Abstract
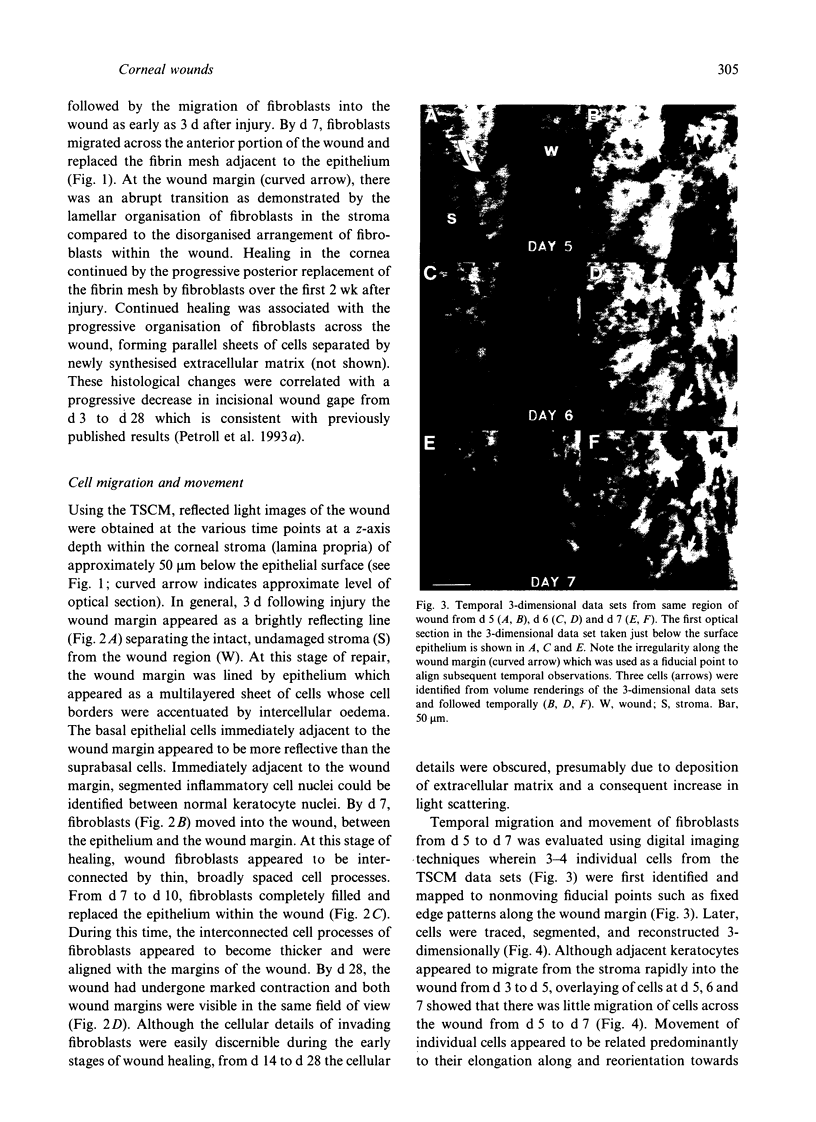
We have evaluated temporally the 3-dimensional cellular anatomy of corneal wound tissue in the rabbit eye using in vivo tandem scanning confocal microscopy. In vivo microscopic studies showed that corneal fibroblast migrated into the wound as an interconnected cellular meshwork with long, thin, randomly oriented cell processes. Interconnection of fibroblasts was further confirmed by localisation of monoclonal antibodies to connexin 43 which demonstrated prominent staining of putative gap junctions between fibroblasts. Temporal observations indicated that the interconnected cells and cellular processes undergo sequential positional changes leading to orientation of cells and interconnected cell processes parallel to the wound margin. Laser scanning confocal microscopy of en bloc, phalloidin-stained corneal wounds showed prominent intracellular f-actin bundles (i.e. stress fibres) within cell processes which formed an extensive interwoven pattern within the wound.
Full text
PDF







Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ABERCROMBIE M., JAMES D. W., NEWCOMBE J. F. Wound contraction in rabbit skin, studied by splinting the wound margins. J Anat. 1960 Apr;94:170–182. [PMC free article] [PubMed] [Google Scholar]
- Bement W. M., Forscher P., Mooseker M. S. A novel cytoskeletal structure involved in purse string wound closure and cell polarity maintenance. J Cell Biol. 1993 May;121(3):565–578. doi: 10.1083/jcb.121.3.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyer E. C., Kistler J., Paul D. L., Goodenough D. A. Antisera directed against connexin43 peptides react with a 43-kD protein localized to gap junctions in myocardium and other tissues. J Cell Biol. 1989 Feb;108(2):595–605. doi: 10.1083/jcb.108.2.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhathal P. S. Presence of modified fibroblasts in cirrhotic livers in man. Pathology. 1972 Apr;4(2):139–144. doi: 10.3109/00313027209068932. [DOI] [PubMed] [Google Scholar]
- Darby I., Skalli O., Gabbiani G. Alpha-smooth muscle actin is transiently expressed by myofibroblasts during experimental wound healing. Lab Invest. 1990 Jul;63(1):21–29. [PubMed] [Google Scholar]
- Ehrlich H. P., Rajaratnam J. B. Cell locomotion forces versus cell contraction forces for collagen lattice contraction: an in vitro model of wound contraction. Tissue Cell. 1990;22(4):407–417. doi: 10.1016/0040-8166(90)90070-p. [DOI] [PubMed] [Google Scholar]
- Gabbiani G., Chaponnier C., Hüttner I. Cytoplasmic filaments and gap junctions in epithelial cells and myofibroblasts during wound healing. J Cell Biol. 1978 Mar;76(3):561–568. doi: 10.1083/jcb.76.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbiani G., Hirschel B. J., Ryan G. B., Statkov P. R., Majno G. Granulation tissue as a contractile organ. A study of structure and function. J Exp Med. 1972 Apr 1;135(4):719–734. doi: 10.1084/jem.135.4.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbiani G., Ryan G. B., Majne G. Presence of modified fibroblasts in granulation tissue and their possible role in wound contraction. Experientia. 1971 May 15;27(5):549–550. doi: 10.1007/BF02147594. [DOI] [PubMed] [Google Scholar]
- Garana R. M., Petroll W. M., Chen W. T., Herman I. M., Barry P., Andrews P., Cavanagh H. D., Jester J. V. Radial keratotomy. II. Role of the myofibroblast in corneal wound contraction. Invest Ophthalmol Vis Sci. 1992 Nov;33(12):3271–3282. [PubMed] [Google Scholar]
- Harris A. K., Wild P., Stopak D. Silicone rubber substrata: a new wrinkle in the study of cell locomotion. Science. 1980 Apr 11;208(4440):177–179. doi: 10.1126/science.6987736. [DOI] [PubMed] [Google Scholar]
- Jester J. V., Andrews P. M., Petroll W. M., Lemp M. A., Cavanagh H. D. In vivo, real-time confocal imaging. J Electron Microsc Tech. 1991 May;18(1):50–60. doi: 10.1002/jemt.1060180108. [DOI] [PubMed] [Google Scholar]
- Jester J. V., Barry P. A., Lind G. J., Petroll W. M., Garana R., Cavanagh H. D. Corneal keratocytes: in situ and in vitro organization of cytoskeletal contractile proteins. Invest Ophthalmol Vis Sci. 1994 Feb;35(2):730–743. [PubMed] [Google Scholar]
- Jester J. V., Petroll W. M., Garana R. M., Lemp M. A., Cavanagh H. D. Comparison of in vivo and ex vivo cellular structure in rabbit eyes detected by tandem scanning microscopy. J Microsc. 1992 Jan;165(Pt 1):169–181. doi: 10.1111/j.1365-2818.1992.tb04314.x. [DOI] [PubMed] [Google Scholar]
- Jester J. V., Rodrigues M. M., Herman I. M. Characterization of avascular corneal wound healing fibroblasts. New insights into the myofibroblast. Am J Pathol. 1987 Apr;127(1):140–148. [PMC free article] [PubMed] [Google Scholar]
- Klein C. E., Dressel D., Steinmayer T., Mauch C., Eckes B., Krieg T., Bankert R. B., Weber L. Integrin alpha 2 beta 1 is upregulated in fibroblasts and highly aggressive melanoma cells in three-dimensional collagen lattices and mediates the reorganization of collagen I fibrils. J Cell Biol. 1991 Dec;115(5):1427–1436. doi: 10.1083/jcb.115.5.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luttrull J. K., Smith R. E., Jester J. V. In vitro contractility of avascular corneal wounds in rabbit eyes. Invest Ophthalmol Vis Sci. 1985 Oct;26(10):1449–1452. [PubMed] [Google Scholar]
- MacKenzie L. W., Garfield R. E. Hormonal control of gap junctions in the myometrium. Am J Physiol. 1985 Mar;248(3 Pt 1):C296–C308. doi: 10.1152/ajpcell.1985.248.3.C296. [DOI] [PubMed] [Google Scholar]
- Majno G., Gabbiani G., Hirschel B. J., Ryan G. B., Statkov P. R. Contraction of granulation tissue in vitro: similarity to smooth muscle. Science. 1971 Aug 6;173(3996):548–550. doi: 10.1126/science.173.3996.548. [DOI] [PubMed] [Google Scholar]
- Martin P., Lewis J. Actin cables and epidermal movement in embryonic wound healing. Nature. 1992 Nov 12;360(6400):179–183. doi: 10.1038/360179a0. [DOI] [PubMed] [Google Scholar]
- Miller S. M., Garfield R. E., Daniel E. E. Improved propagation in myometrium associated with gap junctions during parturition. Am J Physiol. 1989 Jan;256(1 Pt 1):C130–C141. doi: 10.1152/ajpcell.1989.256.1.C130. [DOI] [PubMed] [Google Scholar]
- Nagle R. B., Evans L. W., Reynolds D. G. Contractility of renal cortex following complete ureteral obstruction. Proc Soc Exp Biol Med. 1975 Mar;148(3):611–614. doi: 10.3181/00379727-148-38594. [DOI] [PubMed] [Google Scholar]
- Nagle R. B., Kneiser M. R., Bulger R. E., Benditt E. P. Induction of smooth muscle characteristics in renal interstitial fibroblasts during obstructive nephropathy. Lab Invest. 1973 Oct;29(4):422–427. [PubMed] [Google Scholar]
- Petroll W. M., Cavanagh H. D., Barry P., Andrews P., Jester J. V. Quantitative analysis of stress fiber orientation during corneal wound contraction. J Cell Sci. 1993 Feb;104(Pt 2):353–363. doi: 10.1242/jcs.104.2.353. [DOI] [PubMed] [Google Scholar]
- Petroll W. M., Cavanagh H. D., Jester J. V. Three-dimensional imaging of corneal cells using in vivo confocal microscopy. J Microsc. 1993 Jun;170(Pt 3):213–219. doi: 10.1111/j.1365-2818.1993.tb03344.x. [DOI] [PubMed] [Google Scholar]
- Petroll W. M., Cavanagh H. D., Lemp M. A., Andrews P. M., Jester J. V. Digital image acquisition in in vivo confocal microscopy. J Microsc. 1992 Jan;165(Pt 1):61–69. doi: 10.1111/j.1365-2818.1992.tb04305.x. [DOI] [PubMed] [Google Scholar]
- Petroll W. M., New K., Sachdev M., Cavanagh H. D., Jester J. V. Radial keratotomy. III. Relationship between wound gape and corneal curvature in primate eyes. Invest Ophthalmol Vis Sci. 1992 Nov;33(12):3283–3291. [PubMed] [Google Scholar]
- Risek B., Guthrie S., Kumar N., Gilula N. B. Modulation of gap junction transcript and protein expression during pregnancy in the rat. J Cell Biol. 1990 Feb;110(2):269–282. doi: 10.1083/jcb.110.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph R., McClure W. J., Woodward M. Contractile fibroblasts in chronic alcoholic cirrhosis. Gastroenterology. 1979 Apr;76(4):704–709. [PubMed] [Google Scholar]
- Singer I. I., Kawka D. W., Kazazis D. M., Clark R. A. In vivo co-distribution of fibronectin and actin fibers in granulation tissue: immunofluorescence and electron microscope studies of the fibronexus at the myofibroblast surface. J Cell Biol. 1984 Jun;98(6):2091–2106. doi: 10.1083/jcb.98.6.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalli O., Schürch W., Seemayer T., Lagacé R., Montandon D., Pittet B., Gabbiani G. Myofibroblasts from diverse pathologic settings are heterogeneous in their content of actin isoforms and intermediate filament proteins. Lab Invest. 1989 Feb;60(2):275–285. [PubMed] [Google Scholar]
- Stopak D., Harris A. K. Connective tissue morphogenesis by fibroblast traction. I. Tissue culture observations. Dev Biol. 1982 Apr;90(2):383–398. doi: 10.1016/0012-1606(82)90388-8. [DOI] [PubMed] [Google Scholar]
- Tabb T., Thilander G., Grover A., Hertzberg E., Garfield R. An immunochemical and immunocytologic study of the increase in myometrial gap junctions (and connexin 43) in rats and humans during pregnancy. Am J Obstet Gynecol. 1992 Aug;167(2):559–567. doi: 10.1016/s0002-9378(11)91453-7. [DOI] [PubMed] [Google Scholar]
- Tomasek J. J., Hay E. D., Fujiwara K. Collagen modulates cell shape and cytoskeleton of embryonic corneal and fibroma fibroblasts: distribution of actin, alpha-actinin, and myosin. Dev Biol. 1982 Jul;92(1):107–122. doi: 10.1016/0012-1606(82)90155-5. [DOI] [PubMed] [Google Scholar]
- Walshe R., Esser P., Wiedemann P., Heimann K. Proliferative retinal diseases: myofibroblasts cause chronic vitreoretinal traction. Br J Ophthalmol. 1992 Sep;76(9):550–552. doi: 10.1136/bjo.76.9.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts G. T., Grillo H. C., Gross J. Studies in Wound Healing: II. The Role of Granulation Tissue in Contraction. Ann Surg. 1958 Aug;148(2):153–160. doi: 10.1097/00000658-195808000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch M. P., Odland G. F., Clark R. A. Temporal relationships of F-actin bundle formation, collagen and fibronectin matrix assembly, and fibronectin receptor expression to wound contraction. J Cell Biol. 1990 Jan;110(1):133–145. doi: 10.1083/jcb.110.1.133. [DOI] [PMC free article] [PubMed] [Google Scholar]









