Abstract
Biomechanical study of the visual system by ocular response analyzer investigates the inter-structural biological relationships, mechanics, and function of the visual system. This review aimed to investigate the changes in corneal biomechanical parameters with age and sex. The articles published in PubMed between 2000 and 2021 were investigated and critiqued, and valid scientific evidence was collected, reviewed and concluded according to the inclusion and exclusion criteria. Most studies showed that corneal biomechanical changes occur infrequently in children up to the age of 20y, and with increasing age and wider age range, there was a significant decrease in corneal biomechanical indices, especially corneal hysteresis. In children and adults, most studies have shown that these biomechanical indicators, especially corneal resistance factor, were higher in females. Although hormonal changes may contribute to this finding, the role of axial length and other biometric indicators should not be ignored. The axial length, the intraocular pressure, and the corneal thickness are other factors associated with biomechanical parameters that should be taken into account in clinical diagnosis and management especially for patients undergoing refractive surgery as well as keratoconus patients.
Keywords: ocular response analyzer, corneal biomechanics, visual function, children, elderly
INTRODUCTION
Biomechanical study of the visual system investigates the inter-structural biological relationships, mechanics, and function of the visual system[1]. These biomechanical properties are affected in some diseases associated with less corneal stability including keratoconus[2]–[3]. Since biomechanical stability depends on the order and organization of structural components within the cornea, biochemical, cellular, and microstructural changes including a decrease in the mean diameter of corneal fibrils as well as the distance between collagen fibers are expected to have negative consequences on the corneal structural integrity and therefore could lead to abnormal deformation of the cornea under intraocular pressure (IOP)[4].
In addition, corneal biomechanics play a role in the outcome of any procedure in which corneal lamellae are transected. For example, when the structure of the cornea is altered in a procedure that involves central corneal thinning, IOP measurements using conventional tonometry methods would be invalid, and other technologies should be used[5]–[7]. A better understanding of corneal biomechanics helps in improving the outcomes of refractive surgeries, early detection of corneal ectatic disorders, improving treatment methods aimed at strengthening the corneal tissue and diagnosis, management, and follow-up of glaucoma patients[5]–[6],[8]. Studies in this field are significantly limited[9]. On the other hand, the subjects in different available studies were in different age groups while in older people depending on age and sex, the corneal biomechanical changes occur due to age-related hormonal and tissue changes[10]. Also, some reports were not presented completely and separately according to different variables or a specific group of patients, including those with glaucoma, have been studied[11]–[12].
The biomechanical parameters including corneal hysteresis (CH) and corneal resistance factor (CRF) indicate the viscosity, elasticity and corneal rigidity properties[9]. The lower these values, the lower the biomechanical strength of the cornea. The viscoelastic properties of the cornea differ in the elderly compared to younger individuals due to age-related changes in all individual's connective tissues. It has also been suggested that racial differences can cause differences in biomechanical characteristics. Therefore, the results can be different in different races and ages[9],[13].
Limited studies have been conducted worldwide regarding the effect of different demographic and biometric parameters on biomechanical indices. Knowledge of the normal values of corneal biomechanical parameters in the two age groups under 18 and above 60y could provide valuable information for better diagnosis of corneal diseases and differences in the process of treatment and follow-up of these diseases in these two age groups. Therefore, this review study aimed to investigate the corneal biomechanical indices and their differences in these two age groups in the world for practical use in corneal diseases and even systemic and ocular diseases affecting the cornea such as diabetes and glaucoma.
RESEARCH METHODS AND DESCRIPTION OF THE EVIDENCE
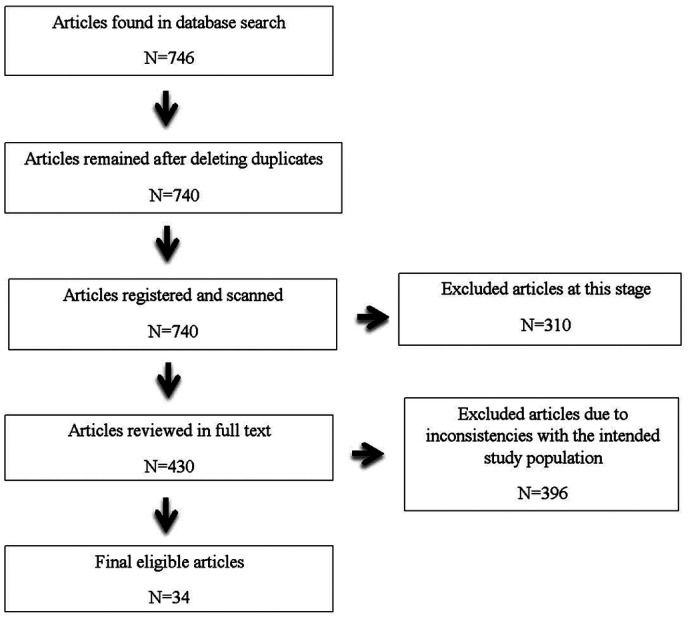
In this study, a search was conducted on Internet databases (between 2008 and 2024) with the following keywords in English: prevalence, epidemiology, incidence, rates, ocular response analyzer (ORA), child, elderly, corneal biomechanics, corneal hysteresis, CRF, central corneal thickness, intraocular pressure. These keywords were independently searched on PubMed, Science Direct, Scopus and Medline (Ovid), Embase, CINAHL, PsycINFO, Cochrane Central (CDSR, DARE, NHS EED, HTA), PSYNDEX plus, Social SciSearch, GIN, and Medion Google Scholar. The search process is described in the flowchart (Figure 1). In this review article, the following inclusion and exclusion criteria were considered for selecting or not selecting the papers:
Figure 1. The flowchart illustrating the selection process of articles.
1) The paper's publication date should be between January 2000 to January 2021.
2) The paper should be focused on the studied subject and related to the title and purpose of the present review article.
3) The paper must be published in full.
4) The paper should consider other ORA-derived parameters related to corneal biomechanics such as IOP.
5) The paper should not be related to specific populations, such as patients with corneal diseases.
6) Similar or duplicate articles were categorized and based on the last year of publication and the impact factor of the publishing journal, the required papers were selected and the rest were excluded from the study.
Thus, different articles were obtained. According to the inclusion and exclusion criteria, 34 final articles were selected and the rest were excluded from the study. These selected articles were discussed, reviewed, critiqued and concluded, in terms of subject matter, method of study, and published conclusions.
RESULTS
Of the 746 articles found, 34 articles were finally included in this study. The study population in the present review was two age groups of children and the elderly in the normal population considering that corneal problems and corneal surgeries affect the results and net values of biomechanical indices are not obtained in these cases for comparison between the two age groups.
Relationship Between Age and Biomechanical Parameters
The results of this review indicate significant age-related changes in corneal biomechanical parameters. Tables 1[6],[13]–[29] and 2[6],[17],[21],[25],[30]–[34] show the results separately for children and the elderly.
Table 1. Studies of CH and CRF by ocular response analyzer in the elderly.
| Study | Year | Sample size | Age (y) | Country | CH (mm Hg) | CRF (mm Hg) |
| Kamiya et al[14] | 2009 | 204 | 19–89 | Japan | 10.10±1.5 | 10.10±1.6 |
| Narayanaswamy et al[15] | 2011 | 1136 | 44–83 | China | 10.6±1.50 | 10.10±1.60 |
| Hwang et al[16] | 2013 | 958 | 26.7±6.1 | South Korea | 10.10±1.4 | 9.90±1.6 |
| Sen et al[17] | 2014 | 122 | 69.6±6.6 | Turkey | 9.10±1.4 | 8.9±1.7 |
| Strobbe et al[18] | 2014 | 400 | 58.8±17.2 | Italy | 10.0±1.6 | 10.5±1.7 |
| Rosa et al[19] | 2015 | 105 | 43.1±15.4 | Italy | 10.26±1.49 | 10.38±1.64 |
| Johannesson et al[20] | 2015 | 43 | 64–79 | Sweden | 10.00±1.3 | 10.20±1.5 |
| Sharifipour et al[21] | 2016 | 51 | 60–69 | Iran | 10.32±1.9 | 10.22±1.8 |
| Schweitzer et al[22] | 2016 | 624 | 75–96 | France | 9.40±1.9 | 9.8±1.9 |
| Al-Arfaj et al[23] | 2016 | 215 | 33.6±11.75 | Saudi Arabia | 11.6±2.11 | 11.07±2.31 |
| Celebi et al[24] | 2018 | 2039 | 42.30±14.64 | Turkey | 11.49±1.89 | 11.40±2.30 |
| El Massry et al[25] | 2020 | 102 | >50 | Egypt | 9.5±1.6 | 9.6±1.8 |
| Shokrollahzadeh et al[13] | 2022 | 420 | 69.3±6.5 | Iran | 8.37±1.55 | 9.60±1.70 |
| Sekimitsu et al[26] | 2023 | 87512 | 56.3 | UK | 10.40±1.91 | 10.55±1.98 |
| Du et al[6] | 2023 | 290 | 27.56±8.50 | China | 10.26±1.34 | 10.20±1.64 |
| Čulina et al[27] | 2024 | 40 | 48–83 | Croatia | 8.86±2.44 | 10.04±2.32 |
| Yii et al[28] | 2024 | 10488 | 40–69 | UK | 10.7±1.8 | 10.8±1.9 |
| Stuart et al[29] | 2024 | 68738 | 56.7±8.0 | UK | 10.6±1.7 | 10.7±1.8 |
| Stuart et al[29] | 2024 | 22845 | 62.7±10.1 | Canada | 10.1±1.7 | 10.0± 1.8 |
CH: Corneal hysteresis; CRF: Corneal resistance factor.
Table 2. Studies of CH and CRF by ocular response analyzer in children.
| Study | Year | Sample size | Age (y) | Country/region | CH (mm Hg) | CRF (mm Hg) |
| Chang et al[30] | 2010 | 126 | 12.02±3.19 | Taiwan, China | 11.00±1.29 | 11.03±1.46 |
| Momeni-Moghaddam et al[31] | 2019 | 468 | 11–15 | Iran | 10.81±2.06 | 11.16±2.08 |
| Bueno-Gimeno et al[32] | 2014 | 293 | 6–17 | Spain | 12.12±1.71 | 12.30±1.89 |
| Sen et al[17] | 2014 | 93 | 13.1±2.9 | Turkey | 10.8±1.6 | 10.8±1.6 |
| Sharifipour et al[21] | 2016 | 56 | 10–19 | Iran | 12.51±1.8 | 12.10±1.9 |
| El Massry et al[25] | 2020 | 508 | 10–20 | Egypt | 10.9±2.4 | 10.9±2.4 |
| Du et al[6] | 2023 | 65 | 13.85±2.81 | China | 11.12±1.20 | 11.00±1.69 |
| Marinescu et al[33] | 2023 | 170 | 15.26±2.69 | Romania | 11.79±1.98 | 11.98±2.17 |
| Aydin Eroglu et al[34] | 2024 | 73 | 6–17 | Turkey | 10.8±1.9 | 11.4±1.9 |
CH: Corneal hysteresis; CRF: Corneal resistance factor.
As seen, there are obvious differences in biomechanical findings between age groups less than 18y and over 60y among different studies. The studies proposed different reasons for observing this difference. For example, the study by El Massry et al[25] show that the overall means of CH and CRF in the oldest group were significantly lower than in the youngest group.
This finding was attributed to the change in the elasticity of the cornea and the decrease in this property due to aging. In another study, Kamiya et al[14] stated that the viscoelastic properties of the cornea remained constant with age, which contradicted the conclusion of the previous study. However, it was also stated that since CRF had a positive relationship with Goldmann-correlated intraocular pressure (IOPg) and CH did not, and a significant increase in IOPg was seen with age, it can be concluded that the viscoelasticity of the cornea decreases with age. As a result, changes in CH and CRF are compensated for simultaneously with an increase in IOP. The authors recommended further studies with larger sample sizes[14]. Narayanaswamy et al[15] also suggested that age-related changes in the corneal stroma, including increased stromal fibril diameter and inter-fibrillary cross-linking, could theoretically lead to increased corneal stiffness. In another study conducted by Hashemi et al[35] in children aged 6y to 18y, these two variables did not show significant age-related changes in this age range. Chang and Lim did not observe significant changes in these indices with age in children aged 12y to 15y[30]. Narayanaswamy et al[15] showed that at older ages, advancing age was associated with a significant decrease in CH and CRF. Kamiya et al[14] also reported that in people aged 19y to 89y, CRF and CH significantly decreased with age without a significant change in the central corneal thickness.
Relationship Between Sex and Biomechanical Parameters
Some studies investigated the relationship between biomechanical parameters with demographic parameters (sex-related differences) and other ocular parameters such as biometric indices. It should be noted that in studies conducted in children such as the study by Momeni-Moghaddam et al's[31], there was a significant difference between males and females and the biomechanical indices were higher in males. This finding was explained based on the difference in structural consistency and hormonal differences. In another study, the means of both biomechanical values (CH and CRF) were higher in females than in males. This study differed from the previous study in terms of age range[21]. The study by Momeni-Moghaddam et al[31] was performed on children aged 7y to 11y; the differences in sex hormones in this age group are not completely evident. However, the study of Sharifipour et al[21] included a wide age range of 10y to 69y, and the differences in sex hormones are expected to be more prominent due to reaching puberty and above. Studies in the older age ranges were also in line with the study of Sharifipour et al[21]. In the study by Narayanaswamy et al[15], the mean CH was higher in women (10.8) than in men (10.4). The mean CRF was also higher in women (10.4) than men (9.8). In another study, the mean CH and CRF were higher in women than men[17]. In contrast, in the study by Strobbe et al[18], the relationship between age and sex with corneal biomechanical parameters was examined and the mean CH in women (9.9) was lower than men (10.2). Also, the mean CRF in women (10.3) was lower than in men (10.8). In this study, it was stated that sex and age both affect corneal biomechanical indices, and attributed this finding to hormonal effects. Hashemi et al[35] also showed that CRF was significantly higher in female children while CH was not significantly different between the two sexes. Narayanaswamy et al[15] showed that females had higher CRF and CH values.
Relationship Between Biomechanical Indices and Ocular Parameters
Guo et al[36] reported in their studies that central corneal thickness is the most important factor affecting corneal biomechanical parameters. Regarding the relationship between intraocular pressure and biomechanical parameters, Li[5] in a Meta-analysis compared the biomechanical characteristics between the normal individuals and patients with glaucoma, he showed that CH and CRF indices are significantly lower in glaucoma patients. In another study, both eyes of the participants were examined. The CH and CRF were significantly inversely related to axial length. The CH difference between the two eyes was also significantly related to the AL difference. Decreased CH in myopic eyes may indicate early changes in corneal or collagen-related markers; as a result, myopic eyes are less resistant to a tensile stress of the normal intraocular pressure, which leads to increased axial length[32],[37]. Also, changes in the metalloprotease matrix in the collagenous tissue of the cornea and sclera can be the cause of reduced CH in myopia[30],[38]. In other studies, this relationship was also observed between biomechanical parameters with axial length and myopia[32]. According to Tables 1 and 2, it can be seen that the average values of corneal biomechanical indices were higher in children and were in the range of 11.50 to 12 mm Hg for children and the range of 10.5 mm Hg for the elderly.
DISCUSSION
The viscoelastic properties are part of the biomechanical properties of the cornea[39]. Knowledge of biomechanical properties provides important biological information[39]. The parameters of CH and corneal resistant factor indicate the viscosity, elasticity and resistant properties of the cornea, and the lower these values, the lower the corneal strength[6]. Practically, knowledge of corneal biomechanical status is important in fitting contact lenses, healing corneal wounds, and cases related to intraocular pressure[40]. In addition, in cases such as keratoconus and changes in the corneal topography, biomechanical indices are important and can be very helpful in diagnosing and managing these conditions[41].
Regarding the relationship between age and corneal biomechanics, there are contradictory results, as stated in the results section. However, it should be noted that most studies have shown a decrease in the biomechanical characteristics of the cornea with age, and the rest of the studies with contradictory results are questionable due to low sample size or sampling and analysis methods.
Table 2 shows the biomechanical values measured in different countries in the age group of less than 18y, which were higher than the values obtained in older ages (Table 1). All studies pointed to the age-related decrease in biomechanical parameters. Also, both CH and CRF values were about 10 mm Hg in people over 60 years old and about 11.5 mm Hg in younger people. A look at all the investigated studies shows that corneal biomechanical parameters are less affected by age under the age of 20y, and these biomechanical changes occur more prominently in the older ages. In other words, we could see corneal biomechanics changes over a wide range of ages. It seems that the energy absorption capability of the cornea and the elastic resistance of the corneal tissue are almost constant in the under-20s, and in the older ages the energy absorption capability and resistance of the cornea are declining. Strobbe et al[18] showed an increase in the corneal stromal fibril with age. Also, with increasing age, inter-fibrillar cross-linking and glycation occur which is associated with an increase in corneal stiffness and strength. These changes in the cornea are inconsistent with decreasing CRF and CH with age. This is because in some studies only CH decreased with age and CRF which is affected by corneal stiffness, did not change with age. However, Sharifipour et al[21] explained the corneal biomechanical changes with age as follows; although increasing collagen cross-linking with advancing age leads to stiffening of the cornea, increasing the corneal water content with age leads to a decrease in CH and CRF.
Regarding the relationship between sex and corneal biomechanical parameters, most studies reported higher biomechanical values, especially CRF, in women than in men. Sex differences in corneal biomechanical indices can be explained based on hormonal differences and their effects on corneal structural strength. However, the role of axial length could not be ignored in this regard. As we know from previous studies, the axial length in females is shorter than in males, and the inverse relationship between axial length and corneal biomechanical indices has been reported in many studies. Therefore, the shorter axial length may contribute to higher corneal biomechanical parameters in women compared to men.
Limited studies are available on the relationship between biomechanical indices and ocular parameters. Therefore, the results are difficult to compare. A common finding among studies is the significant effect of central corneal thickness on biomechanical parameters. Given that the corneal thickness is an important component affecting the elasticity of the cornea and its flexibility, so this finding is logical. Since the intraocular pressure is also affected by corneal thickness and corneal thickness affects the amount of measured intraocular pressure and even the two parameters IOPg and corneal-compensated intraocular pressure (IOPcc) were defined accordingly in the ORA device, so the intraocular pressure also affects the biomechanical characteristics of the cornea.
Some studies found interesting relationships between corneal biomechanical characteristics and some ocular parameters such as axial length and refractive error, and reported a lower CH in myopic eyes. Theories have been proposed in this regard. In eyes with lower CH, the cornea and sclera are more easily deformed, and as a result, these eyes are more prone to increased axial length. It has also suggested that secondary mechanical changes occur following axial length elongation, which leads to a decrease in CH. In some studies, the values of CH and CRF in hyperopic individuals were significantly higher than in myopes and emmetropes which can be explained given the reduction of structural consistency due to the older ages of the participants[14],[42].
In conclusion, corneal biomechanical indices, especially CH decrease with age and these indices (especially CRF) are higher in women than men.
Footnotes
Foundation: Supported by Noor Ophthalmology Research Center.
Conflicts of Interest: Hashemi H, None; Shokrollahzadeh F, None; Ostadimoghaddam H, None; Yekta A, None; Khabazkhoob M, None.
REFERENCES
- 1.Loveless BA, Moin KA, Hoopes PC, Moshirfar M. The utilization of Brillouin microscopy in corneal diagnostics: a systematic review. Cureus. 2024;16(7):e65769. doi: 10.7759/cureus.65769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solodkova EG, Malyugin BE, Zakharov IN, Le VH, Balalin SV, Lobanov EV, Balalin AS. Analysis of corneal biomechanical properties in different keratotopographic patterns of keratoconus. J Curr Ophthalmol. 2023;35(3):249–258. doi: 10.4103/joco.joco_83_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidari Z, Hashemi H, Mohammadpour M, Amanzadeh K, Fotouhi A. Evaluation of corneal topographic, tomographic and biomechanical indices for detecting clinical and subclinical keratoconus: a comprehensive three-device study. Int J Ophthalmol. 2021;14(2):228–239. doi: 10.18240/ijo.2021.02.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Natarajan R, Giridhar D. Corneal scarring after epithelium-off collagen cross-linking. Indian J Ophthalmol. 2024 doi: 10.4103/IJO.IJO_95_24. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li XR. Changes in corneal biomechanics in patients with glaucoma: a systematic review and meta-analysis. BMC Ophthalmol. 2024;24(1):168. doi: 10.1186/s12886-024-03443-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du YR, Zhang YQ, Zhang Y, Li T, Wang J, Du ZY. Analysis of potential impact factors of corneal biomechanics in myopia. BMC Ophthalmol. 2023;23(1):143. doi: 10.1186/s12886-023-02891-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li ZJ, Yang C, Liu SH, Guo J, Duan YH. Changes in corneal biomechanics and posterior corneal surface elevation after FS-LASIK. Int J Ophthalmol. 2023;16(11):1832–1837. doi: 10.18240/ijo.2023.11.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Humayun S, Bangash YW, Ishaq M, Yasmeen H. Changes in corneal biomechanical properties after laser-assisted in situ keratomileusis and photorefractive keratectomy in myopia. J Coll Physicians Surg Pak. 2023;33(9):1023–1027. doi: 10.29271/jcpsp.2023.09.1023. [DOI] [PubMed] [Google Scholar]
- 9.Komninou MA, Seiler TG, Enzmann V. Corneal biomechanics and diagnostics: a review. Int Ophthalmol. 2024;44(1):132. doi: 10.1007/s10792-024-03057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kenia VP, Kenia RV, Pirdankar OH. Age-related variation in corneal biomechanical parameters in healthy Indians. Indian J Ophthalmol. 2020;68(12):2921–2929. doi: 10.4103/ijo.IJO_2127_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elhusseiny AM, Scarcelli G, Saeedi OJ. Corneal biomechanical measures for glaucoma: a clinical approach. Bioengineering. 2023;10(10):1108. doi: 10.3390/bioengineering10101108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Del Buey-Sayas MÁ, Lanchares-Sancho E, Campins-Falcó P, Pinazo-Durán MD, Peris-Martínez C. Corneal biomechanical parameters and central corneal thickness in glaucoma patients, glaucoma suspects, and a healthy population. J Clin Med. 2021;10(12):2637. doi: 10.3390/jcm10122637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shokrollahzadeh F, Hashemi H, Yekta A, Ostadimoghaddam H, Khabazkhoob M. Corneal biomechanical parameters after 60-year-old. J Curr Ophthalmol. 2022;34(3):284–289. doi: 10.4103/joco.joco_201_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamiya K, Shimizu K, Ohmoto F. Effect of aging on corneal biomechanical parameters using the ocular response analyzer. J Refract Surg. 2009;25(10):888–893. doi: 10.3928/1081597X-20090917-10. [DOI] [PubMed] [Google Scholar]
- 15.Narayanaswamy A, Chung RS, Wu RY, Park J, Wong WL, Saw SM, Wong TY, Aung T. Determinants of corneal biomechanical properties in an adult Chinese population. Ophthalmology. 2011;118(7):1253–1259. doi: 10.1016/j.ophtha.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Hwang HS, Park SK, Kim MS. The biomechanical properties of the cornea and anterior segment parameters. BMC Ophthalmol. 2013;13:49. doi: 10.1186/1471-2415-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sen E, Elgin KU, Yüksekkaya P, Tirhiş MH, Aksakal FN, Teke MY, Oztürk F. Age-related changes in biomechanical parameters of the cornea and intraocular pressure in a healthy Turkish population. Turk J Med Sci. 2014;44(4):687–690. [PubMed] [Google Scholar]
- 18.Strobbe E, Cellini M, Barbaresi U, Campos EC. Influence of age and gender on corneal biomechanical properties in a healthy Italian population. Cornea. 2014;33(9):968–972. doi: 10.1097/ICO.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 19.Rosa N, Lanza M, de Bernardo M, Signoriello G, Chiodini P. Relationship between corneal hysteresis and corneal resistance factor with other ocular parameters. Semin Ophthalmol. 2015;30(5-6):335–339. doi: 10.3109/08820538.2013.874479. [DOI] [PubMed] [Google Scholar]
- 20.Jóhannesson G, Hallberg P, Ambarki K, Eklund A, Lindén C. Age-dependency of ocular parameters: a cross sectional study of young and elderly healthy subjects. Graefes Arch Clin Exp Ophthalmol. 2015;253(11):1979–1983. doi: 10.1007/s00417-015-3129-5. [DOI] [PubMed] [Google Scholar]
- 21.Sharifipour F, Panahi-Bazaz M, Bidar R, Idani A, Cheraghian B. Age-related variations in corneal biomechanical properties. J Curr Ophthalmol. 2016;28(3):117–122. doi: 10.1016/j.joco.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schweitzer C, Korobelnik JF, Boniol M, et al. Associations of biomechanical properties of the cornea with environmental and metabolic factors in an elderly population: the ALIENOR study. Invest Ophthalmol Vis Sci. 2016;57(4):2003–2011. doi: 10.1167/iovs.16-19226. [DOI] [PubMed] [Google Scholar]
- 23.Al-Arfaj K, Yassin SA, Al-Dairi W, Al-Shamlan F, Al-Jindan M. Corneal biomechanics in normal Saudi individuals. Saudi J Ophthalmol. 2016;30(3):180–184. doi: 10.1016/j.sjopt.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Celebi ARC, Kilavuzoglu AE, Altiparmak UE, Cosar Yurteri CB. Age-related change in corneal biomechanical parameters in a healthy Caucasian population. Ophthalmic Epidemiol. 2018;25(1):55–62. doi: 10.1080/09286586.2017.1351997. [DOI] [PubMed] [Google Scholar]
- 25.El Massry AAK, Said AA, Osman IM, Bessa AS, Elmasry MA, Elsayed EN, Bayoumi NHL. Corneal biomechanics in different age groups. Int Ophthalmol. 2020;40(4):967–974. doi: 10.1007/s10792-019-01273-8. [DOI] [PubMed] [Google Scholar]
- 26.Sekimitsu S, Xiang D, Smith SL, et al. UK Biobank Eye and Vision Consortium Deep ocular phenotyping across primary open-angle glaucoma genetic burden. JAMA Ophthalmol. 2023;141(9):891–899. doi: 10.1001/jamaophthalmol.2023.3645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Čulina K, Tomić M, Bulum T, Medić A, Šoša I, Ivanišević K, Jukić T. Corneal biomechanics and other factors associated with postoperative astigmatism after cataract surgery. Life. 2024;14(6):655. doi: 10.3390/life14060655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yii F, Strang N, Bernabeu MO, Dhillon B, MacGillivray T. Corneal biomechanics are not exclusively compromised in high myopia. Ophthalmic Physiol Opt. 2024;44(5):977–986. doi: 10.1111/opo.13313. [DOI] [PubMed] [Google Scholar]
- 29.Stuart KV, Madjedi KM, Luben RN, et al. Modifiable Risk Factors for Glaucoma Collaboration and the UK Biobank Eye and Vision Consortium Smoking, corneal biomechanics, and glaucoma: results from two large population-based cohorts. Invest Ophthalmol Vis Sci. 2024;65(1):11. doi: 10.1167/iovs.65.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang PY, Chang SW, Wang JY. Assessment of corneal biomechanical properties and intraocular pressure with the Ocular Response Analyzer in childhood myopia. Br J Ophthalmol. 2010;94(7):877–881. doi: 10.1136/bjo.2009.158568. [DOI] [PubMed] [Google Scholar]
- 31.Momeni-Moghaddam H, Hashemi H, Zarei-Ghanavati S, Ostadimoghaddam H, Yekta A, Aghamirsalim M, Khabazkhoob M. Four-year changes in corneal biomechanical properties in children. Clin Exp Optom. 2019;102(5):489–495. doi: 10.1111/cxo.12890. [DOI] [PubMed] [Google Scholar]
- 32.Bueno-Gimeno I, España-Gregori E, Gene-Sampedro A, Lanzagorta-Aresti A, Piñero-Llorens DP. Relationship among corneal biomechanics, refractive error, and axial length. Optom Vis Sci. 2014;91(5):507–513. doi: 10.1097/OPX.0000000000000231. [DOI] [PubMed] [Google Scholar]
- 33.Marinescu M, Dascalescu D, Constantin M, Coviltir V, Burcel M, Darabus D, Ciuluvica R, Stanila D, Voinea L, Potop V. Corneal biomechanical properties in myopic and emmetropic children. Eur Rev Med Pharmacol Sci. 2023;27(8):3580–3589. doi: 10.26355/eurrev_202304_32139. [DOI] [PubMed] [Google Scholar]
- 34.Aydin Eroglu S, Akyuz Unsal AI, Verdi F, Kurt Omurlu I, Unuvar T, Anik A. The effect of childhood obesity on intraocular pressure, corneal biomechanics, retinal nerve fiber layer, and central macular thickness. J Glaucoma. 2024;33(6):417–421. doi: 10.1097/IJG.0000000000002372. [DOI] [PubMed] [Google Scholar]
- 35.Hashemi H, Jafarzadehpur E, Mehravaran S, Yekta A, Ostadimoghaddam H, Norouzirad R, Khabazkhoob M. Corneal resistance factor and corneal hysteresis in a 6- to 18-year-old population. J Cataract Refract Surg. 2014;40(9):1446–1453. doi: 10.1016/j.jcrs.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 36.Guo YH, Guo LL, Yang WQ, Tian L, Jie Y. Age-related analysis of corneal biomechanical parameters in healthy Chinese individuals. Sci Rep. 2024;14(1):21713. doi: 10.1038/s41598-024-72054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sedaghat MR, Momeni-Moghaddam H, Azimi A, et al. Corneal biomechanical properties in varying severities of myopia. Front Bioeng Biotechnol. 2020;8:595330. doi: 10.3389/fbioe.2020.595330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang RT, Singh K. Myopia and glaucoma: diagnostic and therapeutic challenges. Curr Opin Ophthalmol. 2013;24(2):96–101. doi: 10.1097/ICU.0b013e32835cef31. [DOI] [PubMed] [Google Scholar]
- 39.Padmanabhan P, Elsheikh A. Keratoconus: a biomechanical perspective. Curr Eye Res. 2023;48(2):121–129. doi: 10.1080/02713683.2022.2088798. [DOI] [PubMed] [Google Scholar]
- 40.López-Muñoz A, López-Castaño I, Torres-Parejo Ú, García-Romera MC. A corneal biomechanical study measured with a scheimpflug dynamic analyser in soft contact lens wearers. Life. 2023;13(12):2313. doi: 10.3390/life13122313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bui AD, Truong A, Pasricha ND, Indaram M. Keratoconus diagnosis and treatment: recent advances and future directions. Clin Ophthalmol. 2023;17:2705–2718. doi: 10.2147/OPTH.S392665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kamiya K, Hagishima M, Fujimura F, Shimizu K. Factors affecting corneal hysteresis in normal eyes. Graefes Arch Clin Exp Ophthalmol. 2008;246(10):1491–1494. doi: 10.1007/s00417-008-0864-x. [DOI] [PubMed] [Google Scholar]