Abstract
A 53-year-old woman presented to the surgical emergency with complaints of high-grade fever accompanied by chills for 15 days and pain in the right upper abdomen for 10 days. X-ray of the abdomen and chest X-ray revealed free gas under the right hemidiaphragm. As there were no signs of generalised or localised peritonitis, emergency laparotomy was postponed. Subsequently, a contrast-enhanced computerised tomography scan of the abdomen suggested an emphysematous liver abscess, which was managed by ultrasonography-guided drainage of the abscess cavity.
Keywords: Emphysematous liver abscess, Klebsiella pneumoniae, peritonitis, pigtail drainage, pneumoperitoneum
Introduction
Emphysematous liver abscess is always accompanied by gas formation and hence is also known as gas-forming pyogenic liver abscess.[1] The management of acute emphysematous liver abscess requires urgent external drainage of the abscess cavity. However, the presence of gas under the right hemidiaphragm on radiological imaging can present a serious diagnostic challenge, potentially leading surgeons to perform unnecessary exploratory laparotomy.
Case Presentation
A 53-year-old woman with no known chronic comorbidities such as diabetes or hypertension presented to the emergency surgical ward with complaints of intermittent fever accompanied by rigors and chills for the past 15 days. She also reported pain in the right upper abdomen for 10 days and abdominal distention for 3 days. On clinical examination, right upper abdominal tenderness, guarding, and rigidity were absent. Bowel sounds were normally present. A complete blood count revealed a hemoglobin level of 5.8 g/dL, a total leukocyte count of 20,500 cells/mm3, and a platelet count of 1.8 × 106/mm3. Prothrombin time was 17.7 s, and INR was 1.26. The kidney function test indicated a normal serum urea level of 22 mg/dL and serum creatinine of 1.2 mg/dL. The liver function test showed normal bilirubin levels (1.0 mg/dL), raised serum glutamic-oxaloacetic transaminase of 176 IU/L, serum glutamic pyruvic transaminase of 200 IU/L, serum alkaline phosphatase of 1263.2 IU/L, gamma glutaryl transferase of 48 IU/L, and serum albumin of 2.3 g/dL. She had a raised blood glucose level of 148 mg/dL, with an glycated hemoglobin (HbA1c) of 7.1, indicating poor glycemic control. Urinary ketones were negative, and arterial blood gas tests revealed arterial blood pH values of 7.36, ruling out the possibility of diabetic ketoacidosis. The erect X-ray of the abdomen indicated gas under the right hemidiaphragm [Figure 1]. Acute hollow viscus perforation was diagnosed. However, in the absence of evident signs of peritonitis, a contrast-enhanced computerised tomography of the whole abdomen was performed. It revealed free gas under the right hemidiaphragm, two large hypodense spaces occupying lesions with homogenous collection in the liver parenchyma involving segments 8, 2, and 3. Additionally, specks of air with air-fluid levels were also noted inside the hypodense lesions [Figure 2]. A diagnosis of emphysematous liver abscess was made. The abscess aspirate was reddish brown and purulent. Culture analysis of the aspirate revealed the presence of Klebsiella pneumoniae. Sensitivity testing of pus demonstrated sensitivity to piperacillin, ceftazidime, levofloxacin, fosfomycin, amikacin, sulbactam, gentamicin, meropenem, ceftriaxone, and cefmetazole. No malignant cells were noted on pathological examination of the aspirate.
Figure 1.
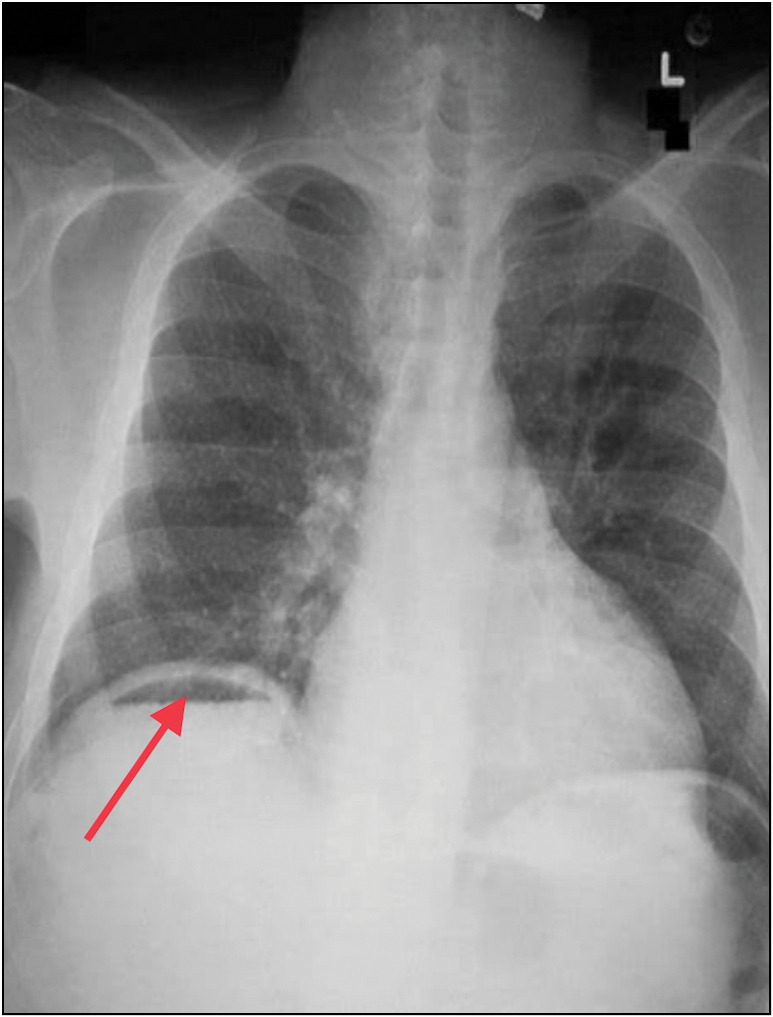
Erect X-ray of the chest showing free gas under the right hemidiaphragm
Figure 2.
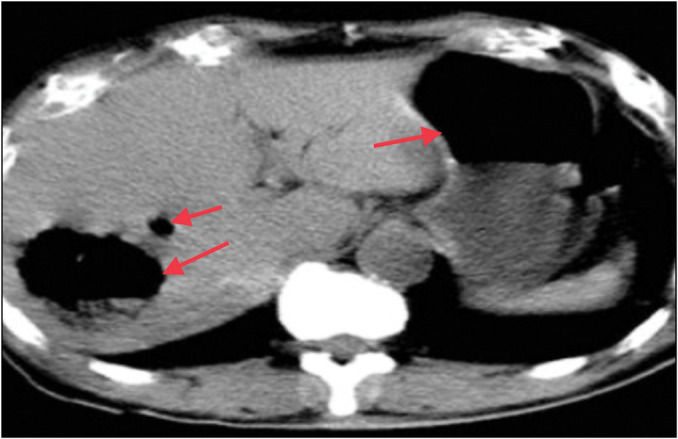
CECT (axial view) of the abdomen showing free gas under the right hemidiaphragm, along with hepatomegaly. Additionally, two large cavities can be seen in the liver parenchyma in both lobes of the liver, along with a homogenous collection involving segments 8, 2, and 3 of the liver. Specks of air were present with air-fluid levels inside the hypodense lesions. CECT: contrast-enhanced computerised tomography
The presence of K. pneumoniae in the abscess aspirate strengthened our diagnosis, as it is the most common cause of emphysematous liver abscess in an Asian setting. The patient was resuscitated with intravenous fluids and intravenous antibiotics (meropenem 3 g/day), along with glycemic control by oral hypoglycemic agents. Urgent ultrasound-guided external drainage of the abscess cavity was performed with a pigtail catheter, which drained 200 mL of pus with air bubbles. The condition of the patient improved gradually, and she was discharged on the fourth postoperative day after drainage, with the pigtail catheter in situ. She continued on oral antibiotics and oral hypoglycemic agents for glycemic control, maintaining fair general conditions, with stable vitals. The pigtail catheter was removed after 14 days with no sequelae.
Discussion
Acute abdominal pain with pneumoperitoneum (gas in the peritoneal cavity, seen under the diaphragm in an erect X-ray of the abdomen) is a medical emergency requiring urgent evaluation and management. Perforated hollow viscus constitutes approximately 90% of cases.[1] Other causes may include intra-abdominal sepsis due to gas-forming organisms, biliary-enteric fistula, post-laparotomy/laparoscopic procedure, gallstone ileus, post-scuba diving, and pneumatosis coli.[2,3,4]
Emphysematous liver abscess is typically characterised by gas formation within the abscess cavity.[1] Emphysematous liver abscesses were first reported by Smith in 1944.[1] Its reported incidence is 6%–24%.[2] The majority of cases are reported in the Asian subcontinent, predominantly from Taiwan.[3] K. pneumoniae (70%) is the most commonly reported pathogen.[4] Diabetics with poor glycemic control (HbA1c ≥ 8%) have a higher predisposition of developing emphysematous liver abscess. Glucose metabolism via the mixed acid fermentation pathway leads to the production of formic acid that gets converted to formic hydrogenylase after excessive accumulation (pH ≤ 6), ultimately breaking down into carbon dioxide and hydrogen.[3] The production of hydrogen is the hallmark feature of the mixed acid fermentation pathway, as it is not generated in any of the other five fermentation pathways.[3] In a study by Lee et al.,[3] analyses of gas samples from five patients with gas-forming liver abscess due to K. pneumoniae showed the following composition: nitrogen—65.8% to 78.1%; oxygen—1.2% to 7.3%; carbon dioxide—5.4% to 14.8%; and hydrogen—9.0% to 18.3%.
A major complication of emphysematous liver abscesses is that it is prone to rupture due to extensive tissue damage and an increase in internal pressure due to the formation of gases.[5] If not promptly treated, they can be fatal, with mortality rates reported as high as 27% in various studies.[3] Computerised tomography (CT) is the preferred diagnostic for accurately detecting gas within abscesses.[6] Treatment primarily involves percutaneous abscess drainage, accompanied by antibiotic therapy and glycemic control.[3] In the study by Lee et al., 22 cases of emphysematous liver abscess were examined, with percutaneous transhepatic abscess drainage performed in 19 cases, while surgery was required in 1 case. Surgery is typically reserved for cases of ruptured abscess and peritonitis.[3]
In our case, the presence of gas under the diaphragm on the chest X-ray, which was a diagnostic challenge and could potentially mislead the surgeon, leading to an unnecessary laparotomy in search of a hollow viscus perforation in the abdomen. This also emphasises the importance of comprehensive clinical examination, supported by clinical imaging, preferably a CT scan of the abdomen.
A PubMed Central search using the keyword “Emphysematous liver abscess” yielded 14 results, including 11 case reports of emphysematous liver abscess summarised in Table 1. Our patient presented with fever, pain in the abdomen, and abdominal distension. Out of the 11 cases, fever was observed in four cases,[8,12,15,16] while abdominal pain was noted in six—right hypochondriac pain in three cases[9,11,15] and epigastric pain in the other three cases.[12,13,14] Other symptoms include fatigue, malaise, jaundice, altered sensorium, anorexia, nausea, vomiting, bilateral pedal oedema, and cough.[6,7,8,9,10,11,12,13,14,15,16] In our case, the abscess was drained using a pigtail catheter under image guidance following an antibiotic course. Similar management was done in 8 out of the 11 reported cases.[6,7,10,11,12,13,15,16] In the remaining cases, only antibiotic therapy,[8] aspiration of the abscess,[14] and surgery[9] were performed. K. pneumoniae was found in the aspirate in our case, which was also observed in 9 out of the 11 cases[6,8,9,10,11,12,13,14,16] [Table 1]. In the other two cases, Edwardsiella tarda and Escherichia coli coinfection[7] and Clostridium paraputificum[15] were identified in the culture.
Table 1.
Summary of a review of the existing literature of cases of “Emphysematous Liver Abscess” in PubMed Central
| Serial number | Title | Authors (year of publication, country) | Patient presentation | Mode of diagnosis | Intervention carried out | Organism | Comments |
|---|---|---|---|---|---|---|---|
| 1. | Emphysematous liver abscess with Edwardsiella tarda infection | Tominaga et al. (2022, Japan) [7] | 51 y/o; female; general fatigue for 2 days | CECT: gas in a large area of the left hepatic lobe | Percutaneous transhepatic abscess drainage with antibiotics | E. tarda and Escherichia coli | The patient has SLE, APLA syndrome, DM, and choledocholithiasis and was being treated with hydroxychloroquine, prednisolone, and tacrolimus |
| 2. | Emphysematous liver abscess and disseminated hypervirulent Klebsiella pneumoniae infection in a patient from southern India | Nayak et al. (2022, India) [8] | 48 y/o; male; myalgia for 10 days, fever for 4 days, jaundice for 4 days, altered sensorium for 1 day; icteric with liver palpable 6 cm BCM |
USG: 2 hypoechoic lesions suggestive of liver abscess (largest 7 × 5 cm); CECT: emphysematous abscess with multiple gas pockets | Antibiotics only | Hypervirulent Klebsiella pneumoniae | Alcoholic for 10 years; acute bacterial meningitis is also present |
| 3. | An easily neglected rapid progressive emphysematous liver abscess | Tsai et al. (2021, Taiwan) [9] | 62 y/o; female; right hypochondriac abdominal pain for 1 week | X-ray: diaphragm elevated on the right side with lieu’s only; CECT: multifocal liver necrosis, gas-forming abscesses, pneumoperitoneum, and retroperitoneal abscesses | Emergency surgery with necrosectomy and drainages on hepatic and retroperitoneal abscesses | Klebsiella pneumoniae | DM with poor glycemic control under Chinese herb |
| 4. | Fatal systemic emphysematous infection caused by Klebsiella pneumoniae: A case report | Zhang et al. (2022, China) [10] | 66 y/o; male; worsening fatigue, anorexia, nausea, and vomiting for 14 days and confusion and jaundice for 3 days | CECT: numerous emphysematous hepatic abscesses, rupture of some liver abscesses, and gas formation in the right subphrenic area | Ultrasound-guided percutaneous liver abscess drainage with antibiotics; hemofiltration for AKI; the patient died in spite of treatment | Klebsiella pneumoniae | Pelvic CT showed intramural gas formation in the bladder and enlarged prostate and left seminal vesicle with abnormal air accumulation; chest CT revealed pulmonary infiltrates in the right lower lobes and small right pleural effusion |
| 5. | Ruptured emphysematous liver abscess: An unusual presentation in Kochs | Bakhshi et al. (2021, India) [11] | 45 y/o; female; pain in the right upper abdomen for 1 month and bilateral pedal oedema for 7 days | X-ray: large air-fluid level under the right diaphragm with multiple air-fluid levels in the right upper part of the abdomen; CECT: ruptured liver abscess in VII and VI segments (300 cc liquid with gas within) with collection tracking along the right parabolic gutter till pelvis (800 cc collection) | USG-guided percutaneous abscess drainage and catheter placement in the liver and pelvis, along with antibiotics | Klebsiella pneumoniae | |
| 6. | Emphysematous liver abscess in a 58-year-old woman | Hsu et al. (2018, Taiwan) [12] | 58 y/o; female; fever, malaise, cough, and epigastric pain for 5 days | X-ray: air-fluid level over the tight subphrenic area; CECT: gas-forming pyogenic liver abscess | Ultrasound-guided pigtail catheter abscess drainage with antibiotics | Klebsiella pneumoniae | Hypertension and type 2 DM present |
| 7. | Emphysematous liver abscess mimicking a gastric bubble | Lee et al. (2019, Taiwan) [13] | 47 y/o; male; epigastric pain (intermittent and increased coughing) for 5 days | X-ray: air accumulation with the air-fluid level on the left hypochondrium; CECT: huge abscess (8cm) with the air-fluid level over the left lobe of the liver | Pigtail drainage, antibiotics, and insulin control | Klebsiella pneumoniae | Alcoholic for more than 10 years |
| 8. | Life-threatening emphysematous liver abscess associated with poorly controlled diabetes mellitus: A case report | Takano et al. (2017, Japan) [6] | 69 y/o, male; fever and general malaise for 2 weeks | CECT: 5cm abscess with gas in the right hepatic lobe | Emergency percutaneous drainage | Klebsiella pneumoniae | Type 2 DM with markedly impaired glucose tolerance |
| 9. | Gas under diaphragm: A rare case of ruptured liver abscess with gas-forming organism | Maliyakkal et al. (2022, Qatar) [14] | 58 y/o; male; generalised fatigue for 2 weeks and epigastric and right shoulder pain for 1 week | X-ray: right subdiaphragmatic free air, with heterogeneous liver shadow and air-fluid level; CECT: large right subcapsular hepatic lesion (11.5 × 8.5 × 9 cm) with irregular outline, containing gas predominantly, with dependant fluid; free air in the right subphrenic region along the anterior and inferior aspect of the liver | Ultrasound-guided aspiration of abscess | Klebsiella pneumonia | Hypertension and type 2 DM present |
| 10. | Clostridium paraputificum septicaemia and liver abscess | Kwon et al. (2018, USA) [15] | 23 y/o; female; right hypochondriac pain, nausea, vomiting, fever, a day after embolisation of adenoma was performed | CECT: embolised adenoma (pre-existing) was replaced with multiple gas pockets | Antibiotics with drainage of the abscess | C. paraputificum | The patient had PCOS and was on OCPs; the patient was diagnosed with a hepatic adenoma 3 months back, and OCPs were discontinued; the adenoma was embolised completely |
| 11. | A complex presentation of an uncommon disease: Gas-forming pyogenic liver abscess complicated by septic pulmonary emboli and muscle abscesses, a case report and review of the literature | Alzibdeh et al. (2023, Qatar) [16] | 46 y/o; man; fever, chills, right hypochondriac discomfort | X-ray: subdiaphragmatic lucency; USG: confirmed X-ray findings; CECT: emphysematous abscess (8 cm) in the right hepatic lobe | Percutaneous abscess drainage with antibiotics | Klebsiella pneumoniae |
AKI: acute kidney injury, APLA: anti-phospholipid antibody, CECT: contrast-enhanced computerised tomography, DM: diabetes mellitus, SLE: systemic lupus erythematosus, USG: ultrasonography, y/o: year old
Conclusions
A combination of clinical and radiological examinations is required for a precise diagnosis of emphysematous liver abscess. Gas under the diaphragm without signs of peritonitis should be evaluated thoroughly for other differential diagnoses. Prompt external drainage of the abscess cavity with strict glycemic control is necessary.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Nil.
References
- 1.Smith RS. Pyogenic liver abscess in the aged. Am J Surg. 1944;63:206–13. [Google Scholar]
- 2.Hagiya H, Kuroe Y, Nojima H, Otani S, Sugiyama J, Naito H, et al. Emphysematous liver abscesses complicated by septic pulmonary emboli in patients with diabetes: Two cases. Intern Med. 2013;52:141–5. doi: 10.2169/internalmedicine.52.8737. [DOI] [PubMed] [Google Scholar]
- 3.Lee HL, Lee HC, Guo HR, Ko W-C, Chen K-W. Clinical significance and mechanism of gas formation of pyogenic liver abscess due to Klebsiella pneumoniae . J Clin Microbiol. 2004;42:2783–5. doi: 10.1128/JCM.42.6.2783-2785.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee CJ, Han SY, Lee SW, Baek YH, Choi SR, Roh MH, et al. Clinical features of gas-forming liver abscesses: Comparison between diabetic and nondiabetic patients. Korean J Hepatol. 2010;16:131–8. doi: 10.3350/kjhep.2010.16.2.131. [DOI] [PubMed] [Google Scholar]
- 5.Chou FF, Sheen-Chen SM, Chen YS, Lee TY. The comparison of clinical course and results of treatment between gas-forming and non-gas-forming pyogenic liver abscess. Arch Surg. 1995;130:401–5. doi: 10.1001/archsurg.1995.01430040063012. [DOI] [PubMed] [Google Scholar]
- 6.Takano Y, Hayashi M, Niiya F, Nakanishi T, Hanamura S, Asonuma K, et al. Life-threatening emphysematous liver abscess associated with poorly controlled diabetes mellitus: A case report. BMC Res Notes. 2017;10:117. doi: 10.1186/s13104-017-2445-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tominaga R, Kashiura M, Hatano H, Moriya T. Emphysematous liver abscess with Edwardsiella tarda infection. IDCases. 2022;29:e01543. doi: 10.1016/j.idcr.2022.e01543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nayak AR, Ramadoss R, Ramanathan V, Honnarudraiah NK. Emphysematous liver abscess and disseminated hypervirulent Klebsiella pneumoniae infection in a patient from Southern India. Indian J Crit Care Med. 2022;26:381–3. doi: 10.5005/jp-journals-10071-24131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai YC, Kung WC, Huang CW. An easily neglected rapid progressive emphysematous liver abscess. ACG Case Rep J. 2021;8:e00631. doi: 10.14309/crj.0000000000000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang JQ, He CC, Yuan B, Liu R, Qi YJ, Wang ZX, et al. Fatal systemic emphysematous infection caused by Klebsiella pneumoniae: A case report. World J Clin Cases. 2022;10:2610–5. doi: 10.12998/wjcc.v10.i8.2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bakhshi GD, Singh G, Shah J, Pawar D, Ram S, Raut N. Ruptured emphysematous liver abscess: An unusual presentation in Kochs. Clin Pract. 2021;11:200–4. doi: 10.3390/clinpract11020029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsu CC, Lee WJ. Emphysematous liver abscess in a 58-year-old woman. Can Med Assoc J. 2018;190:E1111. doi: 10.1503/cmaj.180267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee YH, Yu GS, Tsai KC, Huang CY. Emphysematous liver abscess mimicking a gastric bubble. J Acute Med. 2019;9:198–9. doi: 10.6705/j.jacme.201912_9(4).0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maliyakkal A, Naushad VA, Al Mokdad OI, Hanana F, Basheer SM, Palaki JA. Gas under diaphragm: A rare case of ruptured liver abscess with gas forming organism. Cureus. 2022;14:e21672. doi: 10.7759/cureus.21672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwon YK, Cheema FA, Maneckshana BT, Rochon C, Sheiner PA. Clostridium paraputrificum septicemia and liver abscess. World J Hepatol. 2018;10:388–95. doi: 10.4254/wjh.v10.i3.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alzibdeh AH, Alamami AA, Adam M, Almaslamani M, Hadi HA. A complex presentation of an uncommon disease: Gas-forming pyogenic liver abscess complicated by septic pulmonary emboli and muscle abscesses, a case report and review of the literature. IDCases. 2022;31:e01673. doi: 10.1016/j.idcr.2022.e01673. [DOI] [PMC free article] [PubMed] [Google Scholar]


