Abstract
BACKGROUND
Adult spinal reconstructive surgery that requires multilevel spinal fusion is highly invasive and requires two-stage surgery using lateral lumbar interbody fusion (LLIF) and/or percutaneous pedicle screw (PPS) fixation to make it less invasive. However, it is still difficult to make spinal osteotomy less invasive, and the high complication rate is an issue.
OBSERVATIONS
The authors present the surgical techniques of a two-stage Schwab grade 4 spinal osteotomy using LLIF, which could reduce surgical invasiveness and enable good correction and anterior spinal column reconstruction for lumbar kyphosis, and also report a case treated with this procedure. The first surgery consisted of L2–5 LLIF and L6–S1 posterior lumbar interbody fusion with temporary PPS fixation. The second surgery, 2 weeks after the first surgery, was a grade 4 osteotomy performed in the L4 vertebral body at a 30° angle toward the center of the LLIF cage between L3 and L4, followed by PPS fixation from T10 to the pelvis and additional fixation with two collateral rods.
LESSONS
Two-stage grade 4 osteotomy using LLIF could reduce invasiveness and blood loss while providing good anterior support. This surgical method is expected to make spinal reconstruction surgeries requiring osteotomy less invasive.
Keywords: spinal osteotomy, lateral lumbar interbody fusion, lumbar kyphosis, two-stage surgery, minimally invasive spinal stabilization, case report
ABBREVIATIONS: 3CO = three-column osteotomy, ACR = anterior column realignment, ALIF = anterior lumbar interbody fusion, ASD = adult spinal deformity, CT = computed tomography, LL = lumbar lordosis, LLIF = lateral lumbar interbody fusion, OLIF = oblique lumbar interbody fusion, PI = pelvic incidence, PLIF = posterior lumbar interbody fusion, PPS = percutaneous pedicle screw, PSO = pedicle subtraction osteotomy, PT = pelvic tilt, SVA = sagittal vertical axis.
Adult spinal reconstructive surgery that requires multilevel spinal fusion is highly invasive in older patients with adult spinal deformity (ASD); however, in our aging society, ASD poses a significant burden to older patients, and its incidence is still increasing. Currently, two-stage surgery using lateral lumbar interbody fusion (LLIF) and/or percutaneous pedicle screw (PPS) fixation has been performed to make ASD surgery less invasive. However, it is still difficult to make spinal three-column osteotomy (3CO) less invasive, and adverse events such as neurological complications, perioperative massive blood loss, postoperative correction loss, and rod breakage are issues.1–4 Performing complex adult reconstructive surgery often requires 3CO, including grade 3–5 spinal osteotomy in the Schwab classification5 rather than posterior column osteotomy such as grade 1 or 2 spinal osteotomy. Our approach was to apply staged pedicle subtraction osteotomy (PSO; grade 4 osteotomy)6–11 following LLIF, rather than performing a single-stage anterior support cage insertion following PSO using a posterior lumbar interbody fusion (PLIF) procedure, a so-called closing and opening wedge osteotomy.8, 12 We present the surgical techniques of a two-stage grade 4 spinal osteotomy using LLIF, which could reduce surgical invasiveness and enable good correction and anterior spinal column reconstruction for lumbar kyphosis, and we report a case treated with this procedure.
Illustrative Case
History and Examination
A 57-year-old woman had gait disturbance due to low-back pain for approximately 5 years before her presentation to our institution. There was no medical history other than a low body weight of 40 kg. She presented with kyphosis after spontaneous union of an L5–6 deformity (Fig. 1), low-back pain and claudication, and difficulty walking independently. The inclusion criteria for this procedure were as follows: 1) preoperative lumbar lordosis (LL) of less than 20°, 2) LL–pelvic incidence (PI) mismatch greater than 30° with a pelvic tilt (PT) greater than 25°, 3) LL-PI mismatch greater than 15° after the first-stage surgery of LLIF, and 4) no history of an ipsilateral retroperitoneal operation such as renal surgery. She had a high LL-PI mismatch (LL 8°, PT 46°, PI 68°, and sagittal vertical axis [SVA] 115 mm) and S1 lumbarization.
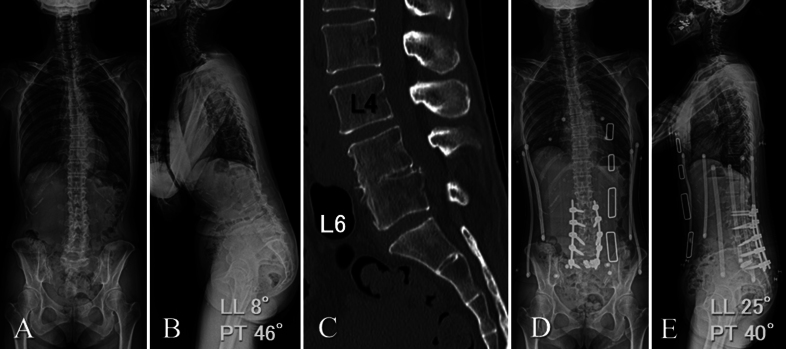
FIG. 1.
A and B:Preoperative whole-spine radiographs show a high LL-PI mismatch (LL 8°, PT 46°, and PI 68°) and S1 lumbarization. C: Preoperative reconstructed sagittal CT image shows fusion of L5–6. D and E:Postoperative whole-spine radiographs 1 week after L2–5 LLIF, L6–S1 PLIF, and temporary PPS fixation as a first surgery, resulting in an LL of 25° and a PT of 40°.
Surgical Technique: Two-Stage Grade 4 Spinal Osteotomy Using LLIF
The first surgery consisted of L2–5 LLIF, L6–S1 PLIF, and temporary PPS fixation, which were performed under fluoroscopic imaging and resulted in an LL of 25° and a PT of 40° (Fig. 1). LLIF, including bone harvesting from the left iliac crest, was done through an approximately 3-cm skin incision for each level, with the patient in the left lateral decubitus position. The dilators and retractors were inserted through the psoas muscle with electromyography monitoring. LLIF cages with 10°–15° lordosis (Coroent XL, NuVasive) filled with autograft fragments and hydroxyapatite were inserted into each level. The L6–S1 PLIF and insertion of PPSs and temporal bent rods were performed under the guidance of C-arm fluoroscopic imaging and electromyography monitoring, with the patient in the prone position. Nerve root monitoring was also performed.13 Two expandable titanium PLIF cages and autograft with hydroxyapatite granules were placed in the anterior part of the intervertebral disc space. Appropriate compressive force was applied between the adjacent PPSs from L3 to S1. During the first surgery, the intraoperative blood loss was 450 ml, and the operation time was 4.5 hours.
The second surgery, 2 weeks later, was performed through an approximately 10-cm midline skin incision and small incisions for the PPSs, with the patient in the prone position. Before the osteotomy, temporary rods were removed and used for collection. The eggshell procedure, which is one of the PSO techniques originally described by Heinig9 and modified by Murrey et al.,10 was performed following an L4 laminectomy, resection of both sets of articular processes, and detachment of the transverse processes. After the removal of bilateral L4 PPSs, the L4 apical pedicles were decancellated, starting from the lateral walls. The medial pedicle walls and posterior walls were preserved. After decancellation up through the resected L3–4 disc space behind the LLIF cage that had already been placed in the first surgery, the preserved walls were removed. Grade 4 osteotomy in the L4 vertebral body at a 30° angle was made by an osteotome and a small drill bar toward the center of the LLIF cage between L3 and L4 under C-arm fluoroscopic lateral imaging guidance (Figs. 2 and 3) and supported by gradually bent temporary rods. PPSs from T10 to the pelvis, ideally bent rods, and two additional collateral rods were inserted using the Reline spinal system (Reline and PRICEPT, NuVasive) after removal of the temporary rods. The extended correction device of the Reline spinal system was reconnected percutaneously at the L2, L6, and S1 levels and openly at the L3 and L5 levels. The T10 to L2 PPSs and S2 alar-iliac screws were inserted percutaneously. During the second surgery, the intraoperative blood loss was 1230 ml and the operation time was 6.5 hours, but because of her low body weight, a salvaged autologous blood transfusion and 4-unit blood transfusion were performed. There were no other intraoperative or perioperative complications. The final spinal alignment maintained LL 55°, PT 29°, and SVA 46 mm, although the LLIF cage slightly subsided (Fig. 2). Two years after her surgery, her back pain and claudication had improved, and she could walk independently without loss of correction or breakage of the insertion metal.
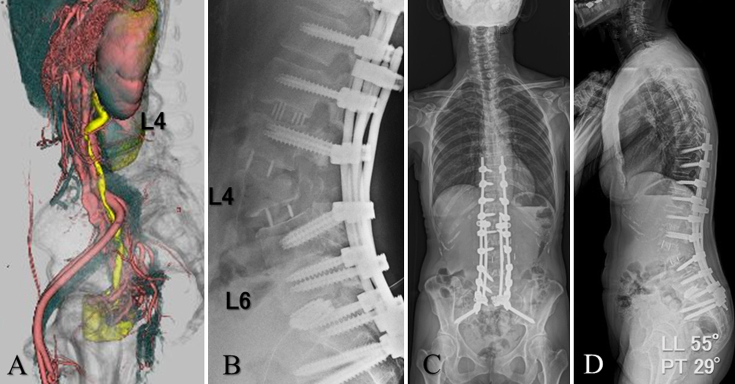
FIG. 2.
A:Preoperative CT reconstruction, followed by three-phase contrast enhancement, indicated that an L5–6 osteotomy was dangerous due to vessels. B:Postoperative lateral radiograph after grade 4 osteotomy in the L4 vertebral body at a 30° angle toward the center of the LLIF cage between L3 and L4 as a second surgery. C and D:Postoperative whole-spine radiographs reveal good sagittal alignment (LL 55° and PT 29°) at the final 2-year follow-up.
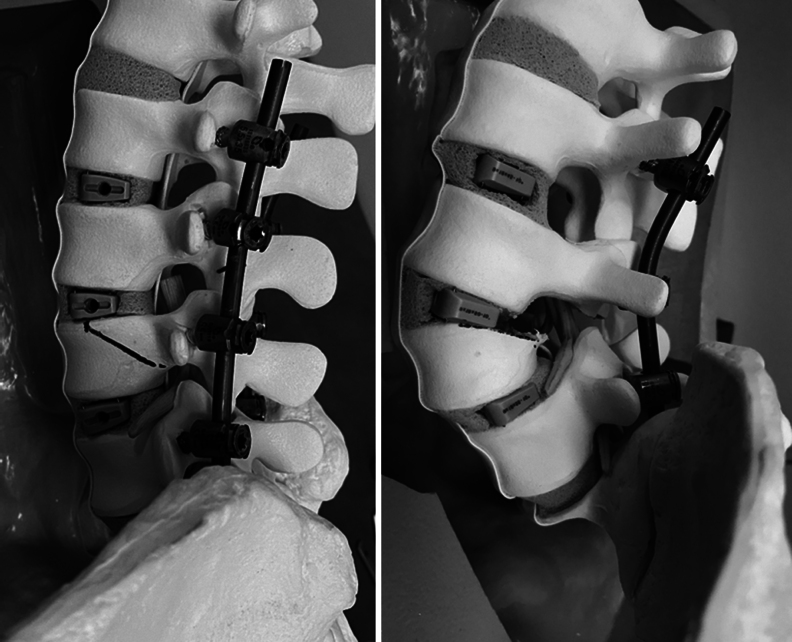
FIG. 3.
Sawbones models of grade 4 osteotomy following LLIF. Grade 4 osteotomy in the L4 vertebral body at a 30° angle was made by an osteotome and a small drill bar toward the center of the LLIF cage between L3 and L4 (left) and supported by gradually bent temporary rods (right). The amount of bone cut is smaller than that typical for grade 4 osteotomy. Stabilization of the anterior longitudinal ligament made the LLIF cage stabilize.
Informed Consent
The necessary informed consent was obtained in this study.
Discussion
Observations
Corrective spinal surgery for ASD is performed cautiously, especially in older patients and in patients with some comorbidities, due to its high invasiveness. LLIF could make it possible to perform anterior release and support less invasively than before. Two-stage spinal reconstructive surgery that combines LLIF with posterior corrective fusion has been performed as a minimally invasive surgical technique for ASD.14–17 Although several previous studies provide some evidence, it is difficult to draw a conclusion regarding the safety of two-stage surgery due to limited patient matching between single-stage and two-stage surgery. However, many advantages encourage us to use two-stage surgery for severe ASD. Yamato et al. reported that two-stage surgery for ASD resulted in significantly better clinical results and degree of spinal correction than posterior-only single-stage surgery.18 Schwab grade 2 osteotomy has already been applied in two-stage spinal reconstructive surgery using LLIF and affected the degree of correction for ASD.19 Splitting a prolonged single-stage procedure reduces the surgeon’s fatigue, improves performance during critical procedures such as spinal osteotomy, and ultimately increases surgical safety.17
On the other hand, 3COs, including grade 3 or 4 osteotomy, pose significantly higher risks of neurological complications and excessive blood loss due to the exposed bone. Yoshida et al. concluded that independent predictors for perioperative complications in ASD surgery were 3CO as well as fusion of ≥ 10 segments, age ≥ 70 years, operation time ≥ 6 hours, and blood loss ≥ 2000 ml.4 In our case, the grade 4 osteotomy itself during the two-stage procedure did not cause excessive bleeding. We speculated that a grade 4 osteotomy made toward the center of the LLIF cage between the upper disc space would harvest less vertebral body, resulting in less bleeding than in a usual grade 4 osteotomy (Fig. 3). In this procedure, the lateral dissection of the vertebral body, especially the segmental artery and vein, was less than usual, and bleeding from the blood vessels was easier to stop under direct vision. Furthermore, since blind osteotomy is not performed in the anterior part of the vertebral body, there is no risk of large blood vessel injury, which is thought to reduce morbidity. In addition, since there is no operation of inserting a large cage from the posterior between the spinal nerve roots, there is less risk of damage to the dura mater and the spinal nerve roots, and we believe that the risk of damage to the endplate and vertebral body during cage insertion could be reduced. Finally, stabilization of the anterior longitudinal ligament could make the LLIF cage stabilize (Figs. 2 and 3).
Lessons
Our case report has some limitations. First, this case has only been followed up for 2 years. We need to continue the follow-up to obtain long-term data. Second, the potential limitations of this procedure should be acknowledged. Although there are pros and cons to the surgical interval of the two-stage surgery, we performed the second surgery 1–2 weeks after the first surgery due to the patient’s general condition and the operating room schedule in our hospital, a period during which the patient was in a brace and out of bed. The lack of spinal stability without posterior spinal fusion can cause cage subsidence between the first and second surgeries, especially in older patients. That is why we used temporary posterior spinal fusion using PPSs and temporary rods. Although the procedure is expected to be complicated when changing from temporary to definitive fixation percutaneously, it is easy and time-saving with the Reline spinal system. Third, anterior column realignment (ACR) is a known less invasive technique that provides similar results to 3COs in treating ASD with sagittal imbalance. In our case, performing L4–5 ACR with a hyperlordotic interbody cage might have avoided the osteotomy and thoracic to pelvic long fixation reported here. However, ACR is still limited in its application in some countries and facilities due to the risk of complications such as vascular injury. Fourth, L6–S1 anterior lumbar interbody fusion (ALIF) with a hyperlordotic interbody cage rather than PLIF can obtain a stronger and larger fixation angle. At our institution, we currently use the OLIF51 procedure (oblique lumbar interbody fusion; Medtronic) with a hyperlordotic cage (Sovereign, Medtronic) or PLIF using PPSs with expandable cages according to the course of the inferior vena cava and the vascular window for lumbosacral fusion. Fifth, because preoperative reconstruction of computed tomography (CT) followed by contrast enhancement indicated that an L5 osteotomy was dangerous due to vessels in our case, we performed the osteotomy at the L4 vertebral body. If the vessels were not in danger, we could perform an osteotomy at L5, where sagittal correction is more effective. Similarly, even if ALIF had been previously performed at L4–5, the same procedure could be performed at L4 if the retroperitoneal adhesions were not severe. Lastly, the number of cases needs to be increased to prove the superiority and lower invasiveness of this procedure over conventional methods.
Two-stage grade 4 osteotomy using LLIF can reduce surgical invasiveness and blood loss, provides good anterior support, and is expected to be a less invasive surgical procedure for spinal reconstruction surgery requiring osteotomy. This osteotomy technique cannot be applied to ALIF cases that have undergone ACR or to fused intervertebral discs but can be applied to OLIF as well as LLIF.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Nakano, Yashima, Kondo, Kawaguchi. Acquisition of data: Nakano, Yashima, Kondo. Analysis and interpretation of data: Nakano, Yashima, Kondo. Drafting the article: Nakano, Yashima, Kondo. Critically revising the article: Nakano, Yashima, Kondo. Reviewed submitted version of manuscript: Nakano, Yashima, Imai, Kondo. Approved the final version of the manuscript on behalf of all authors: Nakano. Statistical analysis: Yashima, Kondo. Administrative/technical/material support: Yashima, Kondo. Study supervision: Yashima, Kondo, Kawaguchi.
Correspondence
Masato Nakano: Takaoka City Hospital, Takaoka City, Toyama, Japan. mnakano-tym@umin.ac.jp.
References
- 1.Bianco K, Norton R, Schwab F, et al. Complications and intercenter variability of three-column osteotomies for spinal deformity surgery: a retrospective review of 423 patients. Neurosurg Focus. 2014;36(5):E18. [DOI] [PubMed] [Google Scholar]
- 2.Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007;32(24):2764-2770. [DOI] [PubMed] [Google Scholar]
- 3.Schwab FJ, Hawkinson N, Lafage V, et al. Risk factors for major perioperative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J. 2012;21(12):2603-2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoshida G, Hasegawa T, Yamato Y, et al. Predicting perioperative complications in adult spinal deformity surgery using a simple sliding scale. Spine. 2018;43(8):562-570. [DOI] [PubMed] [Google Scholar]
- 5.Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2014;74(1):112-120. [DOI] [PubMed] [Google Scholar]
- 6.Boachie-Adjei O, Ferguson JA, Pigeon RG, Peskin MR. Transpedicular lumbar wedge resection osteotomy for fixed sagittal imbalance: surgical technique and early results. Spine (Phila Pa 1976). 2006;31(4):485-492. [DOI] [PubMed] [Google Scholar]
- 7.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976). 2006;31(19 suppl):S171-S178. [DOI] [PubMed] [Google Scholar]
- 8.Chang KW, Cheng CW, Chen HC, Chang KI, Chen TC. Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine (Phila Pa 1976). 2008;33(13):1470-1477. [DOI] [PubMed] [Google Scholar]
- 9.Heinig CA. Eggshell procedure. In: Luque ER, ed. Segmental Spinal Instrumentation. Slack; 1984:221-230. [Google Scholar]
- 10.Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): a retrospective review of 59 patients. Spine (Phila Pa 1976). 2002;27(21):2338-2345. [DOI] [PubMed] [Google Scholar]
- 11.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;Apr(194):142-152. [PubMed] [Google Scholar]
- 12.Pascal-Moussellard H, Klein JR, Schwab FJ, Farcy JP. Simultaneous anterior and posterior approaches to the spine for revision surgery: current indications and techniques. J Spinal Disord. 1999;12(3):206-214. [PubMed] [Google Scholar]
- 13.Futakawa H, Nogami S, Seki S, Kawaguchi Y, Nakano M. Evaluation of triggered electromyogram monitoring during insertion of percutaneous pedicle screws. J Clin Med. 2022;11(5):1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee KY, Lee JH, Kang KC, et al. Minimally invasive multilevel lateral lumbar interbody fusion with posterior column osteotomy compared with pedicle subtraction osteotomy for adult spinal deformity. Spine J. 2020;20(6):925-933. [DOI] [PubMed] [Google Scholar]
- 15.Makino T, Takenaka S, Sakai Y, Yoshikawa H, Kaito T. Factors related to length of hospital stay after two-stage corrective surgery for adult spinal deformity in elderly Japanese. J Orthop Sci. 2021;26(1):123-127. [DOI] [PubMed] [Google Scholar]
- 16.Strom RG, Bae J, Mizutani J, Valone F, Ames CP, Deviren V. Lateral interbody fusion combined with open posterior surgery for adult spinal deformity. J Neurosurg Spine. 2016;25(6):697-705. [DOI] [PubMed] [Google Scholar]
- 17.Yu HH, Asuma MP, Wallace CS, Kelly MP, Kang DG. Should surgery for adult degenerative lumbar deformity be staged? Clin Spine Surg. 2019;32(7):269-271. [DOI] [PubMed] [Google Scholar]
- 18.Yamato Y, Hasegawa T, Yoshida G, et al. Planned two-stage surgery using lateral lumbar interbody fusion and posterior corrective fusion: a retrospective study of perioperative complications. Eur Spine J. 2021;30(8):2368-2376. [DOI] [PubMed] [Google Scholar]
- 19.Nakashima H, Kanemura T, Satake K, et al. Factors affecting postoperative sagittal alignment after lateral lumbar interbody fusion in adult spinal deformity: posterior osteotomy, anterior longitudinal ligament rupture, and endplate injury. Asian Spine J. 2019;13(5):738-745. [DOI] [PMC free article] [PubMed] [Google Scholar]