The National Health Service is facing a shortfall of over a quarter of a million staff by 2036/37 as healthcare demand grows.1 To address this, the UK Government and the NHS have pledged to increase recruitment and also retain 130,000 staff by 2039.1 Retention is vital to address current staff shortages, avoid increasing pressure on remaining staff, and ensure sufficient capacity to train new staff. Up-to-date information is urgently needed to identify factors associated with leaving healthcare and implement effective retention policies.
We analysed questionnaire data collected as part of the UK-REACH (United Kingdom Research study into Ethnicity and COVID-19 outcomes in Healthcare workers) study from UK healthcare workers (HCWs) in 2023–2024 to identify factors associated with intentions and actions to leave the healthcare workforce (‘attrition intentions’). This cross-sectional analysis forms part of the I-CARE study (funded by NIHR Health and Social Care Delivery Program–NIHR157268; see appendix).
A primary binary outcome measure was: considered or acted upon taking early retirement or leaving healthcare role vs not, derived from the item “Has the COVID-19 pandemic made you consider or act upon any of the following in relation to your work?”. A secondary outcome included, within the outcome, those who had considered reducing their hours, changing their field or reducing clinical duties.
Exposures were: age, sex and occupation; ethnicity and migration status; meeting screening criteria for depression, anxiety, Post-Traumatic Stress Disorder (PTSD); burnout; work engagement [one item each from absorption, vigour and dedication domains]. We build on our previous work2 which identified feeling valued and discrimination represented important and modifiable risk factors for attrition, so analysed feeling valued by the Government, employer, and general public, and experience of discrimination from patients, colleagues, or both. We included only participants with complete data on these items. See appendix for details of questionnaire items/variable construction and sample.
We used multivariable logistic regression to determine associations of exposures with outcomes, and adjusted estimates for age, sex and occupation.
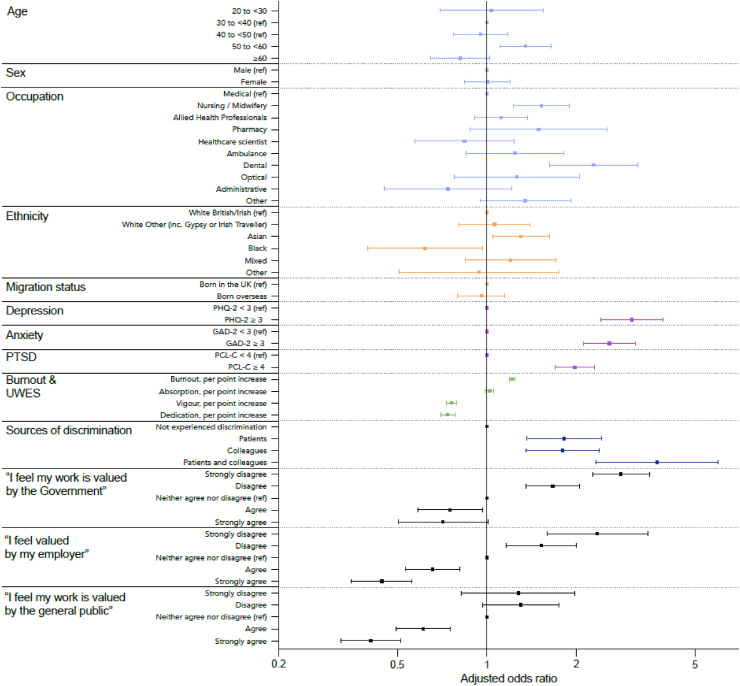
There were 3282 HCW in the main analysis (see Supplementary Figure S1 and Supplementary Tables S1 and S2). 1414 (43.1%) had considered/acted on leaving their role or taking early retirement (36.6% considered only and 6.5% acted upon—see Supplementary Table S4 for further details); 1824 (55.6%) had considered/acted on making any changes to their role. After adjustment, staff aged 50 to <60 (aOR 1.35, 95% CI 1.11–1.64) vs those aged 30 to <40 were more likely to report attrition intentions, as were those in dental (aOR 2.28 95% CI 1.62–3.22) and nursing roles (aOR 1.52 95% CI 1.23–1.90) vs those in medical roles (Fig. 1). Asian staff were more likely to report attrition intentions (aOR 1.30, 95% CI 1.05–1.62) and Black staff were less likely to do so (aOR 0.62, 95% CI 0.40–0.97) vs White British/Irish staff.
Fig. 1.
Logistic regression model showing the association of demographic and occupational characteristics, mental health and wellbeing, discrimination and feeling valued with attrition intentions. The outcome measure is our primary outcome (having considered or acted upon taking early retirement or leaving healthcare entirely). Associations are presented as adjusted odd ratios (circles) together with 95% confidence interval (horizontal spike bars). The base model was age, sex and occupation. Each exposure of interest was added separately to the base model. Analysis of discrimination sources and feeling valued was conducted in a subset (n = 2932) with complete data in these variables. Ref – reference category for categorical variables
We found a striking association between wanting to leave healthcare and meeting screening criteria for depression (aOR 3.07, 95% CI 2.42–3.90), anxiety (aOR 2.58, 95% CI 2.11–3.16), and PTSD (aOR 1.98, 95% CI 1.70–2.30), and scoring higher on the burnout scale (aOR 1.22, 95% CI, 1.19–1.24 per point increase). See Supplementary Tables S1 and S2 for mental health and wellbeing measures. Those scoring higher on the vigour and dedication work engagement scales were less likely to report attrition intentions (vigour: aOR 0.76, 95% CI 0.73–0.79; dedication: aOR 0.74, 95% CI 0.70–0.78) but no association was demonstrated for absorption. As previously,2 there was a very strong association between experiencing discrimination and intending or acting to retire early or leave healthcare, as well as between feeling valued and that outcome (See Fig. 1). Results for the secondary outcome were similar (Supplementary Figure S2 and Supplementary Table S2).
It is concerning that nearly half of HCWs in our sample had considered or taken steps towards leaving healthcare, with highest odds for those aged 50–<60, from the Asian group, and from dental and nursing roles. The profound association between poor mental health and intending to leave the NHS workforce suggests that effective mental health treatment for staff may improve retention alongside their health. Our results also suggest that fostering higher workplace engagement via supportive and collaborative environments and opportunities for personal development,3 as well as organisational changes to minimise burnout, could increase retention.
As we found previously, discrimination and harassment by colleagues and patients were associated with attrition intentions.2 Policies that tackle discrimination may therefore not only address inequity but improve retention. Staff who felt undervalued by the Government were more likely to consider or have acted on leaving. The new UK Government have pledged to reduce the care backlog.4,5 To achieve this, our findings suggest implementing measures to make staff feel the Government appreciates their work, which may include resolving pay disputes.
It should be noted that our outcome measure is derived from questions that specifically ask about pandemic related changes to job roles. However, we believe it is likely that most respondents would report any changes they had made or were planning on making to their role in response to this question even if only indirectly related to or affected by the pandemic. Considering how wide ranging the effects of the COVID-19 pandemic on the healthcare service are, we would expect this measure to capture the impact of equally wide ranging pressures that might lead a healthcare worker to make changes to their role.
Contributors
MP conceived of the idea for UK-REACH and led the application for funding. MP and KW conceived of the idea for I-CARE and led the application for funding with input from CAM, AM, AG and SVK. The questionnaire was designed by CAM, ALG, KW, MP and the study collaborative group. CAM, RM, AM, ALG and SVK formulated the idea for the analysis and contributed to the analysis plan with input from KW and MP. CAM analysed the data with input from RM. CAM and RM have accessed and verified the underlying data. CAM, RM, AM and ALG drafted the manuscript with input from SVK, KW and MP. CAM, RM AM, ALG, SVK, KW and MP edited and approved the final version of the manuscript for publication.
Data sharing statement
To access data or samples produced by the UK-REACH study, the working group representative must first submit a request to the Core Management Group by contacting the UK-REACH Project Manager in the first instance (uk-reach@leicester.ac.uk). For ancillary studies outside of the core deliverables, the Steering Committee will make final decisions once they have been approved by the Core Management Group. Decisions on granting the access to data/materials will be made within eight weeks.
Third party requests from outside the project will require explicit approval of the Steering Committee once approved by the Core Management Group. Note that should there be significant numbers of requests to access data and/or samples then a separate Data Access Committee will be convened to appraise requests in the first instance.
Declaration of interests
ALG reports funding from Orion Pharma, outside of the submitted work. MP reports grants from Sanofi, grants and personal fees from Gilead Sciences and personal fees from QIAGEN, outside the submitted work.
Acknowledgements
I-CARE is supported by a grant from the NIHR Health and Social Care Delivery Program (NIHR157268). UK-REACH was supported by a grant from the MRC-UK Research and Innovation (MR/V027549/1) and the Department of Health and Social Care through the National Institute for Health Research (NIHR) rapid response panel to tackle COVID-19. Core funding was also provided by NIHR Biomedical Research Centres. KW is supported by an NIHR Development Skills Enhancement Award (NIHR302856) and acknowledges funds from the Sutton Trust. MP is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM) and the NIHR Leicester Biomedical Research Centre (BRC). MP is funded by an NIHR Development and Skills Enhancement Award. SVK acknowledges funding from the Medical Research Council (MC_UU_00022/2) and the Scottish Government Chief Scientist Office (SPHSU17). This work is carried out with the support of BREATHE-The Health Data Research Hub for Respiratory Health [MC_PC_19004] in partnership with SAIL Databank. BREATHE is funded through the UK Research and Innovation Industrial Strategy Challenge Fund and delivered through Health Data Research UK.
For the purpose of open access, the author has applied a Creative Commons Attribution license (CC BY) to any Author Accepted Manuscript version arising from this submission.
I-CARE study collaborative group
Manish Pareek (University of Leicester, Chief investigator), Katherine Woolf (University College London, Chief investigator), Carol Woodhams (University of Surrey), Sorin Krammer (University of Surrey), Carol Rivas (University College London), Anna L. Guyatt (University of Leicester), Asta Medisauskaite (University College London), Srinivasa Vittal Katikireddi (University of Glasgow), Padmasayee Papineni (London North West University Healthcare NHS Trust), Susie Lagrata (University College London Hospitals NHS Foundation Trust), Mehrunisha Suleman (University of Oxford), Asad Masood (University of Leicester), Luke Bryant (University of Leicester).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanepe.2024.101133.
Contributor Information
Katherine Woolf, Email: k.woolf@ucl.ac.uk.
Manish Pareek, Email: manish.pareek@leicester.ac.uk.
I-CARE Study Collaborative Group:
Manish Pareek, Katherine Woolf, Carol Woodhams, Sorin Krammer, Carol Rivas, Anna L. Guyatt, Asta Medisauskaite, Srinivasa Vittal Katikireddi, Padmasayee Papineni, Susie Lagrata, Mehrunisha Suleman, Asad Masood, and Luke Bryant
Appendix A. Supplementary data
References
- 1.NHS England . 2023. NHS long term workforce plan. [Google Scholar]
- 2.Martin C.A., Medisauskaite A., Gogoi M., et al. Discrimination, feeling undervalued, and health-care workforce attrition: an analysis from the UK-REACH study. Lancet. 2023;402:845–848. doi: 10.1016/S0140-6736(23)01365-X. [DOI] [PubMed] [Google Scholar]
- 3.Admasachew L., Dawson J. 2010. Staff engagement in the NHS: a multilevel analysis. [Google Scholar]
- 4.BMA NHS backlog data analysis. 2024. https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/nhs-backlog-data-analysis
- 5.Kirk-Wade E., Harker R., Stiebahl S. NHS key statistics: England. https://commonslibrary.parliament.uk/research-briefings/cbp-7281/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.