Abstract
Introduction
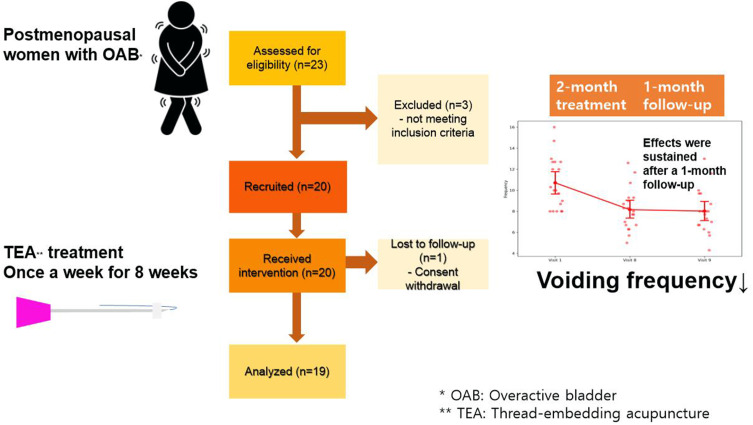
Overactive bladder is a major public health concern that negatively impacts a patient’s quality of life, and it is highly prevalent in menopausal women. Acupuncture has been suggested as a viable therapeutic approach. This study aimed to explore the effectiveness of thread-embedding acupuncture in postmenopausal women with overactive bladder.
Methods
This was a single-centre, single-arm, open-label study conducted on 20 postmenopausal women with overactive bladder. Participants received thread-embedding acupuncture treatment once a week for 8 weeks. Patients were evaluated using a bladder diary, overactive bladder symptom score (OABSS), and King’s Health Questionnaire (KHQ) at three time points: baseline, end of treatment (week 8), and 4 weeks after treatment completion (week 12).
Results
Nineteen participants completed the study. Average daily micturition frequency decreased significantly after thread-embedding acupuncture treatment (week 8: −2.55 ± 0.37, P=0.001, week 12: −2.69 ± 0.37, P=0.001). Daytime and nighttime micturition frequency and OABSS significantly decreased at week 8 and 12. However, no significant differences were observed in urgency, incontinence, or KHQ. No serious adverse events were reported.
Conclusion
Considering that thread-embedding acupuncture was shown to improve daily quality of life by reducing daytime and nighttime episodes, this pilot study suggests that thread-embedding acupuncture is a feasible alternative for treating overactive bladder.
Keywords: overactive bladder, postmenopausal women, quality of life, thread-embedding acupuncture, lower urinary tract symptoms
Graphical Abstract
Introduction
Overactive bladder (OAB) is a common condition that affects a significant proportion of the population, particularly women, with its prevalence known to increase with age.1 This condition is characterised by symptoms such as urinary urgency, frequency, nocturia, and, in some cases, urge incontinence.2 Postmenopausal women are at a higher risk owing to physiological changes such as reduced oestrogen levels and weakened pelvic floor muscles.3 The impact of OAB on quality of life and mental health highlights the critical need for effective and sustained treatment approaches. The prevalence of OAB increases with age and necessitates long-term therapy for sustained symptom management. Given its chronicity, OAB management is often long-term.4 Indeed, there are various treatment options for OAB, but the discontinuation rate is high for various reasons.5
OAB is conventionally managed through behavioural therapies and pharmacological interventions according to guidelines.6 Behavioural therapies, including behaviour modifications, pelvic floor exercises, and bladder retraining, require considerable time and effort and could thus be challenging for some individuals. Anti-muscarinic medications are typically prescribed, but they often have high discontinuation rates owing to side effects such as dry mouth and constipation.7 Surgical approaches such as intravesical botulinum toxin injections, sacral neuromodulation, augmentation cystoplasty, and urinary diversion are also considered.6 However, these approaches are invasive, and each option entails distinct risks and requires careful consideration.8 Therefore, some patients with OAB prefer to explore safe and effective alternative therapies, including acupuncture.
Some clinical studies on acupuncture for OAB have showed a significant effect on OAB.9–11 The studies included in a previous review11 required acupuncture treatment 5 times per week; one RCT found that after 16 sessions of treatment, both active and sham acupuncture significantly reduced the frequency of urgency urinary incontinence (UUI) and both daytime and nighttime urinary frequency.12 However, the necessity for regular and long-term visits poses an inconvenience to patients and reduces treatment adherence. Additionally, it imposes an economic burden on patients, adding to the time spent on frequent hospital visitation.
Thread-embedding acupuncture (TEA), a contemporary form of acupuncture, is a type of acupuncture retention. This involves the insertion of absorbable threads, which are made of degradable materials with non-toxic byproducts, at specific acupuncture points, to provide sustained stimulation and therapeutic effects.13,14 The beneficial long-term effects of TEA have gained attention as a viable treatment for chronic conditions.13 Several studies have assessed the effectiveness and safety of TEA in chronic conditions including urinary diseases.15,16 To the best of our knowledge, no research papers evaluating the effects of TEA on OAB have been published to date.
Reports on the potential benefits of acupuncture in alleviating OAB symptoms remain insufficient, and understanding acupuncture better could reduce the incidence of minor side effects in all patients.9–11 To this end, the present study aimed to investigate the effectiveness and safety of TEA in postmenopausal women with OAB.
Materials and Methods
Study Design
This prospective, single-arm study was designed to evaluate outcomes before and after the intervention. The trial protocol complied with the Transparent Reporting of Evaluations with Nonrandomized Designs and Standards for Reporting Interventions in Clinical Trials of Acupuncture guidelines. The study was approved by the Institutional Review Board of Dongguk University Ilsan Oriental Hospital (DUIOH 2022–07-003-004) and was prospectively registered at the Clinical Research Information Service (KCT0007892, 11/11/2022). All procedures in the study adhered to the Declaration of Helsinki. Full written informed consent was obtained from all participants prior to inclusion in the study.
Participants
The inclusion criteria were as follows: (1) age >40 years and not pregnant; (2) amenorrhea for ≥1 year and no history of hormone replacement therapy in the preceding 6 months; (3) frequent and urgent urination lasting for >3 months; (4) meeting the diagnostic criteria for OAB with a total score of ≥3 on the Korean version of the overactive bladder symptom score (OABSS);17 (5) urinary urgency as defined by the urgency rating scale (URS) as ≥2 points and an average urinary frequency of ≥8 times/day and/or UUI, according to a 3-day bladder diary, over a 1-week screening period; (6) agreement with study protocols after sufficient explanation.
The exclusion criteria were as follows: (1) pregnancy; (2) urinary tract infection upon urine examination; (3) stress urinary incontinence without OAB symptoms; (4) suspected urinary dysfunction due to neurological damage; (5) history of cystocele, uterine prolapse, or similar diseases; (6) history of obstructive uropathy conditions, such as urolithiasis or urinary tract tumours; (7) history of surgery on the urethra or bladder; (8) history of urinary tract malignancy; (9) history of neurological or psychiatric diseases; (10) presence of artificial pacemaker or implantable cardioverter-defibrillator in the chest; (11) experience of hypersensitivity or any other side effect after acupuncture treatment; (12) involvement in any other clinical trial in the preceding 3 months; (13) taking a drug that may affect bladder function within 1 month before trial commencement; (14) insufficient literacy to complete study documents.
Interventions
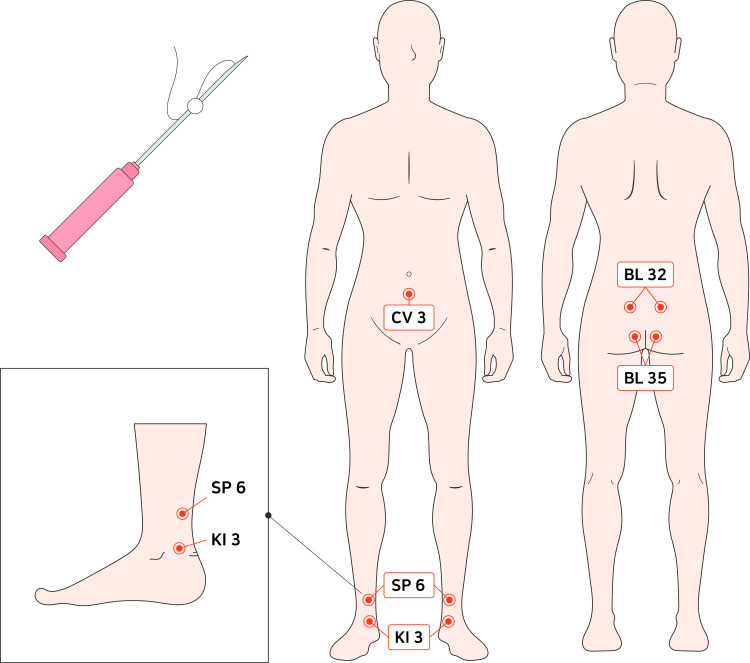
The participants received TEA once a week for 8 weeks using TEA needles (31G, 25 mm; Dong-Bang Acupuncture, Inc., Seoul, Korea) at 9 specific acupoints. These included the traditional acupuncture points CV3, SP6, KI3, BL32, and BL35; CV3 was unilaterally needled, whereas KI3, SP6, BL32, and BL35 were needled bilaterally (Figure 1). The details of the procedure were established through a consensus among clinical experts based on previous related studies.9–11,18–20
Figure 1.
A thread embedding acupuncture needle and location of acupuncture points.
Prior to each session, the skin was sterilised, and TEA was administered at the designated points. Practitioners, who were licensed Korean medicine doctors with at least one year of clinical experience, carefully inserted the TEA needles, leaving the absorbable polydioxanone thread in the body while immediately removing the needle. All interventions were performed using disposable TEA needles, and practitioners wore sterile gloves. Any other therapies for OAB during the course of this study were not allowed.
Assessment and Outcome Measures
Primary Outcome
The primary outcome for this trial was the change in the number of micturitions per 24 hours based on a 3-day bladder diary before and after treatment (baseline and week 8). A 3-day bladder diary was checked at visits 1 (baseline), 8 (week 8), and 9 (follow-up period, week 12). The diary submission included the time of each micturition and the intensity of urgency using a five-point scale (1=no urgency, 2=mild urgency, 3=moderate urgency, 4=severe urgency, and 5=UUI). Urinary urgency was defined in this study as a total count if the URS score recorded in the 3-day bladder diary was >2 points, indicating a mild urinary urgency symptom.
Secondary Outcomes
The secondary outcome measurement included daytime and nocturnal micturitions per 24 hours, the total number of urinary urgencies for 3 days, and the total number of UUI for 3 days, as identified using the same version of the 3-day bladder diary before and after treatment. The OABSS and King’s Health Questionnaire (KHQ) scores were used as secondary measurements. The Korean versions of the OABSS17 and KHQ21 were administered at the initial screening, visit 8, and visit 9.
The OABSS evaluates the severity of OAB symptoms by using a composite score ranging from 0 to 15, with higher scores indicating more severe symptoms.22 Severity is defined as mild if the total score is <5, severe if the score is 6–11, and most severe if the score is ≥12.
The KHQ is a self-described urinary symptom questionnaire used to assess the severity of urinary symptoms and the effect of urination symptoms on quality of life,23 with lower scores indicating better quality of life.
Safety Assessment
Safety assessment was conducted on all 20 participants enrolled in this study and treated at least once. The presence of adverse events (AEs) was monitored for the entirety of the study. Any undesirable or unintentional signs, symptoms, or diseases after the intervention/during the clinical period were considered AEs, regardless of their association with the intervention. The evaluator determined the severity (none, mild, moderate, or severe) and the correlation between the AE and the intervention (definitely related, probably related, possibly related, probably unrelated, definitely not related, or unclear). Vital signs were recorded at each visit along with physical at screening and laboratory tests, including urinalysis, at screening and visit 8.
Sample Size and Statistical Analysis
Because this was a preliminary pilot study for an advanced clinical trial, no sample size calculations were performed. The minimal sample size was determined to explore the effectiveness and safety of TEA treatment in OAB and was based on a previous study.24 The analysis was based on the modified intention-to-treat (ITT) set, which included participants who were enrolled but excluded if they were never treated for or diagnosed with the primary outcome. Continuous variables are presented as means ± standard deviations, and categorical variables are presented as frequencies (%). A linear mixed model for repeated measures was used to compare all outcome measurements over time. The least-squares mean and standard error over time were calculated using the model. The means differences and 95% confidence intervals for scores in visits 8 and 9 were calculated in comparison with the baseline scores (visit 1). Dunnett’s method was used to adjust p-values for multiple comparisons. Statistical analyses were performed using Python 3.9.17 (Python Software Foundation, Wilmington, Delaware, United States), with a significance level of 5% using two-sided tests.
Results
Study Participants
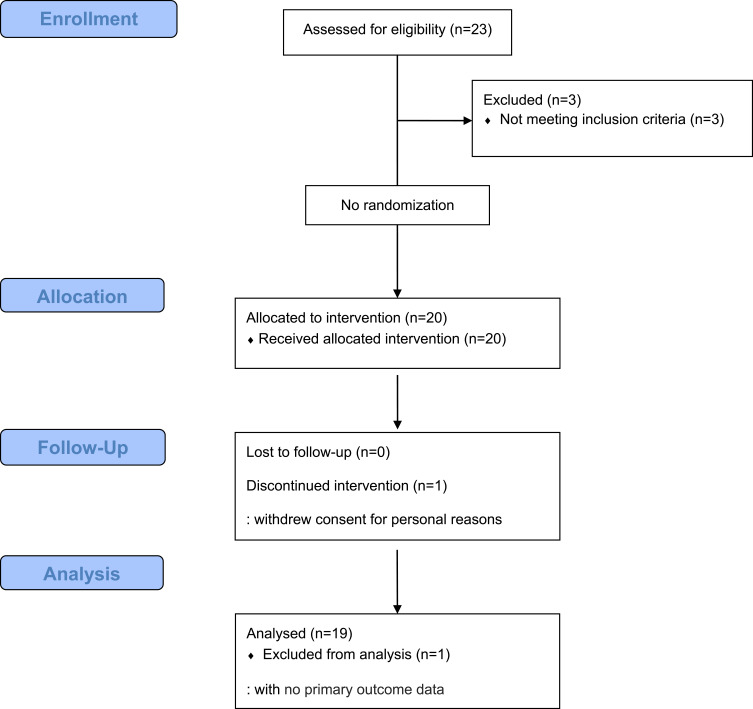
Between October 26, 2022, and April 12, 2023, 23 postmenopausal women with OAB were screened, and 20 participants were ultimately enrolled (recruitment rate, 86.96%). One participant withdrew consent and dropped out of the study. The adherence and completion rates were both 95%. Nineteen participants were included in the ITT analysis (Figure 2).
Figure 2.
Flow chart of the enrollment of study participants.
Baseline patient characteristics are summarised in Table 1. The mean age was 58.26 ± 4.78 years, and body weight was 58.83 ± 4.21 kg. The average duration of OAB symptoms was 107.74 ± 112.44 months, and 8 participants had received previous treatment of OAB (Table 1).
Table 1.
Baseline Participant Characteristics
| Characteristics | Values (mean ± SD) | |
|---|---|---|
| Height (cm), mean (SD) | 159.92 ± 6.21 | |
| Weight (kg) | 58.83 ± 4.21 | |
| Age (years) | 58.26 ± 4.78 | |
| Menopause age (years) | 51.26 ± 4.08 | |
| Full-term delivery, n | 2.05 ± 0.40 | |
| Spontaneous delivery, n | 1.21 ± 1.08 | |
| Caesarean section, n | 0.84 ± 0.96 | |
| Duration of OAB symptoms (months) | 107.74 ± 112.44 | |
| Experience of treating OAB symptoms, n (%) | Yes | 8 (42.11) |
| No | 11 (57.89) | |
| Experience of HRT, n (%) | Yes | 1 (5.26) |
| No | 18 (94.74) | |
| Smoking, n (%) | Yes | 0 (0) |
| No | 19 (100) | |
| Alcohol consumption, n (%) | Yes | 4 (21.05) |
| No | 15 (78.95) | |
Abbreviations: OAB, overactive bladder; HRT, hormone replacement treatment; SD, standard deviation.
Primary Outcome
Table 2 shows a comparison of the average number of micturitions per 24 hours at baseline (visit 1), the end of treatment (visit 8), and 1-month after treatment (visit 9). At baseline, the average 24-hour urination numbers were 10.71 ± 2.47; At the end of the treatment, this decreased to 8.16 ± 1.99; and at the 4-week follow-up, it was 8.02 ± 2.1. The differences between visits 0, 8, and 9 were statistically significant (p=0.001 and p=0.001, respectively; Table 2).
Table 2.
Changes in Outcome Measurements Over Time
| Baseline | Visit 8 (week 8) | Visit 9 (week 12) | ||
|---|---|---|---|---|
| 24-hour micturition | Mean ± SD | 10.71 ± 2.47 | 8.16 ± 1.99 | 8.02 ± 2.1 |
| Difference (95% CI) | −2.55 (−3.27, −1.83) |
−2.69 (−3.41, −1.97) |
||
| p value | 0.001 | 0.001 | ||
| Daytime micturition | Mean ± SD | 8.58 ± 2.24 | 7.02 ± 1.74 | 6.68 ± 1.86 |
| Difference (95% CI) | −1.57 (−2.33, −0.81) |
−1.90 (−2.66, −1.14) |
||
| p value | 0.032 | 0.008 | ||
| Nocturnal micturition | Mean ± SD | 2.13 ± 0.77 | 1.14 ± 0.76 | 1.23 ± 0.82 |
| Difference (95% CI) | −0.99 (−1.30, −0.68) |
−0.90 (−1.21, −0.59) |
||
| p value | 0.001 | 0.002 | ||
| Urinary urgency | Mean ± SD | 19.26 ± 9.87 | 15.68 ± 6.84 | 14.32 ± 8.16 |
| Difference (95% CI) | −3.58 (−7.34, 0.18) |
−4.95 (−8.70, −1.19) |
||
| p value | 0.323 | 0.132 | ||
| Urge urinary incontinence | Mean ± SD | 0.53 ± 0.90 | 0.84 ± 2.12 | 0.16 ± 0.50 |
| Difference (95% CI) | 0.32 (−0.55, −1.18) |
−0.37 (−1.23, 0.50) |
||
| p value | 0.697 | 0.616 | ||
| OABSS | Mean ± SD | 6.74 ± 2.49 | 4.21 ± 2.32 | 4.37 ± 2.19 |
| Difference (95% CI) | −2.53 (−3.42, −1.63) |
−2.37 (−3.26, −1.47) |
||
| p value | 0.003 | 0.006 | ||
| KHQ | Mean ± SD | 409.76 ± 163.01 | 355.26 ± 160.52 | 264.60 ± 143.71 |
| Difference (95% CI) | −54.50 (−108.54, −0.46) |
−145.16 (−199.20, −91.12) |
||
| p value | 0.458 | 0.011 |
Notes: Least-square means and mean differences were calculated using a linear mixed model of repeated measures. Pairwise comparisons were adjusted using Dunnett’s method.
Abbreviations: OABSS, overactive bladder symptom score; KHQ, King’s Health Questionnaire; CI, confidence interval; SD, standard deviation.
Secondary Outcomes
Daytime and Nighttime Micturition per 24 hours
Daytime micturition per 24 hours was defined as the number of urination sessions after waking up in the morning and before bedtime. Daytime voiding frequency showed a reduction from 8.58±2.24 before treatment to 7.02±1.74 post-treatment and 6.68±1.86 at visit 9 (p=0.032, p=0.008, respectively). Significant differences were found before and after treatment and at 1 month after treatment.
Nocturnal micturition per 24 hours was defined as the number of times a patient woke up for urination from bed at night and before waking up on the following day. Nighttime voiding frequency also decreased from 2.13 ± 0.77 before treatment to 1.14 ± 0.76 post-treatment and 1.23 ± 0.82 at visit 9 (p=0.001, p=0.002, respectively). Differences were considered statistically significant.
OABSS Score
At baseline, the OABSS was approximately 7, indicating severe OAB symptoms. The OABSS score decreased to approximately 4 post-treatment, indicating mild symptom severity. At visit 9, a month after treatment, the OABSS score was sustained to approximately 4. These differences were statistically significant (p=0.003, p=0.006, respectively).
Total Number of Urinary Urgencies
At baseline, the number of urgencies was 19.26 ± 9.87. After treatment, the number of urgencies decreased to 15.68 ± 6.84 in visit 8 and 14.32 ± 8.16 in visit 9, and these differences were not statistically significant (p=0.323, p=0.132, respectively).
In this study, UUI was defined as “a situation in which urine leaks after a sudden and intense urge to urinate”. As shown in Table 2, the baseline UUI was 0.53 ± 0.90, ie, below 1 time. After treatment, the numbers of UUI were 0.84 ± 2.12 at visit 8 and 0.16 ± 0.50 at visit 9. There were no significant differences between the groups (p=0.697, p=0.616, respectively).
KHQ Score
Table 2 lists the differences in scores over time from baseline to visit 9. At baseline, the mean KHQ scores were 409.76 ± 163.01, which decreased to 355.26 ± 160.52 at visit 8 (p=0.458) and to 264 ± 143.71 at visit 9 (p=0.011).
Safety
Adverse Events
No AEs occurred during the treatment; however, two AEs were reported in one patient which included lower back pain (one case: moderate severity) and knee pain (one case: mild severity). Given the causal relationship with treatment, the lower back pain and knee pain were likely related.
Laboratory Test Results and Vital Signs
Urinalysis was performed at baseline and week 8 to measure changes before and after treatment. After determining whether the test results were normal or abnormal for all items, no notable differences were observed before and after the clinical trial. Vital signs of the participants were measured during the trial and were all within the normal ranges, with no significant differences in any of the parameters during the study.
Discussion
This preliminary study showed that TEA for menopausal women with OAB improved the frequency of micturition, without any serious AEs, although having no statistically significant effect on episodes of urgency or incontinence. However, there were significant differences in micturition at the 4-week follow-up assessment. It is meaningful that micturition, the main symptom of concern for participants, improved after treatment, and the improvement was sustained until 1 month after treatment. The frequency of urination decreased from an abnormal range of 11 to a normal range of 8. As reducing the frequency of micturition is a crucial evaluation metric for OAB, a mean reduction of 2.55 in frequency had a clinically significant benefit in postmenopausal women with OAB.
Additionally, the OABSS decreased significantly from 7 points (moderate) to 4 points (mild). Further, the quality of life measured using the KHQ questionnaire improved after 4 weeks of follow-up. These results suggest long-lasting effects of TEA.
The strength of the present study is that major OAB symptoms were assessed using various scales, so that we could quantify the impact and discomfort of OAB symptoms in detail. Additionally, by conducting an additional follow-up 1 month later, we were able to confirm not only the therapeutic effect and safety of TEA but also its sustained effectiveness. The effect of treatment on OAB symptoms, such as micturition frequency, remained significant until 1 month after the end of treatment. In particular, a reduction in the number of nocturia episodes in older women was clinically significant. Considering the impact of nocturia on sleep quality and health-related quality of life, a significant reduction in nocturia likely affects overall health.25,26 Nocturia is associated with an approximate 1.2-fold increased risk of falls and a 1.3-fold increased risk of fractures.27 Considering osteoporosis is the most prevalent disease in menopausal women,28 the reduction in the frequency of nocturia is importantly associated with preventing accidents.
This study has some limitations that should be considered. First, this was a single-arm pilot study with a small sample size of 20 participants to obtain information such as recruitment rates, determine the appropriateness of the inclusion and exclusion criteria, and assess the feasibility and preliminary effects of TEA on OAB. While this sample size is appropriate for a pilot study, it may not provide sufficient power to detect smaller but clinically significant differences. The findings will serve as a foundation for calculating sample size and refining methodologies for future randomized controlled trials with larger populations. Second, OAB is a chronic condition that may require longer follow-up to assess the sustained benefits and potential delayed adverse effects of TEA. Previous reviews29,30 suggest that TEA is a relatively safe and convenient therapy, especially with the application of new absorbable surgical sutures. Nevertheless, it would be beneficial to verify its effectiveness over a long-term period. Additionally, because the relationship between the AEs and intervention could not be ruled out, safety needs to be confirmed through additional assessments. Third, the study outcomes relied on self-reported measures, such as bladder diaries and questionnaires. While these tools are widely used in OAB research, they are inherently subject to potential biases, including recall bias and social desirability bias. Although efforts were made to minimize these biases by providing clear instructions and ensuring anonymity, their potential impact on the accuracy of the results cannot be entirely excluded. Fourth, the study’s inclusion criteria focused on postmenopausal women, which limits the generalizability of the results to broader OAB populations. In particular, the findings may not fully apply to individuals with comorbid conditions, different hormonal statuses, or varying demographic and socioeconomic backgrounds. Finally, acupuncture selection was not performed considering individual symptoms and pathologies. Indeed, OAB is a non-specific symptom complex with an unclear pathophysiology, likely including several subtypes of OAB.3 In this study, acupoints that have frequently been used for OAB in previous studies were utilised. However, as numerous factors have been suggested for OAB, it is believed that acupuncture treatment using customised acupoint combinations depending on individual phenotypes may be effective. Future research is needed to identify the precise mechanism of acupuncture treatment by selecting acupoints according to OAB type.
Conclusion
In conclusion, this preliminary study showed that TEA for postmenopausal women with OAB significantly improved the frequency of micturition but had no statistically significant effects on episodes of urgency or incontinence. Our findings suggest that TEA may be an effective and practical strategy for the long-term management of OAB.
Abbreviations
AEs, adverse events; ITT, intention-to-treat; KHQ, King’s Health Questionnaire; OABSS, overactive bladder symptom score; TEA, thread-embedding acupuncture; URS, urgency rating scale; UUI, urgency urinary incontinence.
Acknowledgments
We are grateful to all included women for their participation in the study. The abstract of this paper was presented at the SAR/RCMI PolyU International Research Conference as a poster presentation with interim findings. The poster’s abstract was published in ‘Poster Abstracts’ in Journal of Integrative Medicine: https://doi.org/10.1016/S2095-4964(24)00328-5.
Funding Statement
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: RS-2002-KH127717). The funding source had no involvement in the design, conduct, analysis, or interpretation of the data nor in the writing of the manuscript and the decision to publish the results.
Data Sharing Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Institutional Review Board of Dongguk University Ilsan Oriental Hospital (DUIOH 2022-07-003-004). All participants provided written informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Sadri H, Oliaei A, Sadri S, Pezeshki P, Chughtai B, Elterman D. Systematic review and meta‐analysis of urinary incontinence prevalence and population estimates. Neurourol Urodyn. 2024;43(1):52–62. doi: 10.1002/nau.25276 [DOI] [PubMed] [Google Scholar]
- 2.Haylen BT, De Ridder D, Freeman RM, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. doi: 10.1002/nau.20798 [DOI] [PubMed] [Google Scholar]
- 3.Peyronnet B, Mironska E, Chapple C, et al. A comprehensive review of overactive bladder pathophysiology: on the way to tailored treatment. Eur Urol. 2019;75(6):988–1000. doi: 10.1016/j.eururo.2019.02.038 [DOI] [PubMed] [Google Scholar]
- 4.Durden E, Walker D, Gray S, Fowler R, Juneau P, Gooch K. The economic burden of overactive bladder (OAB) and its effects on the costs associated with other chronic, age‐related comorbidities in the United States. Neurourol Urodyn. 2018;37(5):1641–1649. doi: 10.1002/nau.23513 [DOI] [PubMed] [Google Scholar]
- 5.Hargreaves E, Baker K, Barry G, et al. Acupuncture for treating overactive bladder in adults. Cochrane Database Syst Rev. 2022;9(9). doi: 10.1002/14651858.CD013519.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fontaine C, Papworth E, Pascoe J, Hashim H. Update on the management of overactive bladder. Ther Adv Urol. 2021;13:17562872211039034. doi: 10.1177/17562872211039034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vouri SM, Kebodeaux CD, Stranges PM, Teshome BF. Adverse events and treatment discontinuations of antimuscarinics for the treatment of overactive bladder in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2017;69:77–96. doi: 10.1016/j.archger.2016.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson CB, McKiernan JM. Surgical complications of urinary diversion. Urol Clin North Am. 2018;45(1):79–90. doi: 10.1016/j.ucl.2017.09.008 [DOI] [PubMed] [Google Scholar]
- 9.Zhao Y, Zhou J, Mo Q, Wang Y, Yu J, Liu Z. Acupuncture for adults with overactive bladder: a systematic review and meta-analysis of randomized controlled trials. Medicine. 2018;97(8). doi: 10.1097/MD.0000000000009838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mak TC, Chen HY, Cho WC. Acupuncture for overactive bladder in adults: a systematic review and meta-analysis. Acupunct Med. 2019;37(6):321–331. doi: 10.1136/acupmed-2017-011528 [DOI] [PubMed] [Google Scholar]
- 11.Lee -J-J, Heo J-W, Choi T-Y, Jun JH, Lee MS, Kim J-I. Acupuncture for the treatment of overactive bladder: a systematic review and meta-analysis. Front Neurol. 2023;13:985288. doi: 10.3389/fneur.2022.985288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin Z-X, Chan NHT, Kwan Y-K, et al. A randomized controlled trial to assess the effectiveness and safety of acupuncture for overactive bladder: a study in Hong Kong population. Chin Med. 2020;15(1):108. doi: 10.1186/s13020-020-00388-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee K-H, Lee D-H, Kwon K-R, Park H-S, Park -Y-Y. A literary study on embedding therapy. J Korean Pharmacopuncture Inst. 2003;6(3):15–21. doi: 10.3831/KPI.2003.6.3.015 [DOI] [Google Scholar]
- 14.Gunatillake PA, Adhikari R, Gadegaard N. Biodegradable synthetic polymers for tissue engineering. Eur Cell Mater. 2003;5(1):1–16. doi: 10.22203/ecm.v005a01 [DOI] [PubMed] [Google Scholar]
- 15.Chen Y-B, Chen R-N, Li Y-L. Observation on therapeutic effect of type II early diabetic nephropathies intervened by acupoint thread embedding. Zhongguo Zhen Jiu. 2012;32(5):390–394. PMID: 22650119. [PubMed] [Google Scholar]
- 16.Kim Y-J, Kim M-C, Lee C-H, Kim J-U, Yook T-H. The effect of needle-embedding therapy and pharmacopuncture therapy on patients with urinary incontinence. J Acupunct Meridian Stud. 2011;4(4):220–224. doi: 10.1016/j.jams.2011.10.012 [DOI] [PubMed] [Google Scholar]
- 17.Jeong SJ, Homma Y, Oh S-J. Korean version of the overactive bladder symptom score questionnaire: translation and linguistic validation. Int Neurourol J, Korean Version. 2011;15(3):135. doi: 10.5213/inj.2011.15.3.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nam E-Y, Jung S-H, Bae I-S, Choi S-J, Kim D-I. Efficacy and safety of electroacupuncture and acupuncture in postmenopausal women with overactive bladder; a pilot study of randomized clinical controlled trial. J Korean Obstet Gynecol. 2018;31(1):84–98. doi: 10.15204/JKOBGY.2018.31.1.084 [DOI] [Google Scholar]
- 19.Guo T, Ren Y, Kou J, Shi J, Tianxiao S, Liang F. Acupoint catgut embedding for obesity: systematic review and meta-analysis. Evid Based Complement Altern Med. 2015;2015:401914. doi: 10.1155/2015/401914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho S-I, Kim D-I, Choi S-J. A review of acupuncture treatment methods for urinary incontinence and overactive bladder in postmenopausal women. J Korean Obstet Gynecol. 2022;35(4):121–142. doi: 10.15204/JKOBGY.2022.35.4.121 [DOI] [Google Scholar]
- 21.Oh SJ, Choo MS, Kim HS, et al. Psychometric properties of the Korean version of the king’s health questionnaire in women with stress urinary incontinence. J Korean Continence Soc. 2005;9(2):115–123. doi: 10.5213/jkcs.2005.9.2.115 [DOI] [Google Scholar]
- 22.Homma Y, Yoshida M, Seki N, et al. Symptom assessment tool for overactive bladder syndrome—overactive bladder symptom score. Urology. 2006;68(2):318–323. doi: 10.1016/j.urology.2006.02.042 [DOI] [PubMed] [Google Scholar]
- 23.Kelleher C, Cardozo L, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. BJOG. 1997;104(12):1374–1379. doi: 10.1111/j.1471-0528.1997.tb11006.x [DOI] [PubMed] [Google Scholar]
- 24.Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–191. doi: 10.1002/nur.20247 [DOI] [PubMed] [Google Scholar]
- 25.Bliwise DL, Rosen RC, Baum N. Impact of nocturia on sleep and quality of life: a brief, selected review for the International Consultation on Incontinence Research Society (ICI-RS) nocturia think tank. Neurourol Urodyn. 2014;33(Suppl 1):S15–S18. doi: 10.1002/nau.22585 [DOI] [PubMed] [Google Scholar]
- 26.Choi EPH, Wan EYF, Kwok JYY, Chin WY, Lam CLK. The mediating role of sleep quality in the association between nocturia and health-related quality of life. Health Qual Life Outcomes. 2019;17(1):181. doi: 10.1186/s12955-019-1251-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pesonen JS, Vernooij RWM, Cartwright R, et al. The impact of nocturia on falls and fractures: a systematic review and meta-analysis. J Urol. 2020;203(4):674–683. doi: 10.1097/ju.0000000000000459 [DOI] [PubMed] [Google Scholar]
- 28.Ji M-X, Yu Q. Primary osteoporosis in postmenopausal women. Chronic Dis Transl Med. 2015;1(1):9–13. doi: 10.1016/j.cdtm.2015.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang J-J, Liang J-Q, Xu X-K, Xu Y-X, Chen G-Z. Safety of thread embedding acupuncture therapy: a systematic review. Chin J Integr Med. 2021;27(12):947–955. doi: 10.1007/s11655-021-3443-1 [DOI] [PubMed] [Google Scholar]
- 30.Martins JA, Lach AA, Morris HL, Carr AJ, Mouthuy P-A. Polydioxanone implants: a systematic review on safety and performance in patients. J Biomater Appl. 2020;34(7):902–916. doi: 10.1177/0885328219888841 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.