Abstract
Background:
Primary aldosteronism (PA) is the most common endocrine cause of secondary hypertension and can be effectively managed, or even cured, with targeted treatment. Despite this, it remains largely undiagnosed leaving a significant patient population with resistant hypertension and modifiable cardiovascular risk.
Objective:
To determine expert consensus on key information about PA that should ideally be taught to medical students as a step toward improving the detection of this common, underdiagnosed, and often easily treated condition.
Design:
The study employed a modified Delphi method which consisted of three rounds, the first of which contained an open-ended question about key areas that experts believe to be most important for inclusion in medical teaching resources and then progressing to assessment of individual versus group rankings of consensus items. Experts included both clinician-educator-researchers and patients with lived experience.
Results:
Nine critical knowledge areas in epidemiology, diagnostics, and pathophysiology were identified by the Delphi as consensus items, with the highest ranked being: “PA is common but often under-diagnosed – think about it with every hypertensive patient.”
Conclusion:
Experts reached a consensus, for the first time, on nine critical knowledge areas about PA that should be covered in medical education. Importantly, the consensus accounted for patients’ values and decisions. The results of this study could be used to assess medical student knowledge and their learning resources to facilitate curriculum development and medical resource updates to ensure the timely and accurate diagnosis of PA in hypertensive patients.
Keywords: Conn’s syndrome, Delphi method, endocrinology, hyperaldosteronism, hypertension, medical education, primary aldosteronism
Introduction
Hypertension is the leading cause of cardiovascular disease and the largest preventable risk factor for overall mortality, 1 with up to 22.8% of Australian adults recording blood pressure (BP) measurements over 140/90 mmHg. 2 The poor control is partly attributable to unrecognized primary aldosteronism (PA), the most common endocrine cause of secondary hypertension, accounting for 5%–15% 3 of hypertension in primary care and up to 30% in those with resistant hypertension.4–6
While experts recognize PA as a common cause of hypertension, previous literature has described PA as a rare disease accounting for less than 1% of hypertensive patients,4,5 and at present it remains grossly underdiagnosed in clinical practice. 7 A study of 4660 individuals with resistant hypertension found that only 2.1% were screened for PA despite all of them fulfilling screening criteria. 5 This has significant implications for patients as untreated PA is associated with increased morbidity and reduced quality of life8,9 secondary to cardiovascular, renal, and metabolic consequences.10–12
Poor diagnostic rates are a product of multiple factors including inadequate understanding and acknowledgment of PA. Educating medical students is one component of a multi-pronged approach to ensure increased awareness and improved diagnosis and treatment of PA. Targeted PA teaching during medical training is important as teaching implemented during initial training can have a significant impact on future physician clinical reasoning and diagnostic patterns 13 and may also play a crucial role in improving patient outcomes.
The lack of consensus on what to teach medical students about PA is a critical gap that contributes to deficient knowledge and subsequent underdiagnosis of a common condition. Medical school curricula are prone to overcrowding and, due to continually expanding medical knowledge, face constant pressure from various disciplines to include more content and more detail about more things. 14 A good argument can be made to focus on prevalent and treatable conditions as such knowledge is likely to positively impact patients’ health. Now that the prevalence and treatment for PA are better understood, the degree of attention on this disease in medical schools may warrant review.
Hence, we sought to determine key, up-to-date, knowledge areas about PA that experts believe are most important for medical students to learn. The expert consensus will be invaluable for medical curriculum development. It can also be used to assess whether medical professionals in training have adequate knowledge and whether their learning or teaching resources contain adequate information as determined by experts in PA.
Method and participant
A modified three-round Delphi survey was performed with an international panel, composed of both clinicians with expertise in PA and patients with PA. The Delphi method is a consensus-based iterative process that uses repetitive questionnaires to gather information from a selected panel. 15
The initial Delphi method was first implemented in the 1960s by Dalkey and Helmer to define and predict military priorities. 16 This method has since been refined, from which a conventional Delphi is defined by its ability to utilize anonymity and controlled feedback to assess initial judgments and make alterations to determine panel consensus. 17
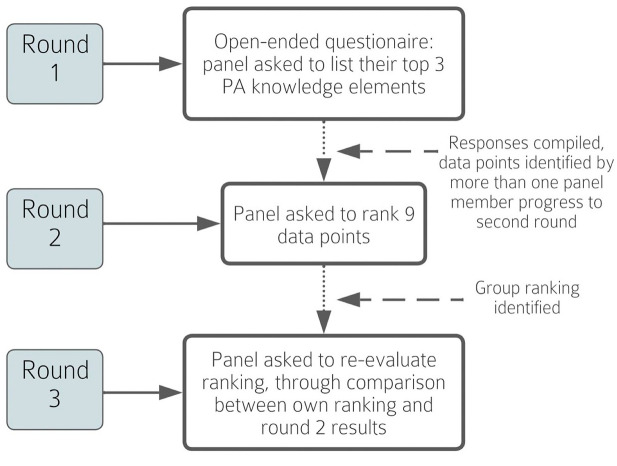
The current study employed a modified Delphi method which consisted of three rounds, the first of which contained an open-ended question about key areas that experts believe to be most important for inclusion in medical teaching resources and then progressed to assessment of individual versus group rankings of PA consensus items (Figure 1). The questionnaires were developed and distributed through Google Forms. The link and instructions to these questionnaires were provided to panel members through email.
Figure 1.
Modified Delphi method.
Panel
Panel participants (other than consumers) were selected for their clinical expertise in managing PA as well as active involvement in research and education. They were also chosen for diverse geographic representation with expertise across Australia, America, Asia, and Europe. All invited panel members accepted the invitation and completed all three stages of the Delphi process.
The consumer panel participants were selected for their advocacy for all individuals with PA through the establishment of the Primary Aldosteronism Foundation and the Conn’s Syndrome/Hyperaldosteronism Support Group. Their lived experience of PA (encompassing both bilateral and unilateral forms) and related comorbidities, including obstructive sleep apnea and atrial fibrillation, are supplemented by extensive consumer feedback via these advocacy platforms. They engage with 200–1500 individuals per month via these platforms.
Written consent was obtained from all panel participants (clinicians and consumers) for their involvement and contributions to this Delphi study.
Round 1
The objective of Round 1 was to confirm panel member involvement with PA research, patient care, and student teaching; alongside identifying aspects of PA that they believe to be most important in medical student teaching.
Questions included in Round 1
Are you a PA clinician or patient?
How many years have you been involved in the management of patients with PA?
Approximately how many patients with PA (new and reviews) do you currently see per month?
Are you involved in teaching medical students?
Are you involved in research on the topic of PA?
Do you currently teach students about PA?
Based on your expertise, what do you believe to be the three most important messages about PA that should be taught to medical students by the time they graduate? Please rank them in the order of importance and provide a short justification for each as to why you believe it to be an important aspect of PA knowledge for medical students.
The final question was used as the primary resource with responses grouped into similar categories and then redistributed to the original panel for calibration and assessment of consensus via survey 2.
The responses to the final question were collated and grouped into key teaching points according to their similarity. Points identified as important by more than one panel member were deemed consensus items and redistributed to the original panel for calibration and assessment of consensus in Round 2.
Round 2
The aspects of PA identified as consensus items were redistributed to the original panel members who were asked to rank them in order of importance from most important to least important.
The mean and median were calculated from the responses of the entire panel (13 participants), patients only (2), and clinicians only (11). A distinction was made to identify whether there was a significant variance between aspects of PA that clinicians versus patients believed to be most important.
Round 3
The responses from survey 2 were compiled to generate an ordered ranking of the previously identified critical knowledge areas of PA. The group ranking was redistributed to panel members alongside their own ranking, from which panelists were allowed to change their initial ranking after comparison to the group ranking.
Results
Round 1
Response to Round 1 of the Delphi confirmed the clinical expertise of the clinician panel members. They have an average of 16 years of experience with PA management, seeing an average of 19 patients with PA per month. They were all involved in PA research and 9/10 were involved with medical student teaching.
The two patients were actively involved in consumer advocacy as founding members of the PA Foundation (based in Arizona) or Conn’s Syndrome/ Hyperaldosteronism Patient Support Group (with 4000 members on Facebook). One of them endured 25 years of unmanaged hypertension with associated hypertensive crises before being diagnosed with bilateral adrenal hyperplasia and commencing medical management with mineralocorticoid receptor antagonists. The other patient was initially diagnosed with an aldosterone-producing adenoma and underwent an adrenalectomy prior to discovering he also had bilateral disease which was then treated with a mineralocorticoid receptor antagonist.
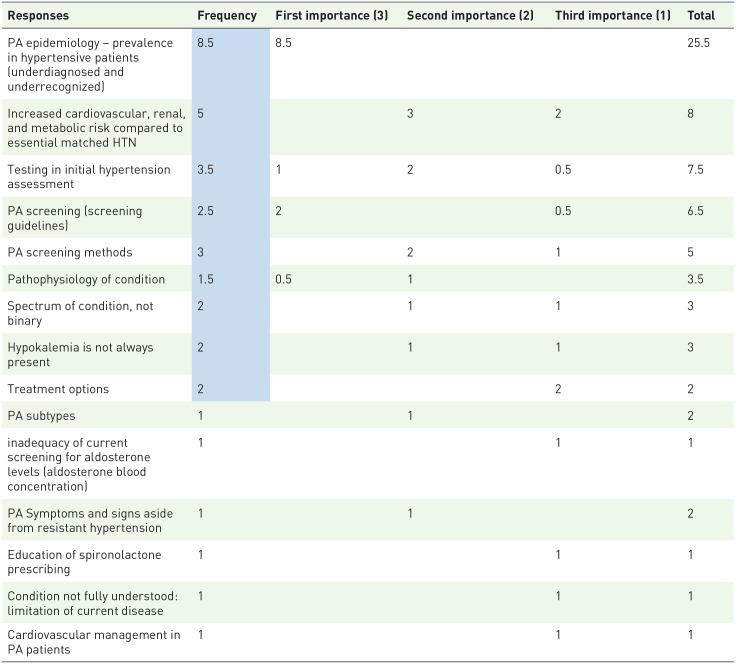
Round 1 also identified nine critical knowledge areas about PA encompassing prevalence, symptoms, diagnostic methods, pathophysiology, treatment methods, and associated risks. Responses were assigned points based on the ranking provided by the panel, that is, most important allocated three points, the second most important two points, third most important one point (Table 1).
Table 1.
Delphi Round 1 results.
|
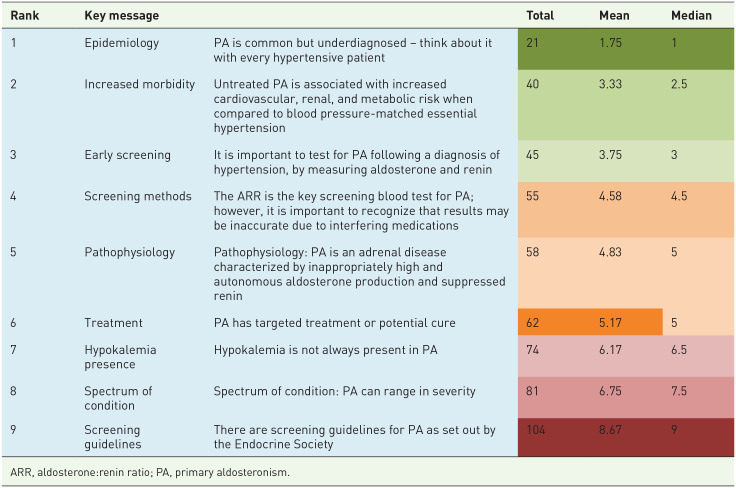
Round 2
A ranking of the points identified from Round 1 was established in Round 2 of this Delphi. Significant variation between groups was not identified; however, some variance was noted between responses from patients and clinicians. The patients gave greater weight to teaching about the spectrum of PA severity and screening all hypertensive patients for PA (Table 2).
Table 2.
Delphi Round 2 results.

|
ARR, aldosterone:renin ratio; PA, primary aldosteronism.
Round 3
The responses from the third survey were closely aligned with the ranking achieved in Round 2 despite 11 members altering their rankings between Rounds 2 and 3. The only difference was a new distinction between points 4 (ARR is a key screening test) and 5 (pathophysiology of PA) which were initially equal in both mean and median (Table 3).
Table 3.
Delphi Round 3 results.
|
ARR, aldosterone:renin ratio; PA, primary aldosteronism.
Discussion
This modified Delphi process identified nine consensus knowledge areas considered by both clinicians and patients with expertise in PA as crucial for medical students to understand.
In addition to inviting clinicians and researchers to join the expert panel, we actively recruited patients because they carry a similar goal to healthcare professionals in seeking optimal treatment for themselves and others with equivalent chronic conditions. 18 They provide a unique perspective about areas of care, including “impact, the practicalities of treatment, and the attitudes of other people, including the medical profession, to [their] condition.” 19 In this circumstance, their involvement allows for a holistic perspective with greater insight into patient experience and allows for emphasis on patient-centered models of care in the continuing development of medical education.
Consensus points that held greatest importance across the panel focused on epidemiological knowledge and the implication of late diagnosis of PA on patient morbidity.
While all nine key knowledge areas identified are relevant to PA and medical education, the top three points and their relevance in current literature are discussed below.
Key knowledge area 1: PA is common but underdiagnosed, think about it with every hypertensive patient
Various studies have demonstrated the high prevalence of PA in patients with resistant hypertension as well as those presenting in primary care facilities. The exact statistics vary across studies, with prevalence estimates of 4%, 5.9%, and 14% in primary care centers in China, Italy, and Australia respectively,10,20,21 and 11%–22% in populations with resistant hypertension.22,23 However, the proportion of patients who are screened or diagnosed is much lower, with <1% of eligible hypertensive patients screened in a Canadian population of more than 245,000 patients identified with resistant hypertension 24 and <0.1% of hypertensive patients having the diagnosis of PA in an Australian primary care setting. 7
These studies support the universal screening of PA in people with hypertension. However, there are high-risk patient groups that warrant specific attention, as recommended by the 2016 Endocrine Society Clinical Practice Guideline 25 :
Sustained BP above 150/100 mmHg on each of three measurements obtained on different days, or
Hypertension (BP >140/90 mmHg) resistant to three conventional antihypertensive drugs (including a diuretic), or
Controlled BP (<140/90 mmHg) on four or more antihypertensive medications
Hypertension and spontaneous or diuretic-induced hypokalemia
Hypertension and adrenal incidentaloma
Hypertension and sleep apnea
Hypertension and a family history of early-onset hypertension or cerebrovascular accident at a young age (<40 years)
All hypertensive first-degree relatives of a patient with PA
At present, screening rates are low even in these high-risk groups, with 1%–3% tested despite having resistant hypertension or hypokalemia.26–29
The wide chasm between the expected prevalence and actual screening and detection rates highlights the importance of PA screening as an important teaching point for medical students.
Key knowledge area 2: Untreated PA is associated with increased cardiovascular, renal and metabolic risk when compared to BP-matched essential hypertension
Increased risk of poor cardiovascular, renal, and metabolic outcomes in inadequately treated PA is well documented in the literature. A retrospective French study comparing 459 patients with PA and 1290 with essential matched hypertension (EH) showed up to 3× increased risk of myocardial infarction, atrial fibrillation, coronary artery disease, and heart failure. 30 A systematic review and meta-analysis of 3838 patients with PA compared to 9284 patients with EH also demonstrated an increased risk of stroke OR 2.58 (CI 1.93–3.45), atrial fibrillation OR 3.52 (CI 2.06–5.99), coronary artery disease OR 1.77 (CI 1.1–2.83) and heart failure OR 2.05 (CI 1.11–3.78) in the PA group. 11 Patients with PA also demonstrated accelerated renal damage compared to patients with EH evidenced by increased urinary albumin excretion, secondary to endothelial dysfunction caused by excess aldosterone.31,32 Specifically, preclinical models have characterized the impact of aldosterone infusion on promoting renal inflammation and fibrosis via actions on the podocytes, infiltrating macrophages and stromal cells. 33 In humans, the Chronic Renal Insufficiency Cohort (CRIC) study identified median baseline serum aldosterone concentration to be higher among 3680 participants who developed chronic kidney disease, at 10.6 ng/dL compared to 9.6 ng/dL. When expressed as a continuous variable, there was an 11% higher risk for chronic kidney disease progression per doubling of serum aldosterone. 34 The FIDELIO study contributed further weight to the impact of aldosterone excess on renal dysfunction by demonstrating a lower risk of chronic kidney disease progression in a randomized clinical trial of mineralocorticoid receptor antagonist, finerenone. 35
Key knowledge area 3: It is important to screen for PA following a diagnosis of hypertension by measuring aldosterone and renin
The high prevalence of PA together with the universal issue of underdiagnosis, logically leads to the third highest-ranked knowledge area. Currently, the Endocrine Society guidelines outline a range of criteria for PA testing (as described above), 25 however, the expert panel established consensus that all patients should be screened upon their diagnosis of hypertension. Screening for PA in all adults with hypertension has recently been recommended by the European Society of Cardiology 2024 Hypertension Guidelines. 36
The benefit of routine screening is evident in the 5–15-fold increase in PA diagnosis following the implementation of the aldosterone to renin ratio (ARR) as a routine test for PA across five international centers. 37 Routine measurement of the ARR in treatment-naïve hypertensive patients in primary care led to the diagnosis of PA in 14%. 21 Early screening of PA also avoids the confounding effect of most antihypertensive agents which commonly cause false negative ARR results. 25 Furthermore, early PA screening has been found to be cost-effective in health economic evaluation studies from China and Australia.38,39
Practical implications
Evaluation of these top three consensus points demonstrated that expert consensus, while obtained via questionnaires, has a strong evidence base. Given that maintaining currency in medical education is usually achieved by virtue of the teachers and educational resources being up to date, 40 consensus on teaching points by international experts, including patient advocates, may be a valuable and time-efficient strategy to achieve currency.
This is particularly the case for PA as current popular medical textbooks and online information resources often contain gaps and outdated information. In a review of original articles published in the New England Journal of Medicine between 2001 and 2010, 146 medical reversals were identified where emerging evidence led to a change in previously established practices. 41 Further research analyzing popular online resources, including UpToDate and Best Practice, found between 23% and 60% variation between these resources and recently published articles on the same topics. 42 While no formal research has been published about the currency of PA medical resources, given the current challenges facing screening and diagnosis, it can be inferred that a proportion of the existing literature fails to adequately articulate the prevalence of PA, the importance of screening and the ease of medical management with mineralocorticoid receptor antagonist such as spironolactone. 25
With the rapid pace of medical innovation and changes in guidelines, clear teaching points as identified in this Delphi study can be incorporated into the medical curriculum to guide student teaching and assessment. Furthermore, to ensure that the key learning points are widely disseminated beyond individual medical schools, collaborations can be sought with popular learning resources.
Further research to evaluate the clinical impact of expert-consensus-guided PA teaching will be important for understanding how this strategy improves the diagnosis, management, and health outcomes of patients with PA.
Strengths and limitations
A key strength of this research is the inclusion of both expert clinicians/educators and patients with lived experience of PA. The engagement of patients brings valuable insights into the practical and patient-centered aspects of care. An extensive literature search did not identify any other studies that utilized the Delphi process to establish learning points for students. This unique approach to developing education content has enabled us to identify and prioritize critical knowledge areas for PA that are important to both clinicians and consumers, creating a focused and relevant framework for curriculum development.
While the expert panel is geographically diverse, it consisted of a relatively small number of experts with 13 in total, including only two consumers. This may have limited the breadth of perspectives, although the selected experts are highly experienced in the PA field and the consumers are affiliated with patient advocacy groups that represent thousands of voices.
Another limitation to the key knowledge areas identified by expert consensus is that they can become outdated over time. However, the three key areas identified in our study are unlikely to change in the near future, especially as the recent European Society of Cardiology Guidelines for the management of hypertension has just recommended that PA screening be considered in all adults with hypertension. 41
Finally, it is important to note that our study has focused on what medical students should learn rather than what their knowledge gaps are and how the gaps can be filled. The next stage of research is to apply the key knowledge areas to student assessments and evaluate the coverage of these areas in popular learning resources.
Conclusion
Clinicians and patients with experience in PA reached consensus on nine key knowledge areas about PA through a modified Delphi process with the top three focusing on the underappreciated prevalence of PA, the high cardiovascular, metabolic, and renal risk associated with PA, and the importance of screening. These results provide a useful tool for evaluating the adequacy of current teaching about PA in medical schools and assessing the students’ knowledge of PA.
The dynamic nature of medical advancements poses significant challenges in ensuring that healthcare providers are equipped with the most current and accurate knowledge. The prevalence of outdated information in widely used medical resources and the observed gaps in educational content underscore the need for continuous updates to medical curricula. Despite evidence showing that targeted education improves patient outcomes, variability in curriculum development and a lack of standardization contribute to inconsistent training across medical schools. Addressing these issues through expert consensus and curriculum reform is essential to enhance the accuracy of medical education and improve patient care, particularly in areas like PA where underdiagnosis remains a concern. Once these students transition to practicing clinicians it is hoped the knowledge will translate to improved diagnosis of PA thus reducing the burden of PA-associated morbidity in patients with hypertension.
Acknowledgments
We acknowledge the contribution of experts in the management of primary aldosteronism and consumers who have lived experience of primary aldosteronism to the Delphi process. This includes Michael Stowasser (AUS), Jinbo Hu (China), John Funder (AUS), Renata Libianto (AUS), Martin Wolley (AUS), Peter Fuller (AUS), John M. Clark (USA), Marianne Leenaerts (USA), Adina Turcu (USA), Jimmy Shen (AUS), Jacques Lenders (The Netherlands) and Moe Thuzar (AUS).
Footnotes
ORCID iD: Jocelyn Widjaja  https://orcid.org/0000-0002-0248-5289
https://orcid.org/0000-0002-0248-5289
Contributor Information
Jocelyn Widjaja, Faculty of Medicine Nursing and Health Sciences, Monash University, Wellington Road, Clayton, VIC 3800, Australia.
Jun Yang, Monash University, Clayton, VIC, Australia; Hudson Institute of Medical Research, Clayton, VIC, Australia.
Julia Harrison, Monash University, Clayton, VIC, Australia.
Declarations
Ethics approval and consent to participate: All Delphi panel participants consented to involvement in this study and dissemination of its findings. All methods were carried out in accordance with the WMA Declaration of Helsinki – Principles for Medical Research Involving Human Subjects. The study was approved by the Monash University Human Research Ethics Committee as a clinical audit/Quality Assurance and Evaluation Activity (HREC Reference Number: QA/74597/MonH-2021-264596). As this study does not involve patient information or intervention, there are minimal risks to consider. Informed consent to participate was obtained from all participants in the study. Written consent was obtained from all panel participants (clinicians and consumers) for their involvement and contributions to this Delphi study.
Consent for publication: Not applicable.
Author contributions: Jocelyn Widjaja: Data curation; Formal analysis; Investigation; Project administration; Writing – original draft.
Jun Yang: Conceptualization; Data curation; Resources; Supervision; Writing – review & editing.
Julia Harrison: Conceptualization; Formal analysis; Supervision; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Competing interests: The authors declare that there is no conflict of interest.
Availability of data and materials: All the information required for the reproduction of the results can be obtained from author Jocelyn Widjaja upon reasonable request.
References
- 1. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159): 1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Australian Beaurea of Statistics. Hypertension and measured high blood pressure, https://www.abs.gov.au/statistics/health/health-conditions-and-risks/hypertension-and-measured-high-blood-pressure/latest-release> (2023, accessed 10 May 2023).
- 3. Olivieri O, Ciacciarelli A, Signorelli D, et al. Aldosterone to Renin ratio in a primary care setting: the Bussolengo Study. J Clin Endocrinol Metab 2004; 89(9): 4221–4226. [DOI] [PubMed] [Google Scholar]
- 4. Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension 2018; 72(5): e53–e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jaffe G, Gray Z, Krishnan G, et al. Screening rates for primary aldosteronism in resistant hypertension: a cohort study. Hypertension 2020; 75(3): 650–659. [DOI] [PubMed] [Google Scholar]
- 6. Ito Y, Takeda R, Karashima S, et al. Prevalence of primary aldosteronism among prehypertensive and stage 1 hypertensive subjects. Hypertens Res 2011; 34(1): 98–102. [DOI] [PubMed] [Google Scholar]
- 7. Yang J, Fuller PJ, Stowasser M. Is it time to screen all patients with hypertension for primary aldosteronism? Med J Aust 2018; 209(2): 57–59. [DOI] [PubMed] [Google Scholar]
- 8. Reincke M. Anxiety, depression, and impaired quality of life in primary aldosteronism: why we shouldn’t ignore it! J Clin Endocrinol Metab 2017; 103(1): 1–4. [DOI] [PubMed] [Google Scholar]
- 9. Sukor N, Kogovsek C, Gordon RD, et al. Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J Clin Endocrinol Metab 2010; 95(3): 1360–1364. [DOI] [PubMed] [Google Scholar]
- 10. Monticone S, Burrello J, Tizzani D, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol 2017; 69(14): 1811–1820. [DOI] [PubMed] [Google Scholar]
- 11. Monticone S, D’Ascenzo F, Moretti C, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2018; 6(1): 41–50. [DOI] [PubMed] [Google Scholar]
- 12. Mulatero P, Monticone S, Bertello C, et al. Long-term cardio- and cerebrovascular events in patients with primary aldosteronism. J Clin Endocrinol Metab 2013; 98(12): 4826–4833. [DOI] [PubMed] [Google Scholar]
- 13. Graber ML, Rencic J, Rusz D, et al. Improving diagnosis by improving education: a policy brief on education in healthcare professions. Diagnosis 2018; 5(3): 107–118. [DOI] [PubMed] [Google Scholar]
- 14. Abrahamson S. Diseases of the curriculum. J Med Educ 1978; 53(12): 951–957. [DOI] [PubMed] [Google Scholar]
- 15. Linstone H, Turoff M. The Delphi Method: techniques and applications. Addison-Wesley Publishing Co, vol. 18, 1975. [Google Scholar]
- 16. Dalkey N, Helmer O. An experimental application of the DELPHI method to the use of experts. Manage Sci 1963; 9(3): 458–467. [Google Scholar]
- 17. Hsu C-C, Sandford B. The Delphi Technique: making sense of consensus. In Practical assessment, research and evaluation. 2007; 12(10): 1–8. [Google Scholar]
- 18. Wykurz G, Kelly D. Developing the role of patients as teachers: literature review. BMJ 2002; 325(7368): 818–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alahlafi A, Burge S. What should undergraduate medical students know about psoriasis? Involving patients in curriculum development: modified Delphi technique. BMJ 2005; 330(7492): 633–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xu Z, Yang J, Hu J, et al. Primary aldosteronism in patients in China with recently detected hypertension. J Am Coll Cardiol 2020; 75(16): 1913–1922. [DOI] [PubMed] [Google Scholar]
- 21. Libianto R, Russell GM, Stowasser M, et al. Detecting primary aldosteronism in Australian primary care: a prospective study. Med J Aust 2022; 216(8): 408–412. [DOI] [PubMed] [Google Scholar]
- 22. Brown JM, Siddiqui M, Calhoun DA, et al. The unrecognized prevalence of primary aldosteronism: a cross-sectional study. Ann Intern Med 2020; 173(1): 10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Douma S, Petidis K, Doumas M, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet 2008; 371(9628): 1921–1926. [DOI] [PubMed] [Google Scholar]
- 24. Leung AA, Williams JVA, Tran KC, et al. Epidemiology of resistant hypertension in Canada. Can J Cardiol 2022; 38(5): 681–687. [DOI] [PubMed] [Google Scholar]
- 25. Funder JW, Carey RM, Mantero F, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016; 101(5): 1889–1916. [DOI] [PubMed] [Google Scholar]
- 26. Hundemer GL, Imsirovic H, Vaidya A, et al. Screening rates for primary aldosteronism among individuals with hypertension plus hypokalemia: a population-based retrospective cohort study. Hypertension 2022; 79(1): 178–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cohen JB, Cohen DL, Herman DS, et al. Testing for primary aldosteronism and mineralocorticoid receptor antagonist use among U.S. Veterans: a retrospective cohort study. Ann Intern Med 2021; 174(3): 289–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kositanurit W, Giacona JM, Xie D, et al. Trends in primary aldosteronism screening among high-risk hypertensive adults. J Am Heart Assoc 2024; 13(15): e036373. [DOI] [PubMed] [Google Scholar]
- 29. Kim V, Shi J, An J, et al. Hyperaldosteronism screening and findings from a large diverse population with resistant hypertension within an Integrated Health System. Perm J 2024; 28(1): 3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Savard S, Amar L, Plouin PF, et al. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension 2013; 62(2): 331–336. [DOI] [PubMed] [Google Scholar]
- 31. Rossi GP, Bernini G, Desideri G, et al. Renal damage in primary aldosteronism: results of the PAPY Study. Hypertension 2006; 48(2): 232–238. [DOI] [PubMed] [Google Scholar]
- 32. Sechi LA, Novello M, Lapenna R, et al. Long-term renal outcomes in patients with primary aldosteronism. JAMA 2006; 295(22): 2638–2645. [DOI] [PubMed] [Google Scholar]
- 33. Yang J, Young MJ, Cole TJ, et al. Mineralocorticoid receptor signalling in primary aldosteronism. J Endocrinol 2023; 259(1): e220249. [DOI] [PubMed] [Google Scholar]
- 34. Verma A, Vaidya A, Subudhi S, et al. Aldosterone in chronic kidney disease and renal outcomes. Eur Heart J 2022; 43(38): 3781–3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bakris GL, Agarwal R, Anker SD, et al. Effect of Finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med 2020; 383(23): 2219–2229. [DOI] [PubMed] [Google Scholar]
- 36. Cohen JB. What is new in the ESC hypertension guideline? Hypertension Epub ahead of print . DOI: 10.1161/HYPERTENSIONAHA.124.23724. [DOI] [PubMed] [Google Scholar]
- 37. Mulatero P, Stowasser M, Loh KC, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab 2004; 89(3): 1045–50. [DOI] [PubMed] [Google Scholar]
- 38. Woode ME, Wong K, Reid CM, et al. Cost-effectiveness of screening for primary aldosteronism in hypertensive patients in Australia: a Markov modelling analysis. J Hypertens 2023; 41(10): 1615–1625. [DOI] [PubMed] [Google Scholar]
- 39. Li N, Huang J, Zheng B, et al. Cost-effectiveness analysis of screening for primary aldosteronism in China. Clin Endocrinol (Oxf) 2021; 95(3): 414–422. [DOI] [PubMed] [Google Scholar]
- 40. Committee on Diagnostic Error in Health Care, Board on Health Care Services, Institute of Medicine, The National Academies of Sciences Engineering Medicine; Balogh EP, Miller BT, Ball JR. (eds.) Improving diagnosis in health care. Washington, DC: National Academies Press (US); 2015. [PubMed] [Google Scholar]
- 41. McEvoy JW, McCarthy CP, Bruno RM, et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension: developed by the task force on the management of elevated blood pressure and hypertension of the European Society of Cardiology (ESC) and endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO). Eur Heart J 2024; 45(38): 3912–4018. [DOI] [PubMed] [Google Scholar]
- 42. Jeffery R, Navarro T, Lokker C, Haynes RB, et al. How current are leading evidence-based medical textbooks? An analytic survey of four online textbooks. J Med Internet Res 2012; 14(6): e175. [DOI] [PMC free article] [PubMed] [Google Scholar]