Abstract
Background:
The deep inferior epigastric perforator (DIEP) flap provides an effective and popular means for autologous breast reconstruction. However, with the complexity of the pathway, the environmental impact of the pathway has yet to be evaluated.
Methods:
A retrospective analysis of 42 unilateral DIEPs at a single reconstructive center was performed. Process mapping and life-cycle analyses were performed for equipment, staff, patients, and land. A bottom-up approach was adopted to calculate carbon dioxide equivalent estimates for the initial consultation, preoperative, intraoperative, and immediate postoperative periods.
Results:
This study estimated the carbon footprint of a patient undergoing DIEP flap surgery to be approximately 233.96 kg CO2eq. Induction, maintenance, and running of anesthesia had the highest overall contribution to the carbon footprint (158.17 kg CO2eq, 67.60% overall). Patient and staff travel contributed more than 15% overall carbon emissions in this study. The impact of sterilization was less than half of that from waste management (0.81 versus 1.81 kg CO2eq, respectively). Waste management alone contributed 4.21 kg CO2eq of the overall carbon emissions, the majority of which was accountable to the incineration of 14.75 kg of noninfectious offensive waste.
Conclusions:
This study estimates the carbon footprint of the DIEP pathway. Strategies to mitigate the impact of carbon emissions including usage of reusable vs single-use equipment, virtual consultations, standardization of equipment packs, and optimizing waste disposal were suggested areas for improvement. Data from manufacturers on life-cycle assessments were limited, and further work is needed to fully understand and optimize the impact of DIEP surgery on the environment.
Takeaways
Question: What is the carbon footprint of deep inferior epigastric perforator (DIEP) flap surgery and where are emissions attributed to?
Findings: The estimated carbon footprint of DIEP flap surgery was 233.24 kg CO2eq. Anesthesia had the highest contribution, and patient and staff travel contributed more than 15% carbon emissions in this study. The impact of sterilization was less than half of that from waste management.
Meaning: This is the first study to estimate the carbon footprint of the DIEP pathway. Suggested strategies to mitigate carbon emissions were usage of reusable versus single-use equipment, virtual consultations, standardization of equipment packs, and optimization of waste disposal.
INTRODUCTION
The acuity of strategies to mitigate the environmental impact of our practices has been recognized by the United Nations as the defining crisis of our times.1 The effects of climate change have global consequences, and 2023 surpassed climate records2 with the World Meteorological Organization announcing it as the hottest year since records began.3 The Paris Agreement was a commitment to limit temperature rise to 1.5° with a shift to net zero by 2050.4 However, data show that these goals are not being met, and the goal of the Conference of the Parties 2028 was to identify solutions for limiting temperature rise.5,6 To slow the progression of climate change, every industry must be evaluated, especially those with the highest carbon emissions.7
Healthcare services account for 4%–5% global net emissions, and in the United Kingdom, the National Health Service (NHS) is responsible for 25% of public sector emissions.8–10 Surgery is particularly resource-intensive, accounting for as much as 25% of hospitals’ emissions, despite fewer than 5% of inpatients undergoing surgery.11,12 Interest in sustainable surgery is growing, and the Intercollegiate Green Theatre Checklist was released as part of a joint initiative from the Royal Colleges in the United Kingdom, highlighting the urgent need for increased environmental sustainability in healthcare.13
To increase sustainability in surgery, carbon hotspots must be identified. Life-cycle assessments seek to compile and evaluate the inputs, outputs, and potential environmental impacts of a product or system throughout its life.14 Process mapping represents a potent tool for achieving this, providing a visual representation of a patient journey encompassing all the transactions and encounters. Through following a patient’s journey, the carbon footprint of its constituent aspects and total effect can be calculated. Process mapping has been performed with varying complexities in different specialities, yet its application within plastic surgery has been limited.15–18
The deep inferior epigastric perforator (DIEP) flap is the most common autologous option for breast reconstruction following mastectomy for breast cancer.19,20 Reconstructive cancer surgery is resource-intensive, owing to its complexity; extensive equipment requirements; and long operative times, with DIEP flaps taking an average of 7–8 hours.21,22 This is likely in turn to have a high carbon footprint; however, this has yet to be quantified. This study seeks to quantify the carbon footprint of DIEP reconstructive surgery through process mapping and performing a thorough life-cycle assessment. This will help to identify carbon hotspots and suggest actionable targets to increase the environmental sustainability of DIEP surgery.
METHODS
Study Design and Population
A retrospective service evaluation was performed using data collected from women undergoing DIEP flap reconstruction from April 1, 2022, to September 11, 2023, in a single plastic surgery department at a large teaching hospital in London. Inclusion criteria were unilateral DIEPs, both immediate and delayed, and both bipedicled and unipedicled DIEPs without any extra procedures performed simultaneously. For immediate DIEPs, variables related to the mastectomy including equipment and personnel were not included.
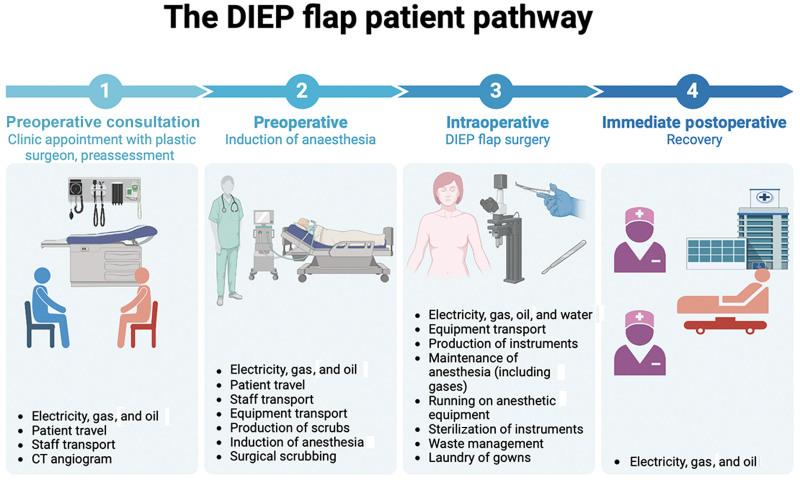
Process mapping for patients undergoing DIEP flap surgery was performed (Fig. 1). Data were categorized into 4 time points: preoperative consultation period (time from first patient encounter with plastic surgery team until final encounter before surgical admission), preoperative (time from admission on the day of the surgery up to entering the theater), intraoperative (time from entering to leaving the theater), and immediately postoperative (recovery area).
Fig. 1.
An illustration of the DIEP flap patient pathway.
Data Collection
This study was registered as an audit at our trust and data were collected using a variety of methods. These included direct data collection through electronic patient records, interviews with staff, raw data collection intraoperatively, surveys, contact with hospital departments including procurement, the central sterilization unit and estates, and contact with external suppliers. Where raw data were not available, reasonable estimates were made using existing literature as benchmarks. (See appendix, Supplemental Digital Content 1, which shows details of data variables and sources, http://links.lww.com/PRSGO/D688.)
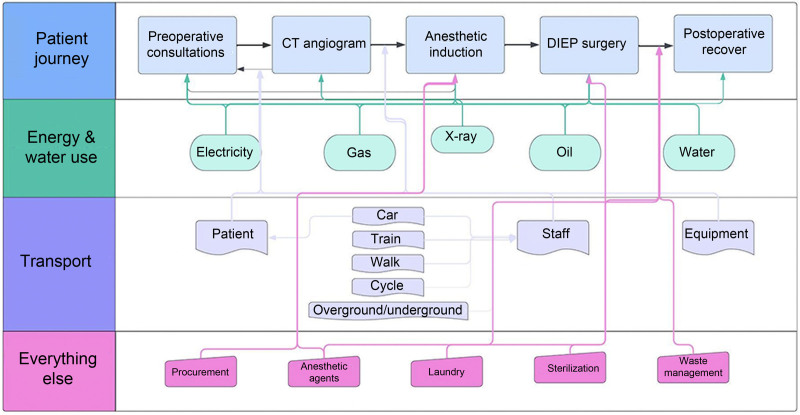
In addition to stratification of data via time frame, data were also categorized by sector. This included procurement of equipment; energy and water supply; staff and patient travel; sterilization of reusable equipment; waste management of disposable equipment; and contribution of anesthesia, including gases and the impact of running anesthetic equipment.
DIEP Protocol
Before the DIEP flap, all patients underwent a computerized tomography angiogram to assess vessel caliber. The personnel intraoperatively included anesthetists, surgeons, nurses, and operating department practitioners/healthcare assistants. Some DIEPs are dual-consultant led; however, most are single consultant with 2 junior assisting surgeons. Postoperatively, all patients follow the enhanced recovery after surgery protocol to encourage early mobility, decrease length of stay, and optimize outcomes.23–25
Carbon Footprint Calculations
The carbon footprint for each sector of the patient journey on the process map was calculated and summed in the units of carbon dioxide equivalents (CO2eq) using multiplication factors from sources including government reports, previous studies, and online resources.26–36 (See appendix, Supplemental Digital Content 2, which shows comprehensive details of the determination of the CO2eq for each sector, http://links.lww.com/PRSGO/D688.)
Boundary Setting
A study of this type requires clear limits to be set and assumptions to be made. Our study observed patients from their first encounter following referral up until leaving the recovery area. The postoperative period was not included due to its highly variable nature.
RESULTS
Patient Characteristics
A total of 42 patients underwent unilateral DIEP flaps between April 1, 2022, and September 11, 2023, at our center (Table 1). Most underwent immediate DIEP surgery and most were unipedicled (71.4%, N = 30). The average time in the anesthetic room before entering the theater was 29.68 minutes and average operative time was just over 9 hours (544.33 min). Most patients received induction with propofol and remifentanil and maintenance with nitrous oxide and oxygen at a low flow rate.
Table 1.
Average Variables Used to Calculate CO2eq for 42 DIEP Flaps
| Variable | N (%) or Mean |
|---|---|
| No. patients |
42 (100) |
| Timing of DIEP | |
| Immediate | 37 (88.1) |
| Delayed | 5 (11.9) |
| Unipedicled or bipedicled | |
| Unipedicled | 30 (71.4) |
| Bipedicled | 12 (28.6) |
| Average no. in-person consultations before DIEP | 2 |
| Average distance from patient postcode to hospital, km | 17.69 |
| Average time in anesthetic room, min | 29.68 |
| Average time in theater, min | 544.33 |
| Most common method of anesthetic induction | Propofol + remifentanil (TIVA) |
| Most common maintenance gases | N2O 5 L/min and supplementary O2 |
| Average no. staff preoperatively | 4 |
| Average no. staff intraoperatively | 10 |
| Average distance from staff postcode to hospital, km | 12.77 |
| Most common method of staff transport | |
| Surgeon | Overground/underground |
| Nurse | Overground/underground |
| HCA | Walk |
| ODP | Train |
| Anesthetist | Cycle |
| Average distance from preoperative equipment supplier postcode to hospital, km | 221.39 |
| Average distance from intraoperative equipment supplier postcode to hospital, km | 192.91 |
| Weight of waste, kg | 18.95 (100) |
| Sharps | 1.10 (5.80) |
| Noninfectious offensive waste | 14.75 (77.84) |
| Dry mixed recyclable waste | 3.1 (16.36) |
HCA, healthcare assistant, ODP, operating department practitioner; TIVA, total intravenous anesthetic.
On average, patients had 2 in-person consultations with either plastic surgeons or anesthetists for preassessment clinics requiring travel to our center before their surgery. Patients generally traveled farther than staff to hospital (17.69 versus 12.77 km, respectively). There was variation in the mode of travel between staff, with surgeons and nurses tending to travel by overground or underground, healthcare assistants tending to walk, operating department practitioners taking the train, and anesthetists choosing to cycle as the most common method of commuting.
There were many different equipment suppliers for surgical instruments, anesthetic equipment, and scrubs, all of which were UK based. The average distance equipment was transported was 221.39 and 192.91 km for preoperative and intraoperative equipment, respectively. Data on the production of individual items was requested from external suppliers but was only available from 1 supplier of anesthetic equipment. A list of the average number of intraoperative surgical equipment for the 42 patients undergoing DIEP flaps is shown (See appendix, Supplemental Digital Content 3, which shows average number of surgical equipment for the 42 patients undergoing DIEP flap surgery, http://links.lww.com/PRSGO/D688).
There were 3 main waste streams from the DIEP surgery: sharps, noninfectious offensive, and dry mixed recyclable waste. More than 77% of the total weight of waste contribution was from noninfectious offensive waste (18.95 kg). Eight consultant surgeons performed the DIEP flaps with minimal variability between them in terms of technical details of procedures performed, number of preoperative in-person consultations, operative time, and equipment used.
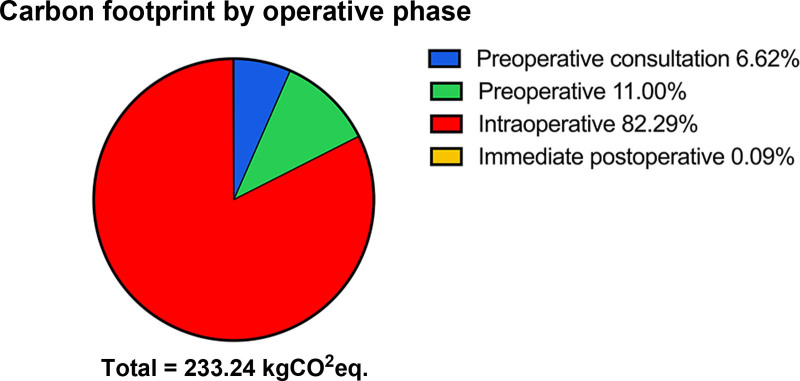
Overall Carbon Footprint
The total carbon footprint for a patient undergoing DIEP flap surgery from first encounter with the plastic surgery department to leaving the recovery area after surgery was calculated to be 233.96 kg CO2eq and involved a complex interplay of contributing factors (Fig. 2). Unsurprisingly, the highest contribution was from the intraoperative period (192.10 kg CO2eq, 82.32%, Fig. 3). However, even before entering the theater, there was 41.14 kg CO2eq emitted.
Fig. 2.
A flowchart showing the complex interplay of factors contributing to the overall carbon footprint of DIEP flap surgery.
Fig. 3.
A pie chart showing the contribution of each operative phase to the overall carbon footprint of DIEP flap surgery.
Consultation Period Contributors
Before the day of surgery, 15.46 kg CO2eq was emitted, 6.60% overall emissions (Table 2) and equivalent to driving 56.34 miles. The majority of this was attributable to patient travel to our hospital (77.81% of the consultation period emissions and 5.14% overall). The second highest contributor to emissions was the running of a computed tomography scanner (2.70 kg CO2eq, 17.46% consultation period emissions), and remaining emissions came from staff travel and building energy usage.
Table 2.
Carbon Dioxide Equivalents (kg CO2eq) for Each Sector in Each Operative Period
| kg CO2eq | % Overall Emissions | |
|---|---|---|
| Total | 233.96 | 100 |
| Preoperative consultation total | 15.46 | 6.60 |
| Electricity, gas, and oil | 0.35 | 0.15 |
| Patient travel | 12.03 | 5.14 |
| Staff travel | 0.38 | 0.16 |
| CT angiogram | 2.70 | 1.15 |
| Preoperative total | 25.68 | 10.97 |
| Electricity, gas, and oil | 0.05 | 0.02 |
| Patient travel | 3.00 | 1.28 |
| Staff travel | 2.66 | 1.14 |
| Equipment transport | 0.07 | 0.03 |
| Production of scrubs | 11.28 | 4.82 |
| Induction of anesthesia | 8.47 | 3.62 |
| Surgical scrubbing | 0.15 | 0.06 |
| Intraoperative total | 192.61 | 82.32 |
| Electricity, gas, oil, and water | 10.46 | 4.47 |
| Equipment transport | 4.31 | 1.84 |
| Production of instruments | 21.52 | 9.20 |
| Maintenance of anesthesia (including gases) | 145.16 | 62.04 |
| Running on anesthetic equipment | 4.54 | 1.94 |
| Sterilization of instruments | 1.90 | 0.81 |
| Waste management | 4.21 | 1.80 |
| Laundry of gowns | 0.51 | 0.22 |
| Immediate postoperative total | 0.21 | 0.09 |
| Electricity, gas, and oil | 0.21 | 0.09 |
CT, computerized tomography.
Preoperative Contributors
During the preoperative period before the patient entered the theater on the day of surgery, there was 25.68 kg CO2eq emitted (10.97% overall, equivalent of driving 93.59 miles), 43.93% of which came from the production of staff scrubs and patient gowns. This was followed by the induction of anesthesia, which made up 32.98% of total preoperative emissions (8.47 kg CO2eq). Staff and patient travel contributed a joint total of 5.66 kg CO2eq (22.04% preoperative emissions), and other contributors included building energy costs, equipment transport, and surgical scrubbing.
Intraoperative Contributors
The intraoperative period had a profound impact on emissions (192.61 kg CO2eq, the equivalent of driving 701.95 miles), owing to the multitude of factors involved and the operative time (average 9.07 h per DIEP). The biggest contributor was the maintenance of anesthesia (including nitrous oxide and oxygen usage at 5L/min), which made up 75.36% intraoperative and 62.04% overall emissions. Production of instruments had the second largest impact on emissions, contributing 21.52 kg CO2eq (9.20% overall emissions and 50.15% intraoperative emissions when excluding anesthesia). Building energy and water usage formed 5.43% of intraoperative emissions (24.38% excluding anesthesia). The differential impact of single-use versus reusable instruments was factored in through accounting for instrument production, transport, sterilization of reusable equipment, and waste management of disposable equipment. Waste management emitted 2.22 times higher kg CO2eq compared with sterilization (4.21 versus 1.90 kg CO2eq), and equipment transport made up over 10% intraoperative emission after excluding the impact of anesthesia.
Postoperative Contributors
The immediate postoperative period had the lowest contribution to overall emissions (0.21 kg CO2eq, 0.09% overall emissions), which came from building energy usage.
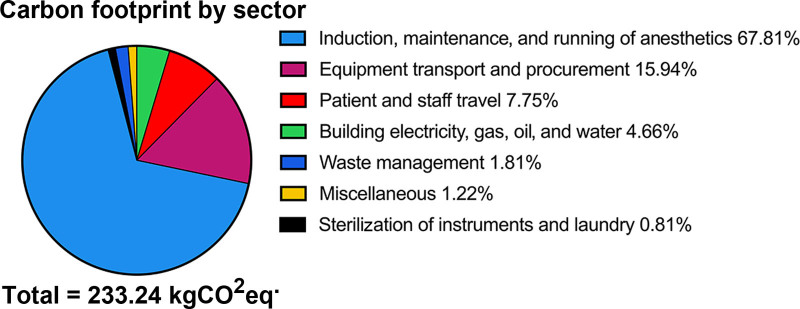
When combining data from operative periods to sum respective sectors, the induction, maintenance, and running of anesthetics was the predominant source of CO2 emissions (158.17 kg CO2eq, 67.61% total; Table 3, Fig. 4). The second highest contribution was from transport and procurement of equipment (37.18 kg CO2eq, 15.89%). Patient and staff travel had a greater impact than building electricity, gas, oil, and water usage (18.07 versus 10.86 kg CO2eq, respectively).
Table 3.
Carbon Dioxide Equivalents (kg CO2eq) for Each Sector
| kg CO2eq | % | |
|---|---|---|
| Total | 233.96 | 100 |
| Induction, maintenance, and running of anesthetics | 158.17 | 67.60 |
| Equipment transport and procurement | 37.18 | 15.89 |
| Patient and staff travel | 18.07 | 7.72 |
| Building electricity, gas, oil, and water | 10.86 | 4.64 |
| Waste management | 4.21 | 1.80 |
| Miscellaneous* | 2.85 | 1.22 |
| Sterilization of instruments and laundry | 2.41 | 1.03 |
Emissions from computerized tomography angiogram and laundry of patient gowns and scrubs.
Fig. 4.
A pie chart showing the contribution of each sector to the overall carbon footprint of DIEP flap surgery.
DISCUSSION
Surgical pathways are intrinsically complex and resource-intensive, requiring robust supply chains to ensure appropriate maintenance, transport, and disposal of equipment, as well as maintenance of land and travel of patients and staff for any surgery. This study calculates the carbon footprint of DIEP flap surgery and maps the patient journey from the preoperative phase until recovery, also including the impact of anesthesia. This study found that the carbon footprint of a patient undergoing DIEP flap surgery is approximately 233.96 kg CO2eq. This is equivalent to driving a car for 1372 km or flying 1549 km, which is roughly the same as flying from London to Florence.37
The magnitude of carbon emissions from DIEP flap surgery emphasizes the importance of process mapping to identify carbon hotspots, which can be targeted to reduce the carbon footprint of the patient pathway. We found that although the intraoperative period had the greatest contribution to the overall carbon footprint (192.61 kg CO2eq, 82.32%), 41.14 kg CO2eq was emitted before a patient entered theater. Through analysis of other operative periods including the preoperative and immediate postoperative period, interventions for each stage can be suggested. For example, in the consultation period, there was an average of 2 clinic appointments. It could be suggested that 1 of these could be virtual to reduce emissions from patient travel and building energy usage, which contributed to more than 80% of emissions in the consultation period. During the COVID-19 pandemic, there was an unprecedented rise in virtual consultations.38 However, even before this, an increased utilization of telemedicine was a priority for the NHS. The 2019 NHS long-term plan detailed benefits of virtual consultations, including reduced financial cost, decreased nonattendance, and overall reduced air pollution in line with NHS net zero by 2040.39 Patient and staff travel contributed more than 15% of overall emissions in this study, and in 2017, 3.5% total UK road travel was accounted for by patients, visitors, staff, and suppliers to the NHS.40 The impact of pollution on population health is significant, causing 8.34 million excess deaths per year from fine particulate and ozone air pollution.41
Subsector analysis of carbon emissions is important to identify targets for reducing carbon emissions. Induction, maintenance, and running of anesthesia had the highest contribution to the carbon footprint (158.17 kg CO2eq, 67.61% overall). The contribution of anesthetic gases on the NHS carbon footprint was highlighted by Whiting et al,42 who estimated that anesthetic gases contributed 42% of annual surgery greenhouse gas emissions. Total intravenous anesthetic is a technique with significantly lower impact on emissions, and ongoing pressure to reduce the use of anesthetic gases is evident with the Royal College of Anaesthetists announcing their plan to decommission desflurane.43,44 Using total intravenous anesthetic in this study would have reduced carbon footprint emissions by a huge 38%. Another way to decrease the impact of anesthesia is through decreased operative time. Surgeons should strive to increase efficiency without compromising patient safety. The emphasis on sustainability within anesthetic equipment suppliers was also evident as the only companies able to provide comprehensive life-cycle assessments and individualized carbon emissions from products. (See appendix, Supplemental Digital Content 4, which shows an example of life-cycle assessments performed for individual anesthetic equipment, http://links.lww.com/PRSGO/D688.) No surgical equipment manufacturers contacted during this study could provide individualized data, highlighting the relatively nascent nature of life-cycle assessments. This suggests that more work is needed by manufacturers in pursuit of sustainability goals, as well as consideration of this regarding procurement. This is particularly important as the second highest contributor to overall emissions during the DIEP patient journey was procurement and transport of instruments (37.18 kg CO2eq, 15.89% overall).
Annually, healthcare services worldwide produce more than 5 million metric tons of waste, and in the United Kingdom, the NHS produces 133,000 metric tons of plastic, only 5% of which is recycled.45,46 Operating departments contribute 50%–70% of clinical waste.47,48 In our study, the weight of waste in each stream was recorded. We found that waste management alone contributed 4.21 kg CO2eq overall emissions, most of which was accountable to incineration of 14.75 kg noninfectious offensive waste. This emphasizes the need for increased recycling, which was highlighted as an area for improvement in the Royal College of Surgeons of England’s Sustainability in the Operating Theatre Good Practice Guide.49 A barrier to recycling noted by operating department staff during our study was that if waste was incorrectly segregated, the whole bag could no longer be recycled and was instead incinerated. Solutions to this may include further recycling waste segregation streams.50
Reuse where possible is also a priority within sustainable surgery, and our study showed that the impact of sterilization was less than half of that from waste management (0.81 versus 1.81 kg CO2eq). Within surgery, there is a reliance on single-use instruments due to concerns surrounding infection risk and financial implications. Although there is growing evidence to suggest reusable instruments can safely be used, Bhutta53 argued that to decrease reliance on single-use equipment there is a need for governmental policy and attitude change among surgeons.51–53 Reuse of equipment is expanding beyond surgical instruments to include the reuse of drapes and patient gowns. Rizan et al32 reported that the reuse of surgical instruments and linens as opposed to single use reduced the carbon footprint by 36%.32 Where it is not possible to switch from single use to reusable instruments, we propose the removal of unutilized instruments from surgical packs, which can be identified through inventories.54–56
This study, through process mapping, calculates the carbon footprint of a complex procedure with the inclusion of the preoperative consultation period, preoperative anesthetic, and immediate postoperative period. Thiel et al15 and Morris et al16 have calculated the carbon footprint of cataract surgery with estimates of up to 181 kg CO2eq emitted. However, cataract surgery is a much shorter procedure requiring far less equipment and personnel. Therefore, our study provides an important progression of existing literature, elucidating where carbon contributions can be attributed for lengthier, complex procedures. Interestingly, our overall carbon footprint calculations were only 28.8% higher than those found in the study by Morris et al16 (52.16 kg CO2eq more), suggesting that the individual setup of the surgery rather than the length of surgery is the most important contributing factor. It can, therefore, be suggested that 1 way to decrease the environmental impact of surgery is to have longer operating lists on fewer days.
This study has considered many factors within the patient pathway to calculate the most representative estimate of the carbon footprint of DIEP flap surgery. This study should not be used by lawmakers or insurance companies but is intended to be used by surgeons to evaluate ways they can increase the sustainability of their practice. A study of this kind has challenges and limitations to data collection and calculations. The global impetus surrounding sustainability and climate change will likely result in medical equipment suppliers performing further research and life-cycle assessments on individual products. Furthermore, due to patient-specific factors, there was inevitably variability between each surgery (mean operative time range, 270 min) and therefore the calculated figures must be interpreted as an estimate. We sought to mitigate patient variability through our large sample size. However, variability between surgeons still exists due to surgeon-specific preferences in equipment, operative time, and operation type (eg, bipedicled versus unipedicled DIEPs).57
This study is novel within plastic surgery and may serve as a framework to calculate the carbon footprint of other pathways. Preliminary calculations suggest that implant-based reconstruction contributes only 21% emissions compared to that from DIEPs (48.80 kg CO2eq). (See appendix, Supplemental Digital Content 5, which shows variation between DIEP and implant-based reconstruction by operative phase, http://links.lww.com/PRSGO/D688.) Further work should be performed to identify carbon hotspots within implant-based reconstruction and the impact of any subsequent revisional procedures in the 2 pathways. It is hoped that such studies may serve as a tool for surgeons, healthcare staff, and clinical directors to benchmark and understand the impact that our work has on the environment and how we can work together to improve the sustainability of surgery.
CONCLUSIONS
This study estimated the carbon footprint of a patient undergoing DIEP flap surgery to be approximately 233.96 kg CO2eq, through process mapping the DIEP pathway for patients, equipment, land, and staff. Strategies to mitigate the impact of carbon emissions including usage of disposable versus reusable equipment, virtual consultations, standardization of equipment packs, and optimizing waste disposal were suggested areas for improvement. Data from manufacturers on life-cycle assessments was limited, and further work is needed to fully understand and optimize the impact of DIEP surgery on the environment.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 26 December 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.United Nations. The climate crisis—a race we can win. 2020. Available at https://www.un.org/en/un75/climate-crisis-race-we-can-win. Accessed February 12, 2023. [Google Scholar]
- 2.Ripple WJ, Wolf C, Gregg JW, et al. The 2023 state of the climate report: entering uncharted territory. BioScience. 2023;73:841–850. [Google Scholar]
- 3.World Meteorological Organization. 2023 Shatters climate records, with major impacts. 2023. Available at https://wmo.int/news/media-centre/2023-shatters-climate-records-major-impacts#:~:text=The%20WMO%20provisional%20State%20of,%2Dindustrial%201850%2D1900%20baseline. Accessed February 18, 2024. [Google Scholar]
- 4.TIAS. Paris agreement to the United Nations framework convention on climate change. 2015. Available at https://unfccc.int/sites/default/files/resource/parisagreement_publication.pdf. Accessed February 18, 2024. [Google Scholar]
- 5.Jones N. When will global warming actually hit the landmark 1.5ºC limit? Nature. 2023;618:20. [DOI] [PubMed] [Google Scholar]
- 6.Boehm SL, Jeffery J, Hecke C, et al. State of climate action 2023. 2023. Available at https://www.wri.org/research/state-climate-action-2023. Accessed February 18, 2024. [Google Scholar]
- 7.NASA. Is it too late to prevent climate change?. 2013. Available at https://climate.nasa.gov/faq/16/is-it-too-late-to-prevent-climate-change/#:~:text=While%20the%20effects%20of%20human,otherwise%20persist%20for%20essentially%20forever. Accessed February 12, 2023. [Google Scholar]
- 8.Watts N, Amann M, Arnell N, et al. The 2019 report of the lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karliner J, Slotterback S, Boyd R, et al. Health care’s climate footprint: how the health sector contributes to the global climate crisis and opportunities for action. Health care without harm. Climate-smart health care series. Green paper number one. Produced in collaboration with ARUP. September 2019. [Google Scholar]
- 10.Tennison I, Roschnik S, Ashby B, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5:e84–e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS England. University Hospitals Birmingham: a world first in carbon net zero surgery. 2022. Available at https://www.england.nhs.uk/greenernhs/whats-already-happening/university-hospitals-birmingham-a-world-first-in-carbon-net-zero-surgery/#:~:text=Operating%20theatres%20are%20an%20important,of%20hospital%20inpatients%20undergoing%20surgery. Accessed February 12, 2023. [Google Scholar]
- 12.MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381–e388. [DOI] [PubMed] [Google Scholar]
- 13.Robb HD, Pegna V. The intercollegiate green theatre checklist. Bull R Coll Surg Engl. 2023;105:64–67. [Google Scholar]
- 14.ISO. ISO 14040:2006. Environmental management—life cycle assessment—principles and framework. 2006.
- 15.Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43:1391–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris DS, Wright T, Somner JE, et al. The carbon footprint of cataract surgery. Eye (Lond). 2013;27:495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rougereau G, Chatelain L, Zadegan F, et al. Estimation of the carbon footprint of arthroscopic rotator cuff repairs in France. Orthop Traumatol Surg Res. 2023;110:103755. [DOI] [PubMed] [Google Scholar]
- 18.Talibi SS, Scott T, Hussain RA. The environmental footprint of neurosurgery operations: an assessment of waste streams and the carbon footprint. Int J Environ Res Public Health. 2022;19:5995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. [DOI] [PubMed] [Google Scholar]
- 20.Zhang A, Dayicioglu D. Outcomes of 270 consecutive deep inferior epigastric perforator flaps for breast reconstruction. Ann Plast Surg. 2018;80:S388–S394. [DOI] [PubMed] [Google Scholar]
- 21.Agbafe V, Berlin NL, Butler CE, et al. Prescriptions for mitigating climate change-related externalities in cancer care: a surgeon’s perspective. J Clin Oncol. 2022;40:1976–1979. [DOI] [PubMed] [Google Scholar]
- 22.Shtarbanov P, Ioannidi L, Hamilton S, et al. Prolonged operative time is a risk factor for adverse postoperative outcomes in the unilateral deep inferior epigastric perforator (DIEP) flap surgery: a retrospective cohort study. J Plast Reconstr Aesthet Surg. 2023;87:180–186. [DOI] [PubMed] [Google Scholar]
- 23.Gort N, van Gaal BGI, Tielemans HJP, et al. Positive effects of the enhanced recovery after surgery (ERAS) protocol in DIEP flap breast reconstruction. Breast. 2021;60:53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haddock NT, Garza R, Boyle CE, et al. Observations from implementation of the ERAS protocol after DIEP flap breast reconstruction. J Reconstr Microsurg. 2022;38:506–510. [DOI] [PubMed] [Google Scholar]
- 25.Linder S, Walle L, Loucas M, et al. Enhanced recovery after surgery (ERAS) in DIEP-flap breast reconstructions: a comparison of two reconstructive centers with and without ERAS-protocol. J Pers Med. 2022;12:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin M, Mohnke A, Lewis GM, et al. Environmental impacts of abdominal imaging: a pilot investigation. J Am Coll Radiol. 2018;15:1385–1393. [DOI] [PubMed] [Google Scholar]
- 27.GOV.UK. Conversion factors 2023: condensed set (for most users). Updated June 28, 2023. Available at https://www.gov.uk/government/publications/greenhouse-gas-reporting-conversion-factors-2023. Accessed February 18, 2024. [Google Scholar]
- 28.FreeMapTools. Distance between UK postcodes. Available at https://www.freemaptools.com/distance-between-uk-postcodes.htm. Accessed February 18, 2024. [Google Scholar]
- 29.Ritchie H. Which form of transport has the smallest carbon footprint?. 2023. Available at https://ourworldindata.org/travel-carbon-footprint. Accessed February 18, 2024. [Google Scholar]
- 30.Narayanan H, Raistrick C, Tom Pierce JM, et al. Carbon footprint of inhalational and total intravenous anaesthesia for paediatric anaesthesia: a modelling study. Br J Anaesth. 2022;129:231–243. [DOI] [PubMed] [Google Scholar]
- 31.Association of Anaesthetists. 2022. The anaesthetic impact calculator. Available at https://anaesthetists.org/Home/Resources-publications/Environment/Guide-to-green-anaesthesia/Anaesthetic-gases-calculator. Accessed February 18, 2024. [Google Scholar]
- 32.Rizan C, Lillywhite R, Reed M, et al. The carbon footprint of products used in five common surgical operations: identifying contributing products and processes. J R Soc Med. 2023;116:199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathers J. Green Freight Math: how to calculate emissions for a truck move 2015. 2015. Available at https://business.edf.org/insights/green-freight-math-how-to-calculate-emissions-for-a-truck-move/. Accessed February 18, 2024. [Google Scholar]
- 34.Cannings E, Kenington C, Cox K. Sustainability prize 2 calculating the carbon footprint of surgical scrubbing. Br J Surg. 2022;109:1. [Google Scholar]
- 35.NHS England and NHS Improvement. Scrubs, gowns, alginate bags and linen cages. 2020. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0294-letter-linen-and-laundry-15-april-2020.pdf. Accessed February 18, 2024. [Google Scholar]
- 36.Shahmohammadi S, Steinmann Z, Clavreul J, et al. Quantifying drivers of variability in life cycle greenhouse gas emissions of consumer products—a case study on laundry washing in Europe. Int J Life Cycle Assess. 2018;23:1940–1949. [Google Scholar]
- 37.Distance.to. Distance from London to Geneva. Available at https://www.distance.to/London,Greater-London,England,GBR/Florence,ITA. Accessed March 4, 2024. [Google Scholar]
- 38.NHS England and NHS Improvement. Important and urgent—next steps on NHS response to COVID-19. 2020. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf. Accessed February 21, 2024. [Google Scholar]
- 39.NHS England. The NHS long term plan. 2019:26–38. Available at https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf. Accessed February 21, 2024. [Google Scholar]
- 40.NHS England. Delivering a “Net Zero” national health service. 2020. Available at https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf. Accessed February 23, 2024. [Google Scholar]
- 41.Lelieveld J, Haines A, Burnett R, et al. Air pollution deaths attributable to fossil fuels: observational and modelling study. BMJ. 2023;383:e077784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Whiting A, Tennison I, Roschnik S, et al. Surgery and the NHS carbon footprint. Bull R Coll Surg Engl. 2020;102:182–185. [Google Scholar]
- 43.Sherman J, Le C, Lamers V, et al. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg. 2012;114:1086–1090. [DOI] [PubMed] [Google Scholar]
- 44.Association of Anaesthetists. Joint statement on NHSE’s plan to decommission desflurane by early 2024. 2023. Available at https://anaesthetists.org/Home/News-opinion/News/Joint-statement-on-NHSEs-plan-to-decommission-desflurane-by-early-2024. Accessed February 21, 2024. [Google Scholar]
- 45.Budd K. Hospitals race to save patients—and the planet. 2019. Available at https://www.aamc.org/news/hospitals-race-save-patients-and-planet. Accessed February 22, 2024. [Google Scholar]
- 46.Percival A. Not so fantastic plastic. 2019. Available at https://nhsproviders.org/news-blogs/blogs/not-so-fantastic-plastic. Accessed February 22, 2024. [Google Scholar]
- 47.Guetter CR, Williams BJ, Slama E, et al. Greening the operating room. Am J Surg. 2018;216:683–688. [DOI] [PubMed] [Google Scholar]
- 48.Yates EF, Bowder AN, Roa L, et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann Surg. 2021;273:1108–1114. [DOI] [PubMed] [Google Scholar]
- 49.Royal College of Surgeons of England. Sustainability in the operating theatre a guide to good practice. 2022. Available at www.rcseng.ac.uk/standardsandguidance. Accessed February 22, 2024. [Google Scholar]
- 50.Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives - the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37:3–19. [DOI] [PubMed] [Google Scholar]
- 51.Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: results from 2 million consecutive cataract surgeries. J Cataract Refract Surg. 2019;45:1226–1233. [DOI] [PubMed] [Google Scholar]
- 52.Drew J, Christie SD, Tyedmers P, et al. Operating in a climate crisis: a state-of-the-science review of life cycle assessment within surgical and anesthetic care. Environ Health Perspect. 2021;129:76001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bhutta MF. Our over-reliance on single-use equipment in the operating theatre is misguided, irrational and harming our planet. Ann R Coll Surg Engl. 2021;103:709–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg (Oakv). 2015;23:235–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bhatter P, Cypen SG, Carter SL, et al. Pharmaceutical and supply waste in oculofacial plastic surgery at a hospital-based outpatient surgery center. Ophthalmic Plast Reconstr Surg. 2021;37:435–438. [DOI] [PubMed] [Google Scholar]
- 56.Bravo D, Thiel C, Bello R, et al. What a waste! The impact of unused surgical supplies in hand surgery and how we can improve. Hand (N Y). 2023;18:1215–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahmed Z, Ioannidi L, Ghali S, et al. A Single-center comparison of unipedicled and bipedicled DIEP flap early outcomes in 98 patients. Plast Reconstr Surg Glob Open. 2023;11:e5089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.