Abstract
Introduction
Plastic surgery is an essential yet underdeveloped field in many African nations, especially in rural areas. The demand for plastic surgery is increasing, but differences in access to respective services between rural and urban domiciles remain ever existent, despite the exponentiation of trauma, burns, and congenital disorders. According to this review, urban areas have access to better facilities and specialized surgeons, while rural areas frequently lack infrastructure, educated healthcare personnel, and medical resources. This review compares the quality and accessibility of plastic surgery services in African rural and urban settings in order to determine the variables influencing said differences in access.
Methods
This literature review was performed using electronic search databases comprising PubMed/MEDLINE, Google Scholar, and Africa Journals online (AJOL). Regional medical journals were also reviewed using keywords and associated Boolean operators pertaining to “plastic surgery”, “plastic surgery in rural” and plastic surgery in urban” by selecting studies based on their relevance and content quality. Studies focusing on plastic surgery in Africa were included. A total of 37 articles were analyzed to provide insights into the disparities between rural and urban access to plastic surgery services in Africa. Studies not focusing on plastic surgery were excluded.
Results
The review highlighted significant disparities in access to plastic surgery services between Africa’s rural and urban areas. Rural areas usually lack medical resources, specialized surgeons, infrastructure, while urban areas have access to better facilities and specialized surgeons. Urban regions not only hail more training opportunities for surgeons but also foster further specialized facilities, greater training options, access to modern surgical equipment, sterile facilities and advanced instruments, contributing to clinical and surgical excellence alongside patient satisfaction and outcomes. However, there is a scarcity of qualified plastic surgeons in rural regions, including antiquated technology and a dearth of resources and expertise. Besides, socioeconomic variables that hinder said indifference between rural and urban areas, such as poverty, education, money, and cultural attitudes, precipitated limited access to critical surgical intervention in rural populations.
Conclusion
Further research should be done on how plastic surgery services differ in urban and rural areas. Availability of financial expertise and specialists who can provide specialized care in rural settings is recommended. To enhance patient outcomes, the implementation of technological innovation, improved healthcare infrastructure, and effective training initiatives should be implemented in rural Africa. Also, in the field of plastic surgery, emphasizing the use of telemedicine and mobile surgical units may aid universal healthcare for residents in rural domiciles. Significant progress towards ensuring equitable access to high-quality plastic surgery in rural Africa may be achieved through these initiatives.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12893-024-02735-2.
Keywords: Plastic surgery, Rural healthcare, Urban healthcare, Surgical care access
Introduction
In recent years, there has been growing international interest in expanding access to plastic surgery in underdeveloped nations. However, their need for these services in African countries remains largely not met, which contributes to high rates of mortalities and morbidities [1]. Plastic surgery play an important role in addressing different medical needs such as burns, trauma, and congenital disorders which account for 11% of patients who may require plastic surgery intervention. A plastic surgeon is defined as a medical doctor who has completed specialized training in reconstructive and cosmetic surgical procedures to address functional impairments, injuries, or aesthetic concerns [1]. In Tanzania for instance, cases requiring plastic surgery services account for approximate 16% of population in rural hospitals. Burns attribute as the primary cause of high demand in plastic surgery. In Mozambique, burns account for 19.1% of cases in the emergency departments [2] these highlight the critical need for plastic surgical services to manage complications such as reduction of iatrogenic scar formation, osteomyelitis, and to repair cleft lip and palate.
Despite the rising demand globally, the field of plastic surgery remains underdeveloped in many African regions, such as Nigeria. In Nigeria, mass media is playing a vital role by highlighting both positive and negative impacts of plastic surgery. In terms of its negative impacts, media has played a role in reporting the death of celebrities due to cosmetic procedures [3, 4]. Moreover, due to the shortage of trained plastic surgeons practicing in Nigeria, non-healthcare professionals tend to intervene when a case is deemed of a plastic surgery nature, leading to poor clinical outcomes [1]. In Nigeria, only one plastic surgeon was available for 1.5 million persons, illustrating the urgent the factors that are actively discouraging surgeons to specialize in plastic surgery. Further, a study demonstrated that Nigeria does not have an association that regulates the practice of plastic surgeons like that of developed countries, an observed deficiency in plastic surgeons exposed due to a lack of training and financial capacity [5]. Grimes et al. (2011) found that the highest number of surgeries pertaining to plastic intervention were performed in urban settings rather than in rural districts, whereby disparities between central and district hospitals in the number of operations performed was exhibited. The lack of regulatory bodies for plastic surgery, insufficient training opportunities, and limited financial resources further exacerbate the shortage of qualified surgeons in Nigeria and across sub-Saharan Africa (SSA).
This review seeks to compare the availability and quality of plastic surgery services between rural and urban areas in Africa to identify the factors contributing to such disparities in access and to offer insights into practical solutions that can bridge the gap in access, including policy recommendations, the potential role telemedicine play and the need for targeted training. It explores the unique challenges faced in rural regions such as lack of medical equipment, insufficient sterilization and infection control, and medical staff shortages which may result in subpar patient care [1]. by examining the current landscape of plastic surgery in Africa.
By defining the purpose and scope of this review, we hope to establish a structured narrative that guides the reader through various subtopics, from the specific barriers in rural healthcare systems to innovative strategies that could increase access to quality plastic surgery services across all regions of Africa. Although this review paper primarily focuses on original research, we believe that this review provides a valuable foundation for future studies and initiatives aimed at improving surgical care access in under-resourced areas.
Methods
This literature review was performed using electronic search databases comprising PubMed/MEDLINE, Google Scholar, and Africa Journals online (AJOL). We also reviewed regional medical journals using keywords and associated Boolean operators pertaining to “plastic surgery”, “plastic surgery in rural” and plastic surgery in urban” by selecting studies based on their relevance and content quality. A total of 37 articles were analyzed to provide insights into the disparities between rural and urban access to plastic surgery services in Africa.
Inclusion criteria
Studies were selected based on their focus on plastic surgery in rural and urban Africa regions. Selection was based on studies that provide detailed information on factors affecting access to specialist plastic surgery. Only papers written in English were included to maintain reliability.
Exclusion criteria
Studies that did not specifically address plastic surgery or focused on unrelated medical fields were excluded from this review. Articles that lacked sufficient detail on plastic surgery services in African settings, or that were deemed irrelevant to our focus on rural and urban disparities, were also omitted.
Results
Availability and current state of plastic surgery services in Africa
According to a study by Guzman et al. (2018), inpatient beds in the plastic surgery department of Hospital Central de Maputo (HCM) were not curtained off, and there was a lack of appropriate ventilation equipment, a lack of medical surgical instrumentation, a lack of antibiotics, analgesia, and nutritional supplements, as well as a limited protocol in infection control and hygiene. Additionally, the study depicted that there was no available sedation in the operating room, where sutures for small wounds were performed without sedation in some instances. In 2018, HCM only possessed three plastic surgeons whereas in Mozambique, there were six resident plastic surgeons. Of these, four were working in the capital and the others in the central and north regions of the country [1].
In SSA, many countries exhibit a shortage of plastic surgeons. Less than one plastic surgeon is accounted for every 100,000 individuals. For instance, in Zambia, with a population of approximately 19 million as of 2024, there is only one resident plastic surgeon, highlighting the critical shortage of specialized care in the region. Uganda with a population of approximately 46 million, has three plastic surgeons, and Nigeria, with over 223 million people, has seventy-two. Lack of training, location, finances, and local preferences might all be contributing factors to the shortage of medical personnel. Furthermore, it may be the result of inadequate medical attention and a shortage of reconstructive surgical subspecialties [2]. According to Truche et al. (2021), while five plastic surgeons were identified as practicing full-time in rural regions, many of the 36 surgeons participated in the study also reported providing periodic visiting services to these areas, therefore, this underscores the reliance on itinerant surgical care to address rural needs [6]. According to Semer et al. (2010), the unequal distribution of surgeons nationally is one of the great issues facing African domiciles. Although, rural areas warrant much more plastic surgical interventions than urban areas, most of which prefer to practice in urban rather than rural areas. Cosmetic surgery has been observed to be more accepted in urban than in rural areas, especially among the upper social classes. This may be attributed to a dearth of community awareness, religion beliefs, social taboos, financial deprivation, and absence of a cosmetic surgical society that may enhance one’s perception circumventing cosmetic surgeries [7].
Albutt et al. (2019) stated the many common challenges faced by private and not-for-profit organizations. These comprise the shortage of healthcare professionals, limited transportation, and hospital capacity, medical expenditure, and lack of cooperation between different medical specialties (see Table 1). In many cases, between private and public sectors, the private counterpart employs a higher number of healthcare workers, are generally smaller, and better equipped than public sectors [8]. For example, in Kenya, public and private health sectors are well developed. Howeve, patients are pursuing cosmetic surgeries abroad. The reason behind that may be a lack of specialists and poor marketing pertaining to esthetical procedures performed in Kenya [9].
Table 1.
Geographic distribution of plastic surgery facilities in Africa (Rural vs Urban), focusing on the availability of plastic surgery services
| Availability of plastic surgery services | ||||
|---|---|---|---|---|
| Region | Urban areas | Rural areas | Service availability gap | References |
| North Africa | High availability in major cities like Cairo, Tunis | Very low, limited to regional clinics, often none in remote areas | Large gap due to lack of infrastructure and specialists. < 1 specialist per 100,000 population in rural regions | [10] |
| West Africa | Moderate to high in cities like Lagos, Accra, Dakar | Low, with only basic surgical services, plastic surgery rarely available | Significant gap, especially in rural Nigeria (1 surgeon per 1.5 million people), and Ghana (severely limited rural access) | [11–14] |
| East Africa | High in Nairobi, with specialized centers | Minimal to non-existent, especially in rural Kenya | Major gap due to lack of facilities and resources. Rural regions often rely on periodic visiting surgeons | [14, 15] |
| Southern Africa | High availability in Johannesburg, cape town | Very low, mostly absent in remote rural regions | Substantial gap due to geographic isolation. In South Africa, 72 surgeons serve a population of 223 million, most in cities | [16] |
| Central Africa | Low to moderate in capitals like Kinshasa | Extremely low, often no facilities in rural or forested areas | Severe gap, with less than one surgeon per 100,000 population across most rural areas due to limited infrastructure | [8, 17] |
Quality of plastic surgery services and comparison with urban access
Despite similar qualifications, there exists a huge disparity in training and expertise between rural and urban plastic surgeons in Africa (see Fig. 1) [18]. Patients in urban Africa are more likely to have access to better skilled plastic surgeons who are capable of performing complex procedures because highly trained surgeons tend to gravitate towards urban areas where there is access to professional development opportunities and funding for sub-specialty programs are more robust (see Fig. 1) [18, 19]. Conversely, although while burn injuries, trauma, and other conditions requiring plastic surgeons are common in rural Africa, the quality of plastic surgical interventions performed there is negatively impacted by a lack of specialist training or, in some circumstances, by the complete lack of plastic surgeons [1, 17].
Fig. 1.
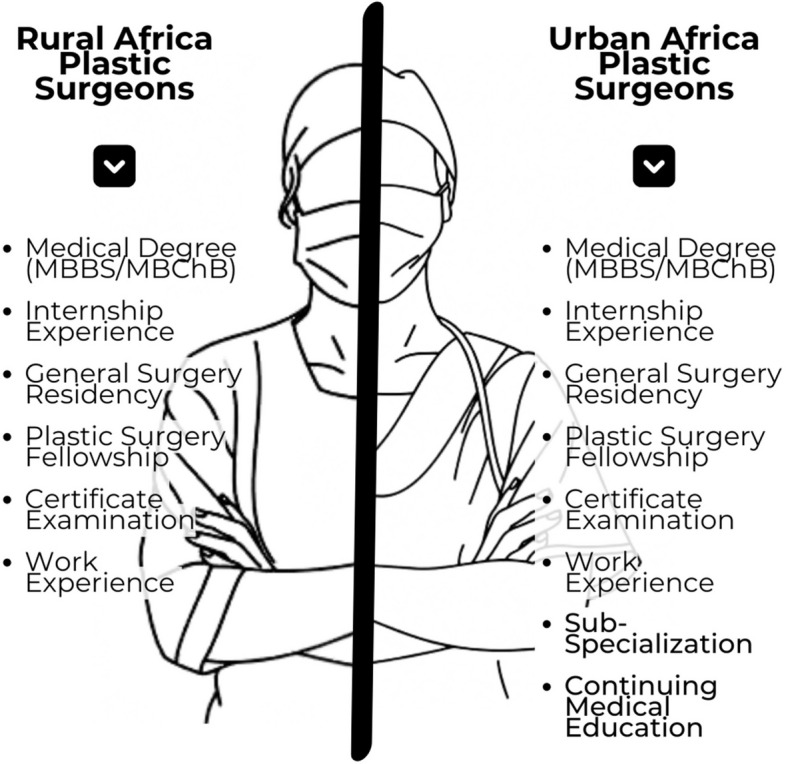
Training levels of plastic surgeons in rural vs. Urban settings
Another significant determinant of quality plastic surgery services in Africa is the availability of infrastructure and modern equipment. Generally, urban hospitals are equipped with better operating rooms, imaging devices as well as sterilization units, which are all enhanced factors towards improvement of quality in plastic surgeries they provide [1, 20]. Surgeons at the urban hospitals benefit from access to the latest technology including specialized tools such as laser devices, endoscopy instruments, and microsurgery kits which allows them to perform intricate plastic surgery procedures (see Table 2). These include neural or blood vessel reconstruction with greater accuracy and minimal risk of complications [21].
Table 2.
Comparison of infrastructure and equipment in rural vs. Urban plastic surgery centers
| Urban Plastic Surgery Centers | Rural Plastic Surgery Centers | |
|---|---|---|
| Operating Rooms | Equipped with state-of-the-art tools | Equipped with basic tools |
| Imaging Devices | High-resolution imaging | Outdated imaging devices |
| Sterilisation Units | Fully operational | Often outdated or inadequate |
| Specialized Tools | Microsurgery kits, laser devices, etc. | Unavailable |
| Emergency Facilities | Well-established and functional | Patient often require to be transferred |
In contrast, hospitals in rural Africa are typically underfunded and may need outdated equipment or techniques to carry out their plastic surgery procedures often sacrificing quality care in the process (see Table 2) [19]. This forces patients to make do with whatever alternative option is available or be transported over a long distance to get the required treatment [1].
It is also important to recognize patient satisfaction as a key metric to validate quality of service. Patients for plastic surgery in urban Africa hospitals generally show better satisfaction as the post-operative care systems allow for better monitoring which ensures faster recovery time while rural Africa hospitals on the other hand, often lack the resources to do the same, giving more room for post-surgery complications and negatively impacting patient satisfaction [1]. Furthermore, patients are more likely to be given more comprehensive detail about their procedures, potential risks and expected outcomes in urban hospitals relative to rural hospitals, which is very important in managing patient expectations and satisfaction as well [22].
Factors contributing to disparities between urban and arural areas
Low-income-countries such as those in Southern Africa face a serious challenge due to the disparities in access to healthcare between rural and urban areas (see Fig. 2). The root causes and the factors contributing to this challenge are many and may be documented in various healthcare fields [23]. Plastic surgery is one of these fields that is marked by significant imbalance in services between rural and urban areas and driven by socioeconomic and cultural factors as well as policy and healthcare system challenges. Based on a study published in July 2022 to assess plastic and reconstructive surgery in Malawi, socioeconomic factors such as education, costs, and accessibility highly affect the availability of plastic surgery services [24]. For example, patients heading to hospitals from rural areas to receive plastic surgery service such as for congenital anomalies and burns have to face the challenges of high transportation costs and unserviceable roads (see Fig. 2) [24].
Fig. 2.
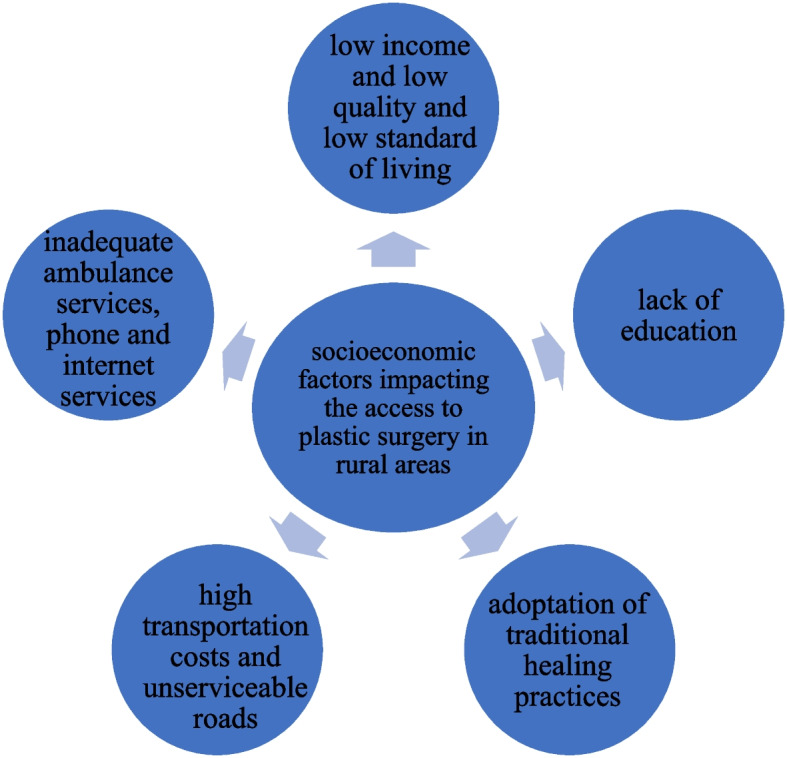
Socioeconomic factors influencing access to plastic surgery in rural African areas
Additionally, a lack of education and medical literacy is considered to be a barrier for receiving plastic surgeries and related care where for example traditional first aid practices will be done for burns or traditional healer practitioners are reached to manage some cases (see Fig. 2). These practices are mainly seen in rural areas thus the authors have suggested increasing public awareness and outreach in these areas [24]. Rural areas also suffer from inadequate ambulance services, phone and internet services mainly due to the low incomes and low standards of living [25]. On the other hand, residents of the urban areas where specialized care centers are present are less likely to face challenges related to incomes and costs of travel [26]. Moreover, individuals living in urban areas have better education and opportunities of obtaining health information resources in comparison to those living in remote rural areas [27]. This increases the disparities in access to plastic surgery between rural and urban areas of Africa.
In addition, policies and healthcare system challenges can contribute to such disparities. Rural settings in South Africa suffer from lack of proper medical equipment and resources which affects both patients’ treatments and training of healthcare professionals. Besides, shortage of staff including specialists is another factor that affects the quality of health care services (see Table 3) [25]. All these factors are influencing access to plastic surgery services. To add to this, in a study done by Truche et al. (2021), most of the identified plastic surgeons that responded to the survey were working in urban areas in comparison to rural areas in low-income-countries including the African Region [6]. This reflects the fact that medical professionals are highly concentrated in urban areas which leads to a discrepancy in access to plastic surgery between rural and urban areas (see Table 3). In terms of governmental policies, there is indeed a lack of appropriate policies to reinforce rural health services such as lack of training and medical insurance coverage in addition to inadequate infrastructure including electricity and water services [25].
Table 3.
Key policy and systemic challenges affecting plastic surgery services in rural and urban African areas. Source: Created by Rawan Noureddine based on Ngene et al., 2023
| Challenge | Rural Areas | Urban Areas |
|---|---|---|
| Lack of resources | Limited availability of proper medical material and surgical equipment | Better access to technologies and materials |
| Shortage in professionals | Shortage of trained surgeons and nurses | Areas of concentration of healthcare professionals and specialists |
| Lack of medical insurance coverage | Most are poor with low-income class and no insurance | Better insurance plans |
| Lack of infrastructure | Lack of electricity and water services, lack of ambulances and poor communications | Better services and faster access to clinics |
Cultural issues are also a factor that play a role in healthcare inequality [25]. In the rural region, due to cultural norms and to the lack of education would affect the uptake of orthodox health services and as a results patients can refer to traditional healers or domestic first aid practices to treat burns for example or any case that requires a plastic surgery. All these factors can explain the discrepancy in access and availability of plastic surgery between rural and urban areas of Africa (See Fig. 2).
Pontential innovative solutions and recommendations
To improve surgical care, developing training programs for healthcare workers, reducing patient medical costs, reinforcing travel amenities to facilitate transportation to regional hospitals, and installing community awareness are all warranted. Better working circumstances for affected personnel, training opportunities, and suitable hospital facilities meant that plastic interventions were being carried out by qualified healthcare professionals in the metropolitan homes of sub-Saharan Africa (SSA). In many cases, non-physicians with less training experience perform similar procedures in remote hospitals that lack diagnostic technology, surgical surplus, and suitable accommodation. Furthermore, non-professionals in rural locations are sometimes faced with delayed renovations, which frustrates and depresses them [26]. According to a study by Banda et al. (2019), there was insufficient care provided both peri- and post-operatively. This lack of healthcare personnel, surgical equipment, and patient monitoring is causing emerging nations to face a dismal outlook. It is advised that medical professionals and surgeons receive the appropriate training to enhance perioperative care. Healthcare practitioners should also be aware that plastic surgeons may perform certain surgeries locally with the assistance of other medical specialties, such as extremity replantation [28].
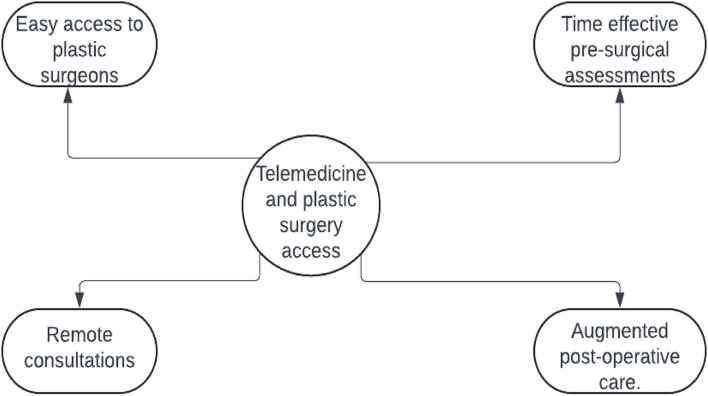
Telemedicine is a service that has been pivotal in fostering the abilities of healthcare providers to effectively take care of people without being where the patient is stationed at (see Fig. 3). It is defined as a whole collection of deliverables depicted to enable patients and their physicians via utilization of telecommunicating and electronic information technologies [29]. Telemedicine includes a broad range of applications both within and across medical specialties from a simple telephone to robots that can be conducted by surgeons many miles away from the operating rooms (see Fig. 3) [30]. During the novel coronavirus disease 2019 (COVID–19) pandemic telemedicine proved to be a reliable health-related service and its utilization was also adopted in the plastic surgery field in activities such as new patient consultations, pre-operative planning and post-operative follow-up [31]. Various disparities in access to health care between patients from urban and rural have been well documented, and the rising of telemedicine into the play has enabled the reduction of such disparities as patients from both urban and rural areas can have access to a diverse group of medical and surgical specialists [32].
Fig. 3.
A figure illustrating how telemedicine can enhance access to plastic surgery
An approximate population of 25 million persons in the United States do not have access to a plastic surgeon which results in sub-optimal care for the patients [33]. As an intervention to enhance the access to plastic surgery in urban areas, the implementation of mobile plastic surgery units has proven to be beneficial. Mobile plastic surgery units same as the mobile health clinic can be defined as a custom-built motor vehicle that travels to different communities providing healthcare services for instance plastic surgery services in this case [34]. There are various stories that depict the success in the use of mobile units to improve access to surgical care in rural areas, for instance the study that was done in Central India reports that over 4,317 patients with cleft lip/palate and post-burn contractures were well treated as an initiative of 60 mobile plastic surgery camps that took place in that region showcasing the role of mobile plastic surgery units [35].
Many surgeons reside in the urban healthy areas and this creates a gap in access to surgical care that in turn brings about maldistribution. To tackle this issue of inequity in access to surgical care, there is need for training local surgeons and involvement of well-trained plastic and reconstructive surgeons in rural areas. Various initiatives promoting the education of local medical professionals equips them with necessary skills, outreach programs for trained plastic surgeons enhance the sharing of knowledge and skill development, and fellowship programs foster enhanced training and expertise in rural areas, thus reducing the surgical disease burden [36]. Advancement of technology worldwide also stands as a pivotal strategy that can be used to enhance and promote trainings and expertise skills sharing through utilization of virtual training programs that would act as a link connecting plastic surgery experts from high income countries to trainees in low-income countries which can be regarded as underprivileged regions in the aspect of plastic surgery These virtual training programs can utilize technologies like virtual and augmented reality since these technologies have proven to be superior to in-person trainings for both clinical skill acquisition and patient specific health outcomes [37].
Discussion
This review has highlighted the disparities in access to plastic surgery services between rural and urban areas in Africa, underscoring the broader challenges faced in providing healthcare to underserved regions. The access to the plastic surgery services in rural Africa is limited by a range of socioeconomic and cultural factors, including inadequate education, professional shortages, lower income levels, insufficient funding, and a lack of essential infrastructure and medical equipment. Establishing well-equipped surgical centers is crucial, but these initiatives must coincide with and come after primary healthcare infrastructure expenditures, which serve as the cornerstone for long-term gains in specialized medical services.
Addressing these multifaceted challenges requires a deliberate, multi-pronged approach to ensure equitable access to care. One of the strategies that could help retain plastic surgeons in rural areas is providing economic and career incentives. Providing financial incentives such as rural hardship allowances and housing subsidies could make rural practice more attractive. In addition to that, providing opportunities such as continuing education and professional advancement, would play an important role in retaining talent in rural areas. Urban surgeons usually create subspecialties because of their greater access to cutting-edge technology, a more varied patient base, and more chances for professional advancement, even if board-certified plastic surgeons in rural and urban locations have comparable credentials.
Rural surgeons must be prepared to handle a range of healthcare requirements by receiving both generalist and specialized training in order to address this imbalance. Providing funding for healthcare infrastructure in rural areas is essential. This could be done by establishing well-equipped surgical centers with adequate medical supplies, reliable power sources as well as improved transportation would support a sustainable healthcare environment that facilitates providing plastic surgery services in African rural areas. Other strategies that can help in having plastic surgery services in rural areas as it is in urban areas is task-sharing and training for general surgeons. By providing training on basic plastic surgery techniques, this could help to meet urgent needs in rural areas and enable general surgeons to perform necessary plastic surgeries, where specialist services are not available. Such task-sharing initiatives should be supported with robust oversight and mentorship to maintain high standards of care. furthermore, since telemedicine and mobile surgical units can facilitate the work in this field, it is essential to develop it more in the needed areas to improve the patient’s outcomes. Telemedicine can facilitate pre- and post-operative consultations, enhance diagnostic accuracy, and provide real-time support for rural practitioners. Also, a collaboration among plastic surgeons in urban and rural regions to ensure a better understanding of the complex procedures.in addition to that, involving partnerships with international training bodies, including the development of an African Plastic Surgery College could facilitate training, mentorship, and resources for surgeons practicing in rural settings, hence, facilitate establishment of an African Plastic Surgery College. This initiative could also foster research and innovation tailored to the unique challenges faced in low-resource settings, ensuring that solutions are context-specific and sustainable.
Limitations of the review
While this review provides valuable insights; it is limited by several factors. First there is limited or incomplete data between urban and rural areas, which can limit the comparison of the availability of plastic surgery services among the regions. The studies included in our review can differ in the quality, where some studies might be of high quality, while others of low quality with a small sample size or outdated data. Also, our review might have excluded some regions due to the geographic variation, with a possibility of bias since each country in the African region might have a distinguished healthcare system and plastic surgery terms’ implementations among the urban and rural areas, which can constraint the comparison between the two. Moreover, since the plastic surgery field can cover many aspects, such as reconstruction or cosmetics, it might have been a bit hard to specify the covered aspect in each comparison between urban and rural areas in our review. Future research should focus on narrowing these gaps by incorporating more robust data collection methods, region-specific analyses, and an emphasis on actionable solutions tailored to different African contexts.
Conclusion
In conclusion, it is highly recommended to accomplish more studies to focus on the disparity of plastic surgery services between urban and rural areas. The access to specialized care such as professionals and fundings should be achieved in rural regions. A better infrastructure, a more advanced technology, and good training programs should be implemented in the rural African regions to improve the patient care. Moreover, a focus on the telemedicine and mobiles surgical units in the plastic surgery field can facilitate the patient’s access to all the necessary services. By prioritizing these efforts, significant strides can be made toward equitable access to quality plastic surgery services across Africa.
Supplementary Information
Acknowledgements
We would like to thank Oli Health Magazine Organization (OHMO)’s members for their contributions and support for this manuscript.
Financial support
None.
Clinical trial number
Not applicable.
Abbreviations
- HCM
Hospital Central de Maputo (HCM)
- AJOL
Africa Journals online (AJOL)
- MBBS
Bachelor of Medicine, Bachelor of Surgery degree
- MBChB
Bachelor of Medicine, Bachelor of Surgery degree
- COVID-19
Coronavirus diseases of 2019
Authors’ contributions
O.U: Conceptualization, Project administration, Writing-review and Designing Data collection and Assembly: N.M, O.U, R.N, B.S.F, C. B, L.F, L.G, V.M, J.W N.M: Reviewed and edited the first draft Manuscript writing: N.M, O.U, R.N, B.S.F, C. B, L.F, L.G, V.M, J.W O.U: Reviewed and edited the second draft O.U: Reviewed and edited the final draft Final approval of manuscript: All authors Table 1. was drawn and analyzed by N.M Table 2. was drawn and analyzed by B.S.F Table 3. was drawn and analyzed by R.N Fig. 1. was drawn analyzed by B.S.F Fig. 2. was drawn and analyzed by R.N Fig. 3. was drawn and analyzed by C.B
Funding
We have not received any financial support for this manuscript.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
All co-authors approved the final manuscript.
All co-authors have read and approved the submission.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guzman KJ, Gemo N, Martins DB, Santos P, DeUgarte DA, Ademo F, et al. Current Challenges of Plastic Surgical Care in Sub-Saharan Africa (Maputo, Mozambique). Plast Reconstr Surg Glob Open. 2018;6(8): e1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ibrahim A. Sub-specialization in plastic surgery in sub-Saharan Africa: capacities, gaps and opportunities. Pan Afr Med J. 2014;19:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chukwuanuku TOG. Plastic Surgery in Nigeria-Scope and Challenges. Nigerian Journal of Surgery. 2011;17(2):68–72. Available from: https://www.ajol.info/index.php/njs/article/view/73053. Cited 2024 Sep 18
- 4.Salawu A, Gbadamosi K, Ipinnimo T, Babalola O, Okunlola A, Emmanuel E, et al. Knowledge, Determinants of Attitude and Willingness for Cosmetic Surgery among Online Media Users in Nigeria. 2022. https://www.researchgate.net/publication/360449933_Knowledge_Determinants_of_Attitude_and_Willingness_for_Cosmetic_Surgery_among_Online_Media_Users_in_Nigeria.
- 5.(14) (PDF) Attitude and Practice of Aesthetic Surgery among Plastic Surgeons in Nigeria. Available from: https://www.researchgate.net/publication/344874744_Attitude_and_Practice_of_Aesthetic_Surgery_among_Plastic_Surgeons_in_Nigeria. Cited 2024 Sep 18
- 6.Truche P, Moeller E, Wurdeman T, Zimmerman K, Cruz N, Nakarmi K, et al. The Plastic Surgery Workforce and Its Role in Low-income Countries. Plast Reconstr Surg Glob Open. 2021;9(4):e3428. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8078243/. Cited 2024 Sep 18 [DOI] [PMC free article] [PubMed]
- 7.Semer NB, Sullivan SR, Meara JG. Plastic surgery and global health: how plastic surgery impacts the global burden of surgical disease. J Plast Reconstr Aesthet Surg. 2010;63(8):1244–8. [DOI] [PubMed] [Google Scholar]
- 8.Albutt K, Drevin G, Yorlets RR, Svensson E, Namanya DB, Shrime MG, et al. ‘We are all serving the same Ugandans’: A nationwide mixed-methods evaluation of private sector surgical capacity in Uganda. PLoS One. 2019;14(10):e0224215. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6812829/. Cited 2024 Sep 18 [DOI] [PMC free article] [PubMed]
- 9.Masitara ES. Assessing the Practice of Aesthetic Surgery in Kenya [Thesis]. University of Nairobi; 2022. Available from: http://erepository.uonbi.ac.ke/handle/11295/161431. Cited 2024 Sep 18
- 10.Understanding barriers to health care for minorities and indigenous peoples in Egypt, Iraq and Tunisia - Egypt | ReliefWeb. Available from: https://reliefweb.int/report/egypt/understanding-barriers-health-care-minorities-and-indigenous-peoples-egypt-iraq-and-tunisia. Cited 2024 Sep 19
- 11.Goodacre T. Plastic surgery in a rural African hospital: Spectrum and implications. Ann R Coll Surg Engl. 1986;68:42–4. [PMC free article] [PubMed] [Google Scholar]
- 12.Agbenorku P, Agbenorku M, Boakye-Yiadom E, Iddi A, Abude F, Sefenu R, et al. Multicenter plastic surgery outreach services for underserved Ghanaian communities. Eur J Plast Surg. 2010;34:111–8. [Google Scholar]
- 13.Nigerian Journal of Plastic Surgery. Available from: https://njpsurg.org/index.php/njps. Cited 2024 Sep 19
- 14.Knowledge and perception of plastic surgery among tertiary education students in Enugu, South-East Nigeria - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/27022793/. Cited 2024 Sep 19 [DOI] [PubMed]
- 15.Nthumba PM, Odhiambo M, Pusic A, Kamau S, Rohde C, Onyango O, et al. The State of Surgical Research in Sub-Saharan Africa: An Urgent Call for Surgical Research Trainers. Plastic and Reconstructive Surgery – Global Open. 2024;12(6):e5903. Available from: https://journals.lww.com/prsgo/fulltext/2024/06000/the_state_of_surgical_research_in_sub_saharan.45.aspx. Cited 2024 Sep 19 [DOI] [PMC free article] [PubMed]
- 16.Rogers AD, dos Passos G, Hudson DA. The scope of plastic surgery. South African Journal of Surgery. 2013;51(3):106–9. Available from: http://www.scielo.org.za/scielo.php?script=sci_abstract&pid=S0038-23612013000300007&lng=en&nrm=iso&tlng=en. Cited 2024 Sep 19 [DOI] [PubMed]
- 17.Essential surgery delivery in the Northern Kivu Province of the Democratic Republic of the Congo | BMC Surgery | Full Text. Available from: https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-024-02386-3. Cited 2024 Oct 30 [DOI] [PMC free article] [PubMed]
- 18.As A, Bhuiyan MdU. Challenges and opportunities in training surgeons in rural areas. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2022 Nov 1;112:886–7.
- 19.A OA, C ND, C OS, O BB, J UT, O NC, et al. Aesthetic Surgery & the Indications at A Sub-Urban Tertiary Hospital in Edo State, Nigeria. Journal of Advances in Medical and Pharmaceutical Sciences. 2024;26(5):37–41. Available from: https://journaljamps.com/index.php/JAMPS/article/view/684. Cited 2024 Sep 19
- 20.Msokera C, Xepoleas M, Collier ZJ, Naidu P, Magee WA. plastic and reconstructive surgery landscape assessment of Malawi: a scoping review of Malawian literature. Eur J Med Res. 2022;27(1):119. 10.1186/s40001-022-00714-y. Cited 2024 Sep 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kania K, Chang DK, Abu-Ghname A, Reece EM, Chu CK, Maricevich M, et al. Microsurgery Training in Plastic Surgery. Plast Reconstr Surg Glob Open. 2020;8(7):e2898. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7413759/. Cited 2024 Sep 19 [DOI] [PMC free article] [PubMed]
- 22.Chen X, Orom H, Hay JL, Waters EA, Schofield E, Li Y, et al. Differences in rural and urban health information access and use. J Rural Health. 2019;35(3):405–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oloyede O. Rural-Urban Disparities in Health and Health Care in Africa: Cultural Competence, Lay-beliefs in Narratives of Diabetes among the Rural Poor in the Eastern Cape Province of South Africa. African Sociological Review / Revue Africaine de Sociologie. 2017;21(2):36–57. Available from: https://www.ajol.info/index.php/asr/article/view/167160. Cited 2024 Sep 19
- 24.Meyerson J, Shields T, Liechty A, O’Brien A. Creating a Rural Plastic Surgery Practice: Social and Financial Impacts. Plast Reconstr Surg Glob Open. 2022;10(5):e4293. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9061147/. Cited 2024 Sep 19 [DOI] [PMC free article] [PubMed]
- 25.Ngene NC, Khaliq OP, Moodley J. Inequality in health care services in urban and rural settings in South Africa. African Journal of Reproductive Health. 2023;27(5s). Available from: https://www.ajrh.info/index.php/ajrh/article/view/3834. Cited 2024 Sep 19 [DOI] [PubMed]
- 26.Grimes CE, Law RSL, Borgstein ES, Mkandawire NC, Lavy CBD. Systematic review of met and unmet need of surgical disease in rural sub-Saharan Africa. World J Surg. 2012;36(1):8–23. [DOI] [PubMed] [Google Scholar]
- 27.Atulomah NO. Information Need, Health Literacy, and Preventive-Health Behaviour among Individuals in a Rural Community of Ikenne Local Government Area, Nigeria. TIJPH. 2020;8(1):33–40. Available from: https://www.texilajournal.com/public-health/article/1581-information-need-health. Cited 2024 Sep 19
- 28.Banda CH, Georgios P, Narushima M, Ishiura R, Fujita M, Goran J. Challenges in global reconstructive microsurgery: The sub-Saharan african surgeons’ perspective. JPRAS Open. 2019;20:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021;2:100117. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8590973/. Cited 2024 Mar 19 [DOI] [PMC free article] [PubMed]
- 30.Gardiner S, Hartzell TL. Telemedicine and plastic surgery: a review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg. 2012;65(3):e47-53. [DOI] [PubMed] [Google Scholar]
- 31.Alba B, Arnold SH, Siotos C, Hansdorfer M, Aminzada A, Dorafshar A, et al. The utility of telemedicine in plastic and reconstructive surgery: provider and patient perspectives. Eplasty. 2023;23:e35. [PMC free article] [PubMed] [Google Scholar]
- 32.Douglas S, Geiger E, McGregor A, Norwich A, Abbate D, Hsia H, et al. Telehealth in Plastic Surgery: A Veterans Affairs Hospital Perspective. Plast Reconstr Surg Glob Open. 2018;6(10):e1840. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6250470/. Cited 2024 Sep 19 [DOI] [PMC free article] [PubMed]
- 33.Meaike JD, Cantwell S, Mills A, Singh K, Moran SL. Is rural plastic surgery feasible and important?: A survey and review of the literature. Ann Plast Surg. 2020;84(6):626–31. [DOI] [PubMed] [Google Scholar]
- 34.Malone NC, Williams MM, Smith Fawzi MC, Bennet J, Hill C, Katz JN, et al. Mobile health clinics in the United States. Int J Equity Health. 2020;19(1):40. 10.1186/s12939-020-1135-7. Cited 2024 Sep 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Plastic Surgery in Camps in Rural India. Available from: http://ouci.dntb.gov.ua/en/works/4YO6v0M9/. Cited 2024 Sep 19
- 36.International Humanitarian Work: A Mindset for Success in Plastic Surgery Training - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/30855363/. Cited 2024 Sep 19 [DOI] [PubMed]
- 37.Ullrich PJ, Ramsey MD. Global plastic surgery: a review of the field and a call for virtual training in low- and middle-income countries. Plast Surg (Oakv). 2023;31(2):118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.