Abstract
Interrupted aortic arch is a rare congenital malformation of the aortic arch that occurs in 3 per million live births. Defined as a loss of luminal continuity between the ascending and descending portions of the aorta, this anomaly entails a very poor prognosis without surgical treatment. To our knowledge, the world medical literature contains only 12 reports of isolated interrupted aortic arch diagnosed in adults. Nine of these patients underwent successful surgical repair, but 1 died during the early postoperative period. We describe a 10th successful surgical repair, which involved a 42-year-old woman who had an asymptomatic type B interrupted aortic arch (characterized by interruption between the left subclavian and left carotid arteries). We performed a single-stage extra-anatomic repair by placing a 16-mm extra-anatomic Dacron graft between the ascending and descending portions of the thoracic aorta and by interposing a 7-mm extra-anatomic Dacron graft between the 16-mm graft and the left subclavian artery. The patient recovered uneventfully and continued to do well 6 months later. (Tex Heart Inst J 2002;29:118–21)
Key words: Anastomosis, surgical, extra-anatomic; aorta, thoracic/abnormalities/surgery; blood vessel prosthesis; female; heart defects, congenital/surgery; human
Interrupted aortic arch (IAA) is a rare congenital malformation that occurs in 3 per million live births. 1 This anomaly is defined as a loss of luminal continuity between the ascending and descending portions of the aorta. 2 In most cases, IAA is associated with an intracardiac malformation such as ventricular septal defect, patent ductus arteriosus, bicuspid aortic valve, left ventricular outflow tract obstruction, or aortopulmonary window.
Interrupted aortic arch was initially described in 1778 by Steidele. 3 The 1st classification system, introduced by Celoria and Patton 4 in 1959, is still used almost universally. This system describes and classifies the site of aortic arch discontinuity, which may be distal to the left subclavian artery (type A); between the left carotid and left subclavian arteries (type B); or between the innominate and left carotid arteries (type C). The most common type is B (53%), followed by A (43%) and C (4%).
To our knowledge, the world medical literature contains only 12 cases of isolated IAA in adults (18 years and older). Nine of these patients underwent successful surgical repair, one of whom died during the early postoperative period. 1,5–10 We describe a 10th successful surgical repair, performed with a single-stage extra-anatomic technique.
Case Report
In November 2001, a 42-year-old woman presented at our hospital because of swelling of her left leg, which had begun 3 days earlier and had been followed by swelling in her right leg. She related a history of increased blood pressure in her right arm; this problem had been observed after the birth of her 2nd child and again after the birth of her 3rd child.
On physical examination, peripheral pulses were palpable over the carotid arteries and in the upper limbs, with a radial pulse that was stronger in the right arm than in the left. Bounding pulses in the neck were also detected. The blood pressure was 144/70 mmHg in the right arm and 82/59 mmHg in the left arm. Lower-limb pulses were not palpable. Echocardiography was not performed, and chest radiography revealed no pathologic abnormalities.
Cardiac catheterization showed occlusion of the thoracic aorta distal to the left carotid artery. The innominate artery, right internal mammary artery, and right common carotid artery were dilated. In addition, the left subclavian artery showed retrograde filling. Magnetic resonance angiography revealed severe hypoplasia of the transverse aortic arch proximal to the origin of the left subclavian artery (Fig. 1). Both common carotid arteries were dilated. The descending thoracic aorta was supplied by extensive collateral vessels from the vertebrobasilar system down to the posterior chest wall and the spine. In accordance with the results of cardiac catheterization, retrograde flow could be seen in the proximal left subclavian artery and the left vertebral artery.

Fig. 1 Preoperative, contrast-enhanced, 3-dimensional, magnetic resonance angiogram (lateral view) reveals severe hypoplasia of the transverse aortic arch (arrow) between the origins of the left common carotid and left subclavian arteries (interrupted aortic arch, type B). Extensive collateral vessels are evident in the paraspinal region (arrowheads) and involve the vertebrobasilar system (asterisk). The dark gray areas show vessels with antegrade flow, and the light gray areas denote those with retrograde flow.
A single-stage operation was performed through a midline sternotomy and a left supraclavicular incision. The aorta was cannulated in the standard fashion, and a 52-F single-stage cannula was inserted into the right atrial appendage for venous return. After the left subclavian artery was exposed, a 7-mm Dacron graft (Hemashiel®, Boston Scientific Corporation; Natick, Mass) was anastomosed to the left subclavian artery, in end-to-side fashion, with a running 5-0 polypropylene suture. The graft was tunneled between the innominate vein and the aortic arch. Cardiopulmonary bypass was then initiated. A 16-mm Dacron graft (Hemashield®) was anastomosed end-to-side to the descending thoracic aorta with a running 4-0 polypropylene suture. The graft was then passed posteriorly around the right atrium. The aorta was cross-clamped, and antegrade cardioplegia was delivered through the aortic root to induce diastolic cardiac arrest. The proximal portion of the 16-mm graft was then anastomosed to the ascending aorta, in end-to-side fashion, with a running 4-0 polypropylene suture. Finally, the distal end of the 7-mm graft was anastomosed end-to-side to the proximal end of the 16-mm graft with a similar suture (Fig. 2).

Fig. 2 Intraoperative photograph shows the distal end of the 7-mm graft, which has been anastomosed end-to-side to the proximal end of the 16-mm graft.
There were no perioperative complications, and postoperative bleeding was minimal. Postoperative magnetic resonance angiography revealed patent grafts and good distal flow (Figs. 3A and 3B). The patient recovered uneventfully and was discharged from the hospital on postoperative day 10. Six months later, she continued to do well.
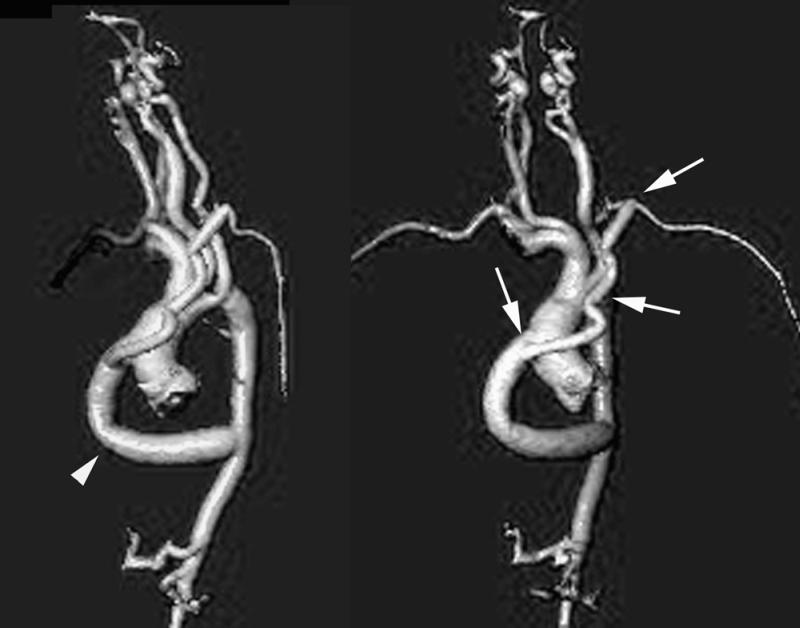
Fig. 3 Postoperative, contrast-enhanced, 3-dimensional, magnetic resonance angiograms. A) The lateral view reveals severe hypoplasia of the transverse arch, as in Figure 1. However, the patient now has 2 grafts: the larger, 16-mm graft (arrowhead) is anastomosed end-to-side to the mid-portion of the ascending aorta and to the distal portion of the descending thoracic aorta. B) The shallow left anterior oblique projection shows the smaller, 7-mm graft (arrows), which has been sutured end-to-side to the proximal 16-mm graft and to the left subclavian artery.
Discussion
Interrupted aortic arch is a rare congenital malformation defined as a complete absence of flow between 2 portions of the aorta. In infants, its clinical presentation involves severe congestive heart failure; if the condition is left untreated, 90% of the affected infants die at a median age of 4 days. 11 In the few documented cases in adults, the presentation ranges from a lack of symptoms to limb swelling with differential blood pressures in all extremities. Substantial collateral circulation must be present to maintain flow and enable survival. However, collateral vessels are subject to atrophy and atherosclerosis, which can lead to other challenging problems. 12
In adults, IAA is so rare that our review of the literature revealed only 12 cases. Nine of the patients underwent surgical repair (Table I 1,5–10); 6 of the IAAs were type A lesions. One of the patients, who had otherwise undergone a successful repair, developed pericardial tamponade on the 10th postoperative day. Surgical re-exploration showed no active bleeding; nevertheless, the patient had a recurrent effusion and died of shock and multiorgan failure. 1
Table I. Adult Patients with Surgical Repair of Isolated Interrupted Aortic Arch
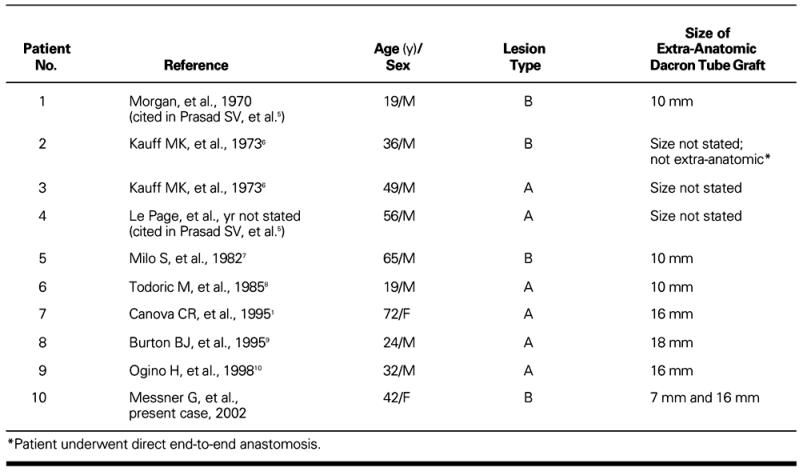
Initially, the issue of whether to repair an interrupted aortic arch in 1 stage or in 2 was controversial, but single-stage repair is now considered the best treatment in infants. 13 Most reported cases in adults have been repaired in 1 stage by means of an extra-anatomic approach (Table I). 1,5–9 One patient, a 36-year-old man with a type B interruption, underwent repair by direct end-to-end anastomosis. 6 Ogino and colleagues 10 performed a 2-stage repair of a type A lesion in a 32-year-old man because of concern about possible intraoperative hemorrhage from the patient's well-developed collateral vessels. We repaired our patient's type B interrupted arch in 1 stage with a 16-mm Dacron graft, including subclavian artery bypass with a 7-mm graft. These procedures resulted in minimal intraoperative blood loss and complete postoperative recovery without neurologic sequelae.
In conclusion, interrupted aortic arch is rarely encountered in an adult patient. When it does occur, the malformation may be repaired in a single-stage procedure with a low risk of morbidity and mortality. Because so few cases have been reported, no meaningful statistical inferences can be made as to whether 1-stage or 2-stage repair is better.
Footnotes
Address for reprints: George J. Reul, MD, Department of Cardiovascular Surgery, Texas Heart Institute, MC 3-258, P.O. Box 20345, Houston, TX 77225-0345
References
- 1.Canova CR, Carrel T, Dubach P, Turina M, Reinhart WH. Interrupted aortic arch: fortuitous diagnosis in a 72-year-old female patient with severe aortic insufficiency [in German]. Schweiz Med Wochenschr 1995;125(1–2):26–30. [PubMed]
- 2.Backer CL, Mavroudis C. Congenital Heart Surgery Nomenclature and Database Project: patent ductus arteriosus, coarctation of the aorta, interrupted aortic arch. Ann Thorac Surg 2000;69(4 Suppl):S298–307. [DOI] [PubMed]
- 3.Steidele RJ. Samml Chir u Med Beob (Vienna) 1778;2:114.
- 4.Celoria GC, Patton RB. Congenital absence of the aortic arch. Am Heart J 1959;58:407–13. [DOI] [PubMed]
- 5.Prasad SV, Gupta SK, Reddy KN, Murthy JS, Gupta SR, Somnath HS. Isolated interrupted aortic arch in adult. Indian Heart J 1988;40:108–12. [PubMed]
- 6.Kauff MK, Bloch J, Baltaxe HA. Complete interruption of the aortic arch in adults. Radiology 1973;106:53–7. [DOI] [PubMed]
- 7.Milo S, Massini C, Goor DA. Isolated atresia of the aortic arch in a 65-year-old man. Surgical treatment and review of published reports. Br Heart J 1982;47:294–7. [DOI] [PMC free article] [PubMed]
- 8.Todoric M, Martinovic N, Jablanov J, Albreht M, Aleksandrov R, Prcovic M. Interrupted aortic arch—case report of a patient successfully operated on in adulthood [in Serbo-Croatian (Roman)]. Acta Chir Iugosl 1985;32:201–6. [PubMed]
- 9.Burton BJL, Kallis P, Bishop C, Swanton H, Pattison CW. Aortic root replacement and extra-anatomic bypass for interrupted aortic arch in an adult. Ann Thorac Surg 1995; 60:1400–2. [DOI] [PubMed]
- 10.Ogino H, Miki S, Matsubayashi K, Ueda Y, Nomoto T. Two-stage repair for aortic regurgitation with interrupted aortic arch. Ann Thorac Surg 1998;65:1151–3. [DOI] [PubMed]
- 11.Collins-Nakai RL, Dick M, Parisi-Buckley L, Fyler DC, Castaneda AR. Interrupted aortic arch in infancy. J Pediatr 1976;88:959–62. [DOI] [PubMed]
- 12.Kreiger KH, Spencer FC. Is paraplegia after repair of coarctation of the aorta due principally to distal hypotension during aortic cross-clamping? Surgery 1985;97:2–7. [PubMed]
- 13.Yasui H, Kado H, Yonenaga K, Kawasaki S, Shiokawa Y, Kouno H, et al. Revised technique of cardiopulmonary bypass in one-stage repair of interrupted aortic arch complex. Ann Thorac Surg 1993;55:1166–71. [DOI] [PubMed]


