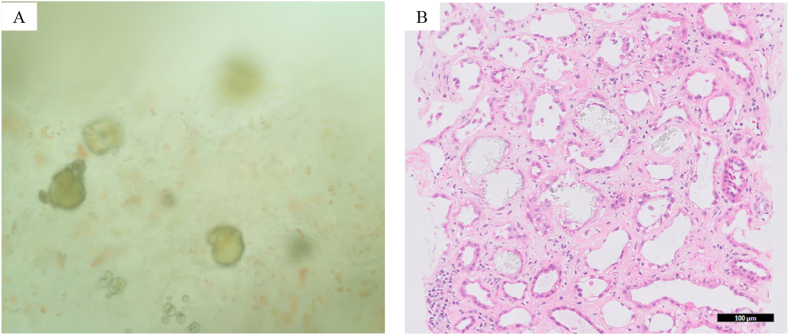
A man in his 70s with a history of total gastrectomy and Roux-en-Y reconstruction 13 years prior presented with increasing malaise and anorexia over the past 6 months. He had a history of hypertension, and his medications included an angiotensin receptor blocker and a calcium channel blocker. He had a serum creatinine level of 3.82 mg/dL (estimated glomerular filtration rate 13 mL/min/1.73 m2) and no edema. Eight months earlier, his kidney function was normal. His urine protein-to-creatinine ratio was 3.5 g/g, with no hematuria on urinalysis. A kidney biopsy revealed round and square crystals under light microscopy before formalin fixation (Fig 1A). After fixation, hematoxylin and eosin staining revealed an acute tubular injury with numerous intratubular calcium oxalate crystals (Fig 1B). The histological diagnosis was oxalate nephropathy. Additionally, a high 24-hour urine oxalate excretion of 59.6 mg/day was observed.
Figure 1.
(A) Kidney biopsy performed before formalin fixation. (B) Hematoxylin and eosin staining.
Diagnosing oxalate nephropathy can be challenging,1 and its prevalence may be underestimated2 despite a poor prognosis.1,2 One reason is that calcium oxalate crystals can be difficult to visualize without polarized light microscopy.3 Oxalate nephropathy can be diagnosed easily with polarized light microscopy. However, it is challenging to suspect oxalate nephropathy without clinical information or confirmation of crystals using kidney biopsy. We visualized crystals using hematoxylin and eosin staining with Carazzi hematoxylin. For further examination, we stained with Carazzi hematoxylin and Mayer’s hematoxylin, both of which allowed observation of the crystals (Fig S1A and S1B). However, crystals were difficult to visualize with Meyer’s stain after periodate treatment (Fig S1C). Although it is unclear why crystals were visible with hematoxylin and eosin staining, these results suggest that crystals may have been dissolved during staining. Furthermore, the contribution to the diagnosis of kidney biopsy is generally enhanced with periodic acid-Schiff and periodic acid-methenamine silver staining, whereas hematoxylin and eosin staining offers relatively lower diagnostic value. This difference may explain why oxalate nephropathy can be missed following kidney biopsy.
When sectioning for immunofluorescence and electron microscopy, kidney specimens are commonly observed using light microscopy before formalin fixation. Our image highlights the importance of actively searching for oxalate crystals before formalin fixation to facilitate an accurate diagnosis.
Article Information
Authors’ Full Names and Academic Degrees
Kenji Yamada, MD, Mari Ikeda, MD, Yoshinori Koyama, MT, Kurumi Seki, MD, Atsuro Kawaji, MD, Tomohiko Inoue, MD, PhD, and Tomo Suzuki, MD, PhD
Support
None.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Patient Protection
The authors declare that they have obtained consent from the patient reported in this article for the publication of information included in this case report and any related supplementary material.
Acknowledgements
We thank the staff of the Department of Nephrology and Pathology of the Kameda Medical Center for their dedicated efforts in caring for these patients.
Peer Review
Received June 17, 2024. Accepted in revised form on October 2, 2024, after editorial review by the Statistics Editor and the Editor-in-Chief.
Footnotes
Complete author and article information provided before references.
Figure S1: Crystal by different hematoxylin stainings.
Supplementary Materials
Figure S1.
References
- 1.Nasr S.H., Valeri A.M., Said S.M., et al. Clinicopathologic characteristics, etiologies, and outcome of secondary oxalate nephropathy. Mayo Clin Proc. 2024;99(4):593–606. doi: 10.1016/j.mayocp.2023.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buysschaert B., Aydin S., Morelle J., et al. Etiologies, clinical features, and outcome of oxalate nephropathy. Kidney Int Rep. 2020;5(9):1503–1509. doi: 10.1016/j.ekir.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fogo A.B., Lusco M.A., Najafian B., et al. AJKD Atlas of renal pathology: oxalosis. Am J Kidney Dis. 2017;69(3):e13–e14. doi: 10.1053/j.ajkd.2017.01.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1.