Abstract
Axillary breasts are a common entity with a reported incidence of 2 to 6% in women and 1 to 3% in men. They are more common amongst Asians than Caucasians, namely amongst South East Asians and Indians, with the highest incidence amongst Japanese. While modalities like CoolScupting™, Kybella™ injections, and BodyTite™ have been used by surgeons for management of axillary breasts, the most effective treatment for this condition remains surgical management involving a combination of liposuction of the axillary breast with excision of the gland and skin. In the author's experience, primary skin excision always leaves a long visible scar that widens over time, at times leading to contractures and restricted axillary movements even when closure looks tension free on the table. Any skin excess is best dealt with secondarily. The author uses a modified protocol without any primary skin excision in axillary breast management to achieve excellent results with minimal scars.
Keywords: axillary breast, accessory breast, axilla, breast, liposuction, excision
Introduction
Axillary breasts are common among Indian women, with an incidence of 2 to 6%. 1 2 The treatment for axillary breasts involves a combination of liposuction with gland and skin excision. The author, however, finds primary skin excision unnecessary in most cases except when the nipple–areola complex is present in axillary breasts and needs excision for aesthetic reasons. Not only does primary skin excision leave long, visible scars but excess skin excision can also restrict axillary movements, resulting in wide stretched-out scars, contractures, and aesthetically suboptimal results. The author describes her technique for class 4 Kajava axillary breasts ( mamma aberrata ) in this article.
Materials and Methods
Twelve women with class 4 Kajava axillary breasts underwent surgery according to the author's protocol between January 2016 and September 2023. Ten women presented with bilateral axillary breasts, while two presented with unilateral axillary breasts.
Author's Protocol
All the patients were managed with a combination of liposuction and gland excision without excising any skin primarily. Detailed counseling of the patients was done preoperatively to discuss complications like nerve injuries, numbness, wound healing problems, and residual gland/skin. They were explained that excess skin after liposuction and gland excision would not be excised primarily and it would be allowed to drape over the axillary hollow created by fat and gland removal ( Fig. 1 ). They were counseled that this excess skin was expected to retract and settle on its own over 6 to 12 months after surgery and that residual skin if any at 1 year would be excised with a smaller incision to result in a finer, smaller scar than can be achieved primarily. They were explained the long-term benefits of leaving this excess skin in terms of inconspicuous scars, no restriction of axillary movements, and no chances of developing any contracture. All the patients were followed up for at least 1 year. The longest follow-up was at 2.5 years.
Fig. 1.
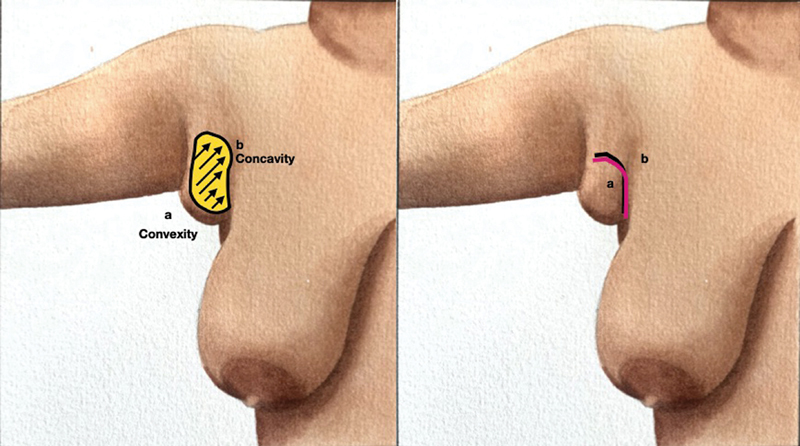
Logic behind the author's protocol: The yellow area marked illustrates the area of liposuction and breast gland excision. Line a represents the inner surface of skin excess presenting as a convexity. Line b represents the hollow/concavity created after liposuction. Skin excess of a lines the hollow b after liposuction and gland excision is done.
The Logic Behind the Modified Protocol
An axilla is a hollow concave space in normal healthy individuals that exhibits various degrees of skin laxity during its range of motion from adduction to complete shoulder abduction. In the case of axillary breasts, the excess tissue bulge presents as a convexity. After fat liposuction and breast gland excision, the hollow of the axilla is restored. The excess loose skin present immediately thereafter is needed to line the concavity of the axilla as illustrated in Fig. 1 . While it may appear as excess on the operation table, the skin is just sufficient to line the axilla without tension in complete abduction once wound healing is complete.
Markings and Surgical Protocol
The anterior and posterior axillary lines along with the area of the axillary breasts projecting onto the chest/paramammary area are marked with the patient standing in a normal anatomical position ( Figs. 2 3 4 ).
Fig. 2.
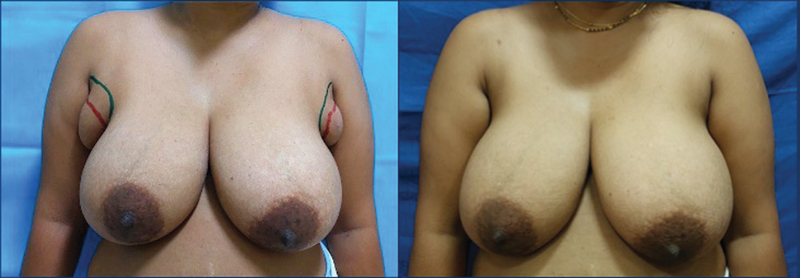
Patient 1 with large axillary breasts. Frontal view preoperatively and at 8 months postoperatively.
Fig. 3.

Patient 1 with large axillary breasts. Right lateral oblique view preoperatively and at 8 months postoperatively.
Fig. 4.

Patient 1 with large axillary breasts. Oblique view preoperatively and at 8 months postoperatively.
The patient is then asked to abduct the arm to mark the axillary breasts. The incision for the residual gland excision is marked at the most prominent region of the axillary breast in the natural skin crease to lie between the anterior and posterior axillary lines. The liposuction stab incisions are also planned within the confines of the anterior and posterior axillary lines.
The author used a combination of power-assisted liposuction (MicroAire™) using a 3-mm cannula and gland excision using a small incision without any primary skin excision.
First, a thorough liposuction was performed with the arm in abduction, leaving behind a skin thickness fold of around 1.0 to 1.5 cm depending on the preexisting skin quality of the patient. Then, using a single 2.5- to 4-cm incision marked on the most prominent region of the axillary breast in natural skin crease, the remaining gland and any visible areas of excess fat that may result in contour irregularities were carefully excised under vision. A uniform thin layer of fat was kept intact under the dermis of the skin flaps raised for gland excision to achieve a smooth contour. Incisions were closed using Monocryl 5–0 CN and Prolene 6–0 CN sutures. No quilting sutures were used to approximate skin over the cavity created after liposuction and gland excision. Drains were used in large axillary breast excisions and removed at 72 hours at first dressing change. The first dressing at the time of surgery was a bulky dressing using tulle with 2% mupirocin as the first layer followed by cover with thin dry gauze pieces. A ball made of small pads and dry gauze was fashioned to match the size of the hollow created to contour the redundant skin to the newly created hollow in the axilla and then covered with another layer of dry gauze pieces. The dressing was then secured with dynaplast. Dressings were changed at an interval of 3 to 4 days and similar dressings as above were done each time. For the first week, only sponge bath was advised. After a week, the patients were instructed to remove their dressings and have a regular bath each time just before coming for their scheduled appointment for dressing. Sutures were removed at 1 week and the contoured pressure dressings were continued for 4 weeks to allow for adequate time for skin redraping. Massages with coconut oil twice a day for 5 minutes alternating with scar modulating creams twice a day were started after 1 month and continued for a year.
All excised breast tissue was sent for histopathological examination. All cases showed breast tissue composed of ducts in fibroadipose stroma. Some case showed secretions within the ducts while periductal edema was present in some cases. Cases with relatively bigger cysts and correlating history of pain in axillary breasts in peri-menstrual period were interpreted as fibrocystic disease of the axillary breasts ( Fig. 5 ). There were no malignant changes in any case in our series.
Fig. 5.
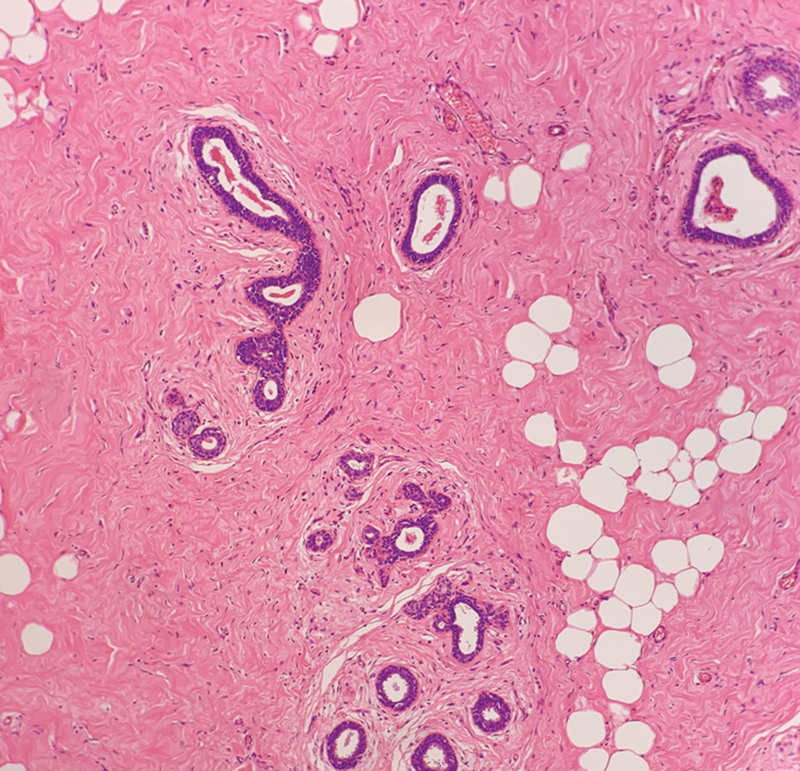
Hematoxylin and Eosin staining of Axillary breast tissue at 40x magnification. Histopathology of axillary breast of Patient 1 showing cystically dilated ducts filled with inspissated secretions, lined by a low cuboidal epithelium. The architecture of the lobules is maintained. The ducts are surrounded by fibroblasts suggestive of fibrocystic changes in the axillary breast tissue.
Results
During the first month after surgery, few patients complained of excess residual skin and edema, four patients complained of loss of sensations on the medial aspect of the arm, and five had minor pain while lifting the arm. Loss of skin sensation was temporary, and all the patients recovered sensations within 3 to 6 months. There were no seromas/hematomas or wound healing complications. In the author's series, all the patients were followed up for at least 1 year and all of them had good skin retraction and none required/requested for skin excision at 1 year. Aesthetically, all the patients showed excellent results at 1 year with inconspicuous scars. No patient had recurrences.
Discussion
Despite being a common entity, axillary breast excision has not received much attention of the plastic surgeons. There are very few studies published about their management protocol globally. Bhave 3 suggests open excision of the gland and skin with an elliptical incision and liposuction to feather the margins of the flap to reduce dog-ears and to contour the axillary folds. Kurtzman et al 1 and Bartsich and Ofodile 4 recommend no skin excision in cases of very small axillary breasts, while they excise skin in all large axillary breasts. However, the author has successfully performed surgeries on patients with even large axillary breasts, categorized as 3 and 4 according to Bartsich and Ofodile's classification, 4 without skin excision, and excellent outcomes were achieved in these patients ( Figs. 2 3 4 and 6 ). In line with principle 16 of Harold Gillies, 5 “Never do today what can honourably[sic] be put off till tomorrow,” the author recommends delaying skin excision for at least 1 year postoperatively until wound healing is complete, scars mature, and skin has draped well over the axilla. This approach allows for addressing any residual skin excess with smaller incisions that result in finer scars. The author has not needed any secondary skin excision to date and her longest follow-up has been 2.5 years. However, larger series with longer follow-ups may be needed to validate the results of this study.
Fig. 6.
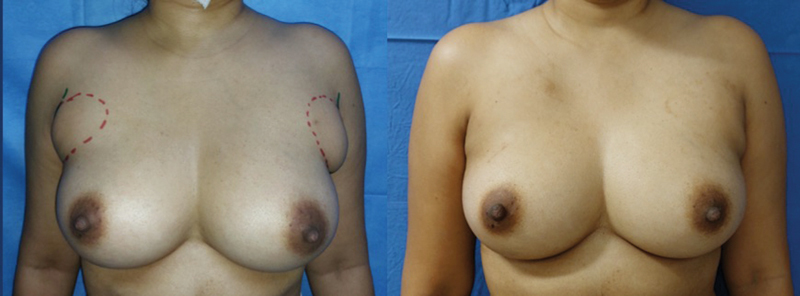
Patient 2 underwent an axillary breast surgery using the author's protocol. Frontal view preoperatively and at 6 months postoperatively.
Conclusion
Axilla is unique in it's extensive range of movements, requiring sufficient skin especially during maximum abduction to prevent any restriction of movements. This must be kept in mind while managing axillary breasts. A combination of liposuction with gland excision through a small incision with no primary skin excision provides excellent aesthetic results with no recurrence and minimal incidence of complications. This is a small series; however, it could be the standard line of treatment for Kajava class 4 axillary breasts. Skin excess, if any, must be dealt with secondarily after a year.
Acknowledgments
The author thanks Dr. Richa Tomar, Consultant Pulmonologist, Gurugram, India, for her watercolor illustration ( Fig. 1 ) and Dr. Kurella Parandhamaiah Suneetha, Senior Consultant Pathologist and Laboratory Director, Manipal Hospital, Hebbal, for sharing the histopathological slide of patient no 1.
Funding Statement
Funding None.
Conflict of Interest None declared.
Note
This paper was presented at ISAPS World Congress 2024 at Cartagena, Colombia, on June 13, 2024.
References
- 1.Kurtzman J S, Pinkasovic E, Preminger B A. Treatment options for the clinical management of axillary breast tissue. Plast Reconstr Surg Glob Open. 2023;11(08):e5189. doi: 10.1097/GOX.0000000000005189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aydogan F, Baghaki S, Celik V et al. Surgical treatment of axillary accessory breasts. Am Surg. 2010;76(03):270–272. [PubMed] [Google Scholar]
- 3.Bhave M A. Axillary breast: navigating uncharted terrain. Indian J Plast Surg. 2015;48(03):283–287. doi: 10.4103/0970-0358.173126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartsich S A, Ofodile F A. Accessory breast tissue in the axilla: classification and treatment. Plast Reconstr Surg. 2011;128(01):35e–36e. doi: 10.1097/PRS.0b013e3182173f95. [DOI] [PubMed] [Google Scholar]
- 5.Pandey S, Chittoria R K, Mohapatra D P, Friji M T, Sivakumar D K. Mnemonics for Gillies principles of plastic surgery and it importance in residency training programme. Indian J Plast Surg. 2017;50(01):114–115. doi: 10.4103/ijps.IJPS_93_16. [DOI] [PMC free article] [PubMed] [Google Scholar]


