Current guidelines on revascularization strategies for patients with acute myocardial infarction are less clear for non–ST‐segment–elevation myocardial infarction (NSTEMI) than ST‐segment–elevation myocardial infarction (STEMI), 1 and Black patients with NSTEMI tend to have longer delays to treatment and lower procedure rates than White patients and patients with STEMI. 2 Furthermore, hospitals serving predominantly Black and Hispanic racially and ethnically segregated communities have the lowest likelihood of adopting percutaneous coronary intervention (PCI) services and the greatest risk of closing services compared with White and integrated communities. 3 Black patients with acute myocardial infarction living in integrated communities experience the greatest improvements in PCI outcomes after a new PCI‐capable facility opens nearby, but it remains unknown whether these benefits extend to patients with NSTEMI. 4 The present study evaluates changes in outcomes for patients with NSTEMI and STEMI after a PCI facility opening nearby, stratified by patient race and community segregation. We hypothesized that patients with NSTEMI and STEMI in all race/segregation categories would experience improved outcomes after a PCI opening nearby, but benefits would be greater for patients with STEMI given heavily protocolized treatment guidelines, and in integrated communities given differences in structural determinants of health and the built environment between integrated and segregated communities.
Because of the sensitive nature of the data collected for this study, requests to access the dataset from qualified researchers trained in human subject confidentiality protocols may be sent to the Centers for Medicare and Medicaid Services at https://www.cms.gov/. This retrospective cohort study used data from Medicare Fee‐for‐Service patients with acute myocardial infarction between 2006 and 2017 whose race was identified as White or Black based on administrative records, as done in prior work. 4 We identified patients diagnosed with NSTEMI versus STEMI and grouped patients into 4 categories based on individual race (Black versus White), and residential segregation (integrated versus segregated), as measured by the Black‐White dissimilarity index of a patient's community. We used each patient's mailing zip code as a proxy for their community and defined racially segregated communities using the White‐Black dissimilarity index, which was constructed at the hospital service area level. Communities with an index value in the top one‐third of the overall dissimilarity index distribution were classified as segregated; all others were classified as integrated. We examined 4 binary outcomes as described in the Figure. We implemented a linear probability model with community fixed effects and adjusted for patient demographics (5‐year age groups, sex, race) and 23 Elixhauser comorbid conditions (complete list in the Figure legend). We also included year dummies to control for time trends that affect all patients. We compared risk‐adjusted percentage point changes in outcomes when a patient experienced a PCI facility opening within a 15‐minute drive relative to a patient from the same race/segregation category who did not experience an opening. The analysis was conducted in Stata 17; a 2‐sided P<0.05 was considered significant. Institutional review board approval was not required because the study did not use identifiable patient data.
Figure 1. Risk‐adjusted percentage point changes in outcomes when there is a PCI facility opening within a 15‐minute driving time.
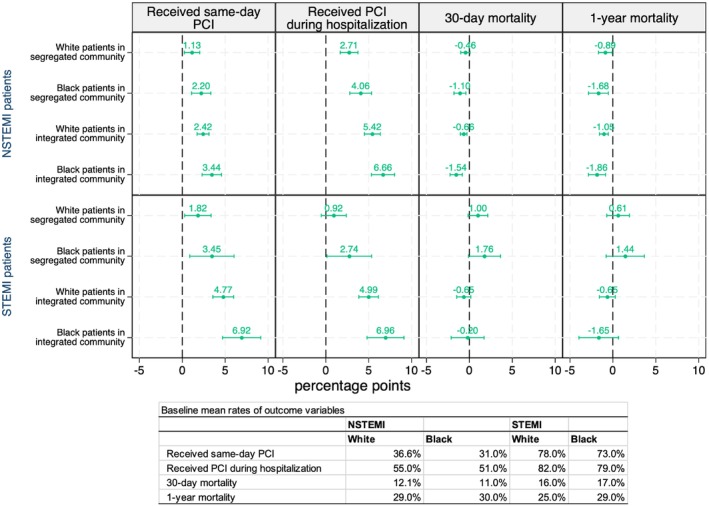
Error bars represent 95% confidence intervals. Community fixed‐effects models are adjusted for patient demographics (5‐year age groups, sex, race) and comorbid conditions (vascular disease, pulmonary disease, diabetes, renal failure, liver disease, cancer, dementia, valvular disease, hypertension, chronic obstructive pulmonary disease, arthritis, coagulopathy, obesity, substance abuse, depression, psychosis, hypothyroidism, paralysis and neurological disorder, ulcer, weight loss, fluid and electrolyte disorder, anemia, stroke) and are controlled for yearly trends. Mortality outcomes are also controlled for access and treatment. Reference groups are patients of the same race and community type who did not experience a PCI facility opening. The total population of patients with AMI is 2 388 180 patients (1 861 732 STEMI and 526 448 NSTEMI). The total population of patients with AMI who experienced a PCI facility opening is 379 668 patients (246 096 in integrated and 133 572 in segregated communities). AMI indicates acute myocardial infarction; NSTEMI, non–ST‐segment–elevation myocardial infarction; PCI, percutaneous coronary intervention; and STEMI, ST‐segment–elevation myocardial infarction.
The Figure reveals risk‐adjusted percentage point (pp) changes in outcomes after a community experienced a PCI‐capable facility opening within a 15‐minute drive, relative to the same community type with no PCI capacity change. Among patients with NSTEMI, Black patients in integrated communities had a 3.44 pp greater risk‐adjusted probability of receiving same‐day PCI and a 6.66 pp greater probability of PCI during hospitalization after a PCI facility opening in their community (compared with no PCI opening in that community). Given the mean rate of 31% and 51% among Black patients with NSTEMI for each outcome, respectively, these changes represent an 11.1% and 13.1% relative increase for Black patients with NSTEMI in integrated communities after a PCI opening. White patients with NSTEMI in integrated communities were also 2.42 pp and 5.42 pp more likely to receive same‐day PCI and PCI during a hospitalization, respectively, after a PCI opening in their community. When looking at NSTEMI mortality, Black patients in integrated communities again showed the most significant improvement (−1.54 pp) in 30‐day mortality after a PCI facility opening, representing a 14.0% overall relative decrease (the mean rate is 11% for this outcome) after a PCI opening nearby.
Among patients with STEMI, Black patients in integrated communities had a 6.92 pp and 6.96 pp greater likelihood of receiving same‐day PCI and PCI during a hospitalization, respectively, after a PCI opening in their community. Of note, Black patients with STEMI had a higher baseline likelihood of receiving PCI than Black patients with NSTEMI (mean rate of 73% for same‐day PCI and 79% for PCI during hospitalization). Therefore, these results represent a 9.5% and 8.8% relative increase, respectively, for the 2 outcomes. Less dramatic but still statistically significant improvements in PCI were also observed for White patients in integrated communities, whereas improvements for Black patients in segregated communities were smaller. No improvements in mortality among patients with STEMI were observed after PCI facility openings. Although Black patients in integrated communities showed the largest improvement (−1.65 pp) in 1‐year mortality after a PCI opening in their community, the standard error was large due to a smaller sample size (compared with patients with NSTEMI).
Overall, Black patients with acute myocardial infarction in integrated communities experienced the greatest improvements in outcomes after a PCI facility opened near their community, with significant benefits for patients with NSTEMI and STEMI. Because of the potential for type I error due to multiple comparisons, our findings should be interpreted as exploratory, and our results should not be construed as causal. Further exploration of potential factors contributing to the smaller benefits observed in segregated communities is warranted, particularly as prior literature has shown that socioeconomic and environmental resources and opportunities differ in segregated versus integrated communities. 5 Taken together, these findings may help promote more equitable resource allocation to improve access to cardiac care and patient outcomes.
Sources of Funding
This project was supported by the Pilot Project Award from the National Bureau of Economic Research Center for Aging and Health Research, funded by a National Institute on Aging grant (P30AG012810); the National Institute on Minority Health and Health Disparities (R01MD017482); and the National Heart, Lung, and Blood Institute (R01HL114822 and R01HL134182). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; or decision to submit the article for publication.
Disclosures
All authors received grants from the National Institute of Aging, the National Institute on Minority Health and Health Disparities, and the National Heart, Lung, and Blood Institute.
Acknowledgments
The authors thank N. Sarkar for analytical support and S. Pandey for her assistance. Dr Shen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This article was sent to Jong‐Ho Park, MD, PhD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 3.
References
- 1. Lawton JS, Tamis‐Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, Bittl JA, Cohen MG, DiMaio JM, Don CW, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022;145:e18–e114. doi: 10.1161/CIR.0000000000001038 [DOI] [PubMed] [Google Scholar]
- 2. Anstey DE, Li S, Thomas L, Wang TY, Wiviott SD. Race and sex differences in management and outcomes of patients after ST‐elevation and non–ST‐elevation myocardial infarct: results from the NCDR. Clin Cardiol. 2016;39:585–595. doi: 10.1002/clc.22570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hsia RY, Shen YC. Structural inequities in the adoption of percutaneous coronary intervention services by US hospitals, 2000–20. Health Aff. 2024;43:1011–1020. doi: 10.1377/hlthaff.2023.01649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hsia RY, Shen YC. Do PCI Facility Openings Differentially Affect AMI Patients by Individual Race and Community Segregation? NBER Working Paper 31626. National Bureau of Economics Research2023. Accessed October 15, 2023. https://www.nber.org/papers/w31626.
- 5. Reddy NM, Mayne SL, Pool LR, Gordon‐Larsen P, Carr JJ, Terry JG, Kershaw KN. Exposure to neighborhood‐level racial residential segregation in young adulthood to midlife and incident subclinical atherosclerosis in black adults: the coronary artery risk development in young adults study. Circ Cardiovasc Qual Outcomes. 2022;15:e007986. doi: 10.1161/CIRCOUTCOMES.121.007986 [DOI] [PMC free article] [PubMed] [Google Scholar]


