Abstract
Background
Although multidisciplinary congestive heart failure clinics in the United States appear to be effective in reducing the number of hospital readmissions, it is unclear whether the same benefit is seen in countries such as Canada, where access to both general and specialized medical care is free and unrestricted. We sought to determine the impact of care at a multidisciplinary specialized outpatient congestive heart failure clinic compared with standard care.
Methods
We randomly assigned 230 eligible patients who had experienced an acute episode of congestive heart failure to standard care (n = 115) or follow-up at a multidisciplinary specialized heart failure outpatient clinic (n = 115). The intervention consisted of a structured outpatient clinic environment with complete access to cardiologists and allied health professionals. The primary outcomes were all-cause hospital admission rates and total number of days in hospital at 6 months. The secondary outcomes were total number of emergency department visits, quality of life and total mortality.
Results
At 6 months, fewer patients in the intervention group had required readmission to hospital than patients in the control group (45 [39%] v. 66 [57%], crude hazard ratio [HR] 0.59, 95% confidence interval [CI] 0.38–0.92. Patients in the intervention group stayed in hospital for 514 days compared with 815 days required by patients in the control group (adjusted HR 0.56, 95% CI 0.35–0.89). The number of patients seen in the emergency department and the total number of emergency department visits were similar in the intervention and control groups. At 6 months, quality of life, which was self-assessed using the Minnesota Living with Heart Failure questionnaire, was unchanged in the control group but improved in the intervention group (p < 0.001). No difference in mortality was observed, with 19 deaths in the control group and 12 in the intervention group (HR 0.61, 95% CI 0.24–1.54).
Interpretation
Compared with usual care, care at a multidisciplinary specialized congestive heart failure outpatient clinic reduced the number of hospital readmissions and hospital days and improved quality of life. When our results are integrated with those from other, similar trials, multidisciplinary disease management strategies for congestive heart failure are associated with clinically worthwhile improvements in survival.
Despite effective pharmacologic regimens,1,2 congestive heart failure remains a common and debilitating illness that has marked deleterious consequences for both the patient3 and the health care system.4 The results of a recent systematic review show that multidisciplinary strategies for congestive heart failure are associated with a reduction in hospital admissions caused by heart failure.5 However, it is still unclear which of several possible formats of multidisciplinary strategies provide the largest health benefits, whether multidisciplinary strategies are associated with meaningful reductions in mortality and whether multidisciplinary clinics are required in a country like Canada, where access to both general and specialized medical care is, at least in theory, unlimited. We therefore sought to compare the impact of care at a multidisciplinary specialized congestive heart failure clinic with that of standard care on outcomes in outpatients with congestive heart failure.
Methods
Between January 1998 and January 2000, we recruited patients seen at the emergency department of or admitted to the Montreal Heart Institute with a primary diagnosis of congestive heart failure. The diagnosis required the presence of both signs (at least 1 of tachycardia, gallop rhythm, increased jugular venous pressure [> 10 cm] or pulmonary crackles) and symptoms (at least 1 of dyspnea at rest or minimal effort, paroxysmal nocturnal dyspnea or orthopnea). Patients also had either radiologic confirmation of their congestive heart failure or a known impaired left ventricular ejection fraction (< 45%). Echocardiography was conducted to document left ventricle function if it had not been performed within the previous 6 months. At discharge, all consecutive eligible patients were approached to participate in the study. In order to maximize the generalizability of the results, exclusion criteria were kept to a minimum: a primary diagnosis of acute myocardial infarction, discharge to a chronic care facility, scheduled cardiac surgery, unwillingness to sign informed consent or to attend the outpatient clinic, participation in another research trial, or residence in an outlying area. Eligible patients who agreed to participate were randomly assigned to the control group or intervention group using consecutively numbered opaque envelopes that contained a random number generating group assignment. Patients assigned to the control group received their baseline evaluation at the time of randomization, and they then received treatment and appropriate follow-up according to the standards of the attending physicians (all staff cardiologists of the same university hospital) but without further direct contact with the research team or the planned intervention.
Patients in the intervention group were referred to a multidisciplinary specialized heart failure outpatient clinic at the Montreal Heart Institute, where they were evaluated by the study team within 2 weeks of hospital discharge. Baseline evaluation included a patient history and physical examination performed by a cardiologist specialized in the management of heart failure. Particular attention was paid to possible remediable exacerbating factors.
The heart failure clinic provided rapid access to expert health care professionals (cardiologists, clinician nurses, dieticians and pharmacists, with access to social workers and other medical specialists as required). At the clinic, the patient could be evaluated both clinically and paraclinically, receive intravenous diuretics if required and be observed for up to 5 hours. Additional to these services, a nurse telephoned all patients in the intervention group within 72 hours of hospital discharge and then monthly, unless a problem occurred that required more frequent contact. During the telephone consultation, the nurse pursued problems as clinically indicated.
After the baseline evaluation, the clinic cardiologists individualized a treatment plan for each patient in the intervention group. Pharmacologic treatment was designed using clinical experience and evidence-based guidelines current at the time of the study. Initiation and titration of angiotensin-converting-enzyme inhibitors, β-blockers and spironolactone were individualized to reach the maximally tolerated dose. Diuretics were titrated according to the patient's response.
One-on-one education of the patient, family members or both with the study nurse was initiated at the first clinic visit. Patient education included an explanation of the disease process, the symptoms and signs of heart failure (including changes in symptoms indicative of worsening heart failure), fluid and sodium intake restrictions, the importance of daily monitoring of body weight and action plans to remedy changes in weight, effects of medications and the importance of compliance, and recommendations regarding exercise and diet. The advice given was individualized and complimented with a patient diary for daily weight measurement, medication record, clinical notes and appointments, physical activity recommendations, an education booklet produced inhouse (“Living with Heart Failure”) and a telephone number to contact the clinic during business hours. This individualized program of patient education was reinforced at each subsequent clinic visit.
Also at baseline, a registered dietician performed individualized dietary assessments, and the study nurse reinforced the dietary instructions at subsequent visits. In addition, an analysis of medications taken by the patient (including over-the-counter drugs) and possible interactions was done by a hospital pharmacist with specific recommendations to eliminate unnecessary medications and simplify the overall regimen. The patient's knowledge of prescribed agents was also assessed.
A follow-up plan was developed for each patient that included monthly visits with both a cardiologist and nurse at the clinic. The study team was available for ad hoc consultation during normal working hours. At times of worsening symptoms, patients were advised to call the clinic nurse. During these telephone calls, patients were evaluated for any signs of clinical deterioration or adverse effects of prescribed medication; those requiring medical assessment were immediately scheduled to see 1 of the clinic cardiologists, usually on the same day. No explicit criteria for readmission to hospital were prespecified, and the decision to request readmission rested with the cardiologist. If admission was not required, then follow-up was scheduled, as needed, at the clinic. Noncardiac medical problems were managed by primary care physicians outside of the specialized heart failure clinic.
Most visits occurred at the clinic, but occasionally they took place at the patient's home. The intervention continued for 6 months. No assistance with travel costs or other incentives were provided for the patients in the intervention group.
The institution's ethics review board approved the study, and written informed consent was obtained from all patients.
The primary hypothesis was that patients randomly selected to receive care from the multidisciplinary clinic would have lower all-cause hospital readmission rates and shorter hospital stays over a 6-month follow-up period than those assigned to usual care. We selected all-cause hospital readmission rates since it is at least theoretically possible that the increased surveillance of the intervention program might reduce the number of hospital admissions caused by congestive heart failure but increase the rates of hospital admissions for other causes. Consequently, the primary endpoints were all-cause hospital readmissions and the total number of associated hospital days. The secondary outcomes measured were the number of emergency department visits, quality of life and mortality.
The number of all outpatient medical visits and hospital admissions were obtained through the Quebec government's administrative databases, which cover all Quebec residents.
Blinded personnel administered the quality-of-life questionnaire to both groups at baseline and at 6 months using the Minnesota Living with Heart Failure questionnaire,6 in which the best total score is 0 and the worst total score is 105.
Assuming that the rate of repeat hospital admissions at 6 months would be 40% and that our intervention would reduce this rate to 20%, we calculated that 107 patients would be needed for each group (α = 0.05, β = 0.20). To allow for potential loss to follow-up and hospital admission rates slightly lower than those predicted, we elected to recruit a total of 230 patients.
All analyses were based on the intention-to-treat principle. Univariate analysis of numeric and categoric variables used t tests and χ2 tests respectively. The number of repeat emergency department visits and hospital admissions were analyzed assuming a Poisson distribution. Time to first clinical event as a function of study group assignment was assessed using the Kaplan–Meier method7 with statistical significance determined by the log-rank test.8 The univariate association of baseline characteristics with clinical events was studied by the same technique, and promising variables (p < 0.20) were entered in a multivariate Cox proportional hazards model to determine the adjusted risks of repeat hospital admission and mortality. All statistical tests were 2-sided.
Results
We recruited 230 patients and randomly assigned 115 into each treatment arm (Fig. 1). There were no losses to follow-up over the study period. The average age of the study participants was 69 years, and 72% were men (Table 1). Coronary artery disease was the primary underlying cause of congestive heart failure, with 50% having experienced myocardial infarction. By study protocol, the population had symptomatically severe heart failure, with 90% of the patients being in the New York Heart Association class III or IV and having radiologic evidence of acute cardiac decompensation at the time of randomization. The average ejection fraction was 35%. There were no differences between the groups in the number of emergency department visits (78%) or hospital admissions (62%) in the 12 months preceding randomization. There was no significant difference in baseline characteristics between the 2 groups.

Fig. 1: Patient recruitment and follow-up.
Table 1

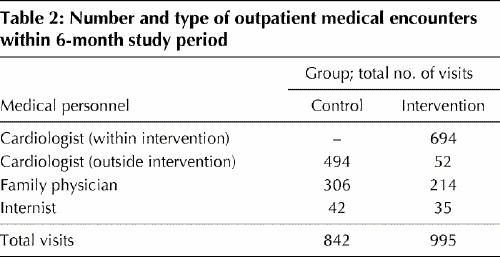
Patients in the intervention group had their first clinic visit a median of 10 days after randomization. The intervention group had a total of 694 visits to the clinic (average 6 per patient, range 0–15) within the 6-month study period. Table 2 shows the number of all medical encounters for both groups. Importantly, the control group also had excellent access to medical, including specialist, care.
Table 2
At 6 months, fewer patients in the intervention group had required readmission to hospital than patients in the control group (45 [39%] v. 66 [57%], crude hazard ratio [HR] 0.59, 95% confidence interval [CI] 0.38–0.92) (Table 3. Patients in the intervention group stayed in hospital for 514 days compared with 815 days required by patients in the control group (adjusted HR 0.56, 95% CI 0.35–0.89). Multivariate baseline predictors of repeat hospital admission included creatinine level (HR 1.04, 95% CI 1.00–1.09 for each 10 μmol/l increase) and diastolic blood pressure (HR 1.28, 95% CI 1.08–1.42 for each 10 mm Hg decrease). After adjustment for these and all other baseline variables reported in Table 1, assignment to the intervention group remained a significant independent predictor of reduced repeat hospital admission in the multivariate analysis (adjusted HR 0.55, 95% CI 0.35–0.88) (Fig. 2).
Table 3
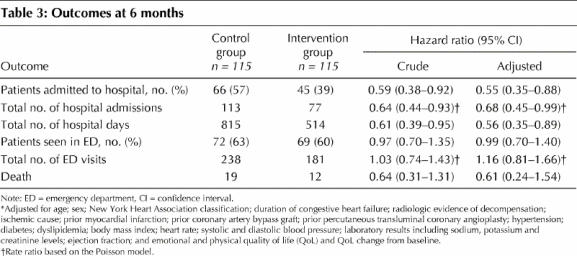

Fig. 2: Survival probability for repeat hospital admissions for the control group and the intervention group (p = 0.0035, log-rank test).
There were no differences at 6 months in the number of patients seen in the emergency department (72 [63%] patients in the control group v. 69 [60%] in the intervention group [HR 0.99, 95% CI 0.70–1.40]), and no difference in the number of deaths (19 in the control group v. 12 in the intervention group [HR 0.61, 95% CI 0.24–1.54]). Quality of life as measured by the Minnesota Living with Heart Failure questionnaire was similar in the 2 groups at baseline (Table 1). At 6-month follow-up, there was substantial improvement in both the emotional and physical quality-of-life scores in the intervention group compared with the control group (p < 0.001).
Interpretation
Patients randomly assigned to care at the specialized heart failure clinic had a meaningful and statistically signifiant reduction in the number of repeat hospital admissions and hospital days. Self-assessed quality of life was improved compared with those receiving standard care. Although there were fewer deaths in the intervention group, this trial was underpowered to demonstrate a difference in mortality.
Several aspects of our study deserve special attention. We included all heart failure patients and did not systematically select subgroups of congestive heart failure patients with either low or high risks of hospital readmission. The study population reflected that found in routine inhospital practice, with an older average age and more renal failure than that observed in populations involved in many other randomized trials. Our intervention was truly multidisciplinary, and included follow-up visits with both nurses and cardiologists with special interest in heart failure management. The cardiovascular physicians played a dominant role and were continuously available during regular clinic hours to modify therapy as required. Moreover, patients in the control group had a well-defined treatment plan including planned follow-up with a primary care physician and often involving outpatient visits at our university hospital with a cardiologist not involved in the present study. Our findings show that the benefits of follow-up in a specialized heart failure clinic exist even when compared with patients with good access to medical follow-up.
In a 2004 meta-analysis of 29 trials using multidisciplinary strategies of treatment for heart failure patients,5 7 studies were identified as using strategies that involved follow-up by a specialized multidisciplinary team in a clinic setting.9,10,11,12,13,14,15 Among this homogenous group of studies, the all-cause hospital admission rates were decreased in the intervention group (risk ratio [RR] 0.76, 95% CI 0.58–1.01); when our study results are included, this reduction attains statistical significance (RR 0.73, 95% CI 0.56–0.96). The reduction in rates of death was not statistically significant in the original meta-analysis (RR 0.66, 95% CI 0.42–1.05), but it becomes significant when our study results are included (RR 0.67, 95% CI 0.45–0.99). Moreover, in 1 of these 7 studies, 50% of the deaths in the intervention arm occurred before the patients were evaluated in the clinic.10 When this trial is excluded and ours is included, a revised meta-analysis calculated using a random effects model demonstrates a more pronounced reduction (RR 0.60, 95% CI 0.39–0.91) (Table 4).
Table 4

To fully appreciate the potential health advantages of a multidisciplinary congestive heart failure clinic, it is helpful to express the benefits not only in relative but also in absolute terms. From the revised meta-analysis of the studies in Table 4, the benefits of these intensive disease management programs involving 1255 heart failure patients include a substantial impact in reducing hospital admissions and mortality: the number needed to treat to prevent 1 hospital admission would be 9 (95% CI 5–25) and to prevent 1 death would be 15 (95% CI 9–33).
Our study had a number of limitations. Although we attempted to systematically record all end points for both groups, the increased contact of the intervention group with the recruiting centre may have led to a detection bias. Similarly, the less intense follow-up of the control group may have led to an ascertainment bias. This is nevertheless unlikely, since the majority of the patients in the control group always returned to the recruiting centre, which is a highly regarded tertiary cardiology centre. Moreover, the medical records of both groups were systematically reviewed. Indeed, if these biases did exist, they would both be expected to bias results toward the null and thereby lead to an underestimate of the true benefit. It is also possible that incomplete blinding of the data extractors may have introduced another bias. To minimize the potential impact of such a bias, we selected outcomes (repeat hospital admission and duration of hospital stay) that are not typically affected by subjective interpretations. The unblinding of the study physicians is also unlikely to have influenced hospital admission patterns since the physicians represent fewer than 10% of the cardiologists with admission privileges at the institution.
In conclusion, we have demonstrated that care at a specialized multidisciplinary clinic for patients with congestive heart failure can lead to significant reductions in patient morbidity, as measured by fewer hospital admissions, shorter hospital stays and improved quality of life. When our results are integrated with those from other, similar trials, multidisciplinary disease management strategies for congestive heart failure are associated with clinically worthwhile improvements in survival. Future work should focus on defining the patient population that is most likely to realize these benefits and on optimizing the type and duration of the intervention.
β See related article page 53
Acknowledgments
We are most appreciative of the excellent nursing care supplied by the heart failure clinic staff. We also thank the hospital administration and unrestricted educational grants from Merck Frosst and GlaxoSmithKline that contributed to making this specialty clinic a reality.
Footnotes
This article has been peer reviewed.
Contributors: Jean Rouleau, James Brophy, Odette Doyon and Michel White were responsible for the conception and design of the study. Jean Rouleau, Odette Doyon and Anique Ducharme were responsible for the collection and assembly of data. James Brophy was responsible for the analysis and interpretation of data. Anique Ducharme and James Brophy drafted the article. All of the authors were responsible for critical revisions, important intellectual content and final approval of the article.
James Brophy and Michel White receive support from les Fonds de la recherche en santé du Québec.
Competing interests: None declared.
Correspondence to: Dr. James Brophy, Cardiology Service Room M4.76, McGill University Health Centre, Royal Victoria Hospital, 687 Pine St. West, Montréal QC H3A 1A1; fax 514 843-1493; james.brophy@mcgill.ca
References
- 1.Garg R, Yusuf S; for the Collaborative Group on ACE Inhibitor Trials. Overview of randomized trials of angiotensin-converting-enzyme inhibitors on mortality and morbidity in patients with heart failure. JAMA 1995;273:1450-6. [PubMed]
- 2.Brophy JM, Joseph L, Rouleau JL. Beta-blockers in congestive heart failure. A Bayesian meta-analysis. Ann Intern Med 2001;134:550-60. [DOI] [PubMed]
- 3.Brophy JM, Deslauriers G, Boucher B, Rouleau JL. The hospital course and short term prognosis of patients presenting to the emergency room with decompensated congestive heart failure. Can J Cardiol 1993;9(3):219-24. [PubMed]
- 4.Rich MW. Management of heart failure in the elderly. Heart Fail Rev 2002;7:89-97. [DOI] [PubMed]
- 5.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: A systematic review of randomized trials. J Am Coll Cardiol 2004;44(4):810-9. [DOI] [PubMed]
- 6.Rector T, Kubo SH, Cohn JN. Patient's self-assessment of their congestive heart failure. Heart Failure 1987;3:198-209.
- 7.Kaplan KL, Meier P. Non-parametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457-81.
- 8.Kalbfleisch JB, Prentice PL. The statistical analysis of failure time data. New York: John Wiley and Sons; 1980.
- 9.Cline CMJ, Israelsson BYA, Willenheimer RB, Broms K, Erhardt LR. Cost effective management programme for heart failure reduces hospitalisation. Heart 1998;80(5):442-6. [DOI] [PMC free article] [PubMed]
- 10.Ekman I, Andersson B, Ehnfors M, Matejka G, Persson B, Fagerberg B. Feasibility of a nurse-monitored, outpatient-care programme for elderly patients with moderate-to-severe, chronic heart failure. Eur Heart J 1998;19:1254-60. [DOI] [PubMed]
- 11.Doughty RN, Wright SP, Pearl A, Walsh HJ, Muncaster S, Whalley GA, et al. Randomized, controlled trial of integrated heart failure management. The Auckland Heart Failure Management Study. Eur Heart J 2002;23(2):139-46. [DOI] [PubMed]
- 12.Kasper EK, Gerstenblith G, Hefter G, Van Anden E, Brinker JA, Thiemann DR, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol 2002;39:471-80. [DOI] [PubMed]
- 13.Capomolla S, Febo O, Ceresa M, Caporotondi A, Guazzotti G, La Rovere MT, et al. Cost/utility ratio in chronic heart failure: comparison between heart failure management program delivered by day-hospital and usual care. J Am Coll Cardiol 2002;40:1259-66. [DOI] [PubMed]
- 14.Stromberg A, Martensson J, Fridlund B, Levin LA, Karlsson JE, Dahlstrom U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective, randomised trial. Eur Heart J 2003;24:1014-23. [DOI] [PubMed]
- 15.Ledwidge M, Barry M, Cahill J, Ryan E, Maurer B, Ryder M, et al. Is multidisciplinary care of heart failure cost-beneficial when combined with optimal medical care? Eur J Heart Fail 2003;5:381-9. [DOI] [PubMed]


