Abstract
Bronchial schwannoma is a rare benign tumor traditionally managed through surgical resection. This case report describes a 69-year-old Chinese woman with an asymptomatic bronchial schwannoma incidentally discovered during routine health check-up. Computed tomography (CT) and bronchoscopy revealed a broad-based mass (27 mm × 16 mm) at the right lower lobe bronchus, causing complete obstruction of the dorsal segment and severe stenosis (>80%) of the basal segment. Histopathological and immunohistochemical analyses confirmed the diagnosis of schwannoma. The patient underwent a single-session multimodal bronchoscopic treatment combining cryotherapy, high-frequency electrocoagulation, and laser therapy, with minimal bleeding (<5 ml). Post-intervention evaluation showed a fully patent right lower lobe bronchus, and at 8-month follow-up, CT confirmed complete resolution without tumor recurrence. This case demonstrates that carefully planned bronchoscopic intervention can effectively manage selected cases of bronchial schwannoma while preserving lung function and minimizing procedural risks.
Keywords: Bronchial schwannoma, bronchoscope, interventional treatment, cryotherapy, electrocoagulation, laser therapy
Introduction
Schwannomas originate from peripheral nerves, the spinal cord, or cranial nerves. 1 It is an encapsulated benign tumor composed of various cell types, such as Schwann cells, macrophages, fibroblasts and so on. These cells form a complex tumor microenvironment and participate in the occurrence and development of schwannoma. 2 According to studies, schwannomas can occur in any peripheral or cranial nerve, but are more common in the head, neck and limbs. 3 Although Straus et al. reported the first case of polypoid schwannoma in the left main bronchus under bronchoscope as early as 1951, 4 endobronchial schwannomas are still extremely rare, accounting for only 2.2 percent of benign tracheobronchial tumors. 5
Currently, despite the absence of standardized treatment guidelines, surgical treatment is still the first choice. At the same time, we found that because of serious complications, some patients were often unable to make preoperative diagnosis, but can only take surgical treatment directly, and even inevitably have to remove a lobe of lung, causing permanent damage to lung function. If a definite diagnosis can be made preoperatively, a more appropriate treatment plan can be developed according to the patient's condition. This approach would allow complete tumor removal while maximally preserving lung function. This case report aims to present an alternative therapeutic approach for bronchial schwannoma. Therefore, we report a case of bronchoscopic resection of bronchial schwannoma using a combination of cryotherapy, high-frequency electrocoagulation and laser interventional therapy. The patient provided informed consent and agreed to publish the relevant data in our manuscript.
Case report
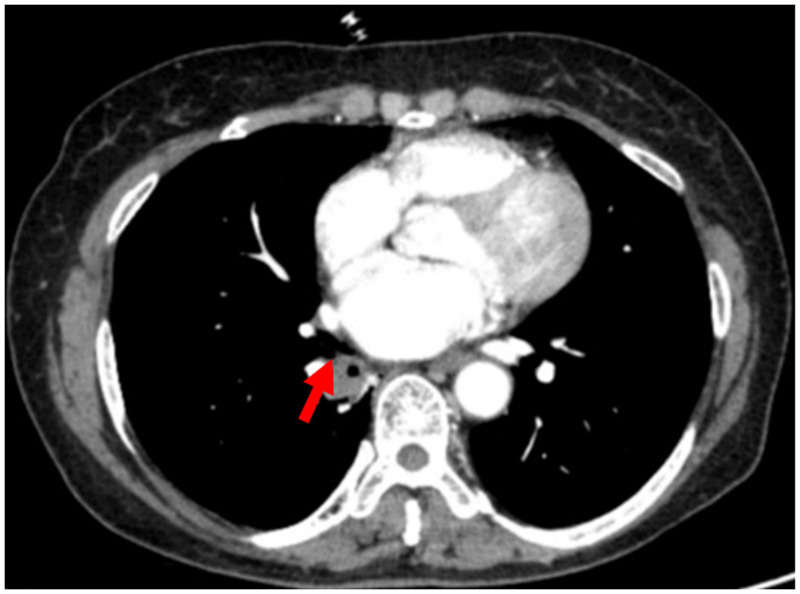
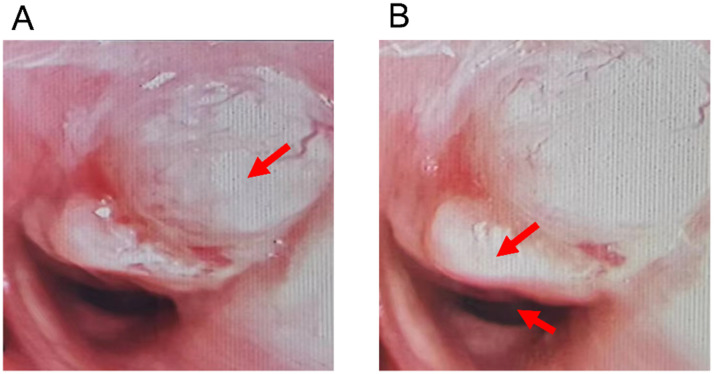
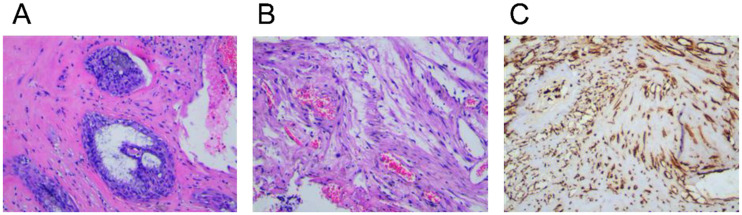
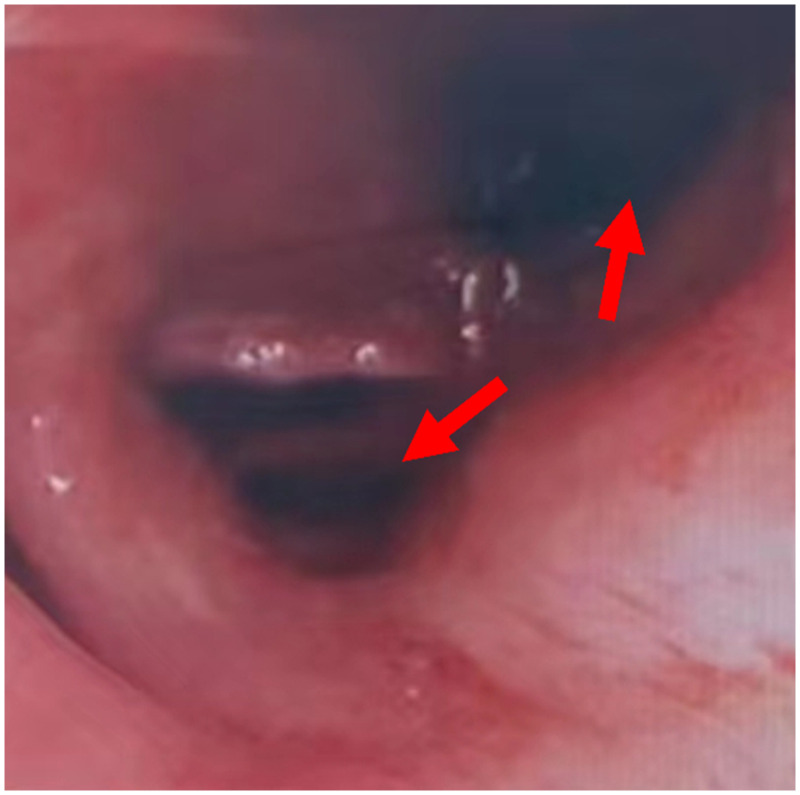
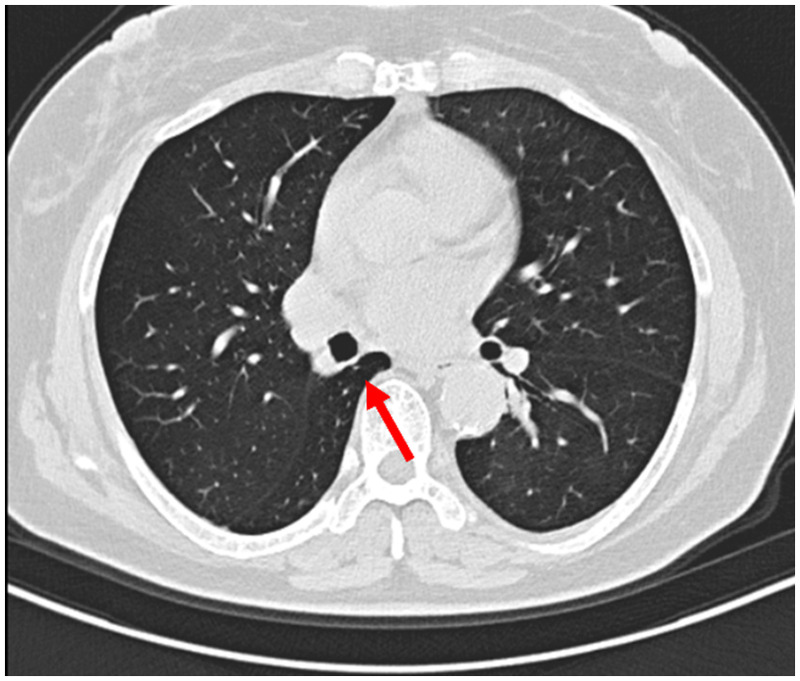
A 69-year-old Chinese woman was found to have an oval nodule in the right lower bronchus during a routine health check-up at a local hospital. Chest CT revealed the lesion, and subsequent bronchoscopy confirmed an oval mass growing on the right side of the lumen at the opening of the right lower lobe bronchus. For further evaluation and treatment, the patient was referred to Wuxi No.2 People's Hospital on 4th June, 2023, where the diagnosis was reconfirmed. The lumen was narrowed with measurements using multi-planar reconstruction (MPR) showing dimensions of approximately 27 mm by 16 mm (Figure 1). Bronchoscopic examination revealed a broad-based mass at the right lower lobe bronchus, resulting in complete obstruction of the dorsal segment and severe stenosis (>80%) of the basal segment with only a small residual opening.(Figure 2) Partial obstruction of the right middle lobe opening was also noted. A sizable tissue sample was obtained from the obstructed bronchial orifice, measuring 1 cm by 0.6 cm by 0.4 cm, and appeared gray in color. Histopathological examination indicated that the tumor cells were elongated, spindle-shaped, and arranged in bundles with palisading features. Also observed were areas of interstitial degeneration and edema. Immunohistochemical analysis revealed positive staining for S100 and Vimentin proteins (Figure 3). These findings were consistent with a diagnosis of schwannoma. The patient had a 5-year history of hypertension but no other significant medical conditions. She denied any family history of similar conditions or relevant genetic disorders. Following confirmation of the diagnosis, the patient underwent bronchoscopy under general anesthesia. The bronchial schwannoma was treated using a multimodal bronchoscopic approach. Cryotherapy was applied first to devitalize and debulk the tumor tissue. This was followed by high-frequency electrocoagulation for precise tissue removal and hemostasis. Finally, laser therapy was utilized to treat the tumor base and ensure complete removal while minimizing damage to surrounding healthy tissue. The entire procedure was completed in a single session with minimal bleeding (<5 ml). Special attention was paid to preserving the bronchial wall integrity throughout the intervention. The bronchial schwannoma was successfully removed using a combination of cryotherapy, high-frequency electrocoagulation and laser interventional therapy. Postoperative evaluation showed a fully patent right lower lobe bronchus, with the dorsal segmental bronchus now open (Figure 4). The patient recovered well without complications and expressed satisfaction with the outcome of the treatment. At the 8-month follow-up in February 2024, chest CT examination showed complete resolution of the bronchial obstruction with no evidence of tumor recurrence. The right lower lobe bronchus remained patent with normal ventilation. The patient reported no respiratory symptoms and maintained normal daily activities during the entire follow-up period.(Figure 5)
Figure 1.
Chest computed tomography images showing nodules at the bronchial opening of the right lung's lower lobe (axial view).
Figure 2.
A broad-based mass is observed at the bronchial opening of the right lower lobe, obstructing the dorsal segmental bronchus (2A). The dorsal segmental bronchus lacks an opening, and the basal segmental bronchus opening is notably narrowed. (2B).
Figure 3.
Histological and immunohistochemical showing that the mass appears as gray-white tissue. Tumor cells are elongated, spindle-shaped, non-pleomorphic, arranged in bundles and palisades, with areas of interstitial degeneration and edema. Immunohistochemistry results: S100 (diffuse +), CD34 (-), EMA (focal +), Vimentin (+), CK (pan) (-), SMA (partial +), Actin (focal +), Desmin (-), Ki-67 (1% +).
Figure 4.
The right lower lobe bronchus was unobstructed after interventional therapy under bronchoscope.
Figure 5.
Follow-up computed tomography images after the operation showing that the bronchus of the lower right lung lobe is open (axial view).
Discussion
Schwannoma can occur in any region of the respiratory tract. According to the literature review of bronchial schwannoma cases over the past two decades (Table 1), we identified 25 reported cases with distinct clinical characteristics. The condition showed a slight female predominance (56.0%), with patient ages ranging from 7 to 86 years, predominantly occurring in the 41–70 age group (56.0%). Notably, there was a decreased reporting rate in the second decade compared to the first (28% vs. 72%), possibly due to increased awareness and improved diagnostic capabilities.
Table 1.
Summary of cases.
| Number of cases (%) | |||
|---|---|---|---|
| Gender | M | 11 (44.0) | |
| F | 14 (56.0) | ||
| Age | 0–10 | 2 (8.0) | |
| 11–20 | 4 (16.0) | ||
| 21–30 | – | ||
| 31–40 | 1 (4.0) | ||
| 41–50 | 4 (16.0) | ||
| 51–60 | 6 (24.0) | ||
| 61–70 | 4 (16.0) | ||
| 71–80 | 2 (8.0) | ||
| 81–90 | 2 (8.0) | ||
| Main symptoms | Cough | 10 (40.0) | |
| Dyspnea | 5 (20.0) | ||
| Massive hemoptysis | 2 (8.0) | ||
| No | 4 (16.0) | ||
| Others | 4 (16.0) | ||
| Lesion location | Left | MB | 7 (28.0) |
| SLB | 2 (8.0) | ||
| ILB | 1 (4.0) | ||
| Right | MB | 3 (12.0) | |
| SLB | 4 (16.0) | ||
| MLB | 1 (4.0) | ||
| ILB | 5 (20.0) | ||
| MLB/ ILB | 1 (4.0) | ||
| Intermediate segmental bronchu | 1 (4.0) | ||
| Treatment method | Surgical excision | 15 (60.0) | |
| Endoscopic intervention | 7 (28.0) | ||
| Surgical excision + Endoscopic intervention | 2 (8.0) | ||
| Not mentioned | 1 (4.0) | ||
M, Male; F: Female; MB, Main bronchus; SLB, Superior lobe bronchus; ILB, Inferior lobe bronchus; MLB, Middle lobe bronchus.
Regarding anatomical distribution, KeiKasahara et al. classified schwannomas into central and peripheral types based on their location and extension. The central type occurs in the trachea or proximal bronchus, including intraluminal and combined types (both intraluminal and extraluminal). The peripheral type refers to lesions in the distal bronchus, detectable by chest X-ray or CT but not readily visible through fiberoptic bronchoscopy. 6 YoonYang Jung et al. proposed a simpler classification: central type (located in trachea or main bronchus) and peripheral type (located in lobar or segmental bronchial area), regardless of bronchoscopic accessibility. 7
Our literature analysis revealed that lesions were most frequently found in the left main bronchus (28.0%), followed by the right lower lobe bronchus (20.0%) and the right upper lobe bronchus (16.0%). Less common locations included the left lower lobe bronchus, right middle lobe bronchus, right middle-lower lobe bronchus, and right middle segmental bronchus (4% each). The clinical presentation primarily depended on the tumor's location and size, with cough and dyspnea being the predominant symptoms. Interestingly, patients with dyspnea typically had lesions in the main bronchus (80.0%), while those presenting with cough had lesions primarily in the lobar bronchus and below (60.0%). Two cases of massive hemoptysis were associated with right lower lobe bronchus lesions.
Historically, surgical resection has been the primary treatment approach (60.0%), typically involving removal of the affected lung lobe. In two notable cases, left pneumonectomy was performed. However, with the advancement of bronchoscopic technology, less invasive approaches have emerged.8,9 Beibei Jin et al.'s retrospective analysis demonstrated that bronchoscopic resection is a viable treatment option, particularly for patients with surgical risks or those preferring non-surgical interventions. 10 Nevertheless, two cases in our review initially treated with bronchoscopic intervention ultimately required surgical resection due to residual lesions and tumor recurrence.
The histological features of typical schwannomas, characterized by alternating Antoni-A and Antoni-B regions, influence treatment approaches. The loosely arranged cells in the Antoni-B region, rich in irregular thick-walled blood vessels, make traditional electrocautery challenging. 11 Modern interventional techniques, including cryotherapy (cooling to −50°C), high-frequency electrocoagulation, and laser therapy, offer advantages in tissue destruction, hemostasis, and prevention of bronchial contracture. 12 Because schwannomas is rich in blood vessels, combined with the principle of thermal effect produced by high-frequency electrocoagulation and argon ion coagulation, it can not only destroy the tissue, but also contract and coagulate blood vessels, 13 achieving the purpose of effective hemostasis. At the same time, the advantage of laser treatment of vaporization and coagulation tissue can be used to reduce the possibility of bronchial contracture and avoid tracheal scar stenosis after operation.
Traditionally, a case presenting with such significant obstruction of the right lower lobe bronchus and partial compression of the right middle lobe would have warranted lobectomy as the primary treatment option. However, considering our patient's absence of significant clinical symptoms and desire for quality of life preservation, we opted for bronchoscopic intervention under general anesthesia. The combined application of cryotherapy, high-frequency electrocoagulation, and laser therapy achieved complete tumor removal with minimal bleeding (<1 ml) while preserving lung function. This outcome demonstrates the potential of minimally invasive approaches in select cases.
In comparison with recent literature, 14 our study presents several distinctive features that contribute to the current understanding of bronchial schwannoma management. While previous investigations have predominantly centered on symptomatic presentations, our report addresses the clinical approach to incidentally detected bronchial schwannoma during routine health screening—a scenario of increasing relevance in the modern era of preventive medicine. The treatment approach, utilizing a combination of cryotherapy, high-frequency electrocoagulation, and laser therapy, achieved complete resolution in a single procedure without residual obstruction. Furthermore, our extended 8-month follow-up with comprehensive imaging assessment provides valuable data on long-term outcomes of bronchoscopic intervention. These findings contribute to the growing evidence supporting minimally invasive approaches for bronchial schwannoma, particularly in asymptomatic cases where preservation of lung function is paramount. As health screening programs become increasingly prevalent, the incidental discovery of asymptomatic bronchial schwannomas may become more common, suggesting potential clinical implications for future practice. While bronchoscopic intervention offers a non-invasive alternative to traditional surgery, long-term follow-up remains essential due to potential recurrence risk. Regular bronchoscopic evaluation is recommended to monitor for disease recurrence.
Conclusion
This case suggests that bronchoscopic intervention combining cryotherapy, laser therapy, and argon plasma coagulation may be an effective approach for managing selected cases of bronchial schwannoma, particularly in asymptomatic patients with significant bronchial obstruction. This minimally invasive strategy achieved complete tumor removal while preserving lung function, offering an alternative to traditional surgical resection in carefully selected patients. However, the success of this approach depends on appropriate patient selection, precise preoperative evaluation, and operator expertise in bronchoscopic techniques. Regular bronchoscopic follow-up is essential to monitor for potential recurrence. Further studies with larger patient cohorts are needed to evaluate the long-term outcomes of this therapeutic strategy.
Acknowledgements
The authors thank the patient’s family who agreed to publish this case report.
The authors thank all anonymous reviewers and editors for their constructive suggestions to improve the quality of this manuscript.
Footnotes
Authors’ contributions: Xiyue Li analyzed the clinical data and sorted out the previously published literature. Ximiao Yu assisted in organizing the previously published literature and participated in the revision of the manuscript. Ruiqi Luo conducted doctor-patient communication, physical examination, and assisted in collecting clinical data. Xun Wang contributed to the pathological examination and diagnosis, performed subbronchial interventional surgery on the patient, and finally revised this manuscript. All the authors read and approved the final manuscript.
Data availability declaration: All data and materials are provided in the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: The reporting of this study conforms to the CARE guidelines. 15 This case report contains no details regarding the patient's identity. Ethical approval to report this case was obtained from Wuxi No.2 People's Hospital Institutional Review Board (Y-211).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Top Talent Support Program for young and middle-aged people of Wuxi Health Committee, the Scientific Research Program of Wuxi Health Commission (grant number MS201937, T201937)and the China Postdoctoral Science Foundation (grant numbers 2020M670069ZX).
ORCID iD: Xun Wang https://orcid.org/0000-0003-0916-3634
Statement of informed consent: Written informed consent was obtained from the patient for all diagnostic procedures and therapeutic interventions described in this report and anonymized information to be published in this article.
References
- 1.Imen T, Sadok BM, Raoudha A, et al. Endobronchial schwannoma in adult: a case report. Respir Med Case Rep 2021; 33: 101396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helbing DL, Schulz A, Morrison H. Pathomechanisms in schwannoma development and progression. Oncogene Aug 2020; 39: 5421–5429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou D, Xing X, Fan J, et al. PD-1/PD-L1 negative schwannoma mimicking obstructive bronchial malignancy: a case report. Thorac Cancer Aug 2020; 11: 2335–2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Straus GD, Guckien JL. Schwannoma of the tracheobronchial tree. A case report. Ann Otol Rhinol Laryngol Mar 1951; 60: 242–246. [DOI] [PubMed] [Google Scholar]
- 5.Aoyama Y, Miyamoto A, Fujii T, et al. Primary bronchial schwannoma: a case report. Medicine (Baltimore) Oct 7 2022; 101: e31062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasahara K, Fukuoka K, Konishi M, et al. Two cases of endobronchial neurilemmoma and review of the literature in Japan. Intern Med Dec 2003; 42: 1215–1218. [DOI] [PubMed] [Google Scholar]
- 7.Jung YY, Hong ME, Han J, et al. Bronchial schwannomas: clinicopathologic analysis of 7 cases. Korean J Pathol Aug 2013; 47: 326–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Criner GJ, Eberhardt R, Fernandez-Bussy S, et al. Interventional bronchoscopy. Am J Respir Crit Care Med Jul 1 2020; 202: 29–50. [DOI] [PubMed] [Google Scholar]
- 9.Khan A, Hashim Z, Gupta M, et al. Rigid bronchoscopic interventions for central airway obstruction - an observational study. Lung India Mar‐Apr 2020; 37: 114–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jin B, Wang T, Wang J, et al. Interventional bronchoscopic therapy in adult patients with tracheobronchial schwannoma. Ann Palliat Med Jun 2021; 10: 6279–6286. [DOI] [PubMed] [Google Scholar]
- 11.Martinez AP, Fritchie KJ. Update on peripheral nerve sheath tumors. Surg Pathol Clin. Mar 2019; 12: 1–19. [DOI] [PubMed] [Google Scholar]
- 12.Schramm D, Freitag N, Kötz K, et al. Cryotherapy in the paediatric airway: indications, success and safety. Respirology Nov 2022; 27: 966–974. [DOI] [PubMed] [Google Scholar]
- 13.Mahajan AK, Ibrahim O, Perez R, et al. Electrosurgical and Laser therapy tools for the treatment of malignant central airway obstructions. Chest. Feb 2020; 157: 446–453. [DOI] [PubMed] [Google Scholar]
- 14.Lina G, Pengguo H, Zhihua X, et al. Tracheobronchial schwannoma: a case report and literature review. J Int Med Res 2023; 51: 03000605221149891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache . 2013;53:1541–1547. [DOI] [PubMed] [Google Scholar]