Abstract
We report a very rare case of a 47-year-old man who had coronary spasm that resulted in a silent myocardial infarction, a ruptured myocardial wall, and a nonruptured left ventricular pseudoaneurysm. The patient presented with a 6-month history of dyspnea on exertion, without evidence of fixed coronary artery stenosis. Coronary angiography showed severe coronary spasm of the left anterior descending and left circumflex arteries; the spasm was relieved promptly by nitroglycerin. Echocardiography and left ventricular angiography revealed the large left ventricular pseudoaneurysm posterolateral to the left ventricle. We performed surgical resection of the pseudoaneurysm and patch repair of the ruptured left ventricular wall, with excellent results.
We present this case because of the highly unusual sequence of events. Early surgical intervention resulted in the patient's recovery. (Tex Heart Inst J 2002;29:122–5)
Key words: Aneurysm, false/diagnosis/surgery; coronary vasospasm; heart rupture, post-infarction/diagnosis/surgery; heart ventricle; human; male; middle age; myocardial infarction/complications
Left ventricular pseudoaneurysm is a rare clinical entity. Rupture of the myocardial wall typically results in immediate collapse of the patient and electromechanical dissociation. In rare cases, however, the rupture is contained by pericardial and fibrous tissue, and the result is a pseudoaneurysm. 1–4 The left ventricular (LV) pseudoaneurysm, in contrast to a true LV aneurysm, contains only pericardial and fibrous elements in its wall—no myocardial tissue. Because of the tendency of LV pseudoaneurysms to rupture, early surgical intervention is recommended. 3
In this case report, we present a patient who underwent successful repair of a LV nonruptured pseudoaneurysm, which followed a silent myocardial infarction that presumably was caused by spasm of the left circumflex coronary artery.
Case Report
In March 2000, a 47-year-old man presented at our institution with history of dyspnea (New York Heart Association functional class III), which had been insidious in onset and slowly progressive over a period of 6 months. He had also been experiencing paroxysmal nocturnal dyspnea, palpitations, and extreme fatigability on exertion, but no angina or syncope. There was no family history of hyperlipidemia or ischemic heart disease, and the patient's lipid profile was within normal limits. He had developed adult-onset diabetes 4 years earlier. He was a heavy cigarette smoker.
The physical examination revealed a regular pulse rate of 90 beats/min, a blood pressure of 110/70 mmHg, and an elevated jugular venous pulse with prominent v waves and a steep y descent. A precordial examination showed an apical impulse in the 6th intercostal space. Pulsations were evident in the 3rd, 4th, and 5th intercostal spaces lateral to the midclavicular line, moving outward during systole. A grade 2/3 parasternal lift and a palpable pulmonary component of the 2nd heart sound were present. He had a grade 2/6 pansystolic murmur in the mitral valve area and a grade 3/6 pansystolic murmur in the tricuspid valve area that increased on inspiration. The liver was enlarged 10 cm below the costal margin and pulsated on systole. The patient had normal vesicular breathing with basal rales.
Electrocardiography showed sinus rhythm, a qR pattern with ST elevation and T wave inversion in leads I and aVL, and a prominent R wave in lead V1, which suggested an old posterolateral infarction. Chest radiographs in the posteroanterior and lateral views showed cardiomegaly with a cardiothoracic ratio of 0.8, biatrial enlargement, bulging of the left border of the heart suggesting LV aneurysm, and grade 2 pulmonary venous congestion. Echocardiography showed mild LV dysfunction with an ejection fraction of 0.48, and akinesia of the inferior septum, posterior wall, and basal lateral wall. There was a large LV pseudoaneurysm 5 measuring 7.4 × 4.8 cm posterolateral to the left ventricle, communicating through a narrow neck of 3 mm in diameter, with ragged margins in the basal lateral wall of the left ventricle (Fig. 1). Color-flow Doppler echocardiography showed turbulence across the neck of the aneurysm. The Doppler tracing showed systolic flow into the pseudoaneurysm and diastolic flow away from the aneurysm into the LV cavity (Fig. 2). 6,7 The patient had moderate mitral regurgitation (grade 2/4) and moderately severe tricuspid regurgitation (grade 3/4); the pulmonary artery pressure level, as determined from the tricuspid regurgitation, was 52 mmHg.
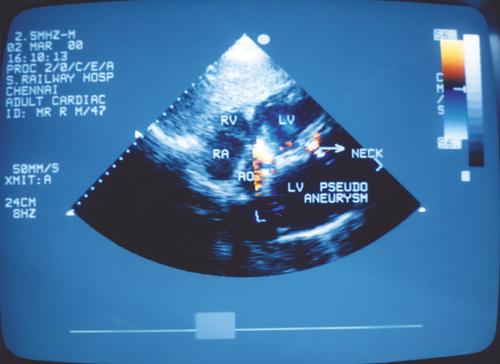
Fig. 1 Echocardiography in the subcostal view shows the left ventricular pseudoaneurysm communicating through a narrow neck in the posterolateral wall of the left ventricle.
Ao = aorta; LV = left ventricle; RA = right atrium; RV = right ventricle
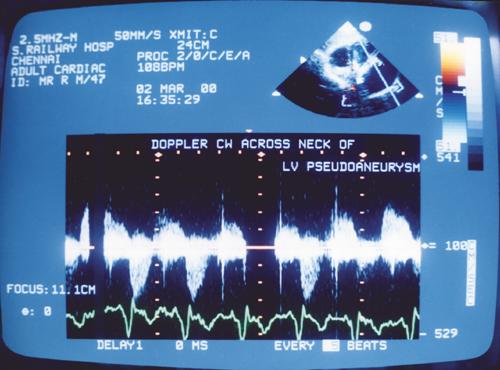
Fig. 2 Continuous Doppler flow across the neck of the pseudoaneurysm shows systolic flow into the pseudoaneurysm and diastolic flow away from the pseudoaneurysm into the left ventricular (LV) cavity.
During coronary angiography, selective left coronary injection with non-ionic contrast medium showed spontaneous severe spasm of the left anterior descending artery and the left circumflex artery over a long segment in their mid-portions (Fig. 3). Normal flow was restored after the administration of 100 μg of intracoronary nitroglycerin (Fig. 4). There was no luminal irregularity and no evidence of a fixed stenotic lesion. The right coronary artery was dominant and normal.
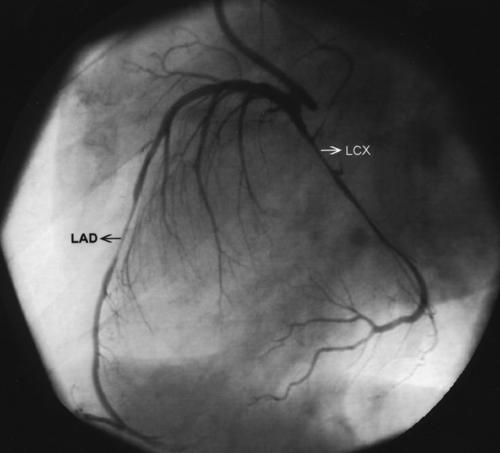
Fig. 3 A left coronary angiogram in the left anterior oblique view shows spontaneous spasm of the mid-portion of the left anterior descending (LAD) and left circumflex (LCX) arteries (arrows).
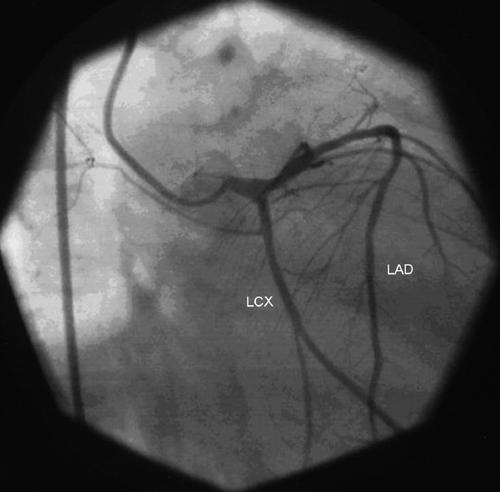
Fig. 4 A left coronary angiogram in the right anterior oblique view shows restoration of normal flow in the left anterior descending (LAD) and left circumflex (LCX) arteries after intracoronary nitroglycerin administration.
Left ventricular angiography showed grade 2 mitral regurgitation and a large LV pseudoaneurysm originating from the lateral wall of the left ventricle (Fig. 5). We made a diagnosis of vasospastic coronary artery disease with silent infarction and rupture of the posterolateral wall, resulting in a LV pseudoaneurysm. At surgery, a large nonruptured posterolateral pseudoaneurysm was seen to communicate through multiple sieve-like openings beneath the posterior papillary muscle. The pseudoaneurysm was resected, and the rupture in the posterolateral wall of the left ventricle was repaired with a polytetrafluoroethylene patch and suture that was reinforced with pledgets of autologous pericardium. Intraoperative transesophageal echocardiography revealed only mild mitral regurgitation; therefore, the mitral valve was left alone.
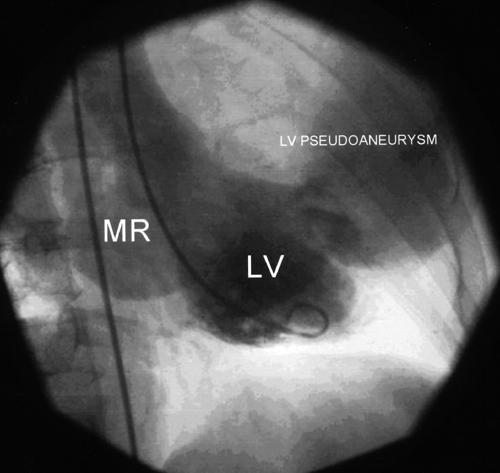
Fig. 5 A left ventriculogram in the right anterior oblique view shows a large left ventricular pseudoaneurysm arising from the lateral wall of the left ventricle and grade 2 mitral regurgitation.
LV = left ventricle; MR = mitral regurgitation
At the 1-year follow-up visit, the patient was in New York Heart Association functional class I and was taking minimal medications.
Discussion
Left ventricular pseudoaneurysms are prone to rupture; 2 however, there are occasional reports of prolonged survival of a patient with an unruptured LV pseudoaneurysm. 4 Left ventricular pseudoaneurysms are most commonly caused by myocardial infarction secondary to atherosclerotic coronary artery disease. However, occurrences after trauma, 8 infective endocarditis, 9 inflammation, 10 and cardiac surgery 11 have been reported. The commonest location of LV pseudoaneurysms is posterolateral, in contrast to true LV aneurysms, which are typically situated in the anterior and apical walls. 3,12,13
Patients with LV pseudoaneurysms usually present with congestive heart failure, arrhythmias, and embolism; the risk of rupture is high. Myocardial infarction rarely occurs in patients with normal coronary arteries; however, when this does occur, it is considered secondary to coronary spasm or coronary thrombosis. 14 In the world medical literature, we found only 2 case reports of myocardial rupture in patients with normal coronary arteries. 15,16 We found only 1 earlier report of a patient who had a LV pseudoaneurysm without major obstruction to the epicardial coronary arteries. Unlike our patient, that patient had a diagonal lesion, and coronary spasm was not demonstrated. 17 In our patient, coronary spasm was convincingly shown; therefore, spasm was considered the most likely cause of the posterolateral myocardial infarction. The myocardial infarction led to rupture of the posterolateral wall of the left ventricle, which, in turn, resulted in the left ventricular pseudoaneurysm. To our knowledge, this is the 1st report of these events occurring in this particular sequence.
Footnotes
Address for reprints: K.A. Abraham, MD, DM, FACC, FRCP (Lond), Chief Cardiologist, Railway Hospital, Ayanavaram, Chennai 600023, India
References
- 1.Treasure T. False aneurysm of the left ventricle [editorial]. Heart 1998;80:7–8. [PMC free article] [PubMed]
- 2.Vlodaver Z, Coe JI, Edwards JE. True and false left ventricular aneurysms. Propensity for the latter to rupture. Circulation 1975;51:567–72. [DOI] [PubMed]
- 3.Komeda M, David TE. Surgical treatment of postinfarction false aneurysm of the left ventricle. J Thorac Cardiovasc Surg 1993;106:1189–91. [PubMed]
- 4.Hung MJ, Wang CH, Chang WJ. Unruptured left ventricular pseudoaneurysm following myocardial infarction. Heart 1998;80:94–7. [PMC free article] [PubMed]
- 5.Catherwood E, Mintz GS, Kotler MN, Parry WR, Segal BL. Two-dimensional echocardiographic recognition of left ventricular pseudoaneurysm. Circulation 1980;62:294–303. [DOI] [PubMed]
- 6.Roelandt JR, Sutherland GR, Yoshida K, Yoshikawa J. Improved diagnosis and characterization of left ventricular pseudoaneurysm by Doppler color flow imaging. J Am Coll Cardiol 1988;12:807–11. [DOI] [PubMed]
- 7.Rueda B, Panidis J, Gonzales R, McDonough M. Left ventricular pseudoaneurysm: detection and postoperative follow-up by color Doppler echocardiography. Am Heart J 1990;120:990–2. [DOI] [PubMed]
- 8.Symbas PN, Ware RE, Belenkie I, Nutter DO. Traumatic biventricular pseudoaneurysm of the heart with ventricular septal defect. J Thorac Cardiovasc Surg 1972;64:647–51. [PubMed]
- 9.Fiorilli R, Tomasco B, Tesler UF. Pseudoaneurysm of the left ventricle: a rare sequela to mitral valve endocarditis. Tex Heart Inst J 1999;26:309–11. [PMC free article] [PubMed]
- 10.Reinecke H, Wichter T, Weyand M. Left ventricular pseudoaneurysm in a patient with Dressler's syndrome after myocardial infarction. Heart 1998;80:98–100. [DOI] [PMC free article] [PubMed]
- 11.Mackenzie JW, Lemole GM. Pseudoaneurysm of the left ventricle. Tex Heart Inst J 1994;21:296–301. [PMC free article] [PubMed]
- 12.Yeo TC, Malouf JF, Reeder GS, Oh JK. Clinical characteristics and outcome in postinfarction pseudoaneurysm. Am J Cardiol 1999;84:592–5,A8. [DOI] [PubMed]
- 13.Sharma S, Mukherjee K, Trivedi A, Pinto R, Bhattacharyya SS. Clinical profile and management of post infarction left ventricular pseudoaneurysm. Indian Heart J 1995;47:369–71. [PubMed]
- 14.Lindsay J Jr, Pichard AD. Acute myocardial infarction with normal coronary arteries. Am J Cardiol 1984;54:902–4. [DOI] [PubMed]
- 15.St Louis P, Rippe JM, Benotti JR, Frankel PW, Vandersalm T, Alpert JS. Myocardial infarction with normal coronary arteries complicated by ventricular septal rupture. Am Heart J 1984;107:1259–63. [DOI] [PubMed]
- 16.Trigano JA, Mourot F, Remond JM, Cabibel JP, Jouven JC, Torresani J. Free ventricular wall rupture in acute myocardial infarction with normal coronary arteries. Am Heart J 1987;113:1027–9. [DOI] [PubMed]
- 17.Tesler UF, Leccese A. Pseudoaneurysm of the free wall of the left ventricle without obstruction of major coronary arteries. Tex Heart Inst J 1996;23:58–61. [PMC free article] [PubMed]


