. The lesion was noticed by the child’s parents approximately 3 months earlier. Since then, there has been a significant increase in the size of the tumor, with the appearance of a mass effect, leading to speech disturbances and eating disorder (Figure 1). During the medical history-taking, trauma and infection were ruled out as causes of the lesion. He had a significant elevation of the floor of the mouth and the tongue, with a shift toward the throat. It was originally suspected that the lesion was a ranula. An MRI scan after intravenous administration of contrast suggested the presence of bilateral retention cysts of the submandibular glands.
Figure 1.
Intra-oral photograph obtained at initial visit. Arrow indicates cystic lesion.
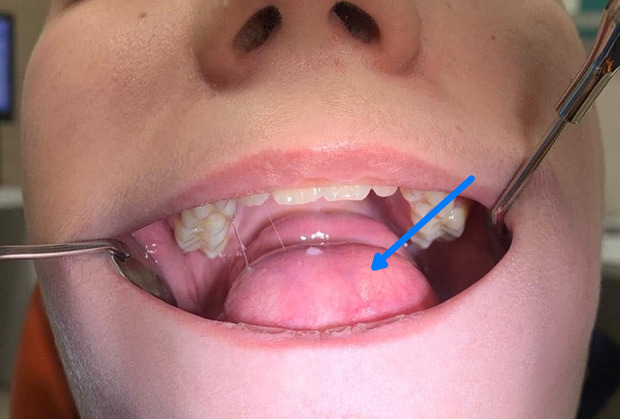
The patient was qualified for surgical removal of the lesion in the operating room. Under general anesthesia with nasal intubation, surgical excision was performed using an intra-oral approach from a midline cut of the floor of the mouth (Figure 2).
Figure 2.
Intraoperative appearance. intra-oral midline incision providing adequate access to the lesion (A) Lesion appearance after incision. (B) After removal.
A tumor measuring 7.2×4.6×3.5 cm (Figure3) was dissected. The thin-walled cyst with a smooth outer surface and an uneven lining was filled with a doughy substance. Histopathologically, the lesion was found to be a dermoid cyst lined with keratinizing squamous epithelium (Figure 4) in contrast to the previously suspected ranula. Sebaceous glands were present in the cyst wall (Figure 5). After radical excision, the patient required intubation postoperatively due to swelling of the tongue. The tube was removed after 24 hours, when the swelling had diminished.
Figure 3.

Macroscopic characteristic of cyst after removal.
Figure 4.
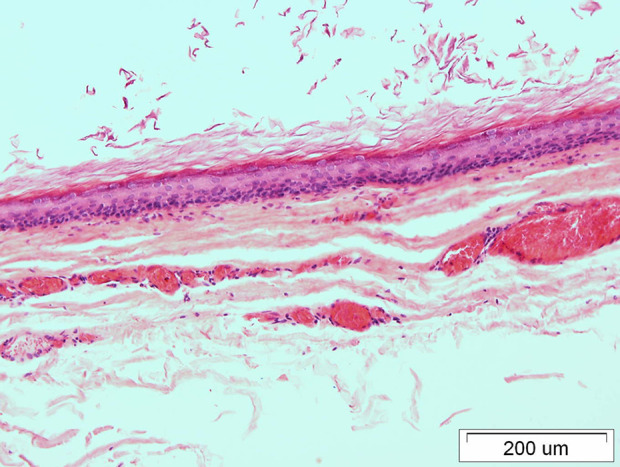
Dermoid cyst lined with keratinizing squamous epithelium (hematoxylin and eosin staining, original magnification ×200).
Figure 5.
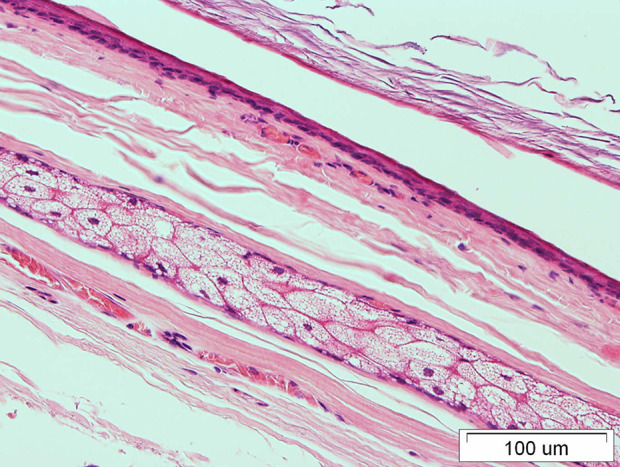
Sebaceous glands in the dermoid cyst wall (hematoxylin and eosin staining, original magnification ×100).
Discussion
This case report describes the importance of a properly conducted diagnostic pathway and the cooperation of physicians from different specialties. Maintaining oncological vigilance is crucial to treating patients quickly and effectively for growing masses on the floor of the mouth. Histopathological examination remains the criterion standard for lesions requiring surgical removal.
In cases involving lesions in the head and neck region, the correct choice of surgical method should also consider cosmetic outcomes. While these outcomes are a desirable factor in modern medicine, they should not outweigh the primary health benefits.
Congenital cysts of ectodermal origin are uncommon in the oral cavity, accounting for only 1.6%, and epidermoid cysts are particularly rare in this location [7]. Dermoid cyst is an epithelial-lined cavity that features keratinization and contains skin appendages, including sebaceous and sweat glands, as well as hair follicles in the cyst wall [8]. Typically, these cysts remain asymptomatic until they rupture [9], or they may become symptomatic due to secondary infection or when they grow large enough to damage surrounding anatomical structures [10]. Dermoid cysts in the floor of the mouth are developmental anomalies caused by the entrapment and subsequent proliferation of epithelial cells during the midline fusion of the first and second branchial arches in the third and fourth weeks of embryonic development [11]. Epidermoid and dermoid cysts are benign inclusion cysts [5,8] Approximately less than 1% of dermoid cysts have been noted to have a malignant transformation, and if so, it they are often reported as squamous cell carcinoma arising within the cyst [12–14]. About 7% of epidermoid and dermoid cysts occur in the head and neck, and only 1.6% are found in the oral cavity, of which <0.01% are on the floor of the mouth [15–17].
Clinically, dermoid cysts appearing in the head and neck region are typically painless, slow-growing masses in the sublingual, submental, or submandibular regions. In the oral cavity, they are either sublingual or submental, initially forming in the midline, that swell from the anterior portion of this region and can grow significantly before becoming noticeable [7]. These cysts result from the entrapment of epithelial remnants during embryonic fusion, making them common in fusion zones, particularly along the midline [10]. They can displace the tongue, leading patients to present with dysphagia, dysphonia, and dyspnea [6]. When located lower, growing in an inferior direction, they often cause a characteristic double-chin appearance [6].
Our case was similar to that of a 17-year-old girl who also had a 3-month history of a growing mass in the mouth floor [18], causing superior and posterior displacement of the tongue. Although she had not yet exhibited any symptoms, histopathological examination following the surgical removal revealed that the mass was a dermoid cyst. Its size was similar to that of our case, measuring 6×5×3.5 cm [18]. Another case comparable to ours is that of a 21-year-old woman who exhibited symptoms of difficulty in chewing and swallowing solid foods for approximately 2 years, which is a lesion growth period 8 times longer than in our patient [7]. The size of the mass was similar to that of our patient’s, measuring 5.5×5.6×4.5 cm. In this case, surgical removal was performed without making any skin incision. Sharp and blunt dissection of mucosa was performed per os, without causing any cosmetic harm to the patient. The course of this surgical procedure was similar to our surgical approach [7].
Depending on their location, the potential differential diagnoses for dermoid cysts encompass lipoma, epidermoid cyst, pilar cyst (including isthmus-catagen cyst and trichilemmal cyst), furuncle, branchial cleft cyst, milia, pilonidal cyst, calcinosis cutis, pachyonychia congenita, steatocystoma, and cutaneous manifestations of Gardner syndrome [9]. with a sublingual location, the foremost differential diagnosis is ranula, accounting for 6% of intra-oral cysts of the salivary glands [4]. Dermoid cysts are usually located superficially or in the anterior orbit, often molding the bone, and rarely causing bone lysis; they are common and typically diagnosed in infancy or early childhood [19]. In contrast, epidermoid cysts can occur anywhere in the body and are usually diagnosed in the later stages of life [20]. When located in the orbit, they typically develop in association with bone. Although generally considered benign, in rare cases they are malignant [19].
Here, we presented a case of a dermoid cyst initially diagnosed as a ranula. Imaging methods like US, CT, and MRI are useful for preoperative diagnosis, to guide the anatomical plane, to determine the type of surgery, and to plan surgery. On US, dermoid cysts typically appear as well-defined, homogeneous, and hypoechoic cystic lesions [20]. CT and MRI are crucial for diagnosing dermoid cysts and planning their surgical removal. CT is effective in confirming the diagnosis of large dermoid cysts, but it is not as effective for smaller ones. Radiologically, dermoid cysts usually present as non-enhancing, low-density masses on CT scans and are hyperintense on T1-weighted (T1-W) MRI sequences, with varying signal intensity on T2-weighted (T2-W) sequences [21].
In our case, only post-surgical histopathological examination allowed a definitive diagnosis of dermoid cyst to be made. In the literature, preoperative fine-needle aspiration cytology (FNAC) was reported to be more informative and guiding than diagnostic imaging [22], and it helps in differentiating ranula from dermoid or epidermoid cysts. However, the dense fluid within cysts makes aspiration difficult, reducing the effectiveness of this method [23].
Treatment for cysts involves surgical enucleation via an intra-oral or extra-oral approach, depending on size and location [7], to remove as much of the cyst capsule as possible to prevent recurrence. In our case, the approach applied was the surgical enucleation of the dermoid cyst using intra-oral approach. It was highly effective in removing the cyst using blind manipulation with the fingertip. An extra-oral approach is employed for very large cysts (>6 cm) impacting the submandibular and submental spaces, as well as in cases of infection that might compromise the patient’s airway [7]. Due to the lack of indications of such a risk, we decided to use an intra-oral approach. Most authors recommend an intra-oral approach for sublingual cysts of small or moderate size (less than 6 cm) located above the mylohyoid muscle, which leads to very good cosmetic and functional results [24]. Therefore, an intra-oral approach should be attempted initially, regardless of whether the cyst is large or of the inferior type [25].
Conclusions
Sublingual dermoid cysts are uncommon in the floor of the mouth, which makes them a diagnostic and therapeutic challenge. Proper differentiation of benign neoplastic conditions from malignant lesions is key to correct diagnosis. Dermoid cysts are easily misdiagnosed, especially as a ranula. CT is quick and cost-effective compared to contrast-enhanced MRI, but MRI is better at showing soft-tissue and vascular involvement, which is helpful for surgical planning. To prevent recurrence, treatment is always radical excision of the lesion via an intra-oral or extra-oral approach. The local anesthetic with epinephrine should be injected around the cyst, avoiding direct injection into it [26]. To prevent skin sagging after removal of larger cysts, a small area of epidermis above the cyst is excised to allow for customized surgical margins. It is essential to subject all surgically removed cysts to histopathological examination to confirm complete removal and avoid mis-diagnosis. Regular histopathologic analysis remains crucial to address the risk of malignant transformation [27]. Once a cyst has ruptured, its removal becomes more challenging [28].
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Dutta M, Saha J, Biswas G, et al. Epidermoid cysts in head and neck: Our experiences, with review of literature. Indian J Otolaryngol Head Neck Surg. 2013;65(Suppl. 1):14–21. doi: 10.1007/s12070-011-0363-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Misch E, Kashiwazaki R, Lovell MA, Herrmann BW. Pediatric sublingual dermoid and epidermoid cysts: A 20-year institutional review. Int J Pediatr Otorhinolaryngol. 2020;138:110265. doi: 10.1016/j.ijporl.2020.110265. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A, Karjodkar FR. Plunging ranula: A case report. ISRN Dent. 2011;2011:806928. doi: 10.5402/2011/806928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olojede ACO, Ogundana OM, Emeka CI, et al. Plunging ranula: Surgical management of case series and the literature review. Clin Case Rep. 2018;6(1):109–14. doi: 10.1002/ccr3.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyngdoh TS, Konsam R, Venkatesh MA, Aggarwal S. Giant sublingual epidermoid cyst – an unusual case report. Indian J Surg. 2010;72(Suppl. 1):318–20. doi: 10.1007/s12262-010-0097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kandogan T, Koç M, Vardar E, et al. Sublingual epidermoid cyst: A case report. J Med Case Rep. 2007;1:87. doi: 10.1186/1752-1947-1-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohta N, Watanabe T, Ito T, et al. A case of sublingual dermoid cyst: Extending the limits of the oral approach. Case Rep Otolaryngol. 2012;2012:634949. doi: 10.1155/2012/634949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahoo NK, Choudhary AK, Srinivas V, Tomar K. Dermoid cysts of maxillofacial region. Med J Armed Forces India. 2015;71:S389–S94. doi: 10.1016/j.mjafi.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zito PM, Scharf R. Epidermoid cyst. StatPearls. 2023. [PubMed]
- 10.de Mendonca JG, Jardim EG, dos Santos C, et al. Epidermoid cyst: Clinical and surgical case report. Ann Maxillofac Surg. 2017;7(1):151–54. doi: 10.4103/ams.ams_68_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meyer I. Dermoid cysts (dermoids) of the floor of the mouth. Oral Surg Oral Med Oral Pathol. 1955;8(11):1149–64. doi: 10.1016/0030-4220(55)90380-7. [DOI] [PubMed] [Google Scholar]
- 12.Pradhan P, Thapa M. Dermoid Cyst and its bizarre presentation. J Nepal Med Assoc. 2014;52(194):837–44. [PubMed] [Google Scholar]
- 13.Arab M, Ashtiani AJ, Faghih N, et al. Malignancy arising in dermoid cysts: A case report and literature review. J Family Reprod Health. 2023;17(4):264–68. doi: 10.18502/jfrh.v17i4.14599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J, Yang Z. Malignant transformation of a dermoid cyst in the maxillo-facial region: Review and case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(6):737–41. [Google Scholar]
- 15.Kim IK, Kwak HJ, Choi J, et al. Coexisting sublingual and submental dermoid cysts in an infant. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(6):778–81. doi: 10.1016/j.tripleo.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 16.Longo F, Maremonti P, Mangone GM, et al. Midline (dermoid) cysts of the floor of the mouth: Report of 16 cases and review of surgical techniques. Plast Reconstr Surg. 2003;112(6):1560–65. doi: 10.1097/01.PRS.0000086735.56187.22. [DOI] [PubMed] [Google Scholar]
- 17.MacNeil SD, Moxham JP. Review of floor of mouth dysontogenic cysts. Ann Otol Rhinol Laryngol. 2010;119(3):165–73. doi: 10.1177/000348941011900304. [DOI] [PubMed] [Google Scholar]
- 18.Kyriakidou E, Howe T, Veale B, Atkins S. Sublingual dermoid cysts: Case report and review of the literature. J Laryngol Otol. 2015;129(10):1036–39. doi: 10.1017/S0022215115001887. [DOI] [PubMed] [Google Scholar]
- 19.Hoang VT, Trinh CT, Nguyen CH, et al. Overview of epidermoid cyst. Eur J Radiol Open. 2019;6:291–301. doi: 10.1016/j.ejro.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakajima K, Korekawa A, Nakano H, Sawamura D. Subcutaneous dermoid cysts on the eyebrow and neck. Pediatr Dermatol. 2019;36(6):999–1001. doi: 10.1111/pde.13976. [DOI] [PubMed] [Google Scholar]
- 21.Kumaran S, Srinivasa R, Ghosal N. Unusual radiological presentation of intracranial dermoid cyst: A case series. Asian J Neurosurg. 2019;14(1):269–71. doi: 10.4103/ajns.AJNS_304_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naik M, Hooda S, Ahmad F. Giant epidermal cyst of floor of mouth: Case report. Indian J Otolaryngol Head Neck Surg. 2023;75(2):1137–39. doi: 10.1007/s12070-022-03412-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mesolella M, Cantone E, Galli V, Iengo M. Challenging management of a giant sublingual dermoid cyst rapidly enlarged throughout pregnancy and influence of hormonal factors. Surg Sci. 2013;4:216–18. [Google Scholar]
- 24.El-Hakim IE, Alyamani A. Alternative surgical approaches for excision of dermoid cyst of the floor of mouth. Int J Oral Maxillofac Surg. 2008;37(5):497–99. doi: 10.1016/j.ijom.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 25.Akao I, Nobukiyo S, Kobayashi T, et al. A case of large dermoid cyst in the floor of the mouth. Auris Nasus Larynx. 2003;30(Suppl.):137–39. doi: 10.1016/s0385-8146(02)00121-9. [DOI] [PubMed] [Google Scholar]
- 26.bin Manie M, Al-Qahtani KH, al Ammar A, et al. Epidermoid cyst of the suprasternal region: A rare case report. Braz J Otorhinolaryngol. 2020;86(1):133–35. doi: 10.1016/j.bjorl.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wollina U, Langner D, Tchernev G, et al. Epidermoid cysts – a wide spectrum of clinical presentation and successful treatment by surgery: A retrospective 10-year analysis and literature review. Open Access Maced J Med Sci. 2018;6(1):28–30. doi: 10.3889/oamjms.2018.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoang VT, Trinh CT, Nguyen CH, et al. Overview of epidermoid cyst. Eur J Radiol Open. 2019;6:291–301. doi: 10.1016/j.ejro.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]