Abstract
Miscommunication in the OR is a threat to patient safety and surgical efficiency. Our objective was to measure the frequency and causes of communication interference between robotic team members. We observed 78 robotic surgeries over 215 h. 65.4% were General Surgery, most commonly cholecystectomy, identifying Speech Communication Interference (SCI) events, defined as “surgery-related group discourse that is disrupted according to the goals of the communication or the physical and situational context of the exchange”. We noted the causes and strategies to correct the miscommunication, near misses, and case delays associated with each SCI event. Post-surgery interviews supported observations and were analyzed thematically. Overall, we observed 687 SCI events (mean 8.8 ± 6.5 per case, 3.2 per hour), ranging from one to 28 per case. 48 (7.0%) occurred during docking and 136 (19.8%) occurred during a critical moment. The most common causes were concurrent tasks (66.1%); loud noises (10.8%) from patient cart, lightbox fan, and suction machine; and overlapping conversations (4.2%). 94.8% resulted in a case delay. These events distracted from monitoring patient safety and resulted in near misses. Mitigating strategies included leaning out of the surgeon console to repeat the message and employing a messenger. These findings help characterize miscommunication in robotic surgery. Possible interventions include microphones and headsets, positioning the surgeon console closer to the bedside, moving loud equipment further away, and upgrading the patient cart speaker.
Keywords: Communication, Robotic surgery, Anesthesia, Interprofessional teamwork, Surgical error, OR nursing staff
Background
Team communication is essential for maintaining patient safety in the OR [1]. Miscommunication in the non-robotic OR occurs 7–8 times per hour [2] and may be a leading contributor to surgical harm [3, 4]. Task distractions, simultaneous overlapping conversations, and loud machines equivalent to a domestic lawn mower have all been observed to obstruct communication between the team members [5–7]. This may be particularly disruptive in robotic surgeries, which typically have a greater physical separation between the team members, a greater need for communication, and where the room is mostly dark and not acoustically designed for loud equipment [8]. The inability of the surgeon to maintain visual contact with the patient, bed, bedside assistants, circulating nurses, and anesthesia providers leads to an increased need for coordination (e.g., docking, instrument changes) [9], which the built-in speakers and microphones on the da Vinci system do not appear to resolve [10–12].
Thus, it is not surprising that frequent communication and coordination disruptions are common in the robotic OR, leading to repeated instructions and occasional misunderstandings [10]. Strained communication in robotic surgery decreases team effectiveness, raises safety concerns, and has been associated with longer operative times and increased blood loss [11]. Our objective was to directly observe miscommunication between robotic team members and measure its frequency and causes. Studying the sources of acoustic interference on surgical team communication and process might enable interventions that reduce speech interference, and enhance teamwork, performance, efficiency, and safety in the robotic OR.
Methods
Setting and participants
This prospective observational study took place at an urban midwestern teaching hospital with an associated medical school and surgical residency and fellowship programs performing more than 400 robotic surgeries per year, primarily in General Surgery, Gynecology, Urology, and Urogynecology specialties. The institutional review board approved this study as exempt. Surgeries are usually staffed by a teaching surgeon, resident and/or fellow, medical students, nursing staff, scrub techs, and anesthesia staff, including anesthesiologists, CRNAs, and SRNAs. All participants were verbally recruited at department meetings, including nursing staff meetings and again prior to each surgery, and were offered the opportunity to privately decline to be observed. This study was approved as exempt by the University of Missouri Kansas City IRB (#2090394).
Data collection
78 robotic surgeries were directly observed, from setup to the patient leaving the room, by a research assistant (AB) with prior experience in OR miscommunication research and robotic surgery observation, including participant interviewing, minimizing participant reactivity, and collecting field notes.
Data collection was accomplished with a Speech Communication Interference (SCI) instrument, deployed previously in non-robotic surgery [5], and supplemented with field notes. Inter-rater reliability was found to be between 0.87 and 0.98 [5]. SCI was defined as “group discourse which is obstructed according to the goals of the communication, or the physical and situational context of the exchange [13].”
The observer positioned themselves between the surgeon consoles and the bed, capturing SCI events involving all team members. Using the SCI instrument, the observer labeled each event with the relevant portion of the surgery, participants involved, evidence of the event, and the context, including any concurrent loud noises, overlapping conversations, or focus on another task. Roles were noted for each event: the sender, defined as the team member originating and often repeating the message (most commonly an instruction), and the receiver, the intended recipient of that instruction. We also identified any team members who repeated the sender’s message to the receiver, who we describe as “messengers”. Evidence of the event included the sender repeating themselves, the receiver not responding, the receiver asking for clarification, or the messenger repeating the message for the receiver. Case delays were defined as the amount of time a surgical task was interrupted until the receiver responded to the message. Other field notes included the locations of team members, machines in the room, descriptions of loud noises, and the tasks being completed by the sender and receiver. We used a PCE Sound Level Meter 322A to measure the loudness (dB(A)) of machines unique to the robotic OR at a 6-inch distance and repeated twice. The frequency of SCI events was calculated per case and per hour to normalize for differences in observational and procedural durations.
Following our prior research [5], we defined two specific time periods, with several sub-periods in each, configured to explore the unique demands of robotic surgery:
Setup: From staff entering the OR to the start of surgery, including setting up the room and prepping and draping the patient. We defined three sub-periods that have unique team communications: (i) Intubation: from the administration of intubation medications to when the anesthesiologist leaves the OR (ii) Timeout: the time from the circulating nurse announcing timeout to its completion, and iii) all other setup activities.
Surgery Start to End: From the primary surgeon saying “incision” to the patient leaving the room. Five sub-periods were extracted (i) Docking (ii) Surgeon in console, (iii) Critical moment of the surgery: defined prior to timeout by the attending surgeon as the portion of the surgery that is either necessary for a good outcome or at most risk of a complication (iv) Extubation: from the patient opening their eyes to the removal of their endotracheal tube, and (v) all other surgery activities, including attending surgeon operating at the bedside.
Occasionally we observed instances that came close to patient injuries, which we deemed as near misses [14], and although our study was not systematically designed to count them, these events provide valuable insights into the mechanisms of harm that might underlie speech interference.
End-of-surgery interviews
Semi-structured interviews were audio-recorded with selected SCI participants immediately after the surgery, lasting between 1 and 3 min. All interviews began with “How would you describe the communication during this surgery?” followed by questions about the details of specific SCI events, including tasks being performed and noises that might have interfered with communication. Recordings were transcribed, with interviewees identified only by role and linked to the specific SCI event. Themes were generated from all field notes and transcripts. We used PowerPoint to create visual representations and timelines related to the themes to demonstrate the chronology of the event and the relationship to tasks and loud sound sources.
Results
215 h of robotic surgery was observed. Of the 78 observed cases, 65.4% were General surgery (mostly cholecystectomy), with Gynecology (19.2%), Urology (7.7%), Gynecologic oncology (5.1%) and Urogynecology (2.6%). The median duration of observation for all 78 cases was 133.5 min, and Q1 and Q3 were 97.3 and 230.5 min. End-of-surgery interviews were conducted with 119 SCI participants, including 33 (27.7%) attending surgeons, 24 (20.2%) scrub techs, 39 (32.8%) resident surgeons, 22 (18.5%) circulating nurses, and 1 (0.8%) CRNA.
Frequency, evidence, timing, and participants
We observed 687 SCI events, with a mean of 8.8 SCI events per case, and 3.2 SCI events per hour. Every case had at least one SCI event, with a maximum of 28 SCI events in a single case. Evidence of the SCI events included the sender asking for repetition or clarification (484, 70.5%), the sender repeating themselves (177, 25.8%), and no response from the receiver (26, 3.8%), meaning the message was entirely lost. 58 (8.4%) SCI events occurred during setup, including nine (1.3%) during intubation, 2 (0.3%) during timeout, and 47 (6.8%) during the rest of setup. 629 (91.6%) SCI events occurred between surgery start to end, including 48 (7.0%) during docking, 277 (40.3%) while the surgeon was in the console, 136 (19.8%) during the critical moment, 8 (1.2%) during extubation, and 160 (23.3%) from the rest of surgery start to end.
Participants were involved 1979 times in 687 SCI events (Table 1). Attending surgeons were the most common sender (346, 50.6%), circulating nurses were the most common receiver (234, 34.9%), and scrub techs were the most common messenger (238, 57.2%). Figure 1 shows the most common sender and receiver combinations. 61.7% of SCI events involved a messenger, most commonly the scrub tech (238, 57.2%). Postoperative interviews indicated that familiarity with both the procedure and the surgeon prevented SCI events. For example, even if a surgeon’s request was not explicitly heard over the room noise, the scrub tech, based on prior experience, knew what instrument was requested.
Table 1.
SCI event participants and participant combinations
| SCI event participants | SCI events (per 687) |
|---|---|
| Surgery attendings | 533 (26.9%) |
| Surgery resident | 531 (26.8%) |
| Scrub tech | 407 (20.6%) |
| Circulating nurse | 385 (19.5%) |
| CRNA | 63 (3.2%) |
| Other* | 60 (3.0%) |
| Total** | 1979* |
Notes:
Other participants include Anesthesia attending, SRNA, a second surgery attending, and a medical student
Participants were implicated 1,979 times in 687 SCI events over 78 observed cases. Percentages are out of a denominator of 1979
Fig. 1.
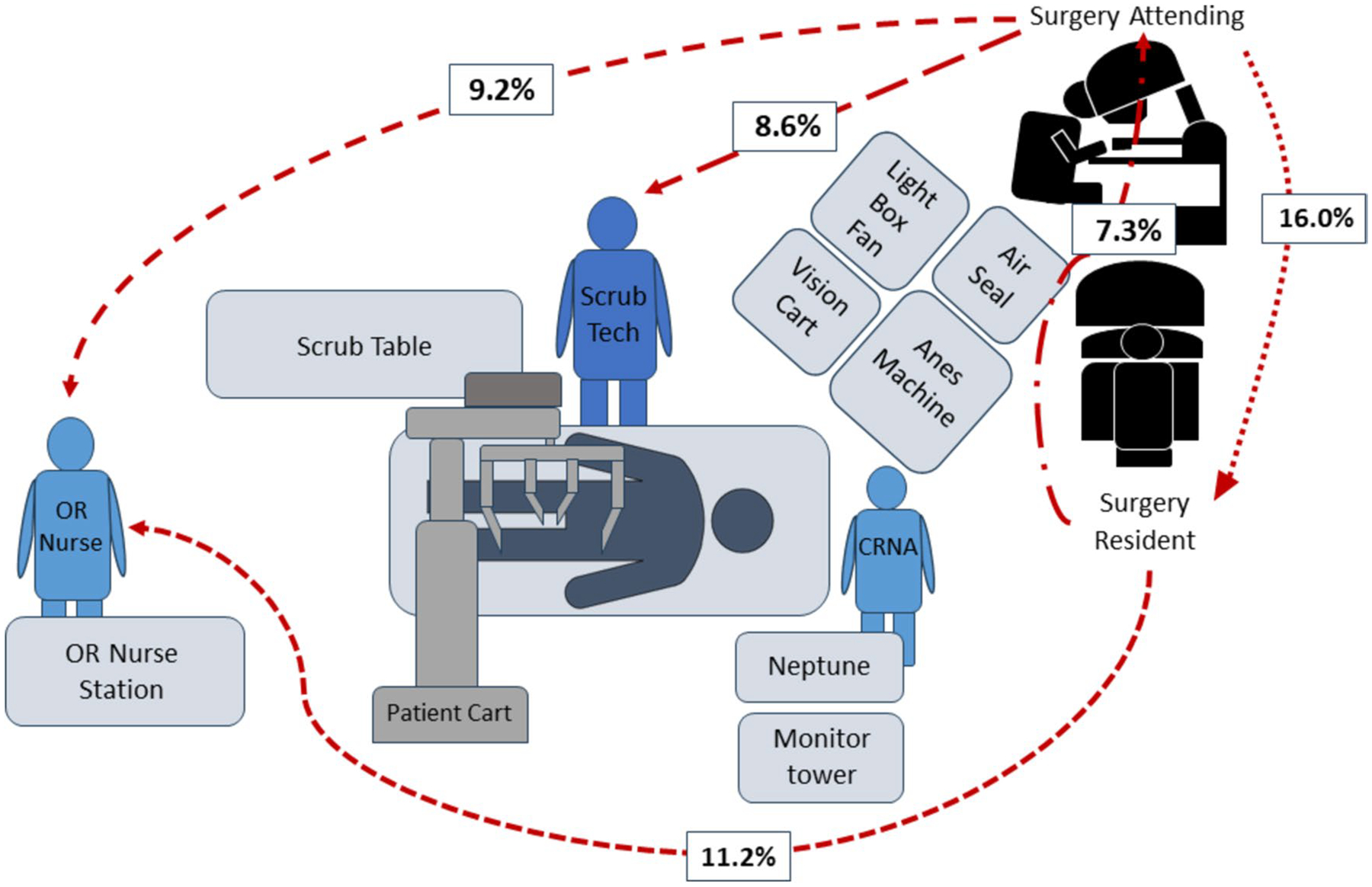
Layout of robotic OR and most common sender and receiver combinations
The most frequent context for the SCI event (Table 2) was the receiver concentrating on another patient-centered task. This included the circulating nurse charting on their laptop, the scrub tech applying covers to the patient cart arms, and the resident at the bedside watching the monitor.
Table 2.
SCI Context, Including Combinations, from 673** Events
| Context | |
| Multitasking* | 445 (66.1%) |
| Concurrent loud noise* | 73 (10.8%) |
| Concurrent overlapping conversation* | 28 (4.2%) |
| Context combinations | |
| Multitasking + loud machine | 37 (5.5%) |
| Multitasking + overlapping conversation | 32 (4.8%) |
| Multitasking + loud machine + overlapping conversation | 31 (4.6%) |
| Other | 27 (4.0%) |
| Total | 673 |
Notes:
Alone, and not in combination with other contexts
14 of the 687 SCI events had missing context data
Loud noises were the second most common context for an SCI. Noise intensity from equipment associated with the robot system, including the patient cart, vision cart, lightbox fan, AirSeal insufflation device, and surgeon console, ranged between 64 and 75 dB. These sound sources were often located between the sender and receiver, who had to “talk over” them. Other interfering noises included the forced air warming device, moving step stools on the floor, opening packaging, and music. Bedside assistants who were receivers of SCI events often spoke of not being able to clearly hear the attending surgeon’s instruction relayed through the speaker on the patient cart.
The third most common context was overlapping conversations, which included: discussions about the patient (e.g., the CRNA and SRNA discussing the patient’s vitals) or other patients (e.g., a patient operated on earlier in the day); teaching conversations (e.g., the attending surgeon teaching the medical student); and sometimes case-irrelevant conversations. There was often more than one conversation occurring simultaneously. For example, in one SCI event, the attending at the bedside did not hear the resident at the console’s question about the dissection while room conversations included those between the attending and another resident, between the scrub tech and circulating nurse, and between the CRNA and SRNA.
Effect on case delay
53 SCI events had missing case delay data. Out of the remaining 634 SCI events, 601 (94.8%) were associated with a case delay. Delays had a median duration of 12.0 s, Q1 and Q3 were 6 and 28, and a range of 1–86 s. 5 s was the most common delay. Most case delays were resolved by clarification or repetition by the sender. Figure 2 shows the distribution of all case delays.
Fig. 2.
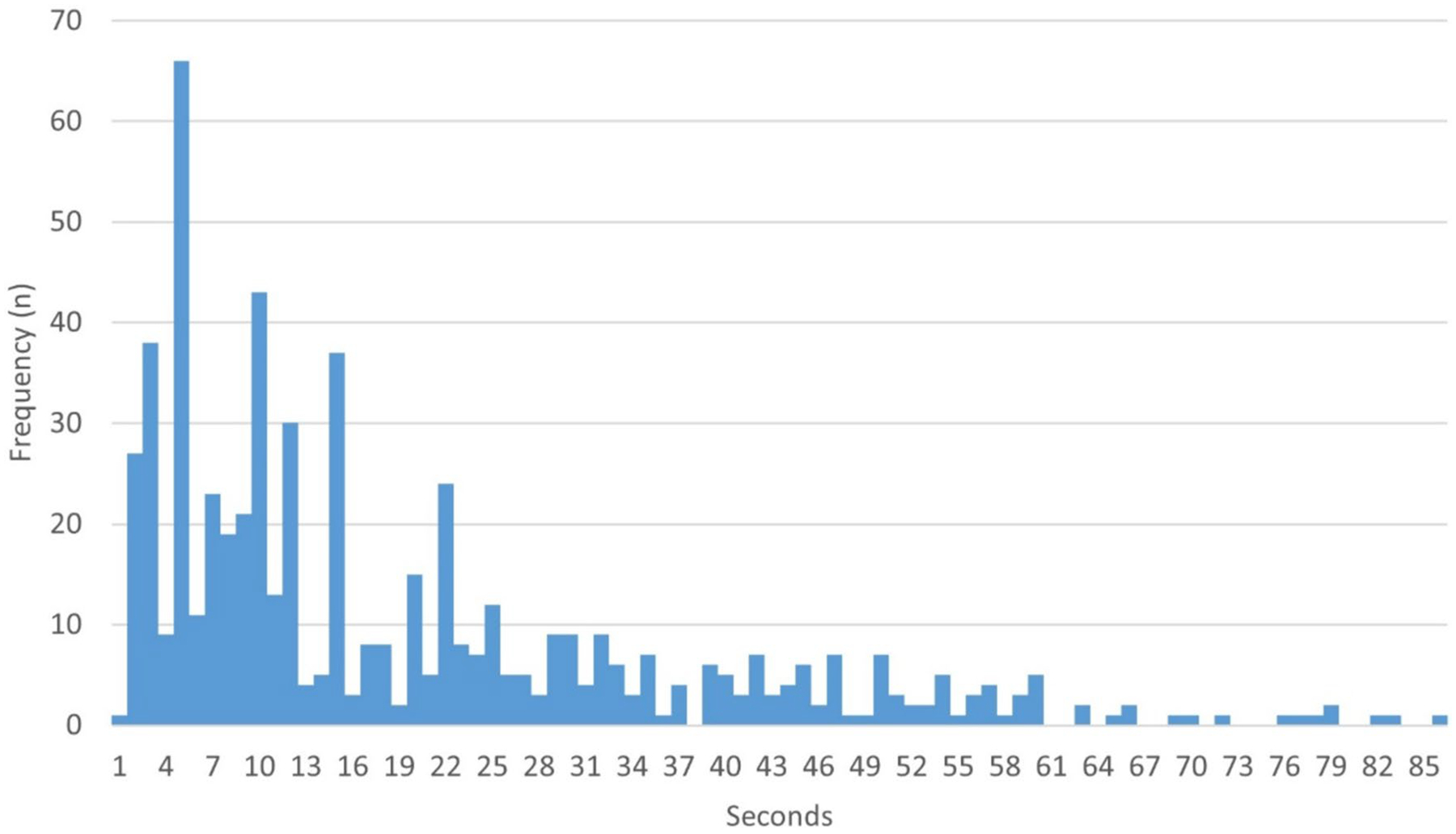
Duration of case delays associated with SCI events (n = 634)
Telephone game and messengers
When SCI events involved a messenger, participants described a “telephone game,” in which the message was transmitted through one or more team members to get to the receiver (Fig. 3). This often involved the attending surgeon’s instruction through the console microphone not being clearly heard by the bedside assistant. 247 (36.0%) of SCI events involved a surgeon leaning out of the console and turning their head toward the bed to repeat the instruction, which was still not clearly heard. One or more messengers, e.g., the resident or the scrub tech, would then relay the message to the receiver. This resulted in a case delay in which the attending surgeon temporarily could not directly view the surgical field.
Fig. 3.
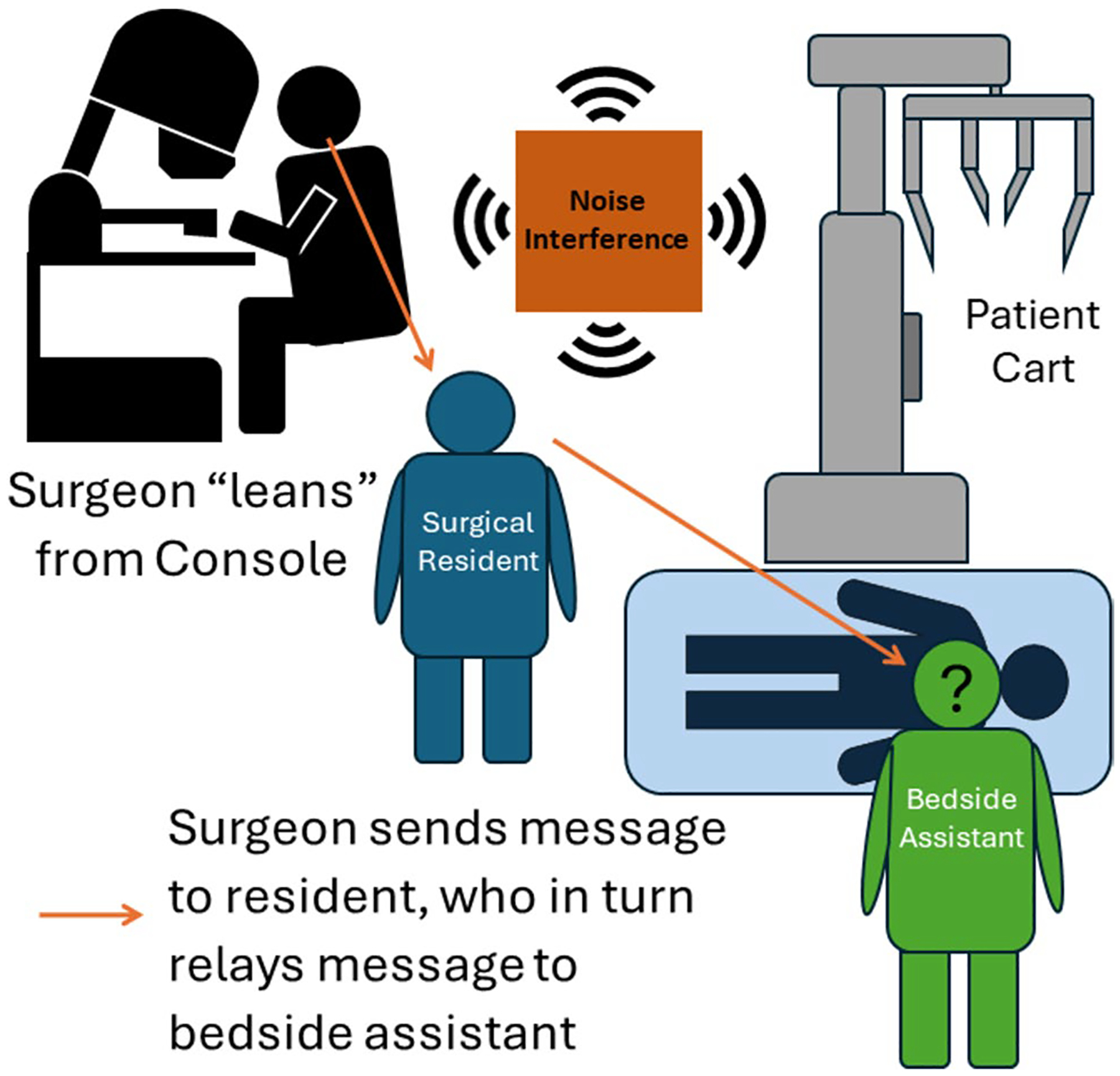
Cartoon demonstrating the “Lean” and the “Telephone Game”
Attending surgeon instructs the bedside assistant by speaking through console microphone, but the message is not heard. The attending removes their head from console viewer, “leans” away from the console, rotates their head, and repeats the message toward the bed, but the message is still not heard. The resident, acting as a “messenger,” then repeats the instruction.
Near misses
No intraoperative patient injury was documented although review of field notes and transcripts of interviews with participants revealed near misses. For example, during an umbilical hernia repair, the resident at the surgeon console requested a clip to address an actively bleeding vessel. The scrub tech was talking to the circulating RN, who was on the phone, and neither heard the request. The attending surgeon repeated the request, and the scrub tech inserted the clip after a 24-s delay. Had the resident lost their tenuous grasp of the vessel during the delay, the patient would have experienced significant blood loss.
In a near miss during a robotic inguinal hernia repair, the attending surgeon, standing by the OR doors and supervising while watching a 2D monitor, told the resident twice to “stop dissecting.” They were separated by the patient cart, vision cart, and lightbox fan. There was music playing and others talking. The resident did not hear the first instruction and asked for clarification after the second instruction. The scrub tech relayed the message to the resident, who then stopped dissecting. Had the resident not heard the instruction and continued their dissection, they may have injured vital organs.
In another near miss, loud machine noise prevented the scrub tech from clearly hearing which arm’s instrument needed to be removed. The scrub tech, began to remove the wrong instrument, prompting the console surgeon to yell “No, that’s 4! You were talking about 2!’” Had the scrub tech removed the wrong instrument, tissue could have been inadvertently damaged.
Discussion
Across 78 robotic surgeries, we found SCI events to occur approximately three times per hour; and nine times per case. Every team member of the OR was affected. SCI occurred at every stage of the surgery, especially while the surgeon was in the console, and was rare during the face-to-face timeout. Every case had at least one event. Approximately 20% of SCIs occurred during the critical moment, 62% involved a messenger, 66% occurred while the receiver was multitasking, 11% in the setting of a loud noise and 4% in the setting of an overlapping conversation. 4% of the time there was no response from the receiver and the message was lost. SCI almost always resulted in a case delay, which, although mostly brief, often extended beyond 25 s. These results suggest that obstructed communication in the loud and busy robotic OR promotes near misses, increases the team’s workload, and threatens employee satisfaction.
These findings partially replicate our prior study of non-robotic surgery [5], with a similar frequency of SCI events. However, the consequences for case delays were higher here, which was likely related to the more frequent use of messengers, the need for the surgeon to “lean” from the console, and the “telephone game”. As well as an inherent risk of the message being changed [15], this has broader implications for both surgical safety and surgeon well-being. Nurses commonly experience [1] and worry about being blamed for miscommunication [12]. The console surgeon may not be aware that the bedside assistant is experiencing difficulties [16]. The need for the surgeon to lean away from the console, and the need for the scrub tech to act as messenger, divides the attention of both, a well observed cause of human error. For the surgeon, there is an added musculoskeletal penalty for leaning and twisting the torso from the console [17–20], the consequences of which may emerge over months or years of repetition.
Most importantly, we found threats to patient safety and extensions of operative time. We witnessed staff repeatedly unable to communicate effectively and efficiently about important tasks. We also witnessed staff distracted from monitoring patient safety. For example, when the surgeon lifted their head out of the console to repeat a message, they were unable to directly observe the surgical field. In another common example, the scrub tech would delay delivering instruments necessary to stop bleeding into the patient cart. Although no patient injuries were observed, we observed several near misses related to miscommunication events.
We join others [16] in calling for novel ways to improve communication in the robotic OR. This could include arranging the OR to facilitate communication between console surgeons and bedside assistants, and relocating loud machines, including the lightbox fan and the vision cart, to reduce communication interference. In the absence of an updated robotic platform with added microphones and speakers, headsets and microphone systems might be beneficial [21]. Standardized language, including scripted speech centered around common tasks [11, 22–24]. and closed-loop communication [1, 12, 22], while also helpful, have been challenging to implement [25]. Other recommendations, including those that bring team members closer in proximity [26], are in Table 3. Rather than there being a single solution for a given OR, constraints, such as feasibility, cost, and sustainability [27], would be valuable to explore.
Table 3.
Suggestions to Reduce Speech Communication Interference in the Robotic OR
| Improve room layout so console surgeons’ backs are not to the bed |
| Remove loud machines located between team members (i.e.: between scrub tech and CRNA) |
| Improve line of sight between team members, perhaps with more screens |
| Headsets and microphones, directed for key communications |
| Conclude any telephone game with closed-loop communication |
| Add more microphones and speakers to the patient cart |
| Sound absorbing materials on the loudest machines |
| Compose robotic teams with high familiarity to each other and the surgery itself |
| Explore nonverbal communication methods to augment verbal communication [28, 29] |
| Standardized scripts for common tasks |
Study limitations
Our study was limited to one hospital although we suspect our findings are generalizable to other robotic ORs. Though we enacted observational methods to limit participant reactivity (Hawthorne Effect) and the observer was largely ignored through careful positioning and familiarity with OR staff it cannot be discounted [30]. This means our SCI estimates may be conservative. We did not collect the durations of the sections of each case, so we are unable to calculate how SCI events per minute differed, for example, in docking. Similarly, for communication disruption pairs the denominator (i.e., how frequently each pair communicated) was not available, so overall failure rates for communication could not be calculated. In future, we plan to experiment with measuring overall communication using video and audio recordings. Future studies should also consider the frequency content rather than just the intensity of the machine noises. As we did not anticipate how serious the near misses would be, we did not start out collecting near misses methodologically, so further work should include methods to systematically collect near misses. Finally, we did not follow the patients post-operatively and thus could not correlate the SCI events or near misses to long-term patient outcomes.
Conclusions
Speech Communication Interference commonly occurs in the robotic OR. Caused by concurrent tasks, noisy equipment, and simultaneous conversation, SCI has a range of implications for surgical performance and safety, including miscommunication, case delays, and potential patient harm. Solutions include alternative OR layout, improved communication technologies, and behavioral training such as closed-loop communication. Future studies should evaluate these interventions and explore the consequences for patients.
Acknowledgements
We ackowledge Austin Bachar for data collection
Funding
This study was funded by a grant from the Intuitive Foundation and from a grant from the Agency for Healthcare Research and Quality (1R01HS029508-01A1). Dr. Sutkin reports grant funding from the Intuitive Foundation and from a grant from the Agency for Healthcare Research and Quality, as described above. No author or family member has any financial interest in the Intuitive Surgical company.
Footnotes
To be presented at the Scientific Forum at American College of Surgeons Clinical Congress 2024: October 19–22, 2024 in San Francisco, CA.
Conflict of interest All authors have no other related conflicts of interest to declare.
Data availability
No datasets were generated or analysed during the current study.
References
- 1.Lee L, Greenway K, Schutz S (2024) What do nurses experience in communication when assisting in robotic surgery: an integrative literature review. J Robot Surg 18(1):50. 10.1007/s11701-024-01830-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu YY, Arriaga AF, Peyre SE, Corso KA, Roth EM, Greenberg CC (2012) Deconstructing intraoperative communication failures. J Surg Res 177(1):37–42. 10.1016/j.jss.2012.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hughes AM, Gregory ME, Joseph DL et al. (2016) Saving lives: a meta-analysis of team training in healthcare. J Appl Psychol 101(9):1266–1304. 10.1037/apl0000120 [DOI] [PubMed] [Google Scholar]
- 4.Thiels CA, Lal TM, Nienow JM et al. (2015) Surgical never events and contributing human factors. Surgery 158(2):515–521. 10.1016/j.surg.2015.03.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bachar A, Brommelsiek M, Simonson R et al. (2024) Speech communication interference in the operating room. J Surg Res 295:723–731. 10.1016/j.jss.2023.11.064 [DOI] [PubMed] [Google Scholar]
- 6.Brommelsiek M, Krishnan T, Rudy P, Viswanathan N, Sutkin G (2022) Human-caused sound distractors and their impact on operating room team function. World J Surg 46(6):1376–1382. 10.1007/s00268-022-06526-9 [DOI] [PubMed] [Google Scholar]
- 7.Gui JL, Nemergut EC, Forkin KT (2021) Distraction in the operating room: a narrative review of environmental and self-initiated distractions and their effect on anesthesia providers. J Clin Anesth 68:110110. 10.1016/j.jclinane.2020.110110 [DOI] [PubMed] [Google Scholar]
- 8.Clanahan JM, Awad MM (2023) How does robotic-assisted surgery change or safety culture? AMA J Ethics 25(8):E615–E623. 10.1001/amajethics.2023.615 [DOI] [PubMed] [Google Scholar]
- 9.Randell R, Alvarado N, Honey S et al. (2015) Impact of robotic surgery on decision making: perspectives of surgical teams. AMIA Annu Symp Proc 2015:1057–1066 [PMC free article] [PubMed] [Google Scholar]
- 10.Catchpole KR, Hallett E, Curtis S, Mirchi T, Souders CP, Anger JT (2018) Diagnosing barriers to safety and efficiency in robotic surgery. Ergonomics 61(1):26–39. 10.1080/00140139.2017.1298845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schiff L, Tsafrir Z, Aoun J, Taylor A, Theoharis E, Eisenstein D (2016) Quality of communication in robotic surgery and surgical outcomes. JSLS 20(3). 10.4293/jsls.2016.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Hamamsy D, Walton TJ, Griffiths TRL, Anderson ES, Tincello DG (2020) Surgeon-team separation in robotic theaters: a qualitative observational and interview study. Female Pelvic Med Reconstr Surg 26(2):86–91. 10.1097/spv.0000000000000829 [DOI] [PubMed] [Google Scholar]
- 13.Lingard L, Espin S, Whyte S et al. (2004) Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care 13(5):330–334. 10.1136/qhc.13.5.330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization (2020) Patient safety incident reporting and learning systems: technical report and guidance [Google Scholar]
- 15.Mesoudi A, Whiten A (2008) The multiple roles of cultural transmission experiments in understanding human cultural evolution. Phil Trans R Soc Lond B Biol Sci 363(1509):3489–3501. 10.1098/rstb.2008.0129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almeras C, Almeras C (2019) Operating room communication in robotic surgery: place, modalities and evolution of a safe system of interaction. J Visc Surg 156(5):397–403. 10.1016/j.jviscsurg.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 17.Craven R, Franasiak J, Mosaly P, Gehrig PA (2013) Ergonomic deficits in robotic gynecologic oncology surgery: a need for intervention. J Minim Invasive Gynecol 20(5):648–655. 10.1016/j.jmig.2013.04.008 [DOI] [PubMed] [Google Scholar]
- 18.Dwyer A, Huckleby J, Kabbani M, Delano A, De Sutter M, Crawford D (2020) Ergonomic assessment of robotic general surgeons: a pilot study. J Robot Surg 14(3):387–392. 10.1007/s11701-019-00996-1 [DOI] [PubMed] [Google Scholar]
- 19.Van’t Hullenaar CDP, Hermans B, Broeders I (2017) Ergonomic assessment of the da Vinci console in robot-assisted surgery. Innov Surg Sci 2(2):97–104. 10.1515/iss-2017-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marshall M, Lux M, Joseph J (2010) Anthropometric assessment of the da Vinci surgical robot. Proc Human Factors Ergon Soc Annu Meet 54(12):899–903. 10.1177/154193121005401220 [DOI] [Google Scholar]
- 21.Tsafrir Z, Janosek-Albright K, Aoun J et al. (2020) The impact of a wireless audio system on communication in robotic-assisted laparoscopic surgery: a prospective controlled trial. PLoS ONE 15(1):e0220214. 10.1371/journal.pone.0220214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong SW, Crowe P (2023) Workflow disruptions in robot-assisted surgery. J Robot Surg 17(6):2663–2669. 10.1007/s11701-023-01728-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alvarado N, Honey S, Greenhalgh J et al. (2017) Eliciting context-mechanism-outcome configurations: experiences from a realist evaluation investigating the impact of robotic surgery on teamwork in the operating theatre. Evaluation 23. 10.1177/1356389017732172 [DOI] [Google Scholar]
- 24.Raheem S, Ahmed YE, Hussein AA et al. (2018) Variability and interpretation of communication taxonomy during robot-assisted surgery: do we all speak the same language? BJU Int 122(1):99–105. 10.1111/bju.14150 [DOI] [PubMed] [Google Scholar]
- 25.Härgestam M, Lindkvist M, Brulin C, Jacobsson M, Hultin M (2013) Communication in interdisciplinary teams: exploring closed-loop communication during in situ trauma team training. BMJ Open 3(10):e003525. 10.1136/bmjopen-2013-003525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pelikan HRM, Cheatle A, Jung MF, Jackson SJ (2018) Operating at a distance—how a teleoperated surgical robot reconfigures teamwork in the operating room. Proc ACM Hum-Comput Interact 2(CSCW):1–28. Article 138. 10.1145/3274407 [DOI] [Google Scholar]
- 27.Lew V (2022) The utilization and validation of the Human Factors Intervention Matrix and the companion assessment tool FACES in the development of novel interventions. Embry-Riddle Aeronautical University. https://commons.erau.edu/edt/684/ [Google Scholar]
- 28.Randell R, Honey S, Alvarado N et al. (2016) Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work 18(2):423–437. 10.1007/s10111-016-0368-0 [DOI] [Google Scholar]
- 29.Tiferes J, Hussein AA, Bisantz A et al. (2019) Are gestures worth a thousand words? Verbal and nonverbal communication during robot-assisted surgery. Appl Ergon 78:251–262. 10.1016/j.apergo.2018.02.015 [DOI] [PubMed] [Google Scholar]
- 30.Paradis E, Sutkin G (2017) Beyond a good story: from Hawthorne effect to reactivity in health professions education research. Med Educ 51(1):31–39. 10.1111/medu.13122 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


