Abstract
Background
Left main coronary bifurcation lesions account for 50% of left main coronary artery disease cases. Although a drug-coated balloon (DCB) has the advantages of immediate release of the drug to the arterial wall and no remaining struts, there is no conclusive evidence to support DCB use.
Methods & Results
We conducted a systematic review in compliance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement. Eighteen retrospective studies and two prospective studies in which left main bifurcation lesions were treated with DCBs were included in our qualitative analysis. The studies were divided into two groups according to the type of DCB used: DCB only and DCB + stent. At the midterm follow-up, the use of DCBs had noninferior or even superior angiographic and clinical outcomes in treating left main bifurcation lesions compared with the use of drug-eluting stents or conventional balloons, whether for de novo or in-stent restenosis lesions. Additionally, side branch late lumen enlargement was observed in several of the included studies, which indicates that DCBs may have the advantage of side branch protection.
Conclusions
According to our descriptive analysis, the DCB technique has a favorable safety and efficacy profiles for the treatment of left main bifurcation lesions. However, additional studies, especially randomized controlled trials, are needed to establish standards for the DCB technique.
Left main coronary artery (LMCA) disease is characterized by high risk and poor prognosis; thus, coronary artery bypass graft surgery (CABG) was the standard treatment for this kind of lesion in the past.[1] Several studies have confirmed that in most circumstances, percutaneous coronary intervention (PCI) with a new generation of drug-eluting stents (DESs) is noninferior to CABG for treating LMCA disease.[2–6] Moreover, left main (LM) coronary bifurcation lesion (CBL) is the most common type of LMCA disease, and accounts for approximately 50% of cases.[7] 2-DES and provisional DES (pDES) are common strategies for treating LM bifurcation lesions. The pDES strategy is supported by a recent study and expert consensus, which recommended it as the standard technique for any noncomplex bifurcation lesions.[8,9] However, regardless of which approach was used, in-stent restenosis (ISR), late side branch occlusion, and flow disturbance caused by a jailing stent strut were not uncommon, and a compromised side branch (mainly the left circumflex coronary artery) was observed in some patients.[10-14] The use of a drug-coated balloon (DCB) has the advantages of immediate drug release to the arterial wall and leaves no polymers or stent struts, which reduce endothelial inflammation and in-stent thrombosis and shorten the duration of dual antiplatelet therapy to only 4 weeks.[15,16] Furthermore, the DCB technique was less likely to cause a carina shift than stenting was, and a meta-analysis reported that DESs were associated with a greater myocardial infarction (MI) risk than was DCB angioplasty.[17]
Previous studies have demonstrated the safety and effectiveness of DCBs for treating intracoronary stent restenosis (ISR), small vessel and bifurcation lesions.[18–26] However, most related studies have excluded LM bifurcation lesions. Considering the advantages of DCBs and the keep it simple and safe (KISS) principle,[9] some studies have explored the use of DCBs for LM bifurcation lesions with or without DES implantation. Therefore, we performed this systematic review to assess the safety and efficacy of DCBs for the treatment of LM bifurcation lesions.
METHODS
Eligibility Criteria
The inclusion criteria of our study were as follows: (1) a randomized controlled trial (RCT) and nonrandomized study (nRS) in which the left main bifurcation lesions were treated with the DCB technique, (2) at least 1 month of follow-up, and (3) available angiographic and/or clinical outcomes. Studies that excluded LMCA or did not report the proportion of LMCA patients were excluded.
Definitions and Outcomes
The clinical outcome was major adverse cardiac events (MACEs), defined as the composite of cardiac/all-cause death, MI and target lesion revascularization (TLR). TLR was defined as any repeat revascularization within the DCB or stented region, either clinically driven or due to > 50% restenosis at follow-up. Angiographic outcomes were follow-up late lumen loss (LLL, defined as the follow-up vessel minimal luminal diameter (MLD) minus the postprocedure MLD) and binary restenosis (defined as a stenosis diameter of at least 50%). The DCB-only strategy involved the use of a DCB to relieve stenosis without the need for stents. The DCB + stent strategy was defined as the use of DES or bioabsorbable vessel scaffolding (BVS) for the main branch and the treatment of the side branch with DCB. The 2-DES strategy involved implanting DESs in the main branch and side branch. The CB + stent approach was used to treat the main branch with a stent, and angioplasty was performed in the side branch with a conventional balloon (CB).
Search Strategy
This was a systematic review conducted in compliance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement. We searched the PUBMED, Embase, Web of Science, Cochrane database of clinical trials, Chinese National Knowledge Infrastructure (CNKI), WanFang Data Knowledge Service Platform (WanFang Data) and Information Resource Integration Service Platform (VIP) without limits on language, publication date, or publication status. Case reports and conference abstracts were excluded. The search strategy was as follows: ((“drug-coated balloon”) OR (“DEB”) OR (“DCB”) OR (“drug-eluting balloon”)) AND (bifurcation lesion). The literature searches were completed in May 2022.
Study Screening and Data Extraction
Two researchers independently screened the identified records and extracted the data by applying the eligibility criteria. The results obtained by the two researchers were compared to determine any discrepancies. The differences were resolved by discussion. General information data (author, year, study design, number of patients), baseline characteristics, procedure angiographic results, and clinical and angiographic outcomes (MACE, LLL, binary restenosis) were extracted from the eligible studies. The baseline characteristics included mean age, sex, hypertension (HTN), diabetes mellitus (DM), angina, myocardial infarction and left ventricular ejection fraction (LVEF). The surgical angiographic results included the proportion of LM bifurcation, ISR/de novo, and CBL types according to Medina and the proportion of true bifurcation lesions.
Quality Assessment
The Newcastle‒Ottawa Scale (NOS) was used to assess the quality of the included nRSs based on selection, comparability, and outcome. The single-arm studies were evaluated without the scale entries of selection of the nonexposed cohort and comparability of cohorts on the basis of the design or analysis. The 20 nRSs were of high quality, as indicated by receiving 5 to 9 stars. The details are shown in Table 1.
Table 1. Newcastle-Ottawa Scales values of 20 nRSs.
| Study | Exposed truly representative of average | Selection non-exposed from same community |
Exposure ascertained by secure record or interview | Demonstration of outcome of interest not present at study start | Comparable based groups based on major factor | Adequate assessment of outcomes | Follow-up long enough for outcome to occur | Adequacy follow-up: subjects lost to follow-up unlikely to introduce bias |
| Non-selective studies | ||||||||
| Schulz, et al.[38] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Harada, et al.[36] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | |
| Naganuma, et al.[37] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ |
| Ikuta, et al.[40] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Elwany, et al.[39] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Herrador, et al.[45] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ |
| Yang, et al.[30] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ |
| Li, et al.[43] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ |
| Kitani, et al.[41] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Okutsu, et al.[35] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Zhao, et al.[31] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | |
| LM-only studies | ||||||||
| Lu, et al.[27] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Ullah, et al.[47] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Lee, et al.[34] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ||
| Kook, et al.[33] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ |
| Xiao, et al.[28] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | |
| Erdoğan, et al.[44] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
| Liu, et al.[46] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | |
| Li, et al.[29] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | |
| Kobayashi, et al.[32] | ☆ | / | ☆ | ☆ | / | ☆ | ☆ | ☆ |
Statistical Analysis
We descriptively analyzed the baseline characteristics, surgical angiographic characteristics, clinical outcomes and, if available, angiographic outcomes among patients whose bifurcation lesions were treated with DCBs. According to our search results, the studies can be divided into two groups: studies targeting only bifurcation lesions at the LMCA (so-called LM-only studies) and studies including all bifurcation lesion locations (so-called nonselective bifurcation lesion studies). Quantitative data with a normal distribution are expressed as the mean ± SD, and categorical data are expressed as a percentage (%).
RESULTS
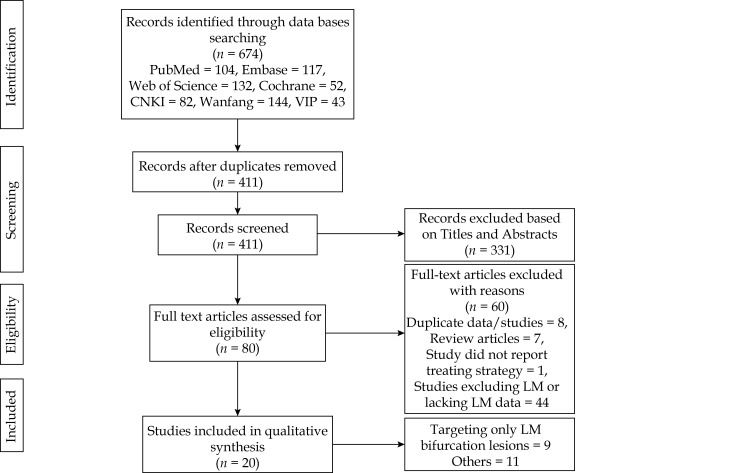
A total of 674 studies were identified. We removed 263 duplicate studies and excluded 331 studies based on their titles and abstracts. After screening of the full text, 60 articles were excluded for various reasons. Eight articles were duplicates, 7 articles were review articles, 1 study did not report the treatment strategy, and 44 studies excluded the LMs or lacked LM data. Twenty studies in which the LM bifurcation lesions were treated with DCBs were included in the qualitative analysis.[27–47] Among these studies, 9 focused on LM bifurcation lesions,[27–29,32–34,44,46,47] while another 11 included bifurcation lesions in all coronaries. [30,31,35–41,43,45] Figure 1 shows the flow chart for literature screening.
Figure 1.
Flow chart for literature screening (PRISMA flow diagram).
LM: left main.
Baseline Characteristics and Interventions
Tables 2 and 4 show the characteristics and angiographic results of the studies included in our qualitative synthesis (18 retrospective studies and 2 prospective studies). Ten studies reported the treatment of bifurcation lesions with DCBs alone (the DCB-only strategy);[27,33–38,41,42,47] among them, there were three studies in which completed lesion preparation was via directional coronary atherectomy (DCA).[35,41,42] Ten studies involved implantation of DES or BVS at the main branch, and the side branch was treated with DCB angioplasty (DCB + stent strategy).[28–31,39,40,43–46] De novo bifurcation lesions were more common than ISR, which can be observed in 4 DCB-only studies.[33,34,36,37] In studies including all types of lesion locations, LM bifurcation lesions varied widely from 2.5% to 80.6%.[30,31,35–41,43,45] True bifurcation lesions can be seen in all nonselective bifurcation lesion studies.[30,31,35–41,43,45] However, in the LM-only group, Ullah, et al.[47] included only Medina classification (1,1,0) bifurcation lesions with substantially compromised side branches after main branch stenting. Erdoğan, et al. focused on LM coronary artery disease with Medina (0, 1, 0) and (0, 0, 1).[44] Supplementary Tables 1 and 2 describe the baseline characteristics of the patients in the two different groups. The majority of the patients in the two groups were male, with a mean age of 64.92 years (62.51 years for the LM-only group[27–29,32–34,44,46,47] and 66.59 years for the nonselective bifurcation lesion group[30,31,35–41,43,45]). Diabetes mellitus (DM) and hypertension (HTN) were common, and nearly half of the studies excluded patients admitted with acute myocardial infarction.[27–29,32,35,37,41,43] Generally, patients in the LM-only studies had better left ventricular function (LVEF) than did those in the other group (59.03 vs. 58.88).[27–47]
Table 2. Characteristics and angiographic results of studies only targeting bifurcation lesion at LMCA.
| Author | Year | Design | Treatment | Simple Size | Lesion Type | CBL Type (Medina) | True bifurcation (%) |
NOS |
| restenosis/de novo | ||||||||
| *Only 116 patients with FFR < 0.8 was treated; **evaluated without the scale entries of selection of the nonexposed cohort and comparability of cohorts on the basis of the design or analysis. ***only included de novo LM stem coronary artery disease with Medina classification (1, 1,0), significant ostial LCx lesion as evidenced by angiographic diameter stenosis (DS > 50%) after MV stenting were enrolled. CB: conventional balloon; CBL: coronary bifurcation lesion; DCA: directional coronary atherectomy; DCB: drug-coated balloon; DES: drug-eluting balloon; LM: left main; LMCA: left main coronary artery; pDES: provisional DES. | ||||||||
| Lu, et al.[27] | 2021 | Retrospective, single-arm study |
DCB | 35 | De novo | All type except (1, 0, 0) | 34.3 | 6** |
| Kobayashi, et al.[32] | 2021 | Retrospective, single-arm study |
DCB | 31 | De novo | Ang type | 3.0 | 6** |
| Lee, et al.[34] | 2018 | Retrospective, comparative study | DCB | 75 | ISR | Ang type | 37.4 | 6 |
| DES | 29 | ISR | 41.3 | |||||
| Kook, et al.[33] | 2020 | Retrospective, comparative study | DCB | 24 | ISR | Ang type except (1, 0, 1) | 29.2 | 9 |
| DES | 51 | ISR | 27.5 | |||||
| Xiao, et al.[28] | 2020 | Retrospective, single-arm study |
DES + DCB | 8 | De novo | (1, 1, 1) (1, 0, 1) (0, 1, 1) | 100.0 | 5** |
| Erdoğan, et al.[44] | 2022 | Prospective, multicenter study |
DCB + pDES | 30 | De novo | (0, 1, 0) (0, 0, 1) | 0.0 | 6** |
| Liu, et al.[46] | 2022 | Retrospective, comparative study | DES + DCB | 50 | De novo | (1, 1, 1) (1, 0, 1) (0, 1, 1) | 100.0 | 7 |
| 2-DES | 50 | De novo | ||||||
| Ullah, et al.[47] | 2021 | Retrospective, comparative study | DES + DCB/DES/CB | 563 (116) * | De novo | (1, 1, 0) *** | 0.0 | 6** |
| Li, et al.[29] | 2019 | Retrospective, comparative study | DES + DCB | 44 | NA | (1, 1, 1) | 100.0 | 7 |
| 2-DES | 58 | NA | ||||||
| DES + CB | 66 | NA | ||||||
Table 4. Characteristics and angiographic results of nonselective bifurcation lesion studies.
| Author | Year | Design | Treatment | Simple size | Lesion type | LM bifurcation lesion |
CBL Type (Medina) |
True bifurcation (%) |
NOS |
| Restenosis/de novo | |||||||||
| *Evaluated without the scale entries of selection of the nonexposed cohort and comparability of cohorts on the basis of the design or analysis. BVS: Bioabsorbale Vessel Scarfolding; CB: conventional balloon; DCA: directional coronary atherectomy; DCB: drug-coated balloon; DES: drug-eluting balloon; LM: left main; NOS: Newcastle‒Ottawa Scale; pDES: provisional DES. | |||||||||
| Schulz, et al.[38] | 2014 | Retrospective, single-arm study |
DCB | 38 | De novo | 33.3 | all type | 28.4 | 6* |
| Harad, et al.[36] | 2017 | Retrospective, single-arm study |
DCB | 177 | ISR | 45.8 | all type | 52.5 | 5* |
| Kitani,et al.[41] | 2021 | Retrospective, multicenter, single-arm study |
DCB | 129 | De novo | 80.6 | all type | 14.0 | 6* |
| Okuts,et al.[35] | 2022 | Retrospective, single-arm study |
DCB | 24 | De novo | 59.3 | all type except (0,0,1) | 25.9 | 6* |
| Naganuma, et al.[37] | 2016 | Retrospective, multi-center, comparative study study |
DCB |
73 | ISR | 24.4 | all type | 67.9 | 8 |
| DES | 85 | ISR | 23.6 | 57.3 | |||||
| Ikuta, et al.[40] | 2021 | Retrospective, single-arm study |
DCB + DES | 138 | De novo | 15.2 | (1,1,1) (1,0,1) (0,1,1) | 100.0 | 6* |
| Zhao, et al.[31] | 2017 | Retrospective, single-arm study |
DCB + DES | 20 | De novo | 15.0 | (1,1,1) (1,0,1) (0,1,1) | 100.0 | 5* |
| Elwany, et al.[39] | 2019 | Retrospective, multi-center, single-arm study |
DCB + BVS | 40 | De novo | 2.5 | all type | 72.5 | 6* |
| Li, et al.[43] | 2021 | Retrospective, comparative study |
DCB + DES | 102 | De novo | 58.8 | (1,1,1) (1,0,1) (0,1,1) | 100.0 | 8 |
| CB + DES | 117 | De novo | 39.3 | 100.0 | |||||
| Herrador, et al.[45] | 2013 | Prospective, comparative study |
DCB + DES | 50 | NA | 8.0 | all type | 56.0 | 8 |
| CB + DES | 50 | NA | 12.0 | 48.0 | |||||
| Yang, et al.[30] | 2020 | Retrospective, comparative study |
DCB + DES | 29 | NA | 3.4 | (1,1,1) (1,0,1) (0,1,1) | 100.0 | 8 |
| CB + DES | 31 | NA | 3.2 | 100.0 | |||||
Clinical and Angiographic Outcomes
Tables 3 and 5 show the clinical and angiographic outcomes of the included studies. The studies were divided into DCB-only and DCB + stent groups according to the use of DCB. Among the LM-only bifurcation lesion studies, four included the DCB-only strategy.
Table 3. Outcomes of studies only targeting bifurcation lesion at LMCA.
| Author | Follow up | Treatment | LLL | Restenosis | MACE | ||||||
| MB (mm) | SB (mm) | MB (%) | SB (%) | TLR (%) | MI (%) | Death (%) | |||||
| *SD was unavailable. BVS: Bioabsorbale Vessel Scarfolding; CB: conventional balloon; CBL: coronary bifurcation lesion; DCA: directional coronary atherectomy; DCB: drug-coated balloon; DES: drug-eluting balloon; LAD: left anterior descending; LCx: left circumflex; LLL: late lumen loss; LM: left main; LMCA: left main coronary artery; MACE: major adverse cardiac event; MB: main branch; MI: myocardial infarction; pDES: provisional DES; SB: side branch; TLR: target lesion revascularization. | |||||||||||
| Lu, et al.[27] | 6 months | DCB | LM: 0.2 ± 0.2; LAD: -0.0 ± 0.2; LCx: -0.1 ± 0.3 |
NA | NA | 2.9 | 0.0 | 0.0 | |||
| Kobayashi, et al.[32] | 12 months | DCB | 0.1 ± 0.5 | NA | NA | 3.2 | 0.0 | 0.0 | |||
| Lee, et al.[34] | 12 months | DCB | NA | NA | NA | NA | 16.4 | 6.0 | 0.0 (cardiac) 6.8 (all cause) |
||
| DES | NA | NA | NA | NA | 16.7 | 12.5 | 10.7 (cardiac) 21.4 (all cause) |
||||
| Kook, et al.[33] | 12 months | DCB | 1.1 ± 1.1 | 46.2 | 16.7 | 0.0 | 0.00 | ||||
| DES | 0.6 ± 0.9 | 20.0 | 21.6 | 2.0 | 2.0 (cardiac) 3.9 (all cause) |
||||||
| Xiao, et al.[28] | 6M | DES + DCB | LM: 0.3 LAD: 0.1 LCx: 0.3* | NA | NA | NA | NA | NA | |||
| Erdoğan, et al.[44] | 6 months | DCB + pDES/DES | -0.3 ± 0.5 | NA | NA | 0.0 | 0.0 | 0.0 | |||
| Liu, et al.[46] | 12 months | DES + DCB | LM: 0.1 LAD: 0.2 LCx: -0.2* | 15.4 | 7.7 | 6.0 | 0.0 | 0.0 | |||
| 2-DES | LM: 0.2 LAD: 0.2 LCx: 0.4* | 8.6 | 30.4 | 12.0 | 2.0 | 0.0 | |||||
| Ullah, et al.[47] | 36 months | DES + DCB | NA | NA | NA | NA | 0.0 | 5.4 | |||
| 2-DES | NA | NA | NA | NA | 7.7 | 10.3 | |||||
| DES + CB | NA | NA | NA | NA | 10.0 | 5.0 | |||||
| Li, et al.[29] | 12 months | DES + DCB | NA | NA | NA | 12.5 | 4.2 | 0.0 | |||
| 2-DES | NA | NA | NA | 10.3 | 5.2 | 1.7 (cardiac) | |||||
| DES + CB | NA | NA | NA | 7.6 | 3.0 | 1.5 (cardiac) | |||||
Table 5. Outcomes of nonselective bifurcation lesion group.
| Author | Follow up | Treatment | LLL | Restenosis | MACE | ||||||
| MB (mm) | SB (mm) | MB (%) | SB (%) | TLR (%) | MI (%) | Death (%) | |||||
| *SD was unavailable. BVS: Bioabsorbale Vessel Scarfolding; CB: conventional balloon; CBL: coronary bifurcation lesion; DCA: directional coronary atherectomy; DCB: drug-coated balloon; DES: drug-eluting balloon; LAD: left anterior descending; LCx: left circumflex; LLL: late lumen loss; LM: left main; MACE: major adverse cardiac event; MB: main branch; MI: myocardial infarction; pDES: provisional DES; SB: side branch; TLR: target lesion revascularization. | |||||||||||
| Schulz, et al.[38] | 4M | DCB | NA | NA | 6.7 | 3.3 | 7.7 | 0.0 | 0.0 | ||
| Harada, et al.[36] | 6M | DCB | -0.1* | 0.2* | 7.2 | 16.8 | 22.0 | 0.0 | 2.0 (all cause) | ||
| Kitani, et al.[41] | 12M | DCB | 0.3 ± 0.5 | 2.3 | 3.1 | 0.8 | 0.0 | ||||
| Okutsu, et al.[35] | 3M | DCB | 0.2 ± 0.6 | NA | NA | 0.0 | 0.0 | 0.0 | |||
| Naganuma, et al.[37] | 24M | DCB | NA | NA | NA | NA | 16.6 | 0.0 | 5.0 (cardiac) | ||
| DES | NA | NA | NA | NA | 17.6 | 0.0 | 2.6 (cardiac) | ||||
| Ikuta, et al.[40] | 12M | DCB + DES | 0.4 ± 0.7 | -0.1 ± 0.4 | 4.3 | 8.0 | 2.1 | 0.7 | 0.7 (cardiac) | ||
| Zhao, et al.[31] | 6M | DCB + DES | NA | NA | NA | NA | 0.0 | 0.0 | 0.0 | ||
| Elwany, et al.[39] | 6M | DCB + BVS | -0.2* | 0.1* | 0.0 | 2.5 | 0.0 | 2.5 | 0.0 | ||
| Li, et al.[43] | 12M | DCB + DES | 0.1 ± 0.1 | 0.1 ± 0.2 | NA | 4.9 | NA | 2.9 | 1.0 (cardiac) | ||
| CB + DES | 0.1 ± 0.1 | 0.2 ± 0.2 | NA | 7.7 | NA | 6.0 | 0.9 (cardiac) | ||||
| Herrador, et al.[45] | 12M | DCB + DES | 0.5 ± 0.6 | 0.1 ± 0.4 | 12.5 | 7.5 | 12.0 | 0.0 | 0.0 | ||
| CB + DES | 0.6 ± 0.7 | 0.4 ± 0.5 | 18.6 | 20.9 | 22.0 | 2.0 | 0.0 | ||||
| Yang, et al.[30] | 9M | DCB + DES | 0.2 ± 0.4 | 0.0 ± 0.7 | NA | NA | NA | 0.0 | 0.0 | ||
| CB + DES | 0.3 ± 0.4 | 0.6 ± 0.6 | NA | NA | NA | 0.0 | 0.0 | ||||
Lu,, et al. performed a prospective, single-arm study treating de novo lesions with DCB angioplasty.[27] Of those, true bifurcation lesions accounted for 34.3%. After the procedure, the stenosis of coronary arteries was significantly relieved, and the MLDs of the target vessels continued to improve at follow-up in more than 50% of patients (LLL: LM 0.16 ± 0.21 mm, LAD: -0.02 ± 0.18 mm, LCx: -0.07 ± 0.25 mm). For the clinical outcomes, no deaths or MIs were reported, and the incidence of TLR was only 2.86% at the 6-month follow-up, which was comparable to the performance of DESs in the DEBIUT registry, with no MACEs occurring at the 4-month follow-up.[19]
Kobayashi, et al.[42] predilated target vessels with DCA and treated the de novo bifurcation lesions with the DCB technique. In their study, the ostium of the left anterior descending (LAD) artery was the most common lesion, accounting for 68% of cases. After treatment with the DCB technique, the target vessel MLD increased from 1.30 ± 0.40 mm to 3.40 ± 0.90 mm, with a preprocedure reference lumen diameter (RLD) of 3.9 ± 1.1 mm. For clinical and angiographic outcomes, Kobayashi, et al. reported more favorable results than did the trials by Chen, et al., who used a pDES strategy to treat LM bifurcation lesions.[42,48] The LLL in the study of Kobayashi, et al. was 0.10 ± 0.50 mm, and the 1-year cumulative incidence of TLR at follow-up was as low as 3.2%. However, Chen, et al. reported that the main branch (MB) LLL was 0.23 ± 0.35 mm, the side branch (SB) LLL was 0.28 ± 0.55 mm, and the incidence of TLR reached 7.9% at the 12-month follow-up.[48]
Lee, et al. and Kook, et al. compared the performance of DCB to that of DES in dealing with ISR bifurcation lesions.[33,34] In Lee, et al.’s study, (0,0,1) was the most common type of bifurcation in the DCB group (accounting for 37.3%), while in the DES group, (1,1,1) and (0,1,0) were more common than other bifurcation lesions (together accounting for more than 40%). However, there was no difference in bifurcation type between the two strategy groups in the study by Kook, et al. with (0,1,0), which was observed in more than 50% of patients, and the DCB group tended to more frequently have stent-in-stent cases (25% vs. 7.8%, P = 0.07) than did the DES group. After the procedure, the MLD significantly improved in the two strategy groups. Kook, et al.’s study showed that the DCB group had smaller postprocedure MLDs of the target lesions (P = 0.03), but the DCB technique resulted in a greater LLL than did the DES (1.06 ± 1.10 vs. 0.60 ± 0.85, P = 0.23). For clinical outcomes, the two LM-ISR treatment studies reported a higher rate of TLR in both technique groups, and a lower incidence of mortality and MI was observed in the DCB group than in the DES group at the 12-month follow-up.
In five studies, bifurcation lesions were treated with DESs implanted in the main branch and DCBs used for side branch angioplasty.
Ullah, et al.[47] included only de novo (1,0,0) bifurcation lesions with a compromised left circumflex (LCx) artery after stenting the main branch. Patients were divided into two groups according to the fractional flow reserve (FFR). Compromised LCx lesions with a low FFR (FFR < 0.8) were treated with a DCB, DES or CB. With a primary endpoint of MACEs at the three-year follow-up, no deaths or TLRs were reported in the DES+DCB group. There was no significant difference among the three techniques in terms of the rate of MACEs (DES+DCB: 8.1%; 2-DES: 20.5%; CB: 17.5%; P = 0.299).
Xiao, et al.[28] performed a prospective, single-arm study using the DCB + DES approach to treat de novo true LM bifurcation lesions. They found that this strategy was effective at reducing stenosis, with side branch diameter stenosis decreasing from 97.1% ± 9.0% to 19.8% ± 10.6%. The follow-up angiographic results showed that the side branch LLL was 0.30 mm, which was similar to the performance of the pDES strategy in the study by Chen, et al. (LLL = 0.28 ± 0.55 mm).[48] No deaths or TLRs were reported at the 6-month follow-up.
Liu, et al. compared the angiographic and clinical outcomes between the DCB + DES and 2-DES groups for treating de novo true LM bifurcation lesions.[46] An increasing trend in the DCB + DES group was observed, which lasted through the follow-up period and resulted in a larger follow-up side branch MLD (1.80 mm vs. 2.41 mm, P = 0.031) and a smaller LLL (-0.17 mm vs. 0.43 mm) than those in the 2-DES group. The incidence of restenosis in the 2-DES group reached 30.4% at the 12-month follow-up, while it was only 7.7% in the DES+DCB group (P > 0.05). There was no significant difference in TLR or mortality between the two strategies.
Li, et al. performed a prospective study targeting (1,1,1) LM bifurcation lesions with LCx diameters ranging from 2.25 mm to 2.75 mm.[29] They found that for the angiographic and clinical outcomes, both the DCB + DES and 2-DES strategies obtained better results than did the DES + CB approach. The DCB + DES strategy had an advantage in relieving side branch stenosis at follow-up (percentages of LLL: 4% ± 5% vs. 11% ± 7% vs. 16% ± 11%). In the DCB + DES group, only 3.22% of patients experienced in-stent restenosis at follow-up. However, 18.60% and 9.76% of patients experienced in-stent restenosis in the 2-DES and DES + CB groups, respectively, experienced in-stent restenosis (P < 0.05), which was similar to the results in the study of Berland, et al.[49] The DES + DCB group had the highest rate of MACEs among the three strategies, which was mainly attributed to a high TLR (12.5% vs. 10.3% vs. 7.58%, P > 0.05).
Erdoğan, et al.[44] performed a prospective, multicenter, proof-of-concept study. They targeted patients admitted with acute coronary syndrome (ACS) having a (0,1,0) or (0,0,1) LM bifurcation lesion. Most of the SB bifurcation lesions were treated with DCBs combined with provisional DESs unless the patients refused or experienced severe dissection, in which case the DES was placed after DCB treatment. This strategy significantly relieved side branch stenosis, with the MLD increasing from 1.00 ± 0.39 mm to 2.25 ± 0.50 mm and the reference vessel diameter (RVD) decreasing from 2.81 ± 0.60 mm to 2.64 ± 0.48 mm after the procedure. This trend continued until the 6-month follow-up, as the LLL was only -0.34 ± 0.48 mm, and no deaths, MIs or TLRs were reported.
Among the nonselective bifurcation lesion studies, five studies utilized a DCB-only strategy.
Schulz, et al.[38] conducted a prospective, single-arm, observational study that involved a DCB-only strategy to treat de novo bifurcation lesions. The LM bifurcation lesions and the true bifurcations accounted for 33.3% and 38.4% of cases, respectively, of the lesions. The restenosis rate (MB 6.67%, SB 3.33%), especially of the side branch, was comparable to or even lower than that after DES treatment, which reported the side branch restenosis rate to be between 11.5% and 19.2% in the Nordic-Baltic Bifurcation Study III,[50] 2.8% and 3.6% in the British Bifurcation Coronary Study.[51] The rate of MACEs was 7.7% at the midterm follow-up, with no deaths or MIs occurring.[38] However, the rate of MACEs at the midterm follow-up varied widely among DES treatment studies, which reported MACEs rates of 15%–15.8% in CACTUS, and of only 2.1%–2.5% in the Nordic-Baltic Bifurcation Study III.[50,52]
Harada, et al.[36] performed the DCB-only strategy for ISR lesions that had been treated with a 2-DES approach before. LM bifurcation lesions accounted for 45.76% of the cases, and true bifurcations were present in 52.5% of the patients. The incidence of restenosis was 24%, and the rate of MACE was 24% at long-term follow-up, which was comparable to the performance of DES in a prior study reporting a MACE rate of 27.6%.[36,37]
Both Kitani, et al. and Okutsu, et al. treated de novo bifurcation lesions with DCA first followed by DCB angioplasty after sufficient debulking without severe dissection.[35,41] The proportions of LM bifurcation lesions in each study were 80.6% and 59.3%, respectively. After the treatment, both studies showed significant improvements in target vessel MLDs (preprocedure 1.80 ± 0.40 mm vs. postprocedure 3.10 ± 0.50 mm, 1.20 ± 0.50 mm vs. 3.10 ± 0.60 mm, respectively). In the study by Kitani, et al., late lumen enlargement, defined as a negative value of LLL, was observed in 28% of the patients.[41] Okutsu, et al. reported that the rate of restenosis was 2.3%, and no deaths were reported at the 3-month follow-up.[35] However, the observation period was too short to reach a conclusion. The overall target vessel LLL in the study of Kitani, et al. was 0.29 ± 0.51 mm, and the incidence of restenosis was 2.3%.[41] The TLR, especially the side branch TLR, was low at the 1-year follow-up because it was only 0.8%. The performance of DCB in Kitani, et al.’s study was comparable to the performance of DES in the PERFECT study, in which bifurcation lesions were also prepared with the DCA technique.[41] In the PERFECT study, the main branch LLL was 0.52 ± 0.53 mm, the side branch LLL was 0.15 ± 0.44 mm, the rate of restenosis was 4.5%, and the percentage of patients with TLR was 2% at the 12-month follow-up.[53]
Naganuma, et al.’s prospective study compared DCB with second-generation DESs in treating ISR bifurcation lesions.[37] Naganuma, et al. reported a higher rate of MACEs in the DCB group than in the DES group (32.1% vs. 27.6%, P = 0.593). This could be explained by the higher incidence of stent-in-stent lesions in the DCB group than in the DES group, which was an independent predictor of MACEs. Moreover, the high rate of MACEs was mainly attributed to TLR, which reached 16.6% in the DCB group and 17.6% in the DES group. Patients with restenosis caused by second-generation DESs (26.9% vs. 6.7%, P < 0.001), restenosis caused by both the MB and SB (42.3% vs. 25.8%, P = 0.025) or restenosis caused by stent-in-stent lesions (25.6% vs. 14.6%, P = 0.074) were more likely to be treated with DCBs in this study.
Among the nonselective bifurcation lesion studies, five involve a DCB + stent strategy.
LM bifurcation lesions accounted for approximately 15% of the cases in the single-arm retrospective studies by Ikuta, et al. and Zhao, et al..[31,40] In both studies, authors were specifically concerned about de novo true bifurcation lesions and treated bifurcation with DCB angioplasty for the side branch before or after main branch DES implantation. Ikuta, et al. reported that the MLD of the side branch increased from 0.69 ± 0.58 mm to 1.33 ± 0.47 mm with a 2.02 ± 0.66 mm preprocedure RVD after DES + DCB treatment. In Ikuta, et al.’s study,[40] the DES + DCB strategy achieved excellent angiographic performance, with a side branch LLL at the 12-month follow-up of only −0.14 mm, which was smaller than that in prior studies in which the DES + CB strategy or 2-DES strategy was conducted (the SB LLL was 0.05 ± 0.31 mm in DES+CB, and the SB LLL was 0.29 ± 0.52 mm in 2-DES).[52,54] A study by Ikuta, et al.[40] showed that the rate of MACEs was 2.9%, with 2.1% of patients having TLR. No MACEs occurred during the 6-month follow-up in the study of Zhao, et al., which was more favorable than that in the study involving the DES + CB or 2-DES strategy. In the DES + CB strategy study, the rate of MACEs was 14%, and TLR was 7%, whereas in the 2-DES study, the rate of MACEs was 18%, and TLR was 7.3%.
Elwany, et al.[39] reported a retrospective, multicenter, single-arm study in which de novo bifurcation lesions were treated with a DCB + BVS strategy. At least one BVS was implanted in the main branch followed by DCB angioplasty of one or more side branches, and no bailout stent was required in the side branch. LM bifurcation lesions were observed in only 2.5% of patients, but the proportion of true bifurcation lesions reached 72.5%. The angiographic outcomes showed that the main branch LLL was -0.20 mm and that the side branch LLL was 0.12 mm. During the 6-month follow-up, no deaths or TLRs were reported, and the rate of MACEs was comparable to that in the studies using BVS to treat bifurcation lesions with or without DESs.[55–57]
Li, et al., Herrador, et al. and Yang, et al. compared the performance of DES + DCB to that of DES + CB in treating bifurcation lesions with DESs implanted in the main branch and DCBs or CBs used for side branch angioplasty.[30,43,45] Li, et al.[43] and Yang, et al.[45] focused on true bifurcation lesions, while all types of bifurcations were included in the study by Herrador, et al.[45] The proportions of left main bifurcation lesions differed widely among the three studies (48.4% vs. 10.0% vs. 3.3%), although they reached the same conclusion that the clinical and angiographic results were favorable for the DCB technique. In Herrador, et al.’s study,[45] DCBs performed better at reducing adverse events at follow-up, especially for reducing TLR (12% vs. 22%), than CBs did. Regarding angiographic outcomes, an advantage of side branch protection was observed in the DCB group, in which the LLL was smaller (0.4 mm vs. 0.09 mm, P = 0.01) and the rate of restenosis was lower (7.5% vs. 20.9%, P = 0.08). Similarly, Yang, et al.[43] also reported more favorable outcomes in the DCB group than in the CB group (LLL 0.03 ± 0.74 mm vs. 0.62 ± 0.64 mm, P = 0.002; MACEs 3.4% vs. 6.5%, P > 0.05). Li, et al. reported that although no significant difference in the main branch LLL was observed between the two groups (P > 0.05), the side branch LLL in the DCB group was smaller than that in the CB group (0.11 ± 0.18 mm vs. 0.19 ± 0.25 mm, P = 0.024). For the clinical outcomes, Li, et al. reported no significant difference in the restenosis incidence between the two strategies, but even after adjusting for compounding factors, multivariate analyses showed that DCBs still had a lower MACE risk than did CBs (P = 0.033).
DISCUSSION
LM bifurcation lesions are a common type of LMCA disease. Currently, the European Bifurcation Club recommends provisional DES or 2-DES as the standard PCI strategy for LM bifurcation.[58] DCBs have the advantages of releasing drugs to the arterial wall to inhibit endothelial hyperplasia without leaving stent struts and leaving room for follow-up treatment.[60,61] The use of DCBs is increasing in bifurcation lesions, but in LMs, their usage is still limited, which is mainly attributed to the unsatisfactory lesion preparation and the requirement for long inflation times considering the importance of these anatomical sites. Several studies have explored the use of DCBs in LM bifurcation lesions, but there are no comprehensive analyses to support this strategy. Thus, we performed this systematic review to evaluate the safety and efficacy of DCBs in treating LM bifurcation lesions.
The present systematic review involved a qualitative analysis, which included 20 studies with a total of 2217 patients. Eighteen of the included studies were retrospective studies, and 2 were prospective studies. Meta-analysis could not be performed due to the significant clinical and methodological heterogeneity and a lack of RCTs. The main findings of our systematic review can be summarized as follows: (1) DCBs achieved noninferior or even superior angiographic and clinical outcomes at the midterm follow-up in treating LM bifurcation lesions compared with DESs or CBs, whether for de novo or ISR lesions. (2) DCBs may have the advantages of side branch protection and hold the potential in treating stent-in-stent lesions.
For de novo bifurcation lesions, two different strategies are used to perform DCB angioplasty. Some of these studies used a DCB-only strategy to relieve vessel stenosis and completed at least a 3-month follow-up period. Among those, Kobayashi, et al., Kitani, et al. and Okutsu, et al. predilated the bifurcation lesions with DCA and achieved good performance. The DCB-only strategy resulted in a small target vessel LLL and a low incidence of MACEs, which was reported to be only 3.2%-7.7%, with no deaths occurring at the 12-month follow-up.[28,33,39,36,42] These results were comparable to the performance of the provisional DES strategy in treating de novo bifurcation lesions.[48] The other studies treated the side branch with a DCB, DES or CB after main branch stenting. Compared with DESs or CBs, DCB angioplasty resulted in a smaller side branch LLL and a lower rate of restenosis and MACEs at the midterm follow-up.[29,32,41,44,47] The incidence of MACEs in the included studies was 1.4%–6.0% in the DES+DCB group, 15% in the DES+CB group and 14%–18% in the 2-DES group, which was consistent with the results of a recent meta-analysis regarding the LM bifurcation stenting strategy. In this meta-analysis, the incidence rates of MACEs in the groups treated with the DES + CB and 2-DES strategies were 15.2% and 19.3%, respectively, at the 12-month follow-up.[59]
Several RCTs that excluded LM lesions evaluated the efficacy and safety of DCBs for the treatment of ISR lesions, and the results were comparable to those of DESs.[18,21,22,24] Similarly, no significant difference in angiographic or clinical outcomes was observed between DCBs and DESs in this systematic review (P > 0.05).[34,35,37,38] ISR lesions had a higher rate of MACEs, which was mainly attributed to a higher rate of TLR, than that of de novo lesions. Furthermore, compared with those in the DES group, the DCB group tended to have more frequent the stent-in-stent cases, which were reported to be approximately 25%. Although stent-in-stent lesions are more prone to restenosis, the rate of TLR in the DCB group remained lower than that in the DES group.
Moreover, the MLD of the side branch was observed to have a tendency to increase after DCB angioplasty, which continued through the follow-up period and even resulted in side branch late lumen enlargement, defined as a negative value for LLL.[28,41,45,47] This finding suggested that DCBs may have the advantage of side branch protection. There is no consensus on which group of patients would benefit the most from treatment with DCBs, and these findings provide additional evidence for the use of DCBs in affected side branches.
For the stenting strategy in LM bifurcation lesions, Chen, et al. used the DEFINITION criteria to determine complex lesions and guide PCI strategies (pDES vs. 2-DES).[48] Despite the increasing usage of this approach, criteria for the DCB strategy are still lacking. In most of the included studies, DCB angioplasty was performed unless there was evidence of satisfactory lesion preparation (i.e., thrombolysis in myocardial infarction (TIMI) III flow, absence of residual stenosis > 30% of the MB or > 75% of the SB and dissection no more than grade B according to the NHLBI classification).[60] Furthermore, the use of DCBs may be more effective for some specific lesions (i.e., side branch lesions and stent-in-stent lesions) than for others. Thus, a standard approach that takes various factors into consideration is needed to guide DCB angioplasty in LM bifurcation lesions.
Considering the importance and complexity of LMCAs, many surgeons are worried about the uncertain risks of DCB use and preferring to use stents. However, our systematic review showed that the use of DCBs for treating LM bifurcation lesions was comparable to the use of DCBs for treating non-LM bifurcation lesions, even though LMCA lesions had an obviously higher risk and poorer prognosis. Moreover, for both de novo and ISR lesions, there were no significant differences in the angiographic or clinical results after treatment with DCBs. Thus, the use of DCBs in LM bifurcation lesions was safe and effective on the basis of satisfactory predilation. However, this conclusion was based on nRSs, which inevitably contain heterogeneity and therefore require confirmation by large-scale RCTs; additional studies are needed to provide solid evidence for the use of DCBs in LM bifurcation lesions.
There were several limitations in our review. First, no RCTs were available, and only studies published in English or Chinese were included in this systematic review, which led to potential selection bias. Second, some of the included studies were single-arm observational studies with small sample sizes, and their rates of clinical events were highly heterogeneous. Third, bifurcation lesions were classified by Medina, and this standard does not account for other important factors, such as the bifurcation angle, extent of the main branch/side branch, vessel diameter, TIMI flow or combined calcification. Fourth, second-generation DESs may have better angiographic and clinical outcomes than first-generation DESs.[18,61] However, we did not report the specific types of DCBs or DESs, which may hamper the interpretation of the included studies.
In conclusion, this systematic review summarized and qualitatively analyzed the study characteristics, baseline data, and clinical and angiographic outcomes of DCB use for LM bifurcation lesions. Based on our descriptive analysis, the DCB technique has favorable safety and efficacy profiles for the treatment of left main bifurcation lesions. More studies, especially randomized controlled trials, are needed to help set standards for the use of the DCB technique and to demonstrate the safety and effectiveness of DCBs in treating LM bifurcation lesions.
DECLEARATIONS
SUPPLEMENTARY DATA
Supplementary data to this article can be found online.
Author Contributions
Yang Cheng: Methodology, Software, Validation, Formal analysis, Investigation, Resources, Data curation, Writing-Original Draft, Writing-Review and Editing, Visualization. Yong Chen: Methodology, Software, Validation, Resources, Data curation, Writing-Original Draft, Writing-Review and Editing. Baotao Huang: Conceptualization, Methodology, Validation, Formal analysis, Writing-Review and Editing, Supervision. Mao Chen: Conceptualization, Writing-Review and Editing, Supervision, Project administration. All authors have read and agreed to the published version of the manuscript.
Funding Statement
None.
Conflict of Interest
None.
References
- 1.Patel MR, Dehmer GJ, Hirshfeld JW, et al ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: A Report of the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology: Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. Circulation. 2009;119:1330–1352. doi: 10.1161/CIRCULATIONAHA.108.191768. [DOI] [PubMed] [Google Scholar]
- 2.Chieffo A, Meliga E, Latib A, et al Drug-eluting stent for left main coronary artery disease. The DELTA registry: a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment. JACC Cardiovasc Interv. 2012;5:718–727. doi: 10.1016/j.jcin.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 3.Morice MC, Serruys PW, Kappetein AP, et al Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645–2653. doi: 10.1161/CIRCULATIONAHA.109.899211. [DOI] [PubMed] [Google Scholar]
- 4.Park DW, Seung KB, Kim YH, et al Long-term safety and efficacy of stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 5-year results from the MAIN-COMPARE (Revascularization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization) registry. J Am Coll Cardiol. 2010;56:117–124. doi: 10.1016/j.jacc.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Park SJ, Kim YH, Park DW, et al Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364:1718–1727. doi: 10.1056/NEJMoa1100452. [DOI] [PubMed] [Google Scholar]
- 6.Stone GW, Kappetein AP, Sabik JF, et al Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med. 2019;381:1820–1830. doi: 10.1056/NEJMoa1909406. [DOI] [PubMed] [Google Scholar]
- 7.Ragosta M Left main coronary artery disease: importance, diagnosis, assessment, and management. Curr Probl Cardiol. 2015;40:93–126. doi: 10.1016/j.cpcardiol.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Kim WJ, Kim YH, Park DW, et al Comparison of single- versus two-stent techniques in treatment of unprotected left main coronary bifurcation disease. Catheter Cardiovasc Interv. 2011;77:775–782. doi: 10.1002/ccd.22915. [DOI] [PubMed] [Google Scholar]
- 9.Lassen JF, Holm NR, Stankovic G, et al Percutaneous coronary intervention for coronary bifurcation disease: consensus from the first 10 years of the European Bifurcation Club meetings. EuroIntervention. 2014;10:545–560. doi: 10.4244/EIJV10I5A97. [DOI] [PubMed] [Google Scholar]
- 10.Lee CH, Choi SW, Hwang J, et al 5-Year Outcomes According to FFR of Left Circumflex Coronary Artery After Left Main Crossover Stenting. JACC Cardiovasc Interv. 2019;12:847–855. doi: 10.1016/j.jcin.2019.02.037. [DOI] [PubMed] [Google Scholar]
- 11.Xu J, Hahn JY, Song YB, et al Carina shift versus plaque shift for aggravation of side branch ostial stenosis in bifurcation lesions: volumetric intravascular ultrasound analysis of both branches. Circ Cardiovasc interv. 2012;5:657–662. doi: 10.1161/CIRCINTERVENTIONS.112.969089. [DOI] [PubMed] [Google Scholar]
- 12.Fujino Y, Attizzani GF, Tahara S, et al Difference in vascular response between sirolimus-eluting- and everolimus-eluting stents in ostial left circumflex artery after unprotected left main as observed by optical coherence tomography. Int J Cardiol. 2017;230:284–292. doi: 10.1016/j.ijcard.2016.12.122. [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Lee JH, Roh JH, et al Randomized Comparisons Between Different Stenting Approaches for Bifurcation Coronary Lesions With or Without Side Branch Stenosis. JACC Cardiovasc Interv. 2015;8:550–560. doi: 10.1016/j.jcin.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 14.Kume T, Yamada R, Terumasa K, et al Neointimal coverage of jailed side branches in coronary bifurcation lesions: an optical coherence tomography analysis. Coron Artery Dis. 2018;29:114–118. doi: 10.1097/MCA.0000000000000563. [DOI] [PubMed] [Google Scholar]
- 15.Loh JP, Barbash IM, Waksman R The current status of drug-coated balloons in percutaneous coronary and peripheral interventions. EuroIntervention. 2013;9:979–988. doi: 10.4244/EIJV9I8A164. [DOI] [PubMed] [Google Scholar]
- 16.Corballis NH, Wickramarachchi U, Vassiliou VS, Eccleshall SC. Duration of dual antiplatelet therapy in elective drug-coated balloon angioplasty. Catheter Cardiovasc Interv 2020;96: 1016–1020.
- 17.Lee JM, Park J, Kang J, et al Comparison among drug-eluting balloon, drug-eluting stent, and plain balloon angioplasty for the treatment of in-stent restenosis: a network meta-analysis of 11 randomized, controlled trials. JACC Cardiovasc Interv. 2015;8:382–394. doi: 10.1016/j.jcin.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Byrne RA, Neumann FJ, Mehilli J, et al Paclitaxel-eluting balloons, paclitaxel-eluting stents, and balloon angioplasty in patients with restenosis after implantation of a drug-eluting stent (ISAR-DESIRE 3): a randomised, open-label trial. Lancet. 2013;381:461–467. doi: 10.1016/S0140-6736(12)61964-3. [DOI] [PubMed] [Google Scholar]
- 19.Fanggiday JC, Stella PR, Guyomi SH, Doevendans PA Safety and efficacy of drug-eluting balloons in percutaneous treatment of bifurcation lesions: the DEBIUT (drug-eluting balloon in bifurcation Utrecht) registry. Catheter Cardiovasc Interv. 2008;71:629–635. doi: 10.1002/ccd.21452. [DOI] [PubMed] [Google Scholar]
- 20.Kleber FX, Rittger H, Ludwig J, et al Drug eluting balloons as stand alone procedure for coronary bifurcational lesions: results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 2016;105:613–621. doi: 10.1007/s00392-015-0957-6. [DOI] [PubMed] [Google Scholar]
- 21.Kufner S, Cassese S, Valeskini M, et al Long-Term Efficacy and Safety of Paclitaxel-Eluting Balloon for the Treatment of Drug-Eluting Stent Restenosis: 3-Year Results of a Randomized Controlled Trial. JACC Cardiovasc Interv. 2015;8:877–884. doi: 10.1016/j.jcin.2015.01.031. [DOI] [PubMed] [Google Scholar]
- 22.Lee WC, Fang YN, Fang CY, et al Comparison of Clinical Results Following the Use of Drug-Eluting Balloons for a Bare-Metal Stent and Drug-Eluting Stent Instent Restenosis. J Interv Cardiol. 2016;29:469–479. doi: 10.1111/joic.12327. [DOI] [PubMed] [Google Scholar]
- 23.Mathey DG, Wendig I, Boxberger M, Bonaventura K, Kleber FX Treatment of bifurcation lesions with a drug-eluting balloon: the PEPCAD V (Paclitaxel Eluting PTCA Balloon in Coronary Artery Disease) trial. EuroIntervention. 2011;7:K61–K65. doi: 10.4244/EIJV7SKA11. [DOI] [PubMed] [Google Scholar]
- 24.Unverdorben M, Vallbracht C, Cremers B, et al Paclitaxel-coated balloon catheter versus paclitaxel-coated stent for the treatment of coronary in-stent restenosis: the three-year results of the PEPCAD II ISR study. EuroIntervention. 2015;11:926–934. doi: 10.4244/EIJY14M08_12. [DOI] [PubMed] [Google Scholar]
- 25.Wöhrle J, Zadura M, Möbius-Winkler S, et al SeQuentPlease World Wide Registry: clinical results of SeQuent please paclitaxel-coated balloon angioplasty in a large-scale, prospective registry study. J Am Coll Cardiol. 2012;60:1733–1738. doi: 10.1016/j.jacc.2012.07.040. [DOI] [PubMed] [Google Scholar]
- 26.Worthley S, Hendriks R, Worthley M, et al Paclitaxel-eluting balloon and everolimus-eluting stent for provisional stenting of coronary bifurcations: 12-month results of the multicenter BIOLUX-I study. Cardiovasc Revasc Med. 2015;16:413–417. doi: 10.1016/j.carrev.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Lu Y GH, Liu HD, Xing JH, Li L Treatment of Left Main Coronary Artery Bifurcation Lesion with Drug Coated Balloon-Only Strategy. Henan Med Res. 2021;30:989–993. [Google Scholar]
- 28.Xiao RX WX, Hao JQ, Liu ZJ The application of drug-eluting stent combined with drug coated balloon in treating coronary lesions located at left main bifurcation site. J Interv Radiol. 2020;29:350–354. [Google Scholar]
- 29.Li M ZY, Chen Y, An ST, et al Efficacy of Drug Coated Balloon for the Treatment of Unprotected Left Main Bifurcation Lesions. Chinese Circ J. 2019;34:1062–1067. [Google Scholar]
- 30.Yang Y LX, Xie Y, et al Protective effect of jailed balloon technique using drug-coated balloon on the side branch of coronary artery bifurcation lesions after percutaneous coronary intervention. J New Med. 2020;51:289–293. [Google Scholar]
- 31.Zhao Y BJ, Liu QY, Deng L, et al Application of drug-coated balloon in treatment of coronary artery bifurcation lesions. Chin J Geriatr Heart Brain Ves Dis. 2017;19:388–390. [Google Scholar]
- 32.Kobayashi N, Yamawaki M, Hiraishi M, et al Vascular Response after Directional Coronary Atherectomy for Left Main Bifurcation Lesion. J Interv Cardiol. 2021;2021:5541843. doi: 10.1155/2021/5541843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kook H, Joo HJ, Park JH, et al A comparison between drug-eluting stent implantation and drug-coated balloon angioplasty in patients with left main bifurcation in-stent restenotic lesions. BMC Cardiovasc Disord. 2020;20:83. doi: 10.1186/s12872-020-01381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee WC, Hsueh SK, Chen CJ, et al The Comparison of Clinical Outcomes After Drug-Eluting Balloon and Drug-Eluting Stent Use for Left Main Bifurcation In-Stent Restenosis. Int Heart J. 2018;59:935–940. doi: 10.1536/ihj.17-540. [DOI] [PubMed] [Google Scholar]
- 35.Okutsu M, Mitomo S, Ouchi T, et al. Impact of directional coronary atherectomy followed by drug-coated balloon strategy to avoid the complex stenting for bifurcation lesions. Heart Vessels 2022.
- 36.Harada Y, Colleran R, Pinieck S, et al Angiographic and clinical outcomes of patients treated with drug-coated balloon angioplasty for in-stent restenosis after coronary bifurcation stenting with a two-stent technique. EuroIntervention. 2017;12:2132–2139. doi: 10.4244/EIJ-D-16-00226. [DOI] [PubMed] [Google Scholar]
- 37.Naganuma T, Latib A, Costopoulos C, et al Drug-eluting balloon versus second-generation drug-eluting stent for the treatment of restenotic lesions involving coronary bifurcations. EuroIntervention. 2016;11:989–995. doi: 10.4244/EIJY14M11_01. [DOI] [PubMed] [Google Scholar]
- 38.Schulz A, Hauschild T, Kleber FX Treatment of coronary de novo bifurcation lesions with DCB only strategy. Clin Res Cardiol. 2014;103:451–456. doi: 10.1007/s00392-014-0671-9. [DOI] [PubMed] [Google Scholar]
- 39.Elwany M, Zaki A, Latib A, et al The impact of the use of bioresorbable vascular scaffolds and drug-coated balloons in coronary bifurcation lesions. Egypt Heart J. 2019;71:31. doi: 10.1186/s43044-019-0033-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ikuta A, Kubo S, Ohya M, et al Impact of late lumen loss on clinical outcomes of side branch bifurcation lesions treated by drug-coated balloon angioplasty with main branch stenting. Cardiovasc Revasc Med. 2022;41:92–98. doi: 10.1016/j.carrev.2021.12.020. [DOI] [PubMed] [Google Scholar]
- 41.Kitani S, Igarashi Y, Tsuchikane E, et al Efficacy of drug-coated balloon angioplasty after directional coronary atherectomy for coronary bifurcation lesions (DCA/DCB registry) Catheter Cardiovasc Interv. 2021;97:E614–e623. doi: 10.1002/ccd.29210. [DOI] [PubMed] [Google Scholar]
- 42.Kobayashi N, Yamawaki M, Mori S, et al Stentless Strategy by Drug-Coated Balloon Angioplasty following Directional Coronary Atherectomy for Left Main Bifurcation Lesion. J Interv Cardiol. 2021;2021:5529317. doi: 10.1155/2021/5529317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li Y, Mao Q, Liu H, Zhou D, Zhao J Effect of Paclitaxel-Coated Balloon Angioplasty on Side Branch Lesion and Cardiovascular Outcomes in Patients with De Novo True Coronary Bifurcation Lesions Undergoing Percutaneous Coronary Intervention. Cardiovasc Drugs Ther. 2022;36:859–866. doi: 10.1007/s10557-021-07225-8. [DOI] [PubMed] [Google Scholar]
- 44.Erdoğan E, Li Z, Zhu YX, et al DCB combined with provisional DES implantation in the treatment of De Novo Medina 0, 1, 0 or 0, 0, 1 left main coronary bifurcation lesions: A proof-of-concept study. Anatol J Cardiol. 2022;26:218–225. doi: 10.5152/AnatolJCardiol.2021.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herrador JA, Fernandez JC, Guzman M, Aragon V Drug-eluting vs. conventional balloon for side branch dilation in coronary bifurcations treated by provisional T stenting. J Interv Cardiol. 2013;26:454–62. doi: 10.1111/joic.12061. [DOI] [PubMed] [Google Scholar]
- 46.Liu H, Tao H, Han X, et al Improved Outcomes of Combined Main Branch Stenting and Side Branch Drug-Coated Balloon versus Two-Stent Strategy in Patients with Left Main Bifurcation Lesions. J Interv Cardiol. 2022;2022:8250057. doi: 10.1155/2022/8250057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ullah H, Elakabawi K, Ke H, et al Predictors and 3-year outcomes of compromised left circumflex coronary artery after left main crossover stenting. Clin Cardiol. 2021;44:1377–1385. doi: 10.1002/clc.23693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen SL, Zhang JJ, Han Y, et al Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol. 2017;70:2605–2617. doi: 10.1016/j.jacc.2017.09.1066. [DOI] [PubMed] [Google Scholar]
- 49.Berland J, Lefèvre T, Brenot P, et al DANUBIO - a new drug-eluting balloon for the treatment of side branches in bifurcation lesions: six-month angiographic follow-up results of the DEBSIDE trial. EuroIntervention. 2015;11:868–876. doi: 10.4244/EIJV11I8A177. [DOI] [PubMed] [Google Scholar]
- 50.Niemelä M, Kervinen K, Erglis A, et al Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123:79–86. doi: 10.1161/CIRCULATIONAHA.110.966879. [DOI] [PubMed] [Google Scholar]
- 51.Hildick-Smith D, de Belder AJ, Cooter N, et al Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010;121:1235–1243. doi: 10.1161/CIRCULATIONAHA.109.888297. [DOI] [PubMed] [Google Scholar]
- 52.Colombo A, Bramucci E, Saccà S, et al Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009;119:71–78. doi: 10.1161/CIRCULATIONAHA.108.808402. [DOI] [PubMed] [Google Scholar]
- 53.Tsuchikane E, Aizawa T, Tamai H, et al Pre-drug-eluting stent debulking of bifurcated coronary lesions. J Am Coll Cardiol. 2007;50:1941–1945. doi: 10.1016/j.jacc.2007.07.066. [DOI] [PubMed] [Google Scholar]
- 54.Yamawaki M, Fujita M, Sasaki S, et al Randomized comparison between provisional and routine kissing-balloon technique after main vessel crossover stenting for coronary bifurcation lesions. Heart Vessels. 2017;32:1067–1076. doi: 10.1007/s00380-017-0977-4. [DOI] [PubMed] [Google Scholar]
- 55.De Paolis M, Felix C, van Ditzhuijzen N, et al Everolimus-eluting bioresorbable vascular scaffolds implanted in coronary bifurcation lesions: Impact of polymeric wide struts on side-branch impairment. Int J Cardiol. 2016;221:656–664. doi: 10.1016/j.ijcard.2016.06.153. [DOI] [PubMed] [Google Scholar]
- 56.Naganuma T, Colombo A, Lesiak M, et al Bioresorbable vascular scaffold use for coronary bifurcation lesions: A substudy from GHOST EU registry. Catheter Cardiovasc Interv. 2017;89:47–56. doi: 10.1002/ccd.26634. [DOI] [PubMed] [Google Scholar]
- 57.Paradies V, Vlachojannis GJ, Royaards KJ, et al Angiographic and Midterm Outcomes of Bioresorbable Vascular Scaffold for Coronary Bifurcation Lesions. Am J Cardiol. 2018;122:2035–2042. doi: 10.1016/j.amjcard.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 58.Burzotta F, Lassen JF, Lefèvre T, et al Percutaneous coronary intervention for bifurcation coronary lesions: the 15(th) consensus document from the European Bifurcation Club. EuroIntervention. 2021;16:1307–1317. doi: 10.4244/EIJ-D-20-00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rigatelli G, Zuin M, Nikolov P, et al One- and 3-year outcomes of percutaneous bifurcation left main revascularization with modern drug-eluting stents: a systematic review and meta-analysis. Clin Res Cardiol. 2021;110:1–11. doi: 10.1007/s00392-020-01679-w. [DOI] [PubMed] [Google Scholar]
- 60.Huber MS, Mooney JF, Madison J, Mooney MR Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol. 1991;68:467–471. doi: 10.1016/0002-9149(91)90780-o. [DOI] [PubMed] [Google Scholar]
- 61.Alfonso F, Pérez-Vizcayno MJ, Cárdenas A, et al A Prospective Randomized Trial of Drug-Eluting Balloons Versus Everolimus-Eluting Stents in Patients With In-Stent Restenosis of Drug-Eluting Stents: The RIBS IV Randomized Clinical Trial. J Am Coll Cardiol. 2015;66:23–33. doi: 10.1016/j.jacc.2015.04.063. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data to this article can be found online.