Abstract
Introduction: The COVID-19 pandemic has triggered several challenges on the front of mental health. Undergraduate medical students face considerable stress in their academic routines. Thus, there is a need to explore the implications for the mental health of undergraduate medical students during the COVID-19 pandemic. Objective: To review the global literature about anxiety and depressive disorders in undergraduate medical students during the COVID-19 pandemic. Method: We developed an integrative literature review on the occurrence of anxiety and depressive symptoms in undergraduate medical students during the COVID-19 pandemic. We included the manuscripts that used the PHQ-9 and/or GAD-7 questionnaires. We excluded systematic reviews, narrative reviews, integrative reviews, meta-analyses, and qualitative analytical studies. We assessed the results on the occurrence of anxiety and depression and the severity of symptoms in medical students during the COVID-19 pandemic using quantitative studies applying the GAD-7 questionnaire for anxiety or the PHQ-9 for depression. Results: We reviewed 85 selected studies, and the results showed a significant prevalence of moderate and severe symptoms of anxiety and depression, with 28.2% of participants presenting scores of ≥10 on the GAD-7 and 38.9% on the PHQ-9. Statistical analyses using simple and multiple regression tests revealed associations between higher rates of anxiety symptoms among students from developing countries and data collected after the lockdown period in 2020 during the pandemic lockdown. In addition, female students were at risk of depressive disorders. We emphasize as a limitation that the diagnosis of depression and anxiety requires a detailed clinical evaluation, which is not focused on in this actual study. Conclusions: Our findings highlight the need for specific interventions to support the mental health of undergraduate medical students, especially female students from developing countries, during a pandemic crisis.
Keywords: anxiety, depression, medical students, pandemic, COVID-19, GAD-7, PHQ-9, mental health
1. Introduction
In December 2019, the first case of a new respiratory disease caused by the SARS-CoV-2 virus was documented [1]. On 11 March 2020, the World Health Organization (WHO)’s executive director officially categorized COVID-19 as a pandemic [2]. In May 2023, the WHO declared an end to the public health emergency of international concern regarding this disease [3,4]. As a result, in response to the global health crisis, the most widely used approach was social isolation, which resulted in the transition of in-person educational activities to an online format [5].
COVID-19 not only causes physical health problems but can also lead to a series of mental disorders [6]. Fear of death and the impacts on physical health, isolation, social distancing, the loss of family members, financial difficulties, misinformation, rumors, and uncertainty about the future are sources of distress. According to the surveys conducted by the WHO, the COVID-19 pandemic triggered a 25% increase in the prevalence of depression and anxiety worldwide [6]. Thus, the effects of the COVID-19 pandemic provide an opportunity to reflect on the state of mental health and highlight the imminent need to implement fundamental preventive measures for collective well-being [6]. Hence, concerns arise regarding the mental health of undergraduate medical students, who represent a population that already suffers from the daily pressures of academic life, which can compromise mental, social, and physical health [7]. Furthermore, there was a higher prevalence of symptoms of anxiety and depression in medical students related to the COVID-19 pandemic [8]. The mental health of medical students presents a vital need to analyze whether depression and anxiety symptoms represent obstacles to their academic careers [9].
Many studies have evaluated scales such as the GAD-7 and PHQ-9 in medical students during the COVID-19 pandemic. The Generalized Anxiety Disorder (GAD-7) scale is a seven-item diagnostic tool that shows probable cases of generalized anxiety disorder and assesses symptom severity. It has been confirmed in remote health surveys, epidemiological studies, and primary care settings [10]. This questionnaire is reliable and has a criterion validity [11]. However, this scale only provides probable diagnoses, which need to be confirmed through further assessment [11]. The Patient Health Questionnaire-9 (PHQ-9) is a nine-item questionnaire that screens for depression in primary care and other medical settings [12]. It is a quick, effective, simple, and reliable tool for screening and assessing the severity of depressive symptoms [13]. However, this questionnaire does not necessarily match the lived experience of depression [14]. Thus, the PHQ-9 is not considered an instrument to confirm a depression diagnosis [15].
Therefore, a literature review that analyzes the rates and severity of depression and anxiety symptoms in undergraduate medical students during the COVID-19 pandemic is essential. Although the emergency phase of this pandemic has already ended, it is essential to analyze the psychological effects on medical students, aiming to provide data that guide the development of strategies for future interventions in similar crises. We hypothesize that there is an increase in the occurrence and severity of symptoms of anxiety and depression in medical students during the COVID-19 pandemic. Hence, we aimed primarily to review the global literature on anxiety and depression disorders with studies that used the PHQ-9 and GAD-7 questionnaires in undergraduate medical students during the COVID-19 pandemic. Moreover, the specific objectives were to analyze the predictive variables for increased symptoms of anxiety and depression in medical educational institutions.
2. Methods
We performed an integrative literature review from February to July 2024 at the Faculty of Medicine at FEMA (Educational Foundation of the Municipality of Assis). Regarding the eligibility and search criteria, we included medical literature in English, Portuguese, and Spanish, using the following keywords: (COVID-19) and (Medical Students) and (anxiety) or (depression) or (mental health). We searched the indexed journals’ databases, PubMed and Bvsalud, and selected the manuscripts with data collection from December 2019 to July 2024. We included the manuscripts that used the PHQ-9 and/or GAD-7 questionnaires in their methodology. We excluded systematic reviews, narrative reviews, integrative reviews, meta-analyses, and qualitative analytical studies. We also excluded manuscripts from non-indexed and pre-print journals.
We aimed to identify peer-reviewed literature and relevant studies focusing on symptoms of depressive and anxiety disorders in undergraduate medical students during the COVID-19 pandemic. To ensure a comprehensive search, we searched PubMed and BVSalud databases using keywords, subject headings, and boolean operators. Our terms were carefully selected to focus on the target population, mental health disorders, and the context of the COVID-19 pandemic.
We used the following variables: Studies with data collected in 2020, during the lockdown period, and studies conducted after 2020, post-lockdown period; the continents in which the institutions were located, which were Europe, Asia, North America, Latin America, Oceania, and Africa; the actualized Human Development Index (HDI) of the country; the number of study participants, gender, percentile of women, and the average age of the participants; the categorization of the GAD-7 questionnaire, organized into scores of 0–4, 5–9, 10–14, 15–21, and the categorization of the GAD-7 was <10 or ≥10; the categorization of the PHQ-9 questionnaire, organized into scores of 0–4, 5–9, 10–14; 15–19 > 19 and the categorization of the PHQ-9 was <10 or ≥10. The primary outcome was the prevalence of moderate or higher symptoms of anxiety and depression in medical students during the COVID-19 pandemic. The secondary outcome was a search for predictive variables on the severity of symptoms in studies in which the GAD-7 and PHQ-9 scores were ≥10.
We adjusted the multiple linear regression models with a normal response to explain a GAD-7 percentage that was greater than or equal to 10 points and a PHQ-9 percentage greater than or equal to 10 points, including, in the deterministic component, only the variables that presented a p < 0.20 in the bivariate investigation. The GAD-7 and PHQ-9 indexes equal to or greater than ten are critical for denoting moderate- and high-severity symptoms [11,16]. The quality of the adjustment of the multiple regression models was analyzed by investigating the behavior of the residuals with the Shapiro–Wilk normality test, scatter plot between residuals and predicted values of the models to investigate homoscedasticity, and Cook’s distance measure to investigate the influence of atypical points on the estimates of the model parameters. The final models considered the associations statistically significant if p < 0.05. All analyses were performed with the SPSS 21 software by IBM trademark.
We collected studies from the literature using secondary data sources. We were concerned about bias risks in the analysis and the interpretation of research data and indirect risks to the physical, mental, spiritual, and social dimensions associated with human beings in any research. Regarding the benefits, we considered the manuscript vital for promoting a positive impact on medical practice in mental health.
3. Results
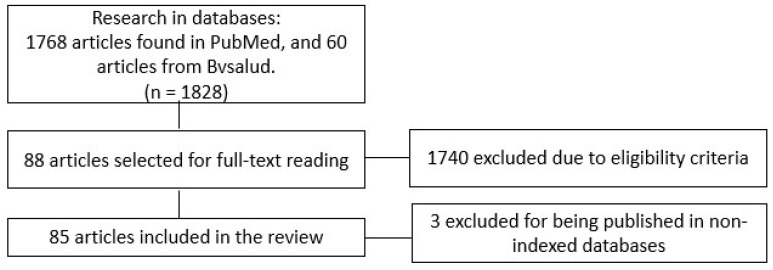
We identified 1768 studies in the PubMed database and 60 articles in Bvsalud. Applying the eligibility criteria, we selected 88 articles from the literature. Of these, 43 contained at least one of the questionnaires (GAD-7 or PHQ-9), while in 42 articles, both questionnaires were used. Figure 1 represents the flowchart of the selection process.
Figure 1.
Flowchart of the selection process of the studies included in the review.
Table 1 contains the list of selected studies. Three manuscripts were excluded because they were published in non-indexed databases. Thus, this study was based on data from 85 manuscripts in the literature.
Table 1.
List of the eligible studies and the percentiles of GAD-7 and/or PHQ-9 scores ≥10.
| Author | Country | N | GAD-7 ≥ 10 (%) | PHQ-9 ≥ 10 (%) | |
|---|---|---|---|---|---|
| 1 | Zheng [17] | China | 468 | 11.30 | 20.70 |
| 2 | Coico-Lama [18] | Peru | 431 | 29.50 | 28.50 |
| 3 | Bhongade [19] | Emirates | 107 | 25.30 | |
| 4 | Din [20] | Pakistan | 444 | 46.17 | 64.41 |
| 5 | Reddy [21] | India | 164 | 20.00 | |
| 6 | Ortega-Moreno [22] | Mexico | 384 | 24.50 | 43.00 |
| 7 | Shahzad [23] | Pakistan | 585 | 41.00 | |
| 8 | Iqbal [24] | India | 261 | 51.70 | 58.70 |
| 9 | Gomez-Duran [25] | Spain | 175 | 34.70 | 26.60 |
| 10 | Wiguna [26] | Indonesia | 1023 | 77.40 | |
| 11 | Tanuseriawan [27] | Indonesia | 635 | 63.40 | |
| 12 | Purnomo [28] | Indonesia | 161 | 8.70 | |
| 13 | Yuryeva [29] | Ukraine | 154 | 27.90 | 44.80 |
| 14 | Arshad I [30] | India | 261 | 65.50 | 67.80 |
| 15 | Lakshmi [31] | India | 200 | 83.00 | |
| 16 | Ernst J [32] | Swiss | 574 | 22.60 | |
| 17 | Cao W [33] | China | 7143 | 3.60 | 27.20 |
| 18 | Chistophers B [34] | USA | 1139 | 20.00 | |
| 19 | Sartorao [8,35] | Brazil | 340 | a | a |
| 20 | Lin S [36] | USA | 154 | 24.00 | |
| 21 | Huarccaya Victoria [37] | Colombia | 1238 | 34.00 | |
| 22 | Pinsai [38] | Tailandia | 37 | 51.35 | |
| 23 | Verma [39] | India | 267 | 28.50 | |
| 24 | Alkwai [40] | Saudi Arabia | 55 | 17.00 | 26.42 |
| 25 | Bartra [41] | Peru | 57 | 22.80 | |
| 26 | Guralwar [42] | India | 604 | 54.14 | |
| 27 | Almarri [43] | Saudi Arabia | 7116 | 40.50 | |
| 28 | Kamran [44] | Pakistan | 324 | 44.50 | |
| 29 | Porwal [45] | Saudi Arabia | 22 | 13.60 | 40.90 |
| 30 | Primatanti [46] | Indonesia | 7949 | 13.90 | |
| 31 | AbuDujain [47] | Saudi Arabia | 345 | 13.90 | |
| 32 | Imran [48] | Pakistan | 1100 | 40.40 | 48.10 |
| 33 | Rafsanjanipoor [49] | Iran | 83 | 24.20 | |
| 34 | Srivastava [50] | India | 97 | 24.74 | 48.10 |
| 35 | Pedraz-Petrozzi [51] | Colombia | 125 | 12.80 | 34.40 |
| 36 | Vajpeyi [52] | Emirates | 798 | 39.10 | |
| 37 | Alshehri [53] | Saudi Arabia | 182 | 30.80 | |
| 38 | Paz D [54] | USA | 152 | 36.70 | 40.90 |
| 39 | Schindler [55] | Germany | 63 | 44.00 | |
| 40 | Lu [56] | China | 519 | 41.50 | |
| 41 | Chakeyanunn [57] | Thailand | 437 | 27.00 | |
| 42 | Huarcaya victoria [37] | Colombia | 1238 | 19.00 | |
| 43 | Camelier-Mascarenhas [58] | Brazil | 310 | 33.50 | 42.60 |
| 44 | Dziedzic [59] | Brazil | 162 | 29.60 | 34.00 |
| 45 | Eleftheriou [60] | Greece | 559 | 67.60 | 43.70 |
| 46 | Cheng [61] | China | 947 | 37.80 | 39.30 |
| 47 | Santander [62] | Peru | 370 | 38.38 | |
| 48 | Çimen [63] | Turkey | 2778 | 44.50 | 46.21 |
| 49 | VIillalon López [64] | Chile | 359 | 41.50 | 60.10 |
| 50 | Villagomes-Lopez [65] | Ecuador | 1528 | 30.30 | |
| 51 | Harries [66] | USA | 741 | 25.60 | |
| 52 | Liu [67] | China | 29,663 | 46.00 | 37.80 |
| 53 | Pattanaseri [68] | Thailand | 224 | a | a |
| 54 | Teh [69] | Malaysia | 371 | 37.00 | 35.70 |
| 55 | Adhikari [70] | Nepal | 223 | a | a |
| 56 | Chalise [71] | Nepal | 315 | 12.90 | |
| 57 | Romic [72] | Croatia | 280 | 32.50 | 52.20 |
| 58 | Nguyen [73] | Vietnan | 747 | 7.90 | 20.63 |
| 59 | Biswas [74] | Bangladesh | 425 | 31.80 | |
| 60 | Song [75] | China | 666 | 17.80 | 15.20 |
| 61 | Guo [76] | USA | 929 | 31.10 | 48.80 |
| 62 | Essangri [77] | Morocco | 549 | 25.70 | 45.70 |
| 63 | Saali [78] | USA | 108 | 32.40 | |
| 64 | Nishimura [79] | Japan | 473 | 7.20 | 74.70 |
| 65 | Sserunkuuma [80] | Uganda | 269 | 24.10 | |
| 66 | Batais [81] | Saudi Arabia | 332 | 13.70 | 15.90 |
| 67 | Crisol-deza [82] | Peru | 1238 | 19.00 | 34.00 |
| 68 | Tsiouris [83] | Germany | 1438 | 34.00 | |
| 69 | Sudi [84] | Malaysia | 196 | 38.90 | |
| 70 | Wercelens [85] | Brazil | 150 | 40.70 | |
| 71 | Yin [86] | China | 5982 | 4.20 | 9.90 |
| 72 | Chwa [87] | USA | 87 | 27.40 | |
| 73 | Pandey [88] | India | 83 | 9.80 | 24.70 |
| 74 | Elhadi [89] | Libya | 2430 | 27.00 | |
| 75 | Xiao [90] | China | 933 | 4.60 | 7.30 |
| 76 | Essadek [91] | France | 668 | 42.80 | |
| 77 | Liu [92] | China | 217 | 7.40 | |
| 78 | Chootong [93] | Thailand | 325 | 12.90 | 7.60 |
| 79 | Saeed [94] | Pakistan | 234 | 62.40 | 64.10 |
| 80 | Huang [95] | China | 1021 | 10.98 | 38.17 |
| 81 | Wang [96] | Korea | 454 | 18.50 | 11.10 |
| 82 | Halperin [97] | USA | 1428 | 30.60 | 31.00 |
| 83 | Bilgi [98] | Turkey | 178 | 37.10 | 20.10 |
| 84 | Alsairafi [99] | Kuwait | 298 | 85.20 | 93.00 |
| 85 | Allah [100] | Saudi Arabia | 1591 | 19.20 | |
| 86 | Khidri [101] | Pakistan | 864 | 40.80 | |
| 87 | Shreevastava [102] | India | 1208 | 40.30 | |
| 88 | Afzal [103] | Pakistan | 433 | 40.65 |
a The manuscripts referenced as 19, 53, and 55 were excluded due to non-indexed publication.
Table 2 shows the manuscripts’ sample characteristics. Of the selected manuscripts, 28 collected information after 2020. Regarding the institution continent area, 49 papers were from Asian institutions. For the HDI (Human Development Index), 35 were from countries with a very high HDI, 31 were from countries with a high HDI, and 22 were from countries with a medium or low HDI.
Table 2.
Manuscripts’ description variables.
| Variable | N | % |
|---|---|---|
| Data collection time | ||
| After 2020 | 28 | 31.8 |
| In 2020 | 60 | 68.2 |
| Continent | ||
| Europe | 9 | 10.2 |
| North America | 8 | 9.1 |
| Asia | 49 | 55.7 |
| Oceania | 5 | 5.7 |
| Latin America | 14 | 15.9 |
| Africa | 3 | 3.4 |
| Human Development Index (HDI) | ||
| Very high | 35 | 39.8 |
| High | 31 | 35.2 |
| Medium or low | 22 | 25.0 |
Table 3 provides the variable range list and the interquartis. Concerning the HDI variable, the median of the countries was 0.79 (0.70–0.88). The median age of the participants was 22.0 years (20.0–23.0). The percentile of women who answered the questionnaires was 63.0% (52.3–68.7). Regarding the GAD-7 questionnaire, we observed a median of 28.2% (18.3–39.4) with a score of ≥10. Regarding the PHQ-9 questionnaire, the median score of ≥10 was 38.9% (26.8–47.2).
Table 3.
Variable range list and the interquartile ranges.
| Variable | Median | Q1 | Q3 |
|---|---|---|---|
| Human Development Index | 0.79 | 0.70 | 0.88 |
| Number of participants | 377.5 | 185.5 | 912.8 |
| Male | 160.0 | 89.0 | 322.0 |
| Female | 240.0 | 113.0 | 597.0 |
| Percentual of women | 63.0 | 52.3 | 68.7 |
| Age | 22.0 | 20.0 | 23.0 |
| GAD-7 score 0–4 | 25.3 | 0.0 | 39.2 |
| GAD-7 score 5–9 | 37.8 | 30.4 | 67.2 |
| GAD-7 score 10–14 | 19.9 | 12.8 | 27.5 |
| GAD-7 score 15–21 | 3.4 | 0.0 | 13.9 |
| GAD-7 score ≥ 10 | 28.2 | 18.3 | 39.4 |
| PHQ-9 score 0–4 | 0.0 | 0.0 | 28.4 |
| PHQ-9 score < 10 | 40.0 | 27.0 | 60.9 |
| PHQ-9 score 10–14 | 23.0 | 19.0 | 36.8 |
| PHQ-9 score 15–19 | 4.9 | 0.0 | 13.9 |
| PHQ-9 score > 19 | 0.0 | 0.0 | 6.2 |
| PHQ-9 score ≥ 10 | 38.9 | 26.8 | 47.2 |
Q1: first interquartile range. Q3: third interquartile range.
Table 4 presents the bivariate associations by simple linear regression to explain the percentage of GAD-7 with a score of ≥10 points (p < 0.20). We observed significant results (p < 0.20) regarding the following variables: data collected in 2020, Latin America, Oceania, and Asia (reference: Europe), with a low, medium, or high HDI (reference: very high HDI).
Table 4.
Bivariate associations by simple linear regression to explain the percentage of GAD-7 scores ≥10.
| Variable | β | 95%CI | p | |
|---|---|---|---|---|
| Data Collection in 2020 (Ref: After 2020) | −15.16 | −23.15 | −7.17 | 0.000 |
| Africa | −13.48 | −40.54 | 13.58 | 0.329 |
| Latin America | −13.22 | −29.79 | 3.35 | 0.118 |
| Oceania | −25.93 | −61.73 | 9.87 | 0.156 |
| Asia | −9.51 | −23.98 | 4.95 | 0.198 |
| North America | −10.72 | −29.16 | 7.72 | 0.255 |
| Continent (ref: Europe) | 0 | |||
| Human Development Index | −34.12 | −68.59 | 0.35 | 0.052 |
| Medium or low | 9.23 | −0.12 | 18.59 | 0.053 |
| High | −10.72 | −19.10 | −2.35 | 0.012 |
| Human Development Index (ref: very high) | 0 | |||
| Number of participants | 0.00 | 0.00 | 0.00 | 0.914 |
| Number of women | 0.00 | 0.00 | 0.00 | 0.963 |
| Percentage of women | 0.08 | −0.30 | 0.46 | 0.684 |
| Average age | 0.67 | −3.82 | 5.15 | 0.771 |
β: beta coefficient; 95%CI: 95% confidence interval; p < 0.20.
Table 5 shows the data obtained after multiple linear regression to explain the percentage of GAD-7 scores that were ≥10 (p < 0.05). After statistical analysis, we observed that studies with data collected in 2020—during the lockdown in most countries worldwide—had a GAD-7 response percentage of ≥10, which was, on average, 14% lower compared to the data collected after 2020 (β: −14.02; 95% CI −21.63 to −6.40; p < 0.001). Countries with a medium or low HDI had a GAD-7 response percentage of ≥10, twelve percent higher than countries with a high or very high HDI (β: 12.61; 95%CI 2.93 to 22.29; p < 0.011).
Table 5.
Multiple linear regression to explain the percentage of GAD-7 scores ≥10.
| Variable | β | 95%CI | p | |
|---|---|---|---|---|
| Data collection in 2020 (ref: after 2020) | −14.02 | −21.63 | −6.40 | 0.000 |
| Africa | −6.26 | −30.28 | 17.76 | 0.610 |
| Latin America | 2.63 | −13.92 | 19.18 | 0.755 |
| Oceania | −22.24 | −53.37 | 8.90 | 0.162 |
| Asia | −7.25 | −20.49 | 5.99 | 0.283 |
| North America | −5.38 | −20.71 | 9.96 | 0.492 |
| Continent (ref: Europe) | 0 | |||
| Medium or low | 12.61 | 2.93 | 22.29 | 0.011 |
| High | −8.37 | −18.37 | 1.63 | 0.101 |
| Human Development Index (ref: very high) | 0 | |||
p < 0.05; homoscedasticity; dCook < 1 = 100%; β: beta coefficient; 95%CI: 95% confidence interval.
Regarding the studies using the PHQ-9, Table 6 shows the bivariate associations by simple linear regression to explain the percentage of PHQ-9 scores ≥10. As a result, the percentage of women was the only association presenting a p-value under 0.20 on the bivariate analysis (β: 0.36; 95%CI: −0.04 to 0.75; p < 0.077). For the PHQ-9 analysis, the multiple linear regression was not carried out because the analysis was inappropriate due to only one significant variable detected by the bivariate analysis. Thus, the multivariate analysis would require multiple predictors to provide value.
Table 6.
Bivariate associations by simple linear regression to explain the percentage of PHQ-9 scores ≥10.
| Variable | β | 95%CI | p | |
|---|---|---|---|---|
| Data Collection in 2020 (Ref: After 2020) | 1.42 | −8.71 | 11.54 | 0.784 |
| Africa | −8.59 | −35.82 | 18.64 | 0.536 |
| Latin America | −4.46 | −21.19 | 12.28 | 0.602 |
| Oceania | 3.61 | −17.48 | 24.70 | 0.737 |
| Asia | −6.21 | −19.92 | 7.49 | 0.374 |
| North America | −7.31 | −28.40 | 13.78 | 0.497 |
| Continent (ref: Europe) | 0 | |||
| Human Development Index | −22.58 | −62.59 | 17.42 | 0.269 |
| Medium or low | 6.67 | −5.34 | 18.68 | 0.276 |
| High | −6.14 | −16.19 | 3.92 | 0.232 |
| Human Development Index (ref: very high) | 0 | |||
| Number of participants | 0.00 | 0.00 | 0.00 | 0.625 |
| Number of women | 0.00 | 0.00 | 0.00 | 0.665 |
| Percentage of women | 0.36 | −0.04 | 0.75 | 0.077 |
| Average age | 4.78 | −5.13 | 14.70 | 0.344 |
β: beta coefficient; 95%CI: 95% confidence interval; p < 0.20.
4. Discussion
We found evidence that studies performed in 2020 during the lockdown period showed students with an average reduction of 14% in their responses to the GAD-7 anxiety symptoms score of ≥10 (moderate and severe symptoms) compared to studies after 2020. The lockdown period and the beginning of the pandemic, as well as a period of uncertainty, may explain this finding [104,105].
Furthermore, we observed that students from developing nations had a significant average increase of 12% in their responses to moderate or severe symptoms of anxiety than those from countries with a high or very high HDI. Moreover, regarding the higher percentage of female students, a significant association was found concerning the PHQ-9 depression symptoms score of ≥10. It is known that females have a predisposition to be more affected by stressors related to the COVID-19 pandemic, such as social isolation, academic disruptions, and health concerns [106,107]. Moreover, it is essential to highlight that developing countries are also associated with a high burden of mental health disorders [108], with some studies suggesting that lower-income countries have a reduced capacity to provide access to depression treatment [109,110].
The COVID-19 pandemic has affected medical students’ mental health. A systematic review found exacerbated feelings of stress, depression, and anxiety among medical students worldwide [111]. Another study reported that 23% of medical students experienced depression, and 11% experienced anxiety during the pandemic [112]. A cross-sectional survey revealed that a staggering 79.6% of medical students experienced heightened anxiety, and 65.1% reported increased depression during the pandemic [54]. Similarly, a Serbian study found that a significant majority of medical students, 64.5%, reported severe depressive symptoms, 66.8% reported severe anxiety, and 66.7% reported severe stress [113].
COVID-19-related mental health issues more significantly affect female medical students, including increased symptoms of depression and anxiety. A study conducted in the United States observed that the female group was significantly more likely to report anxiety risk symptoms among medical students [114].
Another meta-analysis identified that being female, being a junior, being a preclinical student, and having economic troubles were significant risk factors for mental health impairment during the pandemic [115].
In Mexico, factors associated with depression included the female sex, younger age (18–20 years), perceived academic performance, and economic hardship [116].
A meta-analysis published by Jia et al. in 2022 demonstrated the pooled prevalence of depression in 37.9% of medical students (95%CI: 30.7–45.4%) and pooled anxiety prevalence of 33.7% (95%CI: 26.8–41.1%). In addition, their results varied by gender, country, and continent [117].
Another study, in 2024, from Lin et al. [118],reported a pooled prevalence for anxiety of 45% (95%CI: 40–49%) and depression of 48% (95%CI: 43–52%). For moderate and severe anxiety, 28% (95%CI: 24–32%), and for moderate and severe depression, 30% (95%CI: 26–35%). After the meta-regression, medical students in Asia had a lower prevalence of anxiety and depression than those from other regions [118].
Limitations: The review analyzed global data based on observational studies using the questionnaires GAD-7 and PHQ-9, which are recognized as good screening instruments for anxiety and depression symptoms. These questionnaires are widely used in mental health research due to their reliability and validity. We only elected studies using GAD-7 for anxiety and PHQ-9 for depressive disorders because the diversity of tools used across studies can lead to difficulties in comparing and synthesizing results. In addition, the diagnosis of depression and anxiety is not based solely on the application of the questionnaires and requires a detailed clinical evaluation. Other limitations were the heterogeneity of the population, variability in the study design, publication bias, local or context-specific stressors, and cultural and subjective influence on the responses. Moreover, the co-occurrence of depression or anxiety may lead to confounding results in the observational studies. Lastly, dichotomous variables often reduce nuanced information into two categories, which can oversimplify complex relationships in the statistical regression model.
The results cannot be generalized due to the consideration of limitations inherent to observational studies, such as difficulty in controlling variables, potential confounders, temporal ambiguity, and the location where the studies were conducted, in addition to selection and information biases. Overall, our findings underscore the heightened mental health difficulties faced by medical students during the pandemic, highlighting the essential need for targeted support and preventable interventions.
5. Conclusions
A comprehensive review of global literature demonstrated a high occurrence of moderate and severe symptoms of depression and anxiety among the undergraduate medical student population. We observed a higher occurrence of anxiety symptoms among medical students assessed after the lockdown period and from studies assessed in developing countries. We also described a higher occurrence of depressive symptoms in the female population worldwide. These findings highlight the urgency of developing targeted intervention strategies to mitigate these symptoms in populations that demonstrate high susceptibility to mental disorders during pandemic periods.
Author Contributions
The authors contributed equally for the conceptualization, methodology, formal analysis, investigation, resources, data curation, writing and editing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
List of Abbreviations
| PHQ-9 | The Patient Health Questionnaire-9 scale |
| GAD-7 | The Generalized Anxiety Disorder-7 scale |
| HDI | The Human Development Index |
References
- 1.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., Hu Y., Tao Z.W., Tian J.H., Pei Y.Y., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United Nations COVID-19 and the Need for Action on Mental Health. May, 2020. [(accessed on 29 September 2024)]. Available online: https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf.
- 3.Pan American Health Organization OMS Declara Fim da Emergência de Saúde Pública de Importância Internacional Referente à COVID-19. May, 2023. [(accessed on 29 September 2024)]. Available online: https://www.paho.org/pt/noticias/5-5-2023-oms-declara-fim-da-emergencia-saude-publica-importancia-internacional-referente.
- 4.Mehraeen E., Salehi M.A., Behnezhad F., Moghaddam H.R., SeyedAlinaghi S. Transmission Modes of COVID-19: A Systematic Review. Infect. Disord. Drug Targets. 2021;21:27–34. doi: 10.2174/1871526520666201116095934. [DOI] [PubMed] [Google Scholar]
- 5.Leal Filho W., Wall T., Rayman-Bacchus L., Mifsud M., Pritchard D.J., Lovren V.O., Farinha C., Petrovic D.S., Balogun A.-L. Impacts of COVID-19 and social isolation on academic staff and students at universities: A cross-sectional study. BMC Public Health. 2021;21:1213. doi: 10.1186/s12889-021-11040-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed I., Banu H., Al-Fageer R., Al-Suwaidi R. Cognitive emotions: Depression and anxiety in medical students and staff. J. Crit. Care. 2009;24:e1–e7. doi: 10.1016/j.jcrc.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Izaias C., Filho S., Conte De Las W., Rodrigues V., Beauchamp De Castro R., Aparecida Marçal A., Pavelqueires S., Takano L., de Oliveira W.L., Neto C.I.S. Impact of COVID-19 Pandemic on Mental Health of Medical Students: A Cross-Sectional Study Using GAD-7 and PHQ-9 Questionnaires. medRxiv. 2020 doi: 10.1101/2020.06.24.20138925. [DOI] [Google Scholar]
- 9.Mirza A.A., Baig M., Beyari G.M., Halawani M.A., Mirza A.A. Depression and anxiety among medical students: A brief overview. Adv. Med. Educ. Pract. 2021;12:393–398. doi: 10.2147/AMEP.S302897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sapra A., Bhandari P., Sharma S., Chanpura T., Lopp L. Using Generalized Anxiety Disorder-2 (GAD-2) and GAD-7 in a Primary Care Setting. Cureus. 2020;12:e8224. doi: 10.7759/cureus.8224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levis B., Benedetti A., Thombs B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ. 2019;365:l1476. doi: 10.1136/bmj.l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 13.Sun Y., Fu Z., Bo Q., Mao Z., Ma X., Wang C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. 2020;20:474. doi: 10.1186/s12888-020-02885-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malpass A., Dowrick C., Gilbody S., Robinson J., Wiles N., Duffy L., Lewis G. Usefulness of PHQ-9 in primary care to determine meaningful symptoms of low mood: A qualitative study. Br. J. Gen. Pract. 2016;66:78–84. doi: 10.3399/bjgp16X683473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford J., Thomas F., Byng R., McCabe R. Use of the Patient Health Questionnaire (PHQ-9) in Practice: Interactions between patients and physicians. Qual. Health Res. 2020;30:2146–2159. doi: 10.1177/1049732320924625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sousa T.V., Viveiros V., Chai M.V., Vicente F.L., Jesus G., Carnot M.J., Gordo A.C., Ferreira P.L. Reliability and validity of the Portuguese version of the Generalized Anxiety Disorder (GAD-7) scale. Health Qual. Life Outcomes. 2015;13:50. doi: 10.1186/s12955-015-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zheng X., Guo Y., Yang H., Luo L., Ya B., Xu H., Xue Z., Li Q., Shi J., Bi J., et al. A Cross-Sectional Study on Mental Health Problems of Medical and Nonmedical Students in Shandong During the COVID-19 Epidemic Recovery Period. Front. Psychiatry. 2021;12:680202. doi: 10.3389/fpsyt.2021.680202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coico-Lama A.H., Diaz-Chingay L.L., Castro-Diaz S.D., Céspedes-Ramirez S.T., Segura-Chavez L.F., Soriano-Moreno A.N. Asociación entre alteraciones en el sueño y problemas de salud mental en los estudiantes de Medicina durante la pandemia de la COVID-19. Educ. Médica. 2022;23:100744. doi: 10.1016/j.edumed.2022.100744. [DOI] [Google Scholar]
- 19.Bhongade B., Ali A.A., Adam S. Assessment of Factors Associated with Generalized Anxiety Disorder and Psychological Distress amid COVID-19 Pandemic: Cross-Sectional Study on the Students of Ras Al Khaimah Medical and Health Sciences University. Indian J. Pharm. Educ. Res. 2024;58:661–670. doi: 10.5530/ijper.58.2.74. [DOI] [Google Scholar]
- 20.ud Din M., Naveed H.U., Tauseef M., Javed M., Sarfraz S., Waheed J. Anxiety And Depression Among Medical Students During Covid-19 Pandemic In Faisalabad. [(accessed on 29 September 2024)];J. Rawalpindi Med. Coll. 2023 27 Available online: https://www.journalrmc.com/index.php/JRMC/article/view/1791. [Google Scholar]
- 21.Reddy C.R.E., Tekulapally K. Anxiety and Coping Strategies Among Medical Students During COVID-19 Pandemic: A Cross-sectional Study. J. Clin. Diagn. Res. 2022;16:VC05–VC08. doi: 10.7860/JCDR/2022/50677.15981. [DOI] [Google Scholar]
- 22.Ortega-Moreno D., Botello-Hernández E., Aguayo-Samaniego R., García-Espinosa P. The COVID-19 Pandemic. A Psychosocial Approach in Mexican Medical Students. Int. J. Med. Stud. 2023;10:S214. doi: 10.5195/ijms.2022.1793. [DOI] [Google Scholar]
- 23.Shahzad S., Saleem S. Reopening of Universities for On-Campus Teaching In COVID-19 Pandemic: Status of Generalized Anxiety in Medical Students. Proc. West. Mark. Ed. Assoc. Conf. 2022;36:7–13. doi: 10.47489/PSZMC-836362-7-13. [DOI] [Google Scholar]
- 24.Iqbal S.P., Siddiqui N., Gul F., Jaffri S.A. Anxiety and Depression among Medical Students of Karachi During the COVID-19 Pandemic. J. Bahria Univ. Med. Dent. Coll. 2023;13:217–222. doi: 10.51985/JBUMDC2022024. [DOI] [Google Scholar]
- 25.Gómez-Durán E.L., Fumadó C.M., Gassó A.M., Díaz S., Miranda-Mendizabal A., Forero C.G., Virumbrales M. COVID-19 Pandemic Psychological Impact and Volunteering Experience Perceptions of Medical Students after 2 Years. Int. J. Environ. Res. Public Health. 2022;19:7532. doi: 10.3390/ijerph19127532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiguna T., Dirjayanto V.J., Maharani Z.S., Faisal E.G., Teh S.D., Kinzie E. Mental health disturbance in preclinical medical students and its association with screen time, sleep quality, and depression during the COVID-19 pandemic. BMC Psychiatry. 2024;24:85. doi: 10.1186/s12888-024-05512-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tanusetiawan A.N., Surilena S., Tina Widjaja N., Agus D. Relationship of Depression and Sleep Quality among North Jakarta Medical Students during the COVID-19 Pandemic. [(accessed on 29 September 2024)];J. Kedokt. Brawijaya. 2022 32 doi: 10.21776/ub.jkb.2022.032.01.9. Available online: https://jkb.ub.ac.id/index.php/jkb/article/view/3070. [DOI] [Google Scholar]
- 28.Purnomo A.E., Rivami D.S. The Relationship between the Duration of Online Learning during the COVID-19 Pandemic and Symptoms of Depression in Medical Students of Pelita Harapan University: A Cross Sectional Study. Medicinus. 2021;11:68–77. doi: 10.19166/med.v9i2.4705. [DOI] [Google Scholar]
- 29.Yuryeva L., Tymofeyev R., Shornikov A., Kulbytska M. Prevalence of anxiety and depression and risk factors of their occurrence in medical students who had transferred COVID-19. Psychosom. Med. Gen. Pract. 2021;6:e0603309. doi: 10.26766/PMGP.V6I3.309. [DOI] [Google Scholar]
- 30.Arshad I., Maryam L., Mendagudali R.R., Agarwal N. Mental Health Effects of Online Education among Medical Students during the COVID-19 Pandemic in Kalaburagi, Karnataka, India: A Cross-sectional Study. J. Clin. Diagn. Res. 2023;17:LC01–LC05. doi: 10.7860/JCDR/2023/67258.18764. [DOI] [Google Scholar]
- 31.Lakshmi V. Impact of COVID-19 pandemic on the quality of life of medical under graduates and the prevalence of anxiety disorder among them. Int. J. Sci. Res. 2021;10:69–71. [Google Scholar]
- 32.Ernst J., Jordan K.D., Weilenmann S., Sazpinar O., Gehrke S., Paolercio F., Petry H., Pfaltz M.C., Méan M., Aebischer O., et al. Burnout, depression and anxiety among Swiss medical students—A network analysis. J. Psychiatr. Res. 2021;143:196–201. doi: 10.1016/j.jpsychires.2021.09.017. [DOI] [PubMed] [Google Scholar]
- 33.Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christophers B., Nieblas-Bedolla E., Gordon-Elliott J.S., Kang Y., Holcomb K., Frey M.K. Mental Health of US Medical Students During the COVID-19 Pandemic. J. Gen. Intern. Med. 2021;36:3295–3297. doi: 10.1007/s11606-021-07059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sartorão Filho C.I., Rodrigues W.C.d.L.V., de Castro R.B., Marçal A.A., Pavelqueires S., Takano L., de Oliveira W.L., Sartorão Neto C.I. Moderate and severe symptoms of anxiety and depression are increased among female medical students during the COVID-19 pandemic. Res. Soc. Dev. 2021;10:e34610615406. doi: 10.33448/rsd-v10i6.15406. [DOI] [Google Scholar]
- 36.Lin S., Chong A.C., Su E.H., Chen S.L., Chwa W.J., Young C., Schreiber J., Zia S.K. Medical student anxiety and depression in the COVID-19 Era: Unique needs of underrepresented students. Educ. Health. 2022;35:41–47. doi: 10.4103/efh.efh_112_22. [DOI] [PubMed] [Google Scholar]
- 37.Huarcaya-Victoria J., Elera-Fitzcarrald C., Crisol-Deza D., Villanueva-Zúñiga L., Pacherres A., Torres A., Huertas G., Calderón D., Noriega-Baella C., Astonitas E., et al. Factors associated with mental health in Peruvian medical students during the COVID-19 pandemic: A multicentre quantitative study. Rev. Colomb. Psiquiatr. 2023;52:236–244. doi: 10.1016/j.rcp.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Pinsai S., Klaipim C. 1294. COVID-19: Impacts on Medical Students’ Mental Health in Medical Education Center of Chaophya Abhaibhubejhr Hospital. Open Forum. Infect. Dis. 2022;9((Suppl. 2)):ofac492.1125. doi: 10.1093/ofid/ofac492.1125. [DOI] [Google Scholar]
- 39.Verma S., Mahajan R., Gupta V.V. An assessment of the impact of COVID-19 on the mental health of medical students across various medical colleges of Punjab. Int. J. Adv. Res. Med. 2021;3:389–394. doi: 10.22271/27069567.2021.v3.i1g.167. [DOI] [Google Scholar]
- 40.Alkwai H.M. Graduating from Medical School amid a Pandemic: A Study of Graduates’ Mental Health and Concerns. Educ. Res. Int. 2021;2021:8854587. doi: 10.1155/2021/8854587. [DOI] [Google Scholar]
- 41.Saravia-Bartra M.M., Cazorla-Saravia P., Cedillo-Ramirez L. Anxiety level of first-year medical students from a private university in Peru in times of COVID-19. Rev. De La Fac. De Med. Humana. 2020;20:568–573. doi: 10.25176/RFMH.v20i4.3198. [DOI] [Google Scholar]
- 42.Guralwar C., Kundawar A., Sharma S.K. Impact of COVID-19 pandemic on education and mental health of medical students: A nation-wide survey in India. Int. J. Community Med. Public Health. 2022;9:3491–3497. doi: 10.18203/2394-6040.ijcmph20222213. [DOI] [Google Scholar]
- 43.Almarri F.K., Alshareef R.I., Hajr E.A., Alotabi F.Z. Impact of COVID-19 pandemic on Saudi medical students’ career choices and perceptions of health specialties: Findings from a national cross-sectional study. BMC Med. Educ. 2022;22:174. doi: 10.1186/s12909-022-03224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kamran R., Tufail S., Raja H.Z., Alvi R.U., Shafique A., Saleem M.N., Sami W., Mahmood W.A. Post COVID-19 Pandemic Generalized Anxiety Status of Health Professional undergraduate students. Pak. J. Med. Health Sci. 2022;16:144–146. doi: 10.53350/pjmhs20221612144. [DOI] [Google Scholar]
- 45.Porwal A., Masmali S.M., Mokli N.K., Madkhli H.Y., Nandalur R.R., Porwal P., Adawi H. Assessment of Mental Health in Medical and Dental College Students in Jazan Province to See the Delayed Psychological Impact of COVID-19 Pandemic: An Online Survey. World J. Dent. 2023;14:36–40. doi: 10.5005/jp-journals-10015-2105. [DOI] [Google Scholar]
- 46.Primatanti P.A., Turana Y., Sukarya W.S., Wiyanto M., Duarsa A.B.S. Medical students’ mental health state during pandemic COVID-19 in Indonesia. Bali Med. J. 2023;12:1295–1301. doi: 10.15562/bmj.v12i2.4104. [DOI] [Google Scholar]
- 47.AbuDujain N.M., Almuhaideb Q.A., Alrumaihi N.A., Alrabiah M.A., Alanazy M.H., Abdulghani H. The Impact of the COVID-19 Pandemic on Medical Interns’ Education, Training, and Mental Health: A Cross-Sectional Study. Cureus. 2021;13:e19250. doi: 10.7759/cureus.19250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Imran N., Haider I.I., Mustafa A.B., Aamer I., Kamal Z., Rasool G., Azeem M.W., Javed A. The hidden crisis: COVID-19 and impact on mental health of medical students in Pakistan. Middle East Curr. Psychiatry. 2021;28:45. doi: 10.1186/s43045-021-00123-7. [DOI] [Google Scholar]
- 49.Hossini Rafsanjanipoor S.M., Zakeri M.A., Dehghan M., Kahnooji M., Zakeri M. Psychological Consequences of the COVID-19 Disease among Physicians and Medical Students: A Survey in Kerman Province, Iran, in 2020. J. Occup. Health Epidemiol. 2021;10:274–281. doi: 10.52547/johe.10.4.274. [DOI] [Google Scholar]
- 50.Srivastava S., Jacob J., Charles A.S., Daniel P., Mathew J.K., Shanthi P., Devamani K., Mahasampath G., Rabi S. Emergency remote learning in anatomy during the COVID-19 pandemic: A study evaluating academic factors contributing to anxiety among first year medical students. Med. J. Armed Forces India. 2021;77((Suppl. 1)):S90–S98. doi: 10.1016/j.mjafi.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pedraz-Petrozzi B., Krüger-Malpartida H., Arevalo-Flores M., Salmavides-Cuba F., Anculle-Arauco V., Dancuart-Mendoza M. Emotional Impact on Health Personnel, Medical Students, and General Population Samples During the COVID-19 Pandemic in Lima, Peru. Rev. Colomb. Psiquiatr. 2021;50:189–198. doi: 10.1016/j.rcp.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vajpeyi Misra A., Mamdouh H.M., Dani A., Mitchell V., Hussain H.Y., Ibrahim G.M., Alnakhi W.A. Impact of COVID-19 pandemic on the mental health of university students in the United Arab Emirates: A cross-sectional study. BMC Psychol. 2022;10:312. doi: 10.1186/s40359-022-00986-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alshehri A., Alshehri B., Alghadir O., Basamh A., Alzeer M., Alshehri M., Nasr S. The prevalence of depressive and anxiety symptoms among first-year and fifth-year medical students during the COVID-19 pandemic: A cross-sectional study. BMC Med. Educ. 2023;23:411. doi: 10.1186/s12909-023-04387-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paz D.C., Bains M.S., Zueger M.L., Bandi V.R., Kuo V.Y., Payton M., Ryznar R.J. Impact of COVID-19 on Rocky Vista University medical students’ mental health: A cross-sectional survey. Front. Psychol. 2023;14:1076841. doi: 10.3389/fpsyg.2023.1076841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schindler A.K., Polujanski S., Rotthoff T. A longitudinal investigation of mental health, perceived learning environment and burdens in a cohort of first-year German medical students’ before and during the COVID-19 ‘new normal’. BMC Med. Educ. 2021;21:413. doi: 10.1186/s12909-021-02798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lu L., Wang X., Wang X., Guo X., Pan B. Association of COVID-19 pandemic-related stress and depressive symptoms among international medical students. BMC Psychiatry. 2022;22:20. doi: 10.1186/s12888-021-03671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chakeeyanun B., Wongpakaran N., Wongpakaran T., Oon-arom A. Resilience, Perceived Stress from Adapted Medical Education Related to Depression among Medical Students during the COVID-19 Pandemic. Healthcare. 2023;11:237. doi: 10.3390/healthcare11020237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Camelier-Mascarenhas M., Jesuino T.A., Queirós V.O.d., Brito L.L.C., Fernandes S.M., Almeida A.G.d. Mental health evaluation in medical students during academic activity suspension in the pandemic. Rev. Bras. Educ. Med. 2023;47:e087. doi: 10.1590/1981-5271v47.3-2022-0298.ing. [DOI] [Google Scholar]
- 59.Dziedzic D.M., Dell’Agnelo G.S., Schindler Junior E., Lindstron O.A., Andrade F.A., Nisihara R. Anxiety and insecurity in medical interns: The impact of the pandemic COVID-19. Medicina (Ribeirão Preto) 2022;55:e-191222. doi: 10.11606/issn.2176-7262.rmrp.2022.191222. [DOI] [Google Scholar]
- 60.Eleftheriou A., Rokou A., Arvaniti A., Nena E., Steiropoulos P. Sleep Quality and Mental Health of Medical Students in Greece During the COVID-19 Pandemic. Front. Public Health. 2021;9:775374. doi: 10.3389/fpubh.2021.775374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cheng J., Liao M., He Z., Xiong R., Ju Y., Liu J., Liu B., Wu B., Zhang Y. Mental health and cognitive function among medical students after the COVID-19 pandemic in China. Front. Public Health. 2023;11:1233975. doi: 10.3389/fpubh.2023.1233975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Santander-Hernández F.M., Peralta C.I., Guevara-Morales M.A., Díaz-Vélez C., Valladares-Garrido M.J. Smartphone overuse, depression & anxiety in medical students during the COVID-19 pandemic. PLoS ONE. 2022;17:e0273575. doi: 10.1371/journal.pone.0273575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Çimen İ.D., Alvur T.M., Coşkun B., Şükür N.E.Ö. Mental health of Turkish medical students during the COVID-19 pandemic. Int. J. Soc. Psychiatry. 2022;68:1253–1262. doi: 10.1177/00207640211066734. [DOI] [PubMed] [Google Scholar]
- 64.Villalón López F.J., Moreno Cerda M.I., GonzáLez Venegas W., Soto Amaro A.A., Arancibia Campos J.V. [Anxiety and depression among medical students during COVID-19 pandemic] Rev. Med. Chil. 2022;150:1018–1025. doi: 10.4067/S0034-98872022000801018. [DOI] [PubMed] [Google Scholar]
- 65.Villagómez-López A.M., Cepeda-Reza T.F., Torres-Balarezo P.I., Calderón-Vivanco J.M., Villota-Acosta C.A., Balarezo-Díaz T.F., Simbaña-Guaycha F.C., Vallejo-Suárez C.N., Rueda-Benalcazar D.M., Vaca-Salazar J.C., et al. [Depression and anxiety among medical students in virtual education during COVID-19 pandemic] Rev. Med. Inst. Mex. Seguro Soc. 2023;61:559–566. doi: 10.5281/zenodo.8316418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harries A.J., Lee C., Jones L., Rodriguez R.M., Davis J.A., Boysen-Osborn M., Kashima K.J., Krane N.K., Rae G., Kman N., et al. Effects of the COVID-19 pandemic on medical students: A multicenter quantitative study. BMC Med Educ. 2021;21:1–8. doi: 10.1186/s12909-020-02462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu Z., Liu R., Zhang Y., Zhang R., Liang L., Wang Y., Wei Y., Zhu R., Wang F. Latent class analysis of depression and anxiety among medical students during COVID-19 epidemic. BMC Psychiatry. 2021;21:1–10. doi: 10.1186/s12888-021-03459-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pattanaseri K., Atsariyasing W., Pornnoppadol C., Sanguanpanich N.B., Srifuengfung M. Mental problems and risk factors for depression among medical students during the COVID-19 pandemic: A cross-sectional study. Medicine. 2022;101:e30629. doi: 10.1097/MD.0000000000030629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Teh B.L.S., Ang J.K., Koh E.B.Y., Pang N.T.P. Psychological Resilience and Coping Strategies with Anxiety among Malaysian Medical Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Heal. 2023;20:1894. doi: 10.3390/ijerph20031894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Adhikari A., Sujakhu E., Gc S., Zoowa S. Depression among Medical Students of a Medical College in Nepal during COVID-19 Pandemic: A Descriptive Cross-sectional Study. J. Nepal Med Assoc. 2021;59:645–648. doi: 10.31729/jnma.5441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chalise P.C., Singh A., Rawal E., Budhathoki P., Sharma S., Jyotsana P., Kafle R. Composite Anxiety-depression among Medical Undergraduates during COVID-19 Pandemic in a Tertiary Care Hospital: A Descriptive Cross-sectional Study. J. Nepal Med Assoc. 2021;59:881–885. doi: 10.31729/jnma.6947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Romic I., Silovski H., Mance M., Pavlek G., Petrovic I., Figl J., Grbavac D., Moric T., Romic R., Bakula B., et al. Psychological Effects of "Double Crisis" (COVID-19 Pandemic and Earthquakes) on Croatian Medical Students. Psychiatria Danubina. 2021;33:120–125. [PubMed] [Google Scholar]
- 73.Nguyen D.T., Ngo T.M., Nguyen H.L.T., Le M.D., Duong M.L.N., Hoang P.H., Nguyen H.V., Foster K., Duong T.V., Kim G.B., et al. The prevalence of self-reported anxiety, depression, and associated factors among Hanoi Medical University’s students during the first wave of COVID-19 pandemic. PLoS ONE. 2022;17:e0269740. doi: 10.1371/journal.pone.0269740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Biswas A.A.J., Hasan M.T., Samir N., Alin S.I., Homaira N., Hassan Z., Khatun M.R., Anjum A., Hossain S., Koly K.N., et al. The Prevalence and Associated Factors of Depressive Symptoms Among Medical Students in Bangladesh During the COVID-19 Pandemic: A Cross-Sectional Pilot Study. Front. Public Heal. 2022;9:811345. doi: 10.3389/fpubh.2021.811345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Song Y., Sznajder K., Cui C., Yang Y., Li Y., Yang X. Anxiety and its relationship with sleep disturbance and problematic smartphone use among Chinese medical students during COVID-19 home confinement — A structural equation model analysis. J. Affect. Disord. 2021;296:315–321. doi: 10.1016/j.jad.2021.09.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guo A.A., Crum M.A., Fowler L.A. Assessing the Psychological Impacts of COVID-19 in Undergraduate Medical Students. Int. J. Environ. Res. Public Heal. 2021;18:2952. doi: 10.3390/ijerph18062952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Essangri H., Sabir M., Benkabbou A., Majbar M.A., Amrani L., Ghannam A., Lekehal B., Mohsine R., Souadka A. Predictive Factors for Impaired Mental Health among Medical Students during the Early Stage of the COVID-19 Pandemic in Morocco. Am. J. Trop. Med. Hyg. 2021;104:95–102. doi: 10.4269/ajtmh.20-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saali A., Stanislawski E.R., Kumar V., Chan C., Hurtado A., Pietrzak R.H., Charney D.S., Ripp J., Katz C.L. The Psychiatric Burden on Medical Students in New York City Entering Clinical Clerkships During the COVID-19 Pandemic. Psychiatr. Q. 2021;93:419–434. doi: 10.1007/s11126-021-09955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nishimura Y., Ochi K., Tokumasu K., Obika M., Hagiya H., Kataoka H., Otsuka F. Impact of the COVID-19 Pandemic on the Psychological Distress of Medical Students in Japan: Cross-sectional Survey Study. J. Med Internet Res. 2021;23:e25232. doi: 10.2196/25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sserunkuuma J., Kaggwa M.M., Muwanguzi M., Najjuka S.M., Murungi N., Kajjimu J., Mulungi J., Kihumuro R.B., Mamun M.A., Griffiths M.D., et al. Problematic use of the internet, smartphones, and social media among medical students and relationship with depression: An exploratory study. PLOS ONE. 2023;18:e0286424. doi: 10.1371/journal.pone.0286424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Batais M.A., Temsah M.H., AlGhofili H., AlRuwayshid N., Alsohime F., Almigbal T.H., Al-Rabiaah A., Al-Eyadhy A.A., Mujammami M.H., Halwani R., et al. The coronavirus disease of 2019 pandemic-associated stress among medical students in middle east respiratory syndrome-CoV endemic area. Medicine. 2021;100:e23690. doi: 10.1097/MD.0000000000023690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Crisol-Deza D., Poma-Ramírez D., Pacherres-López A., Noriega-Baella C., Villanueva-Zúñiga L., Salvador-Carrillo J., Huarcaya-Victoria J. Factors associated with suicidal ideation among medical students during the initial phase of the COVID-19 pandemic in Peru: A multicenter study. Death Stud. 2022;47:183–191. doi: 10.1080/07481187.2022.2042752. [DOI] [PubMed] [Google Scholar]
- 83.Tsiouris A., Werner A.M., Tibubos A.N., Mülder L.M., Reichel J.L., Heller S., Schäfer M., Schwab L., Rigotti T., Stark B., et al. Mental health state and its determinants in German university students across the COVID-19 pandemic: Findings from three repeated cross-sectional surveys between 2019 and 2021. Front. Public Heal. 2023;11:1163541. doi: 10.3389/fpubh.2023.1163541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sudi R., Chang W.L., Arshad N.H., Abidin S.N.Z., Suderman U., Woon L.S.-C. Perception of Current Educational Environment, Clinical Competency, and Depression among Malaysian Medical Students in Clinical Clerkship: A Cross-Sectional Study. Int. J. Environ. Res. Public Heal. 2022;19:16274. doi: 10.3390/ijerph192316274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wercelens V.O., Bueno M.L., Bueno J.L., Abrahim R.P., Ydy J.G.M., Zanetti H.R., Montayre J., Maximiano-Barreto M.A. Empathy and psychological concerns among medical students in Brazil during the COVID-19 pandemic. Int. J. Psychiatry Med. 2023;58:510–521. doi: 10.1177/00912174231179069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yin Y., Yang X., Gao L., Zhang S., Qi M., Zhang L., Tan Y., Chen J. The Association Between Social Support, COVID-19 Exposure, and Medical Students’ Mental Health. Front. Psychiatry. 2021;12:555893. doi: 10.3389/fpsyt.2021.555893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chwa W.J., Chong A.C., Lin S., Su E.H., Sheridan C., Schreiber J., Zia S.K., Thompson K. Mental Health Disparities among Pre-Clinical Medical Students at Saint Louis University during the COVID-19 Pandemic. Behav. Sci. 2024;14:89. doi: 10.3390/bs14020089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pandey U., Corbett G., Mohan S., Reagu S., Kumar S., Farrell T., Lindow S. Anxiety, Depression and Behavioural Changes in Junior Doctors and Medical Students Associated with the Coronavirus Pandemic: A Cross-Sectional Survey. J. Obstet. Gynecol. India. 2020;71:33–37. doi: 10.1007/s13224-020-01366-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Elhadi M., Buzreg A., Bouhuwaish A., Khaled A., Alhadi A., Msherghi A., Alsoufi A., Alameen H., Biala M., Elgherwi A., et al. Psychological Impact of the Civil War and COVID-19 on Libyan Medical Students: A Cross-Sectional Study. Front. Psychol. 2020;11:570435. doi: 10.3389/fpsyg.2020.570435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xiao H., Shu W., Li M., Li Z., Tao F., Wu X., Yu Y., Meng H., Vermund S.H., Hu Y. Social Distancing among Medical Students during the 2019 Coronavirus Disease Pandemic in China: Disease Awareness, Anxiety Disorder, Depression, and Behavioral Activities. Int. J. Environ. Res. Public Health. 2020;17:5047. doi: 10.3390/ijerph17145047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Essadek A., Gressier F., Robin M., Shadili G., Bastien L., Peronnet J.C., Falissard B., Rabeyron T. Mental health of medical students during the COVID19: Impact of studies years. J. Affect. Disord. Rep. 2022;8:100318. doi: 10.1016/j.jadr.2022.100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Liu J., Zhu Q., Fan W., Makamure J., Zheng C., Wang J. Online Mental Health Survey in a Medical College in China During the COVID-19 Outbreak. Front. Psychiatry. 2020;11:459. doi: 10.3389/fpsyt.2020.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chootong R., Sono S., Choomalee K., Wiwattanaworaset P., Phusawat N., Wanghirankul N., Laojaroensuk P., Thongkhundum P., Saetang R., Euanontat S., et al. The association between physical activity and prevalence of anxiety and depression in medical students during COVID-19 pandemic: A cross-sectional study. Ann. Med. Surg. 2022;75:103408. doi: 10.1016/j.amsu.2022.103408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Saeed N., Javed N. Lessons from the COVID-19 pandemic: Perspectives of medical students. Pak. J. Med. Sci. 2021;37:1402–1407. doi: 10.12669/pjms.37.5.4177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Huang W., Wen X., Li Y., Luo C. Association of perceived stress and sleep quality among medical students: The mediating role of anxiety and depression symptoms during COVID-19. Front. Psychiatry. 2024;15:1272486. doi: 10.3389/fpsyt.2024.1272486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yun J.Y., Kim J.W., Myung S.J., Yoon H.B., Moon S.H., Ryu H., Yim J.J. Impact of COVID-19 on Lifestyle, Personal Attitudes, and Mental Health Among Korean Medical Students: Network Analysis of Associated Patterns. Front. Psychiatry. 2021;12:702092. doi: 10.3389/fpsyt.2021.702092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Halperin S.J., Henderson M.N., Prenner S., Grauer J.N. Prevalence of Anxiety and Depression Among Medical Students During the Covid-19 Pandemic: A Cross-Sectional Study. J. Med. Educ. Curric. Dev. 2021;8:238212052199115. doi: 10.1177/2382120521991150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bilgi K., Aytaş G., Karatoprak U., Kazancıoǧlu R., Özçelik S. The Effects of Coronavirus Disease 2019 Outbreak on Medical Students. Front Psychiatry. 2021;12:637946. doi: 10.3389/fpsyt.2021.637946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Alsairafi Z., Naser A.Y., Alsaleh F.M., Awad A., Jalal Z. Mental Health Status of Healthcare Professionals and Students of Health Sciences Faculties in Kuwait during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2021;18:2203. doi: 10.3390/ijerph18042203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Allah A.A., Algethami N.E., Algethami R.A., ALAyyubi R.H., Altalhi W.A., Atalla A.A.A. Impact of COVID-19 on psychological and academic performance of medical students in Saudi Arabia. J. Fam. Med. Prim. Care. 2021;10:3857–3862. doi: 10.4103/jfmpc.jfmpc_1004_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Khidri F.F., Riaz H., Bhatti U., Shahani K.A., Kamran Ali F., Effendi S., Rani K., Chohan M.N. Physical Activity, Dietary Habits and Factors Associated with Depression Among Medical Students of Sindh, Pakistan, During the COVID-19 Pandemic. Psychol. Res. Behav. Manag. 2022;15:1311–1323. doi: 10.2147/PRBM.S364540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shreevastava A.K., Mavai M., Mittal P.S., Verma R., Kaur D., Bhandari B. Assessment of the psychological impact of COVID-19 pandemic on undergraduate medical students in India. J. Educ. Health Promot. 2022;11:214. doi: 10.4103/jehp.jehp_1273_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Afzal S.S., Qamar M.A., Dhillon R., Bhura M., Khan M.H., Suriya Q., Siddiqui S., Ali Khan M.R., Abbas S.A. Budding Medical Professionals and Covid-19: The Impact of COVID-19 on Mental Health and Medical Students. J. Ayub Med. Coll. Abbottabad. 2022;34:483–488. doi: 10.55519/JAMC-03-9572. [DOI] [PubMed] [Google Scholar]
- 104.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sazakli E., Leotsinidis M., Bakola M., Kitsou K.S., Katsifara A., Konstantopoulou A., Jelastopulu E. Prevalence and Associated Factors of Anxiety and Depression in Students at a Greek University during Covid-19 Lockdown. J. Public Health Res. 2021;10:jphr-2021. doi: 10.4081/jphr.2021.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wade M., Prime H., Johnson D., May S.S., Jenkins J.M., Browne D.T. The disparate impact of COVID-19 on the mental health of female and male caregivers. Soc. Sci. Med. 2021;275:113801. doi: 10.1016/j.socscimed.2021.113801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brenneisen Mayer F., Souza Santos I., Silveira P.S.P., Itaqui Lopes M.H., de Souza A.R.N.D., Campos E.P., de Abreu B.A.L., Hoffman II I., Magalhães C.R., Lima M.C.P., et al. Factors associated to depression and anxiety in medical students: A multicenter study. BMC Med. Educ. 2016;16:282. doi: 10.1186/s12909-016-0791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lund C., Breen A., Flisher A.J., Kakuma R., Corrigall J., Joska J.A., Swartz L., Patel V. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc. Sci. Med. 2010;71:517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Demyttenaere K., Bruffaerts R., Posada-Villa J., Gasquet I. Prevalence, Severity, and Unmet Need for Treatment of Mental Disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 110.Rai D., Zitko P., Jones K., Lynch J., Araya R. Country- and individual-level socioeconomic determinants of depression: Multilevel cross-national comparison. Br. J. Psychiatry. 2013;202:195–203. doi: 10.1192/bjp.bp.112.112482. [DOI] [PubMed] [Google Scholar]
- 111.Paz D.C., Bains M.S., Zueger M.L., Bandi V.R., Kuo V.Y., Cook K., Ryznar R. COVID-19 and mental health: A systematic review of international medical student surveys. Front. Psychol. 2022;13:1028559. doi: 10.3389/fpsyg.2022.1028559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ewid M., Amal Y., Billah S.M.B., Kalou Y., Zitoun O.A., Alnaser A.R., Nashawi M.O., Almazrou A. Impact of the COVID-19 pandemic on the psychological status of undergraduate medical students in Saudi Arabia: A cross-sectional double-scale study. Medicine. 2023;102:e33487. doi: 10.1097/MD.0000000000033487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mirilović N., Janković J., Latas M. The impact of the COVID-19 epidemic on students’ mental health: A cross-sectional study. PLoS ONE. 2022;17:e0275167. doi: 10.1371/journal.pone.0275167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lee C.M., Juarez M., Rae G., Jones L., Rodriguez R.M., Davis J.A., Boysen-Osborn M., Kashima K.J., Krane N.K., Kman N., et al. Anxiety, PTSD, and stressors in medical students during the initial peak of the COVID-19 pandemic. PLoS ONE. 2021;16:e0255013. doi: 10.1371/journal.pone.0255013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Peng P., Hao Y., Liu Y., Chen S., Wang Y., Yang Q., Wang X., Li M., Wang Y., He L., et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2023;321:167–181. doi: 10.1016/j.jad.2022.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Juanico-Morales L., Nava-Aguilera E., Morales-Pérez A., Morales-Nava L., Valdez-Bencomo M.A., Emigdio-Vargas A., Serrano-de Los Santos F.R., Andersson N. Depression and associated factors in medical students in Acapulco during the COVID-19 pandemic: A cross-sectional study. PLoS ONE. 2023;18:e0285903. doi: 10.1371/journal.pone.0285903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jia Q., Qu Y., Sun H., Huo H., Yin H., You D. Mental Health Among Medical Students During COVID-19: A Systematic Review and Meta-Analysis. Front. Psychol. 2022;13:846789. doi: 10.3389/fpsyg.2022.846789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lin Y.K., Saragih I.D., Lin C.J., Liu H.L., Chen C.W., Yeh Y.S. Global prevalence of anxiety and depression among medical students during the COVID-19 pandemic: A systematic review and meta-analysis. BMC Psychol. 2024;12:338. doi: 10.1186/s40359-024-01838-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.