Abstract
Introduction
This study protocol specifies the primary research line and theoretical framework of the 2023 Survey of the Psychology and Behavior of the Chinese Population. It aims to establish a consistent database of Chinese residents' psychological and behavioral surveys through multi‐center and large‐sample cross‐sectional surveys to provide robust data support for developing research in related fields. It will track the public's physical and psychological health more comprehensively and systematically.
Methods
The study was conducted from June 20, 2023 to August 31, 2023, using stratified and quota sampling methods. A total of 150 cities across 800 communities/villages were surveyed, selected from China (Despite extensive coordination, we have been unable to contact our counterparts in the Taiwan region of China to obtain relevant statistical data). The questionnaires were distributed to the public one‐on‐one and face‐to‐face by trained surveyors. The questionnaires included basic information about the individual, personal health status, basic information about the family, the social environment in which the individual lives, psychological condition scales, behavioral level scales, other scales, and attitudes towards topical social issues. Supervisors conducted quality control during the distribution process and returned questionnaires, logically checked and cleaned for data analysis.
Discussion
Data collection has been finished, and scientific outputs based on this data will support the development of health promotion strategies in China and globally. In the aftermath of the pandemic, it will guide policymakers and healthcare organizations to improve their existing policies and services to maximize the physical and mental health of the Chinese population.
Trial Registration
This study was filed in the National Health Security Information Platform (Record No.: MR‐37‐23‐017876) and officially registered in the China Clinical Trials Registry (Registration No.: ChiCTR2300072573).
Keywords: Chinese residents, physical and psychological health, health behavior, cross‐sectional study
Surveyed from June 20 to August 31, 2023, across 150 cities and various urban–rural settings in China, our study employed stratified sampling to gather comprehensive data on Chinese residents' psychology and behavior. Trained surveyors conducted face‐to‐face interviews, covering health, family, social environment, psychological conditions, and behavioral patterns. Quality control ensured robust data for informing health policies and services.
Abbreviation
- PBICR
Psychology and Behavior Investigation of Chinese Residents
1. BACKGROUND
Mental health is an integral and essential component of health. It allows individuals to handle life's stress, realize their potential, learn and work effectively, and contribute to their community [1]. An important implication of this definition is that mental health is more than just the absence of mental disorders or disabilities [2]. Health behaviors encompass both health‐enhancing and health‐impairing actions. The World Mental Health Report 2022 states that approximately 9.7 million people globally suffer from mental disorders [3]. During the first year of the COVID‐19 pandemic, the incidence of anxiety and depression increased by over 25% worldwide [3, 4]. Studies have shown that COVID‐19 infection is significantly linked to higher rates of psychiatric disorders, albeit with modest associations [5]. Among Chinese nationals, the risk of depression was found in 10.6%, and the risk of anxiety in 15.8% [6]. In the initial national survey on psychological distress during the 2020 COVID‐19 outbreak in China, 35% of respondents reported experiencing distress, encompassing anxiety and depression. These findings indicate that the pandemic is a notable stressor for the public, as evidenced by evolving trends in mental disorder prevalence. Health behaviors were defined in 2011 by B. Renner as “Health behaviors belong to the broader category of health‐directed activities. They are aimed at preventing or detecting illnesses at an asymptomatic stage.” [7]. Health behaviors, including diet quality, physical activity, alcohol use, smoking, and sleep, especially sleep, have a significant correlation with mental health [8]. The survey conducted this year also covered some special dimensions of access, such as children's adverse experiences [9]. Since the COVID‐19 pandemic, smoking cessation and quit attempts have risen, sleep disorders have become more prevalent, and overall health behaviors and mental health have been profoundly impacted [10, 11, 12].
Mental health is influenced by a complex interplay of individual, family, community, and structural factors (sociocultural, geopolitical, and environmental), particularly health behaviors. These factors vary over time and space, leading to unique experiences for everyone [3, 13, 14, 15]. Health behaviors and mental health often interact with each other. Physical activity affects the generation of psychological problems [16]. Regular physical activity is associated with better mental health [17]. Besides, social factors, including social activities, influence the generation of psychological problems. Exposure to unfavorable social, economic, geopolitical, and environmental circumstances—including poverty, violence, inequality [18], and environmental deprivation—also increases people's risk of experiencing mental health conditions. Mental health can also directly influence behavior [19]. Due to the interplay between mental health and health behaviors, and their collective impact on physical health, many countries have implemented measures to promote both mental health and health behaviors [20]. For example, the UK has proposed a population‐wide strategy, and Japan has detailed its past efforts and future priorities on its government website [21, 22]. These national mental health strategies rely on representative data, highlighting the need for a high‐quality database of mental health and health behavior surveys.
In Chinese studies, surveys mainly concentrated on common factors like anxiety, depression, social aspects, and lifestyle, with a relatively narrow focus on the study population.
The impact of the pandemic on the mental and behavioral health of global people is significant [23, 24]. A national survey conducted during the COVID‐19 epidemic in 2020 found that 35% of respondents experienced psychological distress, including anxiety and depression [12]; Lu et al., [25] Yu et al. [26], Wu et al. [27], and Liu et al. [28] conducted research studies on depression, anxiety, and their associated factors for older adults in Shenzhen, medical and nonmedical staff during the new coronavirus pneumonia epidemic, hospitalized patients with severe novel coronavirus pneumonia, and hypertensive co‐morbidities in Beijing and Jilin, respectively; Wei et al. [29], He et al. [30], Yang et al. [31], and Sun and Lyu [32] studied social factors, such as residents' sense of social justice, income inequality and social capital, social participation, about physical and mental health; Liang et al. [33], Chen et al. [34], and Jin et al. [35] studied the relationship between behavior and mental health, such as short video use among female college students, unhealthy lifestyles of Chinese psychiatrists, and risky sexual behaviors among Chinese college students, respectively. Cross‐sectional studies in China have typically examined a limited range of variables, overlooking factors such as literacy, family dynamics, and past experiences that influence mental health and established health behaviors. Additionally, prior studies often targeted specific groups, hindering the ability to provide a robust scientific foundation for broad population health promotion efforts.
In summary, there is a recent lack of research on various aspects of public mental and behavioral health in China across multiple groups, which could offer academics and policymakers valuable empirical data and references. The Psychology and Behavior Investigation of Chinese Residents (PBICR) has conducted surveys for three consecutive years [36, 37, 38], with variables updated annually. This year's post‐COVID‐19 survey aimed to create a comprehensive nationwide database for mental and behavioral health research [39, 40]. The database facilitates the exploration of correlations between psychological and behavioral variables across diverse populations, contributing to the enrichment of theoretical and practical research in mental health. Ultimately, this effort supports the advancement of the “Healthy China” strategy [41] on all fronts, and responds to the WHO Comprehensive Action Plan on Mental Health 2013–2030.
2. METHODS
2.1. The study design and setting
This cross‐sectional survey was collaboratively launched by the School of Public Health at Peking University, the Institute of Healthy Yangtze River Delta at Shanghai Jiao Tong University, and Shandong Provincial Hospital. It was conducted from June 20, 2023 to August 31, 2023, with all respondents from China. The study received approval from the Biomedical Ethics Committee of Shandong Provincial Hospital (Grant No.: SWYX: NO.2023‐198) on May 5, 2023. Subsequently, it was filed in the National Health Security Information Platform (Record No.: R‐37‐23‐017876) and officially registered in the China Clinical Trials Registry (Registration No.: ChiCTR2300072573).
2.2. Study participants and data collection
This study is a cross‐sectional study with an unlimited number of subjects, and the final minimum sample size required for this study was determined according to this sample size formula (1).
| (1) |
where the prevalence refers to the results of the meta‐analysis by Krishnamoorthy et al. [42], the prevalence of depression in the general population of China is 24%. The given formula establishes the probability of Type I error (α) as 0.05, while the acceptable error is determined to be 0.02. Consequently, the minimum sample size is computed as 1752. Given that the planned sample size for this study surpasses the minimum requirement, the allocation of sample size for each provincial administrative region is based on the proportion of its respective population.
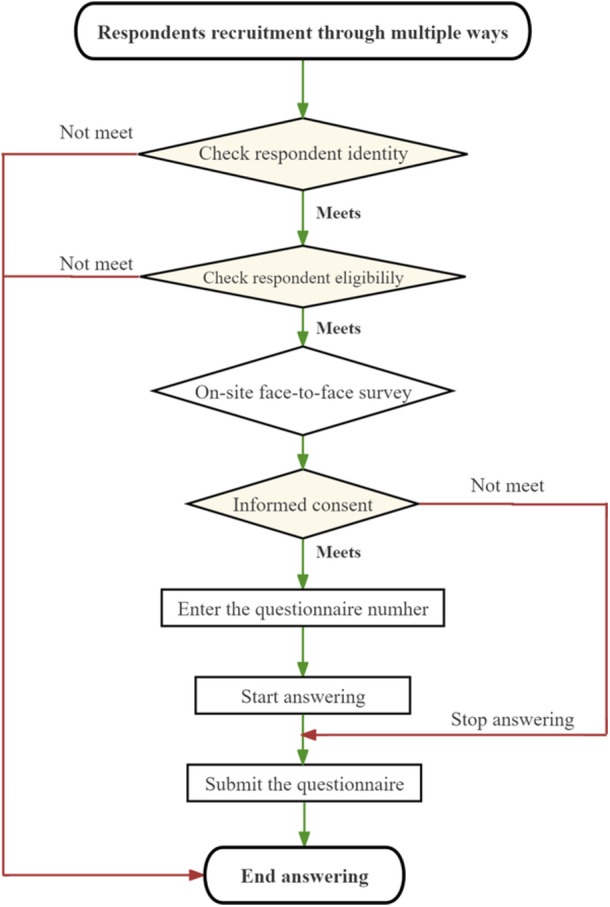
The study was conducted in China, with the sample proportions based on the 7th National Census. Sampling proportions were determined accordingly. From each province/autonomous region/municipality, a minimum of 500/1000/1500/2000/2500/3000 individuals were sampled, expect two special administrative regions, where 200 individuals were sampled each. The total estimated sample size for the study was 40,000 individuals. The sampling process included selection at various administrative levels, such as city, district, county, township, street, and community/village levels. Additionally, sampling was carried out at the individual level, considering both gender and age as quota attributes. The proportion of the sample size expected to be recovered in each provincial administrative region is shown in Figure 1.
Figure 1.
Sampling Process. (1) A total of 150 cities involving 800 communities/villages were sampled for this survey. (2) Equal probability sampling (stratified sampling) at provincial, municipal, district, county, township/township/street, and community/village levels, and non‐equal probability sampling (quota sampling) at the community/village to an individual level. Note: Despite extensive coordination, we have been unable to contact our counterparts in the Taiwan region of China to obtain relevant statistical data.
A multi‐stage sampling approach was adopted for this study. During the initial phase, the research team included capital cities from across China (Despite extensive coordination, we have been unable to contact our counterparts in the Taiwan region of China to obtain relevant statistical data). Additionally, 2–12 cities were selected from each noncapital prefecture within every province and autonomous region, resulting in 150 cities. The number of cities selected in each province is determined by the weight of the population size in that province, with each province including its capital city and the rest of the cities selected by convenience sampling. Moving on to the second stage, of the 150 municipalities sampled, the number of communities to be sampled was determined based on the population base of the first‐level administrative district in which the municipality was located, with a total of 10–60 communities in the ratio of urban (3) to rural (2) communities in the municipalities sampled in each province, for a total of 800 communities. In the third stage, a quota sample of 150 urban residents was drawn, considering the findings of the “7th National Census in 2021” [43]. This sample specifically accounted for attributes such as gender and age. For instance, if a province required 1000 data points, a balanced ratio of men to women at 1:1 would be upheld, entailing 500 men and no fewer than 500 women. Moreover, the urban areas would comprise at least 400 individuals, while the rural areas would include at least 600 individuals.
The survey included Chinese permanent residents who hold citizenship of the People's Republic of China and have an annual departure time of ≤1 month. Eligible participants had to be at least 18 years old (born before August 31, 2005), possess the ability to comprehend each item in the questionnaire, and be capable of independently completing the questionnaire or doing so with the assistance of an investigator. All participants volunteered to participate in the study and were required to provide informed consent by signing a consent form. Exclusions encompassed individuals with confusion, psychiatric abnormalities, or cognitive impairment. Moreover, those who had previously participated in similar studies or expressed a lack of interest in participating in this particular study were also excluded.
2.3. Quality control
The research team implemented quality control measures across six stages in this survey. These stages encompassed questionnaire design, pre‐survey activities, investigator training, questionnaire distribution, logic checking, and data processing. During the questionnaire design stage, the scale design team carefully assessed the logical structure of the questionnaire and diligently identified any evident errors in its design. In the pre‐survey stage, the quality control team conducted three pre‐surveys to identify any issues related to the questionnaire setup. Feedback on these issues was provided and promptly communicated to the scale design group for timely revisions. In the investigator training stage, the training and coordination group ensured the selection of high‐quality provincial leaders and investigators or investigator teams. Through three comprehensive survey trainings, the team enhanced the investigators' understanding of the project and their research skills, guaranteeing that their work adhered to the rigorous standards established by the research team. In the questionnaire distribution stage, provincial leaders and investigators or investigator teams were required to adhere to the survey standards provided by the research team when distributing the questionnaires. Please comply with these standards to avoid exclusion from the pool of qualified questionnaires. During the logic‐checking phase, the research team screened the collected questionnaires once a week and eliminated those that needed to meet the logic‐checking rules set in advance. Lastly, during the data processing stage, upon completion of the survey, the research team diligently checked and cleaned the questionnaire data by stringent quality screening standards.
To ensure the quality control of every aspect of the project, we have set up a complete organizational framework to execute every aspect of the project. The organizational framework of this survey project follows a general manager system, wherein each team is led by an individual who oversees and coordinates their collaborative efforts to complete the survey project. The research team comprises five distinct research groups, namely the expert committee, survey group, training and coordination group, scale design group, and quality control group:
-
(1)
The expert committee comprises invited experts in psychology, behavior, public health, and statistics. Their role is to provide expertize and guidance throughout the project.
-
(2)
The survey group comprises provincial heads, investigator teams, and investigators. Each provincial administrative region is assigned a research team member to supervise operations. The provincial heads assume responsibility for recruiting, training, organizing, and coordinating investigators or investigator teams.
-
(3)
The training and coordination group focuses on investigator training, ethical review submission, study protocol registration, and survey protocol writing.
-
(4)
The scale design group is primarily responsible for screening questionnaire variables, developing original scales, incorporating international scales, simplifying scales, and establishing logic settings for skip questions.
-
(5)
The quality control group is pivotal in expert consultations, pre‐survey activities, ensuring sampling quality, and verifying questionnaire logic. The supervisor responsible for questionnaire distribution and retrieval followed the study throughout.
2.3.1. Questionnaire design phase
The questionnaire design phase commenced with the research team conducting a comprehensive scientific review of relevant literature and scholarly works. To ensure the questionnaire's efficacy, the research team organized online expert consultation and discussion from March to June 2023. Forty‐two experts (all experts hold associate senior titles or above), possessing esteemed credentials in fields such as social medicine, behavioral epidemiology, psychology, health education, health statistics, health service management, humanistic medicine, journalism and communication, clinical medicine, pharmacy, nursing, sociology, and philosophy, were invited to evaluate the quality of the initial draft questionnaire and provide recommendations for revisions. Subsequently, the research team meticulously incorporated the experts' feedback, resulting in a refined version of the questionnaire. To validate its effectiveness, the research team conducted three rounds of pre‐survey research based on the revised questionnaire.
At the early stage of questionnaire design, the relevant workers of the project group retrieved a large number of English literature libraries while referring to the questioning methods of well‐known databases at both domestic and foreign countries to select a large number of scales, and all the scales included in the survey were determined through multiple rounds of expert consultation and voting by forty‐two experts.
2.3.2. Pre‐investigation phase
The pre‐investigation phase of the survey consisted of three rounds conducted during three distinct periods: June 5–June 8, June 10–June 13, and June 15–June 18, 2023. The sampling method employed in the pre‐survey stage was fixed with fixed attributes, consistent with the method employed in the official survey. The pre‐survey sample sizes for the three rounds were 100, 100, and 200, respectively. The research team collected and compiled respondents' feedback and modifications throughout the pre‐survey period. They extensively discussed and revised the questionnaire based on the results of statistical analyses about questionnaire reliability. The revised questionnaire underwent subsequent review by the expert committee and was finalized. It is important to note that the questionnaires collected during the pre‐survey phase were not included in the final study analysis.
2.3.3. Investigators' training process
The research team publicly released the “Announcement on the Recruitment of Provincial Leaders for the National Cross‐Section Survey” online and conducted an initial screening of the received resumes. The primary screening criterion for provincial leaders was relevant survey experience and scientific research background. Subsequently, the research team notified the applicants for an interview, which assessed their scientific research proficiency, managerial competence, communication skills, decision‐making abilities, stress tolerance, and adaptability to language environments. Applicants who pass the interview will be formally appointed as provincial leaders, with at least two leaders assigned per provincial administrative region. The research team conducted intensive training sessions lasting 1–2 h on May 13, May 14, and May 28, 2023, to ensure that the provincial leaders possess comprehensive knowledge and a deep understanding of this survey project. Once the training of provincial leaders is completed, the research team will assist them in recruiting investigators or investigation teams in each provincial administrative region. The provincial leaders will be responsible for organizing investigators' recruitment, screening, and training. Those investigators who pass the training assessment will be assigned specific investigation tasks within their designated areas.
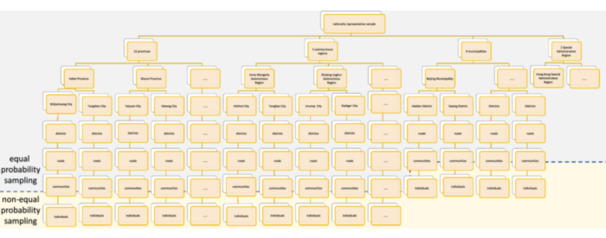
2.3.4. Questionnaire distribution process
The research team adhered to scientific design principles and statistical methodology requirements to ensure rigorous control over the questionnaire distribution process, minimizing potential biases in data collection. The project team asked all investigators to distribute the return questionnaires face‐to‐face. The data collection flow can be visualized in Figure 2 presented below. Initially, the team‐mandated investigators applied a coding system to each questionnaire. The coding principle aimed to facilitate traceability of questionnaires to the corresponding subjects, investigators or investigation teams, and provincial leaders. Questionnaires failing to adhere to the coding rules were deemed invalid. Additionally, before commencing the official survey, provincial leaders reiterated potential challenges to investigators multiple times, aiming to maximize the validity of each collected questionnaire. Subsequently, once the official survey commenced, the research team established weekly communication sessions with provincial leaders via Tencent Meeting, every Sunday at 8:00 p.m. (from June 20, 2023 to August 31, 2023). These sessions encompassed providing feedback on the quality of the week's questionnaires, addressing existing issues, and responding to inquiries from provincial leaders. In case of any problems encountered during the investigation process, provincial leaders were expected to rectify them according to the research team's guidelines. Real‐time discussions were required to propose and deliberate upon potential solutions in the event of disagreements.
Figure 2.
Data collection flow chart.
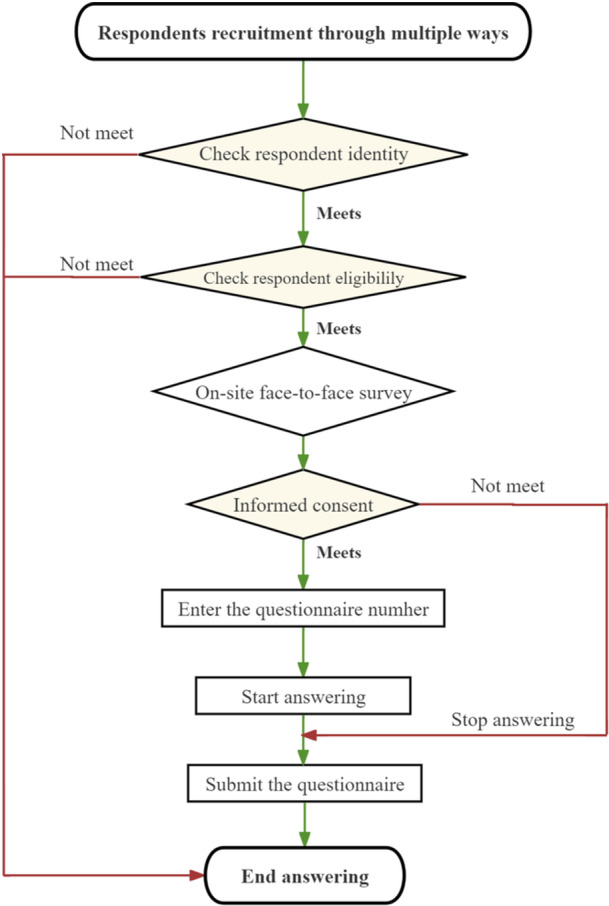
2.3.5. Questionnaire retrieval and analysis process
The research team will establish stringent criteria for screening valid questionnaires before the official survey commencement. Each criterion will undergo logical verification by two investigators consecutively to ensure the accuracy and validity of the assessment. Questionnaires must meet the criteria to be deemed valid. The questionnaire screening criteria include (1) Questionnaires with response times below 600 s. (2) Questionnaires that do not pass the logic check (such as selecting “have religious beliefs” in question 5 or selecting “member of the Communist Party of China,” “Probationary Member of the Communist Party of China,” or “member of the Communist Youth League of China” in question 9; Questionnaires where the selected “highest level of education” in question 11 is higher than the selected “current study period” in question 12; Questionnaires where the “current place of residence” in question 17 matches the “place of birth” in question 21 and etc. (3) Incompletely filled out questionnaire (Questionnaires with more than 20% missing values). (4) Questionnaires that are filled out repeatedly. (5) Questionnaires with the same selected options or regular patterns (straight‐lining participants will be judged to have completed all the scales with the same answers). Additionally, the research team will conduct a statistical analysis of the questionnaires. If any irregular values are identified, the team will trace them back to the original questionnaires or consult with the investigators to verify the information. The study design flow can be visualized in Figures 3 and 4 presented below.
Figure 3.
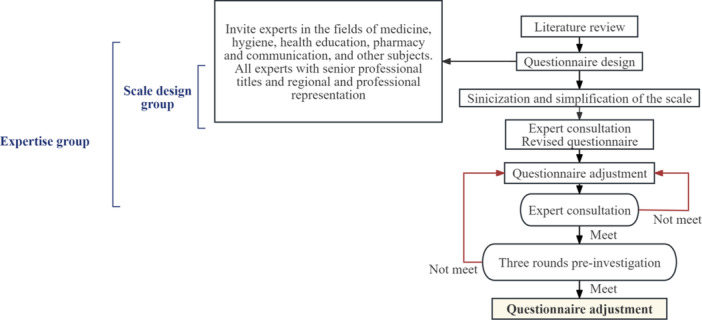
Questionnaire design flowchart.
Figure 4.
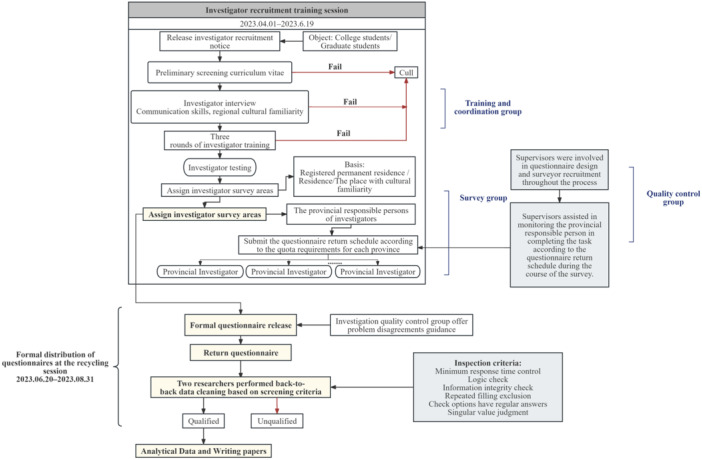
Flow chart of questionnaire collection.
2.4. Measurements
In addition to informed consent and questionnaire numbering, the questionnaire for this study consisted of seven main areas: fundamental personal details, personal health condition, family demographic information, psychological level scales, behavioral level scales, and other scales (they are made up of maturation scales, self‐administered scales, and questionnaires), and attitudes toward socially topical issues. Detailed information of the scales is shown in Table 1.
Table 1.
Scales used for the questionnaire.
| Scale | Abbreviation | Level | Applicable age (years) | Target population | Dimension | Item | Score |
|---|---|---|---|---|---|---|---|
| Adverse Childhood Experiences [44] | ACEs | Other scale | ≥18 | All populations | 7 | 17 | “Yes” or “No”, with a total score can be categorized by binary groups or more groups |
|
Big Five Inventory‐10 Items [45] |
BFI‐10 | Psychological Level Scale | ≥12 | All populations | 5 | 10 |
1–5 (strongly disagree to strongly agree). reverse score: questions 1.3.4.5.7, forward score: questions 2.6.8.9.10 Higher scores indicate higher levels of a given personality trait. |
|
Patient Health Questionnaire‐9 items [46] |
PHQ‐9 | Psychological Level Scale | ≥12 | All populations | 1 | 9 |
0–3 (never to nearly every day) 0–4 no depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderate to severe depression, 20–27 severe depression |
|
Generalized Anxiety Disorder‐7 items [47] |
GAD‐7 | Psychological Level Scale | ≥12 | All populations | 1 | 7 |
0–3 (never to nearly every day) 0–4 no anxiety, 5–9 mild anxiety, 10–13 moderate anxiety, 14–18 moderate anxiety, 19–21 severe anxiety |
|
Perceived Stress Scale‐4 |
PSS‐4 | Psychological Level Scale | ≥12 |
Junior high school or above |
2 | 4 | 0–4 (never to always) with a total score ranging from 0 to 16 points, higher scores indicating more perceived stress. |
|
Perceived Social Support Scale [50] |
PSSS‐SF | Psychological Level Scale | ≥18 | All populations | 1 | 3 | 1–7 (strongly disagree to strongly agree), higher scores indicating greater perception of social support |
|
New General |
NGSES‐SF | Psychological Level Scale | ≥12 | All populations | 1 | 3 | 1–5 (strongly disagree to strongly agree), with a total score ranging from 3 to 15 points, with higher scores indicating greater self‐efficacy |
| Body Image–Acceptance and Action Questionnaire–5 [53] | BI‐AAQ‐5 | Psychological Level Scale | ≥18 | All populations | 1 | 5 | 1–7 (never ture to always ture), the total score range is 5–35 points, higher scores indicate higher levels of body image flexibility. |
| Connor‐Davidson Resilience Scale‐2 [54] | CD‐RISC2 | Psychological Level Scale | ≥18 | All populations | 1 | 2 | 0–4 (not true at all to true nearly all of the time), with a total score ranging from 0 to 8 points, with higher scores indicating greater resilience. |
| General Risk Propensity Scale [55] | GRiPS | Psychological Level Scale | ≥18 | All populations | 1 | 8 | 1–5 (strongly disagree to strongly agree), with a total score ranging from 5 to 40 points, with higher scores indicating a higher propensity to take risks. |
| The Stigma‐9 Questionnaire [56] | STIG‐9 | Psychological Level Scale | ≥18 | All populations | 1 | 9 | 0–3 (disagree to agree), with a total score ranging from 0 to 27 points, with higher scores indicating more stigmatization. |
| Public Service Motivation Scale‐8 items [57] | PSM‐SF | Psychological Level Scale | ≥18 | All populations | 4 | 8 | 1–5 (strongly disagree to strongly agree), with a total score ranging from 5 to 40 points, with higher scores indicating higher public service motivation. |
| Smoking and Alcohol Behavior Questionnaire | Behavior Level Scale | ≥18 |
People over 18 years old |
Self‐developed scale |
11 | ||
| Fagerstrom Test of Nicotine Dependence [58] | FTND | Behavior Level Scale | ≥18 |
People over 18 years old |
Self‐developed scale |
6 | The total scores ranging from 0 to 10, with higher scores indicating higher nicotine dependence. |
|
The International Physical Activity |
IPAQ‐7 | Behavior Level Scale | ≥18 | All populations | 4 | 7 | (1) Walking MET = 3.3 × average daily walking time × weekly walking days. (2) Moderately strong MET = 4.0 × average time engaged in moderate intensity activity per day × days engaged in moderate intensity activity per week. (3) Strenuous activity MET = 8.0 × average time engaged in strenuous activity per day × days engaged in strenuous activity per week. Therefore, basal metabolic time per week (minutes) = (1) + (2) + (3). |
|
Pittsburgh Sleep Quality Index [61] |
B‐PSQI | Behavior Level Scale | ≥18 | All populations | 5 | 6 | Total score ranges from 0 to 15, with higher scores indicating poorer sleep quality |
| Morningness‐Eveningness Questionnaire‐5 items [62] | MEQ‐5 | Other scale | ≥15 | All populations | 1 | 5 |
1–5, with total scores ranging from 4 to 25. 4–7 Definitely Evening, 8–11 Moderately Evening, 12–17 Neutral, 18–21 Moderately Morning, 22–25 Definitely Morning. |
| Community Citizen Behavior Scale‐5 items *1 | CCB‐5 | Behavior Level Scale | ≥18 | All populations | 1 | 5 | 1–5 (strongly disagree to strongly agree), with a total score ranging from 5 to 25 points, with higher scores indicating more community citizenship behavior. |
|
Intimate Relationship Violence Scale *2 |
Behavior Level Scale | ≥12 | All populations |
Self‐developed scale |
6 | 1–5 (never to almost always), the total score range is 5–25 points, scores from 5 to 8 indicate a low level, 9–13 represent a moderate level, and 14–25 correspond to a high level. | |
| Media Use Behavior Scale [63, 64] | Behavior Level Scale | ≥12 | All populations |
Self‐developed questionnaire |
6 | 1–5 (never to always), with a total score ranging from 6 to 30 points, with higher scores indicating more frequent use of media | |
|
Family Communication Scale [65] |
FCS‐4 | Other scale | ≥11 | All populations | 1 | 4 |
1–5 (strongly disagree to strongly agree), with a total score ranging from 4 to 20 points, with higher scores indicating higher levels of family communication |
| Antibiotic Use Behavior and Cognition Questionnaire | Behavior Level Scale | ≥12 | All populations |
Self‐developed scale |
17 | 1–5 (strongly agree to strongly disagree), with a total score ranging from 17 to 85 points. | |
| Simplified Nutritional Appetite Questionnaire [66, 67] | SNAQ | Other scale | ≥18 | All populations | 2 | 4 | 1–5 (from “a” to “e”), with total scores ranging from 4 to 20 points, a total score less than 14 indicates that there is a risk of weight loss of more than 5% or 10% in the next months. |
| Quality of Life Scale [68] | EQ‐5D‐5L | Other scale | ≥18 | All populations | 5 | 5 + EQ‐ VAS | 1–5, with total scores ranging from 5 to 25, with higher scores indicating higher quality of life. Gliding multiple choice questions with EQ‐VAS score of 0–100. |
| the Electronic Health Literacy Scale [69, 70] | eHEALS‐SF | Other scale | ≥18 | All populations | 1 | 5 | 1–5 (strongly disagree to strongly agree), with a total score ranging from 5 to 25 points, with higher scores indicating a higher level of electronic health literacy. |
|
Family Health |
FHS‐SF | Other scale | ≥18 | All populations | 4 | 10 | 1–5 (strongly disagree to strongly agree), with total scores ranging from 10 to 50 points, with higher scores indicating higher levels of family health |
|
Health Literacy Scale‐Short Form‐4 [73] |
HLS‐SF4 | Other scale | ≥12 | All populations | 3 | 4 | 0–3 (very difficult to very easy), with total scores ranging from 0 to 12, with higher scores indicating higher levels of health literacy |
| Doctor‐patient Communication Preferences Questionnaire | Other scale | ≥12 | All populations |
Self‐developed scale |
7 | ||
| Medication Literacy Scale [74] | Other scale | ≥12 | All populations | 6 | 1–5 (always ture to never ture), with total scores ranging from 6 to 30 points. |
Abbreviations: CFI, Comparative Fit Index; GFI, Goodness‐of‐Fit Index; RMSEA, Root Mean Square Error of Approximation; TLI, Tucker–Lewis Index.
1. Community Citizen Behavior Scale‐5 items: The Cronbach's alpha (α) for internal consistency was 0.744. The Kaiser‐Meyer‐Olkin measure of sampling adequacy was 0.830. The Bartlett's test of sphericity was significant (p < 0.01), with a chi‐square value of χ² = 599.756467, and df = 21.
2. Intimate Relationship Violence Scale: Cronbach's α of 0.948 and a split‐half reliability of 0.914 (both > 0.800). Factor analysis of the 5 items yielded a KMO value of 0.900 and Bartlett's test of sphericity was significant (p < 0.001). One factor was extracted via principal axis factoring, explaining 83.227% of the variance (greater than 40%). All item loadings on this factor ranged from 0.862 to 0.926, aligning with the unidimensional construct. Model fit indices confirmed good validity (χ²/df = 1.61, GFI = 0.88, CFI = 0.95, RMSEA = 0.05, TLI = 0.99). The average variance extracted was 0.832 (>0.5), and composite reliability was 0.961 (>0.7). The optimal cut‐off points based on the Youden Index are 8.5 and 13.5, classifying the categories.
2.4.1. Personal demographic details
This section encompasses 23 inquiries regarding various aspects, including gender, ethnicity, religion, height, weight, waistline, political status, occupation, and occupational status, the highest level of education attained, academic background (in terms of schooling, college, and major), migration details (birthplace, current residence, length of residency, and place and time of migration), and preferred hand.
2.4.2. Personal health condition
This section comprises 10 questions about chronic disease diagnoses, classification of hypertension, complications associated with hypertension, types of diabetes mellitus, respiratory disease classification, urinary disease classification, digestive disease classification, tumor types, status of injury events, and experiences of life events.
2.4.3. Family demographic information
This section includes 21 questions addressing permanent residence, household registration, marital status, family type, romantic relationship status, living arrangements (whether living alone, with a spouse, with spouse's parents, or with parents), number of children, living situation with children, age of youngest and oldest child, number of siblings, living situation with siblings, residential area, number of residential properties, debt status, monthly per capita household income, and methods of medical expense coverage.
3. DISCUSSION
The primary objective of this study is to offer an all‐encompassing and methodical comprehension of the Chinese populace's present mental health and health behaviors. This will be achieved through a cross‐sectional survey conducted across multiple centers, utilizing a large sample size. The study aims to furnish robust data support for research endeavors in diverse health‐related domains within China. It is necessary to conduct a nationwide survey on the mental health status and health behaviors of the population in promptly after the end of the COVID‐19 pandemic, which will help us to understand the alterations that the pandemic has brought about in the mental health of the Chinese population as well as in their health behaviors. The survey will also help experts and scholars produce more appropriate research results and provide more timely guidance for health care after a pandemic to promote Chinese residents' health. The survey encompasses a comprehensive range of factors, including physical health status, the influence of diseases on the personal life and work, basic family situation, access to medical care, and participation in public service behaviors.
Additionally, the questionnaire assesses residents' mental health status, perceived stress capacity, and psychological resilience. It also gathers information on residents' medication usage, activity levels, dietary habits, sleep patterns, and interpersonal interactions. Furthermore, the survey examines self‐rated health status, health literacy, family communication, and childhood experiences. The questionnaire design employed in this study exhibits a comprehensive coverage and breadth of the survey, enabling a thorough examination of our residents' mental health status and health behaviors.
Alterations in the broader sociocultural milieu can induce modifications in the mental well‐being of individuals, particularly among adults, after the cessation of the COVID‐19 pandemic [75]. Depression and anxiety, as an essential assessment of mental health, were included in this investigation and the study by Zhu et al. [76] suggested a significant change in the prevalence of depression and anxiety among the respondents during the blockade period, so it was necessary to investigate the depression and anxiety status of the respondents after the full unblocking in this study. In addition, this study also focuses on the psychological resilience of the individual. The results of this study suggest that having good psychological resilience will reduce adverse effects on psychological well‐being when negative external events occur [77]. Based on the above, in the individual dimension, this study also included the measure of individual's perception of stress, the measure of the individual's social support, the measure of an individual's self‐efficacy, the individual's perception of body image, and the individual's tendency to take external risks. As for the social dimension, this study measured public attitudes towards people with mental disorders and citizens' motivation to participate in public services. This study aims to comprehensively explore the mental health status of the Chinese population more comprehensively by measuring of more mental status variables.
The correlation between individual health‐related literacy and the preservation of physical and mental well‐being becomes notably pronounced during significant social occurrences [78]. The prevalence of electronic devices and the widespread adoption of electronic screen usage patterns among individuals have underscored the significance of e‐health literacy as a crucial determinant of personal health. Research has consistently demonstrated a positive association between e‐Health literacy and health‐related behaviors, with e‐health literacy as a potential intermediary in the pathway from health‐related information to changes in health‐related behaviors [79]. Adverse childhood experiences significantly impact the emergence of mental health issues in adulthood, with the deleterious consequences of such experiences being transmitted intergenerationally within the family unit via maternal channels [80]. A high level of drug literacy is fundamental during a pandemic when many residents increase their self‐medication behaviors due to lockdowns or the inaccessibility of health services. In a survey of hypertensive older adults, medication‐related health literacy was shown to affect long‐term safe adherence to medication for people with chronic conditions [81].
An individual's health behaviors, both within their family and social environment, exert significant influence on their physical and mental well‐being. Despite focusing on conventional health behaviors such as smoking, alcohol consumption, and diet, this study also looks at health‐related behaviors that are gaining attention among scholars, such as individuals' participation in unpaid household chores, public service, and participation in the arts. According to the research conducted by Ervin et al. [82], there is evidence to suggest that prolonged engagement in unpaid domestic work within the household harms individuals' mental well‐being. Furthermore, the allocation of unpaid domestic responsibilities between genders within the household also subtly influences the mental health of both partners involved. A study conducted amidst the COVID‐19 pandemic indicates that the engagement of medical patients in social volunteering has the potential to foster a more favorable psychological state [83]. In a similar vein, consistent involvement in social volunteering has been found to have a favorable influence on cognitive abilities. In contrast, substantial social engagement acts as a protective factor against amygdala deterioration, thereby safeguarding emotionally significant memories and mitigating the likelihood of developing dementia [84]. Studies conducted in the United States and Colombia suggest that participation in the arts can lead to a reduction in the prevalence of depression and anxiety and an increase in the health and well‐being of individuals [85, 86].
This study employed a meticulous questionnaire design and conducted an on‐site survey to establish the inaugural survey database on Chinese residents' mental health and health behaviors in the aftermath of the COVID‐19 pandemic. The findings from this database will provide valuable guidance to policymakers and healthcare institutions in formulating more targeted policy recommendations to enhance the physical and mental well‐being of Chinese residents post‐pandemic. In 2021 and 2022, a cross‐sectional study was conducted to investigate the psychology and behavior factors of Chinese residents, resulting in significant research findings [87, 88, 89]. It is anticipated that the forthcoming study in 2023 will further contribute to the well‐being of the Chinese population and global health, as well as advance research in the health field. The release of research protocols improves the transparency of research. It informs the scientific community of what research is being done, which helps to avoid duplication and better coordinate research efforts.
AUTHOR CONTRIBUTIONS
Diyue Liu: Data curation (lead); formal analysis (lead); project administration (lead); supervision (lead); visualization (lead); writing—original draft (lead); writing—review and editing (lead). Siyuan Fan: Data curation (lead); formal analysis (lead); investigation (lead); project administration (lead); supervision (lead); visualization (lead); writing—original draft (lead); writing—review and editing (lead). Xincheng Huang: Investigation (equal); supervision (equal); writing—original draft (equal). Wenjing Gu: Resources (equal); writing—original draft (supporting). Yifan Yin: Data curation (lead); investigation (lead). Ziyi Zhang: Investigation (equal); writing—review and editing (supporting). Baotong Ma: Investigation (equal). Ruitong Xia: Investigation (equal). Yuanwei Lu: Investigation (equal). Jingwen Liu: Investigation (equal). Hanjia Xin: Investigation (equal). Yumeng Cao: Investigation (equal). Saier Yang: Investigation (equal). Runqing Li: Investigation (equal). Han Li: Investigation (equal). Ji Zhao: Investigation (equal). Jin Zhang: Investigation (equal). Zheng Gao: Investigation (equal). Yaxin Zeng: Investigation (equal). Yixiao Ding: Investigation (equal). Zhuolun Ren: Investigation (equal). Yan Guan: Investigation (equal). Na Zhang: Investigation (equal). Jia Li: Investigation (equal). Yan Ma: Investigation (equal). Pei Wei: Investigation (equal). Jingjing Dong: Investigation (equal). Yajing Zhou: Investigation (equal). Yong Dong: Investigation (equal). Yan Qian: Investigation (equal). Chen Chen: Investigation (equal). Yujie Zhao: Investigation (equal). Yimiao Li: Investigation (equal). Yujia Zheng: Investigation (equal). Rongyi Chen: Investigation (equal). Xiaomeng Li: Investigation (equal). Yuke Han: Investigation (equal). Yaoyao Xia: Investigation (equal). Huixin Xu: Investigation (equal). Zhaolin Wu: Investigation (equal). Mingyou Wu: Investigation (equal). Xinrui Wu: Investigation (equal). Junyi Hou: Investigation (equal). Yuelai Cai: Investigation (equal). Xiaofan Dai: Investigation (equal). Wenbo Li: Investigation (equal). Ting Nie: Investigation (equal). Chongzhe Zhang: Investigation (equal). Xiaoya Wang: Investigation (equal). Dan Li: Investigation (equal). Siyao Yan: Investigation (equal). Zhiheng Yi: Investigation (Equal). Chenxi Liu: Writing—review and editing (supporting). Xinyue Zhang: Writing—review and editing (supporting). Lei Shi: Writing—review and editing (supporting). Haomiao Li: Writing—review and editing (supporting). Feng Jiang: Writing—review and editing (supporting). Xiaoming Zhou: Writing—review and editing (supporting). Xinying Sun: Resources (lead); supervision (lead); writing—review and editing (lead). Yibo Wu: Conceptualization (lead); data curation (lead); funding acquisition (lead); methodology (lead); resources (lead); supervision (lead); writing—review and editing (lead).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
This study (SWYX: NO.2023‐198) has been approved by the Ethics Research Committee of Shandong Provincial Hospital. This study was filed in the National Health Security Information Platform (Record No.: MR‐37‐23‐017876) and officially registered in the China Clinical Trials Registry (Registration No.: ChiCTR2300072573).
INFORMED CONSENT
The cover page of the questionnaire will explicitly outline the study's objectives and ensure the preservation of anonymity, confidentiality, and the participants' right to decline participation. Informed consent has been duly acquired from all individuals involved in the study.
ACKNOWLEDGMENTS
None.
Liu D, Fan S, Huang X, Gu W, Yin Y, Zhang Z, et al. Study protocol: a national cross‐sectional study on psychology and behavior investigation of Chinese residents in 2023. Health Care Sci. 2024;3:475–492. 10.1002/hcs2.125
Diyue Liu and Siyuan Fan contributed equally to this study and share the co‐first authorship.
Contributor Information
Xinying Sun, Email: xysun@bjmu.edu.cn.
Yibo Wu, Email: bjmuwuyibo@outlook.com.
DATA AVAILABILITY STATEMENT
The PBICR project has been ongoing from 2020 to the present, with an annual multi‐center extensive sample size transect survey. We usually distinguish between different years of surveys by the suffix (e.g., PBICR2023 denotes surveys conducted by PBICR in 2023). The historical materials and any associated protocols supporting this study's findings are available from the corresponding authors upon request (Email: bjmuwuyibo@outlook.com).
REFERENCES
- 1. World Health Organization . Mental health[Internet]. 2022. [cited 2023 Sept 8]. World Health Organization. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
- 2. World Health Organization . Health and Well‐Being[Internet]. 2023. [cited 2023 Sept 8]. World Health Organization. Available from: https://www.who.int/data/gho/data/major-themes/health-and-well-being
- 3. World Health Organization . World mental health report: Transforming mental health for all[Internet]. 2022. [cited 2024 July 15]. World Health Organization. Available from: https://www.who.int/publications/i/item/9789240049338
- 4. Najafipour H, Shahrokhabadi MS, Banivaheb G, Sabahi A, Shadkam M, Mirzazadeh A. Trends in the prevalence and incidence of anxiety and depressive symptoms in Iran: findings from KERCADRS. Family Med Commun Health. 2021;9(3):e000937. 10.1136/fmch-2021-000937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weich S. Mental health after COVID‐19. BMJ. 2022;376:o326. 10.1136/bmj.o326 [DOI] [PubMed] [Google Scholar]
- 6. Shen C. 2022. edition of the Blue Book of Mental Health released in Chinese— Chinese Academy of Sciences. Chinese Science Daily [Internet]. 2023 [cited 2023 Sept 8]. Chinese academy of science. Available from: https://www.cas.cn/cm/202302/t20230227_4875996.shtml
- 7. James D. International Encyclopedia of the Social & Behavioral Sciences. ScienceDirect [Internet]. 2015. [cited 2024 Jan 29]. ScienceDirect. Available from: http://www.sciencedirect.com:5070/referencework/9780080970875/international-encyclopedia-of-the-social-and-behavioral-sciences
- 8. Oftedal S, Kolt GS, Holliday EG, Stamatakis E, Vandelanotte C, Brown WJ, et al. Associations of health‐behavior patterns, mental health and self‐rated health. Prev Med. 2019;118:295–303. 10.1016/j.ypmed.2018.11.017 [DOI] [PubMed] [Google Scholar]
- 9. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med. 1998;14(4):245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 10. Sorokin M, Markin K, Kibitov A, Palchikova E, Zubova E. The mind‐body problem in the context of neuropsychiatric symptoms in patients with coronavirus disease 2019. Alpha Psychiatry. 2024;24(6):257–260. 10.5152/alphapsychiatry.2023.231178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McBride E, Arden MA, Chater A, Chilcot J. The impact of COVID‐19 on health behaviour, well‐being, and long‐term physical health. Br J Health Psychol. 2021;26(2):259–270. 10.1111/bjhp.12520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lancet T . Mental health after China's prolonged lockdowns. Lancet. 2022;399(10342):2167. 10.1016/S0140-6736(22)01051-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xu Z, Zhu C. Effect of adverse childhood experiences, parenting styles, and family accommodation on patients diagnosed with obsessive‐compulsive disorder. Alpha Psychiatry. 2024;24(6):261–269. 10.5152/alphapsychiatry.2023.231247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Na H, Lee C, Jung YE. Effect of childhood adversity and positive psychological resources on stress response‐comparison between depressed and nondepressed young adults. Alpha Psychiatry. 2023;24(3):79–84. 10.5152/alphapsychiatry.2023.221055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shaw P, Blizzard S, Shastri G, Kundzicz P, Curtis B, Ungar L, et al. A daily diary study into the effects on mental health of COVID‐19 pandemic‐related behaviors. Psychol Med. 2021;53(2):1–9. 10.1017/S0033291721001896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mukhtar S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int J Soc Psychiatry. 2020;66(5):512–516. 10.1177/0020764020925835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stubbs B, Vancampfort D, Smith L, Rosenbaum S, Schuch F, Firth J. Physical activity and mental health. Lancet Psychiatry. 2018;5(11):873. 10.1016/S2215-0366(18)30343-2 [DOI] [PubMed] [Google Scholar]
- 18. d'Elia A, Gabbay M, Rodgers S, Kierans C, Jones E, Durrani I, et al. Artificial intelligence and health inequities in primary care: a systematic scoping review and framework. Family Med Commun Health. 2022;10(Suppl 1):e001670. 10.1136/fmch-2022-001670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kunzler AM, Helmreich I, König J, Chmitorz A, Wessa M, Binder H, et al. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst Rev. 2020;2020(7):CD013684. 10.1002/14651858.CD013684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Aoki T, Yamamoto Y, Shimizu S, Fukuhara S. Physical multimorbidity patterns and depressive symptoms: a nationwide cross‐sectional study in Japan. Family Med Commun Health. 2020;8(1):e000234. 10.1136/fmch-2019-000234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Japan Health Policy NOW . Mental Health [Internet]. 2021. [cited 2023 Sept 8]. Japan Health Policy NOW. Available from: https://japanhpn.org/en/mental-health-1/
- 22. Department of Health and Social Care . The mental health strategy for England ‐ GOV.UK. [Internet]. 2011. [cited 2023 Sept 8]. Department of Health and Social Care. Available from: https://www.gov.uk/government/publications/the-mental-health-strategy-for-england
- 23. Zhai Y, Du X. Differential effectiveness of COVID‐19 health behaviors: the role of mental health conditions in mask‐wearing, social distancing, and hygiene practice. Health Care Sci. 2023;2(4):286–290. 10.1002/hcs2.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rao S, Dimitropoulos G, Williams JVA, Sharifi V, Fahim M, Munir A, et al. Associations between negative COVID‐19 experiences and symptoms of anxiety and depression: a study based on a representative Canadian national sample. Health Promot Chronic Dis Prev Can. 2024;44(2):56–65. 10.24095/hpcdp.44.2.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lu C, Guan T, Yang J, Zhamg D, Lin X. Residence patterns, level of community service and depressive symptoms of old adults in shenzhen (in Chinese). Sci Res Aging. 2022;10(5):44–57. [Google Scholar]
- 26. Yu L, Xu Y, Li W, Gao X, Wang X. Anxiety and depression in medical and non‐medical staff during the COVID‐19 epidemic (in Chinese). Chin Mental Health J. 2022;36(5):451–456. 10.3969/j.issn.1000-6729.2022.05.016 [DOI] [Google Scholar]
- 27. Wu Y, Peng Y. Investigation on the status of anxiety and depression in hospitalized patients with severe coronavirus disease 2019 (in Chinese). Chin J Nurs. 2020;55(S1):606–607. [Google Scholar]
- 28. Liu C, Yu Y, Kang L, Wu Y, Liao J, Wang S, et al. The prevalence of hypertension comorbid of depression and anxiety disorder in Beijing and Jilin: an analysis of risk factors (in Chinese). Chin J Psychiatry. 2015;48(2):86–91. 10.3760/cma.j.issn.1006-7884.2015.02.008 [DOI] [Google Scholar]
- 29. Wei C, Li Q, Luo Y, Xiang G, Lian Z, Chen H. The relationship between perceived societal fairness and depression among residents: a cross‐lagged analysis (in Chinese). Chin J Clin Psychol. 2023;31(2):426–431. 10.16128/j.cnki.1005-3611.2023.02.034 [DOI] [Google Scholar]
- 30. He Y, Zhou L, Li J, Wu J. An empirical analysis of the impact of income inequality and social capital on physical and mental health—take China's micro‐database analysis as an example. Int J Equity Health. 2021;20(1):241. 10.1186/s12939-021-01560-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yang H, Hagedorn A, Zhu H, Chen H. Mental health and well‐being in older women in China: implications from the Andersen model. BMC Geriatr. 2020;20(1):254. 10.1186/s12877-020-01639-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sun J, Lyu S. Social participation and urban‐rural disparity in mental health among older adults in China. J Affect Disord. 2020;274:399–404. 10.1016/j.jad.2020.05.091 [DOI] [PubMed] [Google Scholar]
- 33. Liang X, Guo X, Zhao T. The impact of short‐video use on depression of female undergraduate: a chain mediating model of self objectification and body satisfaction [J/OL]. J Psychol Sci. 2020;43(5):1220–1226. [Google Scholar]
- 34. Chen Y, Wang P, He Y, Jiang F, Liu H, Liu Y, et al. Gender differences in the association between lifestyle behaviors and mental health among psychiatrists in China. J Affect Disord. 2022;318:196–203. 10.1016/j.jad.2022.08.089 [DOI] [PubMed] [Google Scholar]
- 35. Jin Z, Cao W, Wang K, Meng X, Shen J, Guo Y, et al. Mental health and risky sexual behaviors among Chinese college students: a large cross‐sectional study. J Affect Disord. 2021;287:293–300. 10.1016/j.jad.2021.03.067 [DOI] [PubMed] [Google Scholar]
- 36. Chinese Family News . 2021. China Family Health Index Survey General Report (in Chinese) [Internet]. 2021 [cited 2023 Sept 9]. Chinese Family News. Available from: https://cfnews.org.cn/newsinfo/2685237.html
- 37. Qiao Y. Chinese People's Health Status Report 2020 (in Chinese). [Internet]. 2021. [cited 2023 Sept 8]. People.cn. Available from: http://health.people.com.cn/n1/2021/0105/c14739-31989769.html
- 38. Wang Y, Kaierdebieke A, Fan S, Zhang R, Huang M, Li H, et al. Study protocol: a cross‐sectional study on psychology and behavior investigation of Chinese residents, PBICR. Psychosomatic Med Res. 2022;4(3):19. 10.53388/202219 [DOI] [Google Scholar]
- 39. Wu Y, Fan S, Liu D, Sun X. Psychological and behavior investigation of Chinese residents: concepts, practices, and prospects. Chin Gen Pract J. 2024;1(3):149–156. 10.1016/j.cgpj.2024.07.006 [DOI] [Google Scholar]
- 40. Yang Y, Fan S, Chen W, Wu Y. Broader open data needed in psychiatry: practice from the psychology and behavior investigation of Chinese residents. Alpha Psychiatry. 2024;25(4):564–565. 10.5152/alphapsychiatry.2024.241804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang W, Zakus D. Healthy China 2030: “Without national health, there will be no comprehensive well‐being”. Family Medicine and Community Health. 2016;4(4):75–76. 10.15212/fmch.2016.0126 [DOI] [Google Scholar]
- 42. Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID‐19 patients amidst the COVID‐19 pandemic: a systematic review and meta‐analysis. Psychiatry Res. 2020;293:113382. 10.1016/j.psychres.2020.113382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chen Y. Bulletin of the seventh National Census__China government network (in Chinese). [Internet]. [cited 2024 Nov 12]. Available from: https://www.gov.cn/guoqing/2021-05/13/content_5606149.htm
- 44.World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE‐IQ). [Internet]. 2020 [cited 2024 Oct 8]. World Health Organization. Available from: https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq)
- 45. Carciofo R, Yang J, Song N, Du F, Zhang K. Psychometric evaluation of Chinese‐language 44‐item and 10‐item big five personality inventories, including correlations with chronotype, mindfulness and mind wandering. PLoS One. 2016;11(2):e0149963. 10.1371/journal.pone.0149963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ‐9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–544. 10.1016/j.genhosppsych.2014.05.021 [DOI] [PubMed] [Google Scholar]
- 47. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med. 2006;166(10):1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 48. Ingram PB, Clarke E, Lichtenberg JW. Confirmatory factor analysis of the perceived stress scale‐4 in a community sample. Stress and Health. 2016;32(2):173–176. 10.1002/smi.2592 [DOI] [PubMed] [Google Scholar]
- 49. She Z, Li D, Zhang W, Zhou N, Xi J, Ju K. Three versions of the perceived stress scale: psychometric evaluation in a nationally representative sample of Chinese adults during the COVID‐19 pandemic. Int J Environ Res Public Health. 2021;18(16):8312. 10.3390/ijerph18168312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wu Y, Tang J, Du Z, Chen K, Wang F, Sun X, et al. Development of a Short Version of the Perceived Social Support Scale: Based on Classical Test Theory and Item Response Theory [Internet]. PsyArXiv; 2022. 10.31234/osf.io/d95zg [DOI]
- 51. Chen G, Gully SM, Eden D. Validation of a new general self‐efficacy scale. Org Res Methods. 2001;4(1):62–83. 10.1177/109442810141004 [DOI] [Google Scholar]
- 52. Wang F, Chen K, Du Z, Wu Y, Tang J, Sun X, et al. Reliability and validity analysis and Mokken model of New General Self‐Efficacy Scale‐Short Form (NGSES‐SF) [Internet]. PsyArXiv; 2022. 10.31234/osf.io/r7aj3 [DOI]
- 53. Basarkod G, Sahdra B, Ciarrochi J. Body image‐acceptance and action questionnaire‐5: an abbreviation using genetic algorithms. Behav Ther. 2018;49(3):388–402. 10.1016/j.beth.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 54. Vaishnavi S, Connor K, Davidson JRT. An abbreviated version of the Connor‐Davidson resilience scale (CD‐RISC), the CD‐RISC2:psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007;152(2–3):293–297. 10.1016/j.psychres.2007.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhang DC, Highhouse S, Nye CD. Development and validation of the general risk propensity scale (GRiPS). J Behav Decision Making. 2019;32(2):152–167. 10.1002/bdm.2102 [DOI] [Google Scholar]
- 56. Gierk B, Löwe B, Murray AM, Kohlmann S. Assessment of perceived mental health‐related stigma: the stigma‐9 questionnaire (STIG‐9). Psychiatry Res. 2018;270:822–830. 10.1016/j.psychres.2018.10.026 [DOI] [PubMed] [Google Scholar]
- 57. Song H, Fan S, Han Q, Jiang F, Wu Y. A Concise and Widely Applicable Tool for Measuring Motivation in Public Services, China (2024). https://osf.io/h7px8. Accessed October 15, 2024.
- 58. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The fagerström test for nicotine dependence: a revision of the fagerstrom tolerance questionnaire. Br J Addict. 1991;86(9):1119–1127. 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- 59. Aadahl M, Jørgensen T. Validation of a new self‐report instrument for measuring physical activity. Med Sci Sports Exercise. 2003;35(7):1196–1202. 10.1249/01.mss.0000074446.02192.14 [DOI] [PubMed] [Google Scholar]
- 60. Qu NN, Li KJ. [Study on the reliability and validity of international physical activity questionnaire (Chinese Vision, IPAQ)]. Chin J Epidemiol. 2004;25(3):265–268. [PubMed] [Google Scholar]
- 61. Sancho‐Domingo C, Carballo JL, Coloma‐Carmona A, Buysse DJ. Brief version of the Pittsburgh Sleep Quality Index (B‐PSQI) and measurement invariance across gender and age in a population‐based sample. Psychol Assess. 2021;33(2):111–121. 10.1037/pas0000959 [DOI] [PubMed] [Google Scholar]
- 62. Adan A, Almirall H. Horne & östberg morningness‐eveningness questionnaire: a reduced scale. Pers Individ Differ. 1991;12(3):241–253. 10.1016/0191-8869(91)90110-W [DOI] [Google Scholar]
- 63. Li W, Cho H. The knowledge gap on social media: examining roles of engagement and networks. New Media Soc. 2023;25(5):1023–1042. 10.1177/14614448211009488 [DOI] [Google Scholar]
- 64. Khan ML. Social media engagement: what motivates user participation and consumption on YouTube? Comput Human Behav. 2017;66:236–247. 10.1016/j.chb.2016.09.024 [DOI] [Google Scholar]
- 65. Fan S, Li Y, Hou R, Wenjing G, Han Q, Wu Y. Development and validation of a short form of the Family Communication Scale. 2024. 10.31219/osf.io/d2tjb [DOI]
- 66. Wang Y, Ye S, Chen L, Tang L, Fan D. Loss of appetite in patients with amyotrophic lateral sclerosis is associated with weight loss and anxiety/depression. Sci Rep. 2021;11(1):9119. 10.1038/s41598-021-88755-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lau S, Pek K, Chew J, Lim JP, Ismail NH, Ding YY, et al. The simplified nutritional appetite questionnaire (SNAQ) as a screening tool for risk of malnutrition: optimal cutoff, factor structure, and validation in healthy community‐dwelling older adults. Nutrients. 2020;12(9):2885. 10.3390/nu12092885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five‐level version of EQ‐5D (EQ‐5D‐5L). Qual Life Res. 2011;20(10):1727–1736. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tian H, Chen J. The relationship between the eHealth literacy and computer skills of university students. Educ Inf Technol. 2023;28(8):10691–10707. 10.1007/s10639-023-11610-1 [DOI] [Google Scholar]
- 70. Ma Z, Wu M. The psychometric properties of the Chinese eHealth literacy scale (C‐eHEALS) in a Chinese rural population: cross‐sectional validation study. J Med Internet Res. 2019;21(10):e15720. 10.2196/15720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Crandall A, Weiss‐Laxer NS, Broadbent E, Holmes EK, Magnusson BM, Okano L, et al. The family health scale: reliability and validity of a short‐ and long‐form. Front Public Health. 2020;8:587125. 10.3389/fpubh.2020.587125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Wang F, Wu Y, Sun X, Wang D, Ming WK, Sun X, et al. Reliability and validity of the Chinese version of a short form of the family health scale. BMC Primary Care. 2022;23(1):108. 10.1186/s12875-022-01702-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Sun XN, Chen K, Wu YC, Tang JQ, Wang F, Sun XY, et al. Development of a short version of the health literacy scale based on classical test theory and item response theory (in Chinese). Chin Gen Pract. 2024;27(23):2931–2940. 10.12114/j.issn.1007-9572.2023.0072 [DOI] [Google Scholar]
- 74. Zhenzhen C, Jiabao R, Tingyu D, Ke C, Ruyi H, Yimiao L, et al. Development and validation of a short form of the medication literacy scale for Chinese College Students. 2024. http://arxiv.org/abs/2405.02853
- 75. Meaklim H, Junge MF, Varma P, Finck WA, Jackson ML. Pre‐existing and post‐pandemic insomnia symptoms are associated with high levels of stress, anxiety, and depression globally during the COVID‐19 pandemic. J Clin Sleep Med. 2021;17(10):2085–2097. 10.5664/jcsm.9354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zhu C, Zhang T, Li Q, Chen X, Wang K. Depression and anxiety during the COVID‐19 pandemic: epidemiology, mechanism, and treatment. Neurosci Bull. 2023;39(4):675–684. 10.1007/s12264-022-00970-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Blanc J, Briggs AQ, Seixas AA, Reid M, Jean‐Louis G, Pandi‐Perumal SR. Addressing psychological resilience during the coronavirus disease 2019 pandemic: a rapid review. Curr Opin Psychiatry. 2021;34(1):29–35. 10.1097/YCO.0000000000000665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Cudjoe J, Delva S, Cajita M, Han HR. Empirically tested health literacy frameworks. HLRP: Health Literacy Res Pract. 2020;4(1):e22–e44. 10.3928/24748307-20191025-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kim K, Shin S, Kim S, Lee E. The relation between eHealth literacy and health‐related behaviors: systematic review and meta‐analysis. J Med Internet Res. 2023;25:e40778. 10.2196/40778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kang NR, Kwack YS, Song JK, Kim MD, Park JH, Kim BN, et al. The impact of maternal adverse childhood experiences on offspring's internalizing and externalizing problems. Psychiatry Investig. 2021;18(11):1050–1057. 10.30773/pi.2021.0343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Shi S, Shen Z, Duan Y, Ding S, Zhong Z. Association between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. 2019;10:822. 10.3389/fphar.2019.00822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ervin J, Taouk Y, Hewitt B, King T. The association between unpaid labour and mental health in working‐age adults in Australia from 2002 to 2020: a longitudinal population‐based cohort study. Lancet Public Health. 2023;8(4):e276–e285. 10.1016/S2468-2667(23)00030-0 [DOI] [PubMed] [Google Scholar]
- 83. Phillips HE, Jennings RB, Outhwaite IR, Grosser S, Chandra M, Ende V, et al. Motivation to impact: medical student volunteerism in the COVID‐19 pandemic. Med Sci Educ. 2022;32(5):1149–1157. 10.1007/s40670-022-01639-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Carlson M. Social volunteering in aging adults increases regions of the amygdala and correlates with enhanced generativity. Innovation in Aging. 2020;4(Suppl 1):795. 10.1093/geroni/igaa057.2881 [DOI] [Google Scholar]
- 85. Bone JK, Bu F, Fluharty ME, Paul E, Sonke JK, Fancourt D. Who engages in the arts in the United States? A comparison of several types of engagement using data from The General Social Survey. BMC Public Health. 2021;21(1):1349. 10.1186/s12889-021-11263-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gómez‐Restrepo C, Casasbuenas NG, Ortiz‐Hernández N, Bird VJ, Acosta MPJ, Restrepo JMU, et al. Role of the arts in the life and mental health of young people that participate in artistic organizations in Colombia: a qualitative study. BMC Psychiatry. 2022;22(1):757. 10.1186/s12888-022-04396-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Wang X, Wu Y, Meng Z, Li J, Xu L, Sun X, et al. Willingness to use mobile health devices in the post‐COVID‐19 era: nationwide cross‐sectional study in China. J Med Internet Res. 2023;25:e44225. 10.2196/44225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Li H, Wu Y, Bai Z, Xu X, Su D, Chen J, et al. The association between family health and frailty with the mediation role of health literacy and health behavior among older adults in China: nationwide cross‐sectional study. JMIR Public Health Surveill. 2023;9:e44486. 10.2196/44486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Wang D, Sun X, He F, Liu C, Wu Y. The mediating effect of family health on the relationship between health literacy and mental health: a national cross‐sectional survey in China. Int J Soc Psychiatry. 2023;69(6):1490–1500. 10.1177/00207640231166628 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The PBICR project has been ongoing from 2020 to the present, with an annual multi‐center extensive sample size transect survey. We usually distinguish between different years of surveys by the suffix (e.g., PBICR2023 denotes surveys conducted by PBICR in 2023). The historical materials and any associated protocols supporting this study's findings are available from the corresponding authors upon request (Email: bjmuwuyibo@outlook.com).


