Abstract
Primary cardiac malignancy presents an unusual and difficult surgical challenge. Malignant tumors of the left atrium have proved problematic due to their posterior location and difficulty of surgical exposure. The technique of cardiac explantation, ex vivo resection and cardiac reconstruction, and reimplantation—the cardiac autotransplantation procedure—was developed to solve this anatomic problem. Herein, we discuss the development of this approach and describe the surgical technique. (Tex Heart Inst J 2002;29:105–8)
Key words: Heart atrium/surgery; heart neoplasms/surgery; heart transplantation; transplantation, autologous/methods
Primary cardiac malignancies are rare; almost all are sarcomas. The presenting symptoms depend on the size and location of the tumor and include 1) heart failure due to obstruction of intracardiac blood flow or impingement of valve function; 2) embolism of tumor fragments; 3) conduction abnormalities due to infiltration of the conduction system; and 4) systemic constitutional symptoms. Chemotherapy and radiotherapy have been used but are not as successful as surgery in relieving symptoms or prolonging survival. 1–4 Surgical resection, when feasible, has been the treatment of choice, both to relieve local symptoms and to attempt complete excision. Surgical series have suggested that local recurrence often leads to death before metastatic disease develops, 3,5 and that life expectancy is twice as long for patients with primary cardiac sarcoma who undergo complete resection and adjuvant chemotherapy compared with those who do not. 4 It seems clear that the goal of surgery in such cases should be complete resection with clear margins and maintainance of normal cardiac function. The success in achieving this goal is affected by 1) the local invasiveness of the tumor; 2) the anatomic location; and 3) the surgical accessibility of the tumor. Cardiac autotransplantation was developed for left atrial primary cardiac neoplasms to establish a method of surgical access and to facilitate resection of the tumor and reconstruction of the heart in an area of difficult anatomy, thus eliminating the need for donor organs and the immunosuppression attendant upon orthotopic cardiac transplantation.
For left atrial primary cardiac sarcomas, there are 3 potential surgical approaches. The first is a method in which the surgeon leaves the heart in situ and opens the left atrium via any of the approaches used for standard mitral valve or left atrial surgery. Although this method may work well for small or posteriorly situated left atrial tumors, it is not as effective for large anterior tumors, which can still be difficult to see, resect, and reconstruct in the area of the mitral valve anterior leaflet and the aortic root. This might explain why local recurrence is common after this approach. 3,5 The 2nd approach is standard orthotopic cardiac transplantation. Although this method provides the best possibility for complete excision, it necessitates use of a scarce donor organ, in addition to lifelong immunosuppression, with its known complications and cost and the unknown effect of immunosupression on any remaining malignant cells. 6–8 The 3rd approach is cardiac autotransplantation.
Cardiac Autotransplantation
Cardiac autotransplantation in the animal laboratory was an integral part of the early development of cardiac transplantation and resulted in satisfactory cardiac function despite disconnection of the heart from the autonomic nervous system and the lymphatic system. 9–12 Clinical human orthotopic heart transplantation was developed by Barnard in South Africa 13 and Cooley in the United States. 14 Their work confirmed that an explanted human heart could function when reimplanted.
Autotransplantation of the human heart was first attempted for treatment of Prinzmetal's angina 15,16 but was soon abandoned because of the high morbidity and mortality rates associated with the procedure. The technique was reintroduced by Dr. Cooley in 1985 as an approach to a large left atrial pheochromocytoma that could not be resected by standard means. 17 Although the procedure was technically accomplished, the patient developed severe coagulopathy from the very vascular neuroendocrine tumor and subsequently died. This initial experience served as the impetus for the 1st successful cardiac autotransplantation for primary cardiac malignancy, which was performed by Reardon and colleagues. 18 The patient was a 20-year-old man who was in congestive heart failure (New York Heart Association functional class IV) and had a large, recurrent, malignant fibrous histiocytoma of the left atrium. 18 The surgical success of this procedure was built upon prior experience, since Dr. Reardon was Dr. Cooley's resident and was first assistant at Dr. Cooley's 1985 procedure. Further knowledge and experience gained from our respective programs in heart transplantation, complex congenital defect reconstruction, and valve reconstruction, as well as improvements in myocardial protection, have enabled the development of cardiac autotransplantation.
Surgical Technique
Cardiac autotransplantation differs from standard orthotopic cardiac transplantation in several technical details. First, the right atrial anastomosis must be performed in a bicaval fashion to preserve the coronary sinus. Second, unlike standard orthotopic heart transplantation (in which excess tissue can be left in the recipient and excess tissue harvested from the donor to allow tailoring), excision of the heart in cardiac autotransplantation must be precise, and important structures such as the coronary sinus must be carefully preserved during excision. Furthermore, reimplantation suture lines take up tissue and “shrink” the heart. Resection and reconstruction of the heart is further complicated by the lack of excess tissue for tailoring. Having set forth these limitations, we will proceed with the description of our technique for cardiac autotransplantation and the technical points of interest.
Cannulation for cardiopulmonary bypass and cardiac autotransplantation differs slightly from our standard techniques. The distal ascending aorta can be cannulated for arterial return in the routine fashion. However, venous cannulation must be done in such a way as to allow bicaval excision and reanastomosis. Therefore, the superior vena cava is mobilized by dividing the pericardium along the superior vena cava to the innominate vein. This enables exposure and direct cannulation of the superior vena cava, with at least 1 cm of caval tissue left below the cannula for division and reanastomosis. Inferior vena cava cannulation and reconstruction tends to be the most problematic. The inferior vena cava should be mobilized from its diaphragmatic attachment in order to allow low cannulation into the anterolateral inferior vena cava. At least 1 cm of inferior vena cava should be left between the cannula and the right atrium for division and reconstruction. When divided, this area retracts; therefore, as much tissue as possible should be left in the inferior vena cava for reimplantation of the heart.
Cardiopulmonary bypass is instituted, and the ascending aorta and pulmonary artery are dissected free of one another. Caval tapes are placed, the aorta is cross-clamped, and standard, cold-blood, antegrade, potassium cardioplegia is administered. The caval tapes are tightened, and the interatrial groove is dissected free. The left atrium is then opened just posterior to the interatrial groove, and the tumor is examined. In the event that the tumor is too large or is situated in a position such that it cannot be adequately seen despite extensive opening of the superior vena cava, the superior vena cava can be transected 1 cm below the cannula and the inferior vena cava transected 1 cm above the cannula. The ascending aorta is divided just beyond the sinotubular junction, and the pulmonary artery is divided 1 cm proximal to its bifurcation. The left atrium is then excised just anterior to the pulmonary veins; the incision must be posterior to the mitral valve and the atrial appendage (Fig. 1). This enables removal of the heart, which is placed in a bucket of ice. The posterior pericardium is then examined for any tumor, which, if present, is resected and replaced with pericardium. With the heart outside the chest (in ice), it can be inverted so that the left atrium is now the anterior structure, which provides excellent exposure of the tumor for radical resection and precise reconstruction (Fig. 2). This repositioning also permits the direct administration of antegrade cardioplegia into the left main coronary artery during the repair of any areas of bleeding. The heart is reimplanted with use of a running 3-0 polypropylene suture for the left atrial anastomosis—a technique very similar to that used in standard orthotopic cardiac transplantation (Fig. 3). Careful attention must be paid to the orientation of the heart: there is very little margin for error in lining up the superior and inferior vena cavae. The inferior vena cava is then repaired with a running 4-0 polypropylene suture. If the gap appears to be too wide for suturing alone, a 20-mm GORETex® graft can be used to span the gap without difficulty (Fig. 4). The superior vena cava is closed with a running 4-0 polypropylene suture, and the great arteries are then closed with the same sized running suture. Postoperative care is quite similar to that given to patients undergoing orthotopic heart transplantation; however, no immunosuppression is necessary.
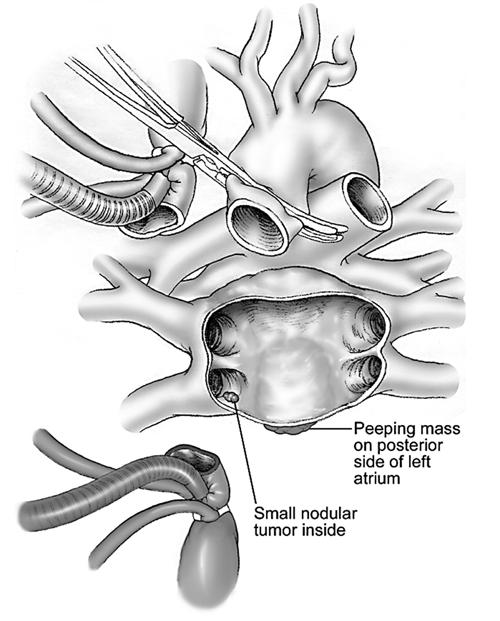
Fig. 1 Excision of the left a trium and removal of the posterior left atrial tumor.
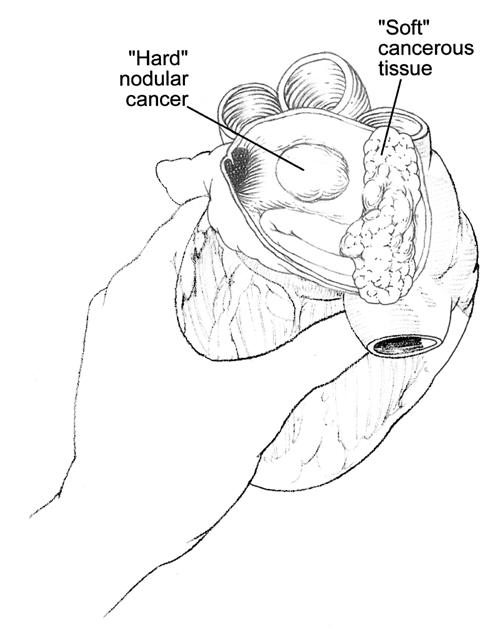
Fig. 2 Ease of manipulation of the heart allows excellent visibility and accessibility to the tumors.
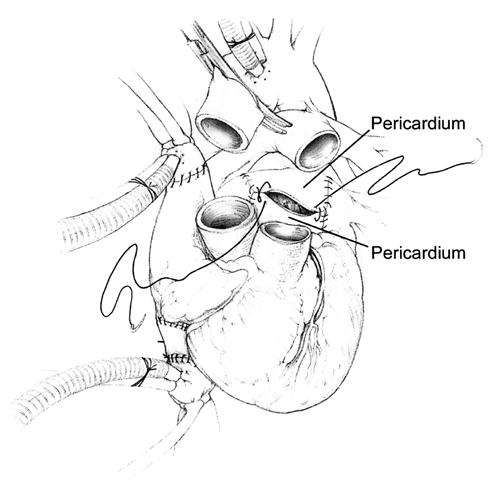
Fig. 3 Reimplantation technique.
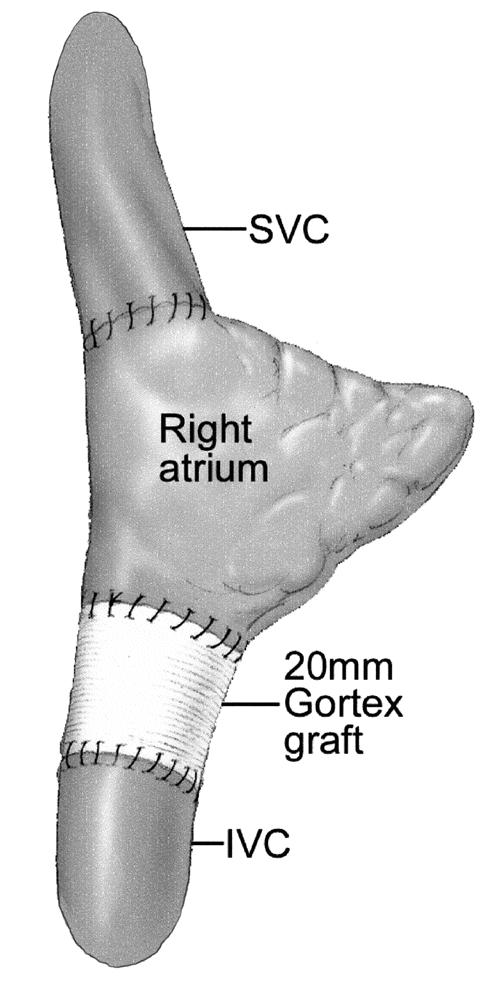
Fig. 4 Repair of the gap created in the inferior vena cava.
IVC = inferior vena cava; SVC = superior vena cava
In conclusion, this technique has proved useful in the approach to complex left atrial primary cardiac malignancies and was developed on the basis of Dr. Cooley's work at the Texas Heart Institute.
Editorial Commentary
Clinical experience and success of cardiac transplantation reveals the feasibility of explantation and reimplantation of the heart for major reconstruction. Although the long-term results of the technique for malignant tumors may prove disappointing, the method should be better suited for extensive benign lesions. Transplantation interrupts the lymphatic flow and also the extrinsic nervous connections of the heart. Modifications of the incisions used for explantation may be applicable in managing certain intractable dysrhythmias.
Follow-up on Dr. Reardon's experience with cardiac autotransplantation should reveal important facts for clinical practice.
Denton A. Cooley, MD
Surgeon-in-Chief, Texas Heart Institute at St. Luke's Episcopal Hospital, Houston
References
- 1.Dein JR, Frist WH, Stinson EB, Miller DC, Baldwin JC, Oyer PE, et al. Primary cardiac neoplasms. Early and late results of surgical treatment in 42 patients. J Thorac Cardiovasc Surg 1987;93:502–11. [PubMed]
- 2.Murphy MC, Sweeney MS, Putnam JB Jr, Walker WE, Frazier OH, Ott DA, Cooley DA. Surgical treatment of cardiac tumors: a 25-year experience. Ann Thorac Surg 1990; 49:612–8. [DOI] [PubMed]
- 3.Okita Y, Miki S, Ueda Y, Tahata T, Sakai T, Matsuyama K. Recurrent malignant fibrous histiocytoma of the left atrium with extracardiac extension. Am Heart J 1994;127:1624–8. [DOI] [PubMed]
- 4.Putnam JB Jr, Sweeney MS, Colon R, Lanza LA, Frazier OH, Cooley DA. Primary cardiac sarcomas. Ann Thorac Surg 1991;51:906–10. [DOI] [PubMed]
- 5.Gabelman C, Al-Sadir J, Lamberti J, Fozzard HA, Laufer E, Replogle RL, Myerowitz PD. Surgical treatment of recurrent primary malignant tumor of the left atrium. J Thorac Cardiovasc Surg 1979;77:914–21. [PubMed]
- 6.Gowdamarajan A, Michler RE. Therapy for primary cardiac tumors: is there a role for heart transplantation? Curr Opin Cardiol 2000;15:121–5. [DOI] [PubMed]
- 7.Goldstein DJ, Oz MC, Rose EA, Fisher P, Michler RE. Experience with heart transplantation for cardiac tumors. J Heart Lung Transplant 1995;14:382–6. [PubMed]
- 8.Michler RE, Goldstein DJ. Treatment of cardiac tumors by orthotopic cardiac transplantation. Semin Oncol 1997;24:534–9. [PubMed]
- 9.Willman VL, Cooper T, Cian LG, Hanlon CR. Autotransplantation of the canine heart. Surg Gynecol Obstet 1962; 115:229. [PubMed]
- 10.Dong E, Hurley DJ, Lower RR, Shumway NE. Performance of the heart two years after autotransplantation. Surgery 1964;56:270. [PubMed]
- 11.Willman VL, Cooper T, Kaiser GC, Hanlon CR. Cardiovascular response after cardiac autotransplant in primates. Arch Surg 1965;91:805–6. [DOI] [PubMed]
- 12.Daggett WM, Willman VL, Harada Y, Barner HB, Cooper T, Hanlon CR. Work capacity and efficiency of the autotransplanted heart. Surg Forum 1966;17:222–4. [PubMed]
- 13.Barnard CN. The operation. A human cardiac transplant: an interim report of a successful operation performed at Groote Schuur Hospital, Cape Town. S Afr Med J 1967;41:1271–4. [PubMed]
- 14.Cooley DA, Bloodwell RD, Hallman GL, Nora JJ. Transplantation of the human heart. Report of four cases. JAMA 1968;205:479–86. [PubMed]
- 15.Bertrand ME, Lablanche JM, Tilmant PY, Ducloux G, Warembourg H Jr, Soots G. Complete denervation of the heart (autotransplantation) for treatment of severe, refractory coronary spasm. Am J Cardiol 1981;47:1375–8. [DOI] [PubMed]
- 16.Clark DA, Quint RA, Mitchell RL, Angell WW. Coronary artery spasm. Medical management, surgical denervation, and autotransplantation. J Thorac Cardiovasc Surg 1977; 73:332–9. [PubMed]
- 17.Cooley DA, Reardon MJ, Frazier OH, Angelini P. Human cardiac explantation and autotransplantation: application in a patient with a large cardiac pheochromocytoma. Tex Heart Inst J 1985;12:171–6. [PMC free article] [PubMed]
- 18.Reardon MJ, DeFelice CA, Sheinbaum R, Baldwin JC. Cardiac autotransplant for surgical treatment of a malignant neoplasm. Ann Thorac Surg 1999;67:1793–5. [DOI] [PubMed]
Footnotes
Address for reprints: Michael J. Reardon, MD, 6565 Fannin, #A853, Houston, TX 77030


