Abstract
Background
Gigantomastia is a disabling condition characterized by excess breast tissue. Historically, free nipple graft (FNG) has been preferred, prioritizing the nipple-areola complex (NAC) vascularity. The NAC-carrying pedicle technique, which is most commonly used in case of hypertrophy of the breast, has been suggested as a viable alternative for gigantomastia according to recent evidence, with reduced rates of NAC necrosis and improved outcomes. Nevertheless, a detailed outcome evaluation of the technique in terms of sensory preservation is currently lacking. Therefore, this systematic review and meta-analysis aimed to assess the risk of sensory loss associated with the NAC-carrying pedicle technique in cases of gigantomastia.
Methods
Following the PRISMA guidelines, a literature search identified studies reporting postoperative sensitivity with the NAC-carrying pedicle technique in resections exceeding 1000 g of adipo-glandular tissue. Then, a proportion meta-analysis was conducted to assess the pooled rate of sensation loss through the NAC-carrying pedicle technique.
Results
Seventeen studies (843 patients, 1685 breasts) met the inclusion criteria. The meta-analysis revealed an exceptionally low risk of sensory loss with the NAC-carrying pedicle technique (1.3%; 95% confidence interval: 0.7-2.0), without significant statistical heterogeneity.
Conclusion
This study provides the first comprehensive evaluation of sensory preservation with the NAC-carrying pedicle technique in gigantomastia. The NAC-carrying pedicle technique emerges as the first choice, offering safety and favorable functional outcomes. Surgical caution remains crucial with the option to switch to FNG as required, ensuring patient safety and procedure success. Further research on the impact of different NAC-carrying pedicle techniques on sensory preservation is warranted.
Keywords: NAC-carrying pedicle technique, Free nipple graft, Gigantomastia, Meta-analysis, Reduction mammoplasty, Sensation
Introduction
Reduction mammoplasty is a well-established surgical procedure used to reduce breast volume and relieve the symptoms caused by breast hypertrophy.1 Gigantomastia, which is characterized by an even more excessive breast tissue growth, exacerbates physical and psychological discomfort in the patients.2, 3, 4, 5, 6, 7 However, currently there is no universal consensus in the literature concerning the definition of gigantomastia. Dancey et al. defined it as breast hypertrophy requiring resections exceeding 1000 g of tissue per breast.8 Preoperatively, the grams of breast tissue to be removed can be reliably predicted by evaluating the nipple-areola complex (NAC)-lift distance.9 Moreover, there has been considerable debate regarding the ideal reduction mammoplasty technique to limit complications and optimize functional and aesthetic outcomes. Historically, the most commonly used approach was the free nipple graft (FNG). In fact, the primary concern has always been ensuring adequate vascularity to the NAC due to the substantial breast hypertrophy.10,11 However, the NAC-carrying pedicle technique could represent a valid alternative as demonstrated recently.12 If dermoglandular NAC-carrying pedicles are standard in nongigantomastia reduction mammoplasty to treat hypertrophy1,13, the technique of retaining the NAC attached to the dermoglandular pedicle in gigantomastia and/or massive ptosis is far less common.10,11 However, the actual advantage of the NAC-carrying pedicle technique over FNG in gigantomastia in terms of aesthetic and functional outcomes has not yet been systematically assessed. Several studies have highlighted an improvement in aesthetics in terms of breast shape and postoperative pigmentation disorders.13,14 Additionally, the ability to breastfeed postsurgery remains possible among the patients. This opportunity is a noteworthy advantage in contrast to those undergoing FNG.13,15, 16, 17, 18, 19, 20 Finally, another crucial point is NAC sensitivity, which is also completely lost after FNG, resulting in significant psychosocial sequelae for the patients. Interestingly, the rate of sensation loss associated with the NAC-carrying pedicle technique in cases of gigantomastia has not yet been systematically evaluated. Therefore, this study aimed to comprehensively assess sensory preservation in gigantomastia by providing evidence for the preferential use of the NAC-carrying pedicle technique when performing reduction mammoplasty for gigantomastia.
Materials and methods
Review question and search strategy
The systematic review and meta-analysis were conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (http://www.prisma-statement.org). The research question was formulated according to the PICO (population, intervention, comparison, and outcome) framework as follows: “What is the risk of loss of NAC sensation following reduction mammaplasty with NAC-carrying pedicle technique in cases of gigantomastia?”. Subsequently, a comprehensive literature search was conducted in the PubMed/Medline and Cochrane library databases using the following search algorithm: ((breast reduction) OR (mammoplasty) OR (free nipple graft) OR (NAC-carrying pedicle technique)) AND ((gigantomastia) OR (gigantic breast hypertrophy)) NOT (cancer).
The literature search encompassed studies published up to July 2023, and bibliographic references in identified articles were cross-checked for additional relevant publications that were not captured by the initial database search. No language or publication date restrictions were applied. Duplicate records were removed. The authors used a protocol for this systematic review and meta-analysis, but the protocol was not registered in any public database.
Selection criteria
Inclusion and exclusion criteria were established before undertaking the search. Eligibility criteria encompassed articles with original clinical data from reported cases of gigantomastia treated with reduction mammoplasty, where >1000 g of adipo-glandular tissue per breast were removed. To be eligible, the articles needed to report data on the weight of the tissue removed and levels of pre- and postoperative sensitivity. Excluded study types comprised abstracts, letters, editorials, comments, case reports, case series, reviews, and studies involving patients treated solely using FNG.
Two authors (F. B. and C. P.) performed the literature search and study selection independently, yet in a nonblinded way, initially relying on titles and abstracts, and subsequently evaluating the full text in detail to determine the eligibility. In case of discrepancies, a third author (M. DM.) was consulted.
Data extraction
Each included study underwent data extraction by the two authors (F. B. and C. P.), with key investigation points organized in specially designed tables: name of first author, year of publication, country of publication, number of patients included, number of breasts treated, mean age of patients, comorbidities of patients (i.e., diabetes, hypertension, and others), tobacco use, mean body mass index (BMI) of patients (kg/m2), weight of breast tissue resected (g), type of NAC-carrying pedicle used, mean sternal notch-to-nipple distance (cm), mean length of NAC-carrying pedicle (cm), rate of conversion to FNG due to insufficient NAC perfusion during surgery, quality of NAC sensation after surgery (preserved or decreased), and quality assessment of the study.
Quality assessment
Quality assessment of the included articles was performed by two authors (F.B. and E.L.) using the NIH tools (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) and provided a final judgment including three possible options for each article: poor/fair/good quality.
Statistical analyses
Quantitative analysis (meta-analysis) was performed by one author (F.B.) for all the included studies using the OpenMeta[Analyst] software developed by the Center for Evidence Synthesis in Health of Brown University, USA. The cumulative estimated risk of NAC sensory loss associated with the NAC-carrying pedicle technique was assessed as the pooled prevalence through a meta-analysis, along with a 95% confidence interval (95% CI). The analysis considered the number of events as the numerator and number of breasts as the denominator. Those cases in which conversion to FNG had to be performed were not considered when assessing the risk of loss of sensitivity. Statistical pooling of the data was conducted using a random-effects model. Heterogeneity between studies was evaluated using the I2 test, to quantify the percentage of variation attributed to heterogeneity rather than to chance.21,22 An I2 value >50% indicates a significant statistical heterogeneity between the studies. Subgroup analyses were planned in case of I2 value >50% to explore the heterogeneity.
Qualitative analysis (systematic review) included demographic characteristics, comorbidities of the patients, and pre- and intraoperative breast features. If the studies reported a specific value for each breast, the mean value was considered.
Results
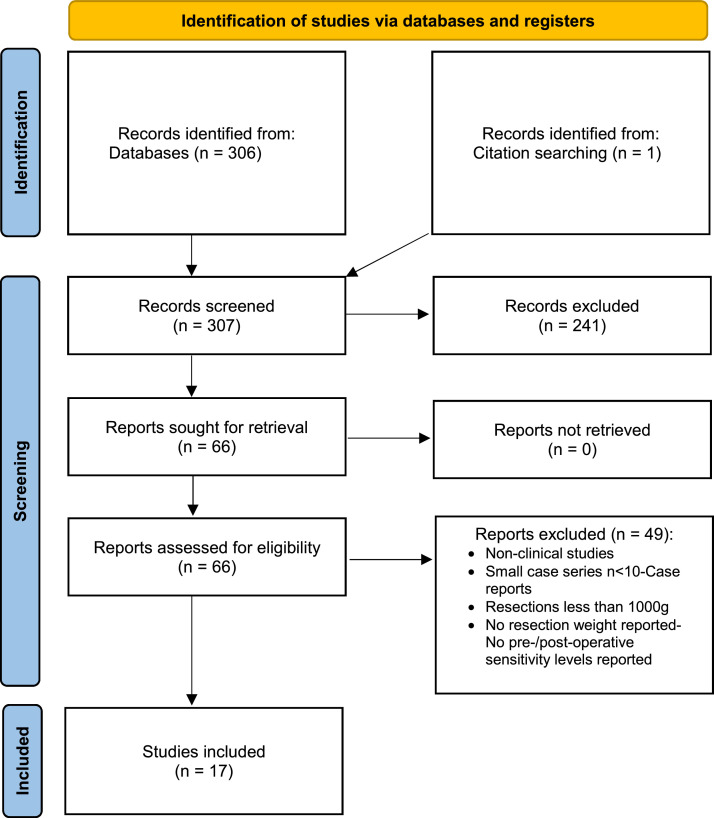
The initial database search in PubMed/Medline and Cochrane Library identified a total of 306 articles published between December 1996 and July 2023. An additional record was identified through a review of the bibliographies of these articles. After title and abstract screening, 66 studies were selected for full-text review. Among these, 49 studies did not meet the inclusion criteria and were not considered. Consequently, 17 articles were included in the analysis, encompassing surgical procedures on 843 patients for a total number of 1685 operated breasts. Details of all the included studies are summarized in Table 1, Table 2, whereas a flowchart of the study selection process is presented in Figure 1.
Table 1.
Summary of all the included studies: patient demographics-comorbidities and preoperative-intraoperative breast characteristics.
| Name of 1st author |
Year of publication | Country | Nr. of patients included | Nr. of breasts treated | Mean age (years) | Diabetes (nr. of patients) | Hypertension (nr. of patients) | Comorbidities other than D/H (nr. of patients) | Tobacco use (nr. of patients) | Mean BMI (kg/m2) | Weight of breast tissue resected (g) | Type of NAC-carrying pedicle | Mean SN-N (cm) | Mean pedicle length (cm) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amini et al.41 | 2010 | Germany | 23 | 46 | 49 | 4 | 6 | 13 | 13 | 33 | 1304 R, 1245 L | SM | 41 R, 41 L | NR |
| Ashour et al.25 | 2018 | Egypt | 40 | 80 | 31 | 4 | NR | NR | NR | 31 | 1690 | SM | 38 R; 38 L | NR |
| Basaran et al.26 | 2011 | Turkey | 16 | 32 | 41 | NR | NR | NR | NR | 32,6 | 1780 L, 1810 R | Based on radiographic analysis | NR | NR |
| Bilgen et al.18 | 2019 | Turkey | 72 | 144 | 41 | 10 | NR | 53 | 8 | 34 | 1640 L, 1586 R | I | NR | NR |
| Bucaria et al.42 | 2018 | Italy | 22 | 44 | 48 | NR | NR | NR | NR | 28 | 1048 | SM | 44 R, 44 L | NR |
| Chang et al. (1)23 | 1996 | USA | 74 | 148 | NR | NR | NR | NR | NR | NR | >1000 | I | 33 | NR |
| Chang et al. (2)23 | 48 | 96 | NR | NR | NR | NR | NR | NR | >2000 | 35 | NR | |||
| Chang et al. (3)23 | 24 | 48 | NR | NR | NR | NR | NR | NR | >3000 | 41 | NR | |||
| Chetty et al.43 | 2016 | South Africa | 31 | 62 | 30 | 0 | 0 | 0 | 0 | 28 | 1835 | SM | 44 | 22 R, 22 L |
| Elmelegy et al.44 | 2017 | Egypt | 25 | 50 | 38 | 0 | 0 | 0 | 0 | 32 | 1434 | ML | 41 | NR |
| Karacaoglu et al.45 | 2016 | Turkey | 26 | 52 | 38 | 2 | 5 | 2 | 12 | 26 | 1513 | IM | 32 | NR |
| Karacor-Altuntas et al.46 | 2016 | Turkey | 53 | 106 | 45 | 9 | 7 | NR | 4 | 40 | 1496 R, 1417 L | C | 44 R, 43 L | NR |
| Kemaloglu et al. (1)47 | 2018 | Turkey | 25 | 50 | 42 | 2 | NR | NR | 1 | 32 | 1320 R+1355 L | I | 33 R+32 L | NR |
| Kemaloglu et al. (2)47 | 25 | 50 | 39 | 3 | NR | NR | 1 | 32 | 1380 R+1310 L | SM | 33 R+34 L | NR | ||
| Lacerna et al.48 | 2005 | USA | 15 | 30 | NR | NR | NR | NR | NR | NR | >2000 | I | NR | NR |
| Letertre et al.49 | 2008 | France | 20 | 40 | 31 | NR | NR | NR | 7 | 32 | 1340 | PS | NR | NR |
| Lugo et al.15 | 2013 | USA | 200 | 400 | 39 | NR | NR | NR | NR | 36 | 1277 R, 1283 L | SM | 36 R, 36 L | 11 R, 11 L |
| Mojallal et al.50 | 2010 | France | 50 | 100 | 33 | 8 | NR | NR | 5 | 27 | 1231 | PS | 38 | NR |
| Nahabedian et al.51 | 2000 | USA | 23 | 45 | 31 | NR | NR | NR | NR | NR | 1604 | ML | 38 R, 39 L | 17 |
| Talwar et al. (1)13 | 2023 | USA | 21 | 42 | 42 | 1 | NR | 2 | 3 | 35 | 1486 | SM | 42 | 9 |
| Talwar et al. (2)13 | 9 | 18 | I | |||||||||||
| Talwar et al. (3)13 | 1 | 2 | S |
Nr., number; D/H, diabetes/hypertension; BMI, body mass index; SN-N, sternal notch-to-nipple distance; R, right; L, left; SM, supero-medial; NR, not reported; I, inferior; ML, medio-lateral; IM, infero-medial; C, central; PS, postero-superior; S, superior.
Table 2.
Summary of all studies included: postoperative sensation and quality assessment.
| Name of 1st author | Conversion to FNG (nr. of breasts) | Sensation preserved (nr. of breasts) | Sensation decreased (nr. of breasts) | Grade of quality |
|---|---|---|---|---|
| Amini et al.41 | 0 | 44 | 2 | Fair |
| Ashour et al.25 | 1 | 73 | 6a | Fair |
| Basaran et al.26 | 0 | 29 | 3 | Fair |
| Bilgen et al.18 | NR | 144 | 0 | Fair |
| Bucaria et al.42 | NR | 44 | 0 | Fair |
| Chang et al. (1)23 | NR | 138 | 10 | Fair |
| Chang et al. (2)23 | NR | 96 | 0 | |
| Chang et al. (3)23 | NR | 48 | 0 | |
| Chetty et al.43 | NR | 59 | 3 | Fair |
| Elmelegy et al.44 | NR | 50 | 0 | Fair |
| Karacaoglu et al.45 | NR | 52 | 0 | Fair |
| Karacor-Altuntas et al.46 | NR | 106 | 0 | Fair |
| Kemaloglu et al. (1)47 | NR | 48 | 2 | Fair |
| Kemaloglu et al. (2)47 | NR | 48 | 2 | |
| Lacerna et al.48 | 0 | 30 | 0 | Fair |
| Letertre et al.49 | NR | 40 | 0 | Fair |
| Lugo et al.15 | NR | 392 | 8 | Fair |
| Mojallal et al.50 | NR | 100 | 0 | Fair |
| Nahabedian et al.51 | 1 | 43 | 1* | Fair |
| Talwar et al. (1)13 | NR | 42 | 0 | Fair |
| Talwar et al. (2)13 | NR | 18 | 0 | |
| Talwar et al. (3)13 | NR | 2 | 0 |
FNG, free nipple graft; nr., number; NR, not reported.
Cases in which conversion to FNG had to be performed were not considered.
Figure 1.
Flow diagram of the search strategy.
Systematic review (qualitative analysis)
Demographic characteristics, comorbidities, and pre- and intraoperative breast characteristics are reported in Table 3, Table 4.
Table 3.
Patient demographics and comorbidities.
| Feature | Results |
|---|---|
| Mean age (years: range) | 39 (30–49) |
| Mean BMI (kg/m2: range) | 33 (26–40) |
| Comorbidities total (%: number of patients out of 843) | 14 (115) |
| • Active smokers | 6 (54) |
| • Diabetes | 5 (43) |
| • Hypertension | 2 (18) |
| • Others | 8 (70) |
BMI, body mass index.
All figures referred represent the percentage and number of concerned patients.
Table 4.
Preoperative and intraoperative breast characteristics.
| Feature | Results |
|---|---|
| Mean preoperative sternal notch-to-nipple distance (cm: range) | 38 (32–44) |
| Mean breast tissue resected (g: range) | 1497 (1048–3066) |
| NAC-carrying pedicle type (%: number of breasts out of 1685) | |
| • Supero-medial | 43% (724) |
| • Inferior | 32% (534) |
| • Postero-superior | 8% (140) |
| • Central | 6% (106) |
| • Medio-lateral | 6% (95) |
| • Infero-medial | 3% (52) |
| • Superior | 0,1% (2) |
| Mean pedicle length (cm: range) | 13 (9–23) |
All figures referred represent the percentage and number of concerned patients.
The evaluation of tissue resection did not include the study by Chang et al.23 and Lacerna et al.23 because they only provided a range for the tissue removed without specifying the precise value. Additionally, the study by Lacerna and colleagues also not considered as it only described the age range for assessing the mean age of patients.24 Similarly, the study conducted by Ashour et al. was not considered in the assessment of the exact pedicle length, as the authors provided only a range of NAC-carrying pedicle lengths.25 In the study by Basaran et al., several types of NAC-carrying pedicles were used, though based on the result of radiographic analysis. Therefore, this article was also excluded from the evaluation of pedicle type.26
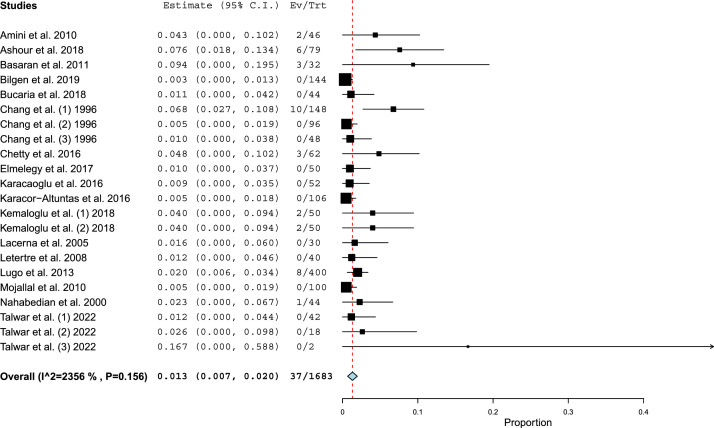
Meta-analysis (Quantitative Analysis)
The analysis of all the included studies revealed that the pooled risk of NAC sensory loss with the NAC-carrying pedicle technique was 1.3% (95% CI: 0.7-2.0) (Figure 2). Statistical analysis indicated an I2 value of 23.56%, demonstrating the absence of a significant statistical heterogeneity in terms of the variable analyzed.
Figure 2.
Forest plot.
Discussion
The surgical management of gigantomastia remains a surgical challenge in the field of plastic surgery. The two possible approaches are the FNG10 and NAC-carrying pedicle technique.1,25 The FNG approach involves the complete removal and subsequent grafting of the NAC as a free full thickness skin graft. Even though this technique facilitates a larger reduction in terms of breast volume, it is associated with potential complications. These encompass suboptimal nipple projection, cessation of breastfeeding, loss of sensation, and hypopigmentation of the nipple graft.13,14,27, 28, 29 The NAC-carrying pedicle technique, in contrast, preserves the NAC by maintaining its continuity with the dermoglandular pedicle, different variants of which are described in the literature. This method has several advantages, including better core projection of the breast, superior projection of the nipple, preserved pigmentation of the NAC, and enhanced potential for NAC sensation.
Critical considerations in reduction mammoplasty for gigantomastia include the preservation of NAC vascularity and postoperative nipple sensation. The viability of the NAC-carrying pedicle technique was questioned due to concerns surrounding NAC perfusion attributed to the length of the NAC-carrying pedicle, potential arterial inflow compromise, and risk of venous congestion.30,31 However, a recent meta-analysis addressed the safety concerns associated with the NAC-carrying pedicle technique, challenging the long-standing belief of a high risk of necrosis in the NAC. The analysis revealed a minimal risk of NAC necrosis, confirming the safety of the NAC-carrying pedicle technique and redefining the indications of reduction mammoplasty for gigantomastia.12 However, surgical caution remains crucial, with the possibility of switching to FNG approach in cases of intraoperative concerns about NAC perfusion, which can be readily assessed during surgery, for example with indocyanine green fluorescence angiography.32, 33, 34
Concerning postoperative sensory preservation, the NAC-carrying pedicle technique has demonstrated a clear advantage compared to FNG. Interestingly, recent studies showed that sensitivity of the breast tissue following the procedure is not correlated with the volume of tissue removed35, 36, 37 but rather depends on the surgical technique employed. Anatomical studies on breast innervation have shown that the latter is supported by the anterior and lateral cutaneous branches of the second through sixth intercostal nerves, and the NAC mainly by anterior and lateral cutaneous branches of the third through fifth intercostal nerves.38,39 Therefore, it is clear that FNG results in complete transection of the sensory fibers for the NAC with a complete loss of sensation. In contrast, the continuity that is guaranteed by the NAC-carrying technique at least partially preserves the nerve fibers, resulting in maintained sensitivity of the NAC. The evidence presented in this study clearly demonstrated that the NAC-carrying pedicle technique is associated with a remarkably low estimated risk of NAC sensory loss, confirming its functional benefits over FNG. For this reason, considering the aforementioned and present meta-analysis, the NAC-carrying pedicle technique can be confidently recommended as a superior choice for reduction mammoplasty in case of gigantomastia.
Furthermore, to minimize the loss of sensitivity, it is necessary to mention some considerations regarding the different available NAC-carrying pedicles. Based on the anatomy and in analogy with the data described for hypertrophy40, it can be speculated that different NAC-carrying pedicles may affect sensitivity preservation differently. In particular, in case of superior and superolateral pedicles, the risk of decreased sensitivity appears to be higher. Indeed, the injury of the lateral and medial cutaneous branches of the fourth intercostal nerve can likely occur during mammoplasty with superior NAC-carrying pedicles. Simultaneously, the supero-lateral NAC-carrying pedicles lead to a transection of the anterior cutaneous branches of the third, fourth, and fifth intercostal nerves and can interrupt the lateral cutaneous branch of the fourth intercostal nerve. However, sensory preservation would be higher with the other NAC-carrying pedicle techniques, such as supero-medial, inferior, or septum-based NAC-carrying pedicles.40 For this reason, further studies to evaluate this possible correlation with different NAC-carrying pedicle techniques would maximize the efficacy of this surgical approach.
Despite the interesting findings of this study, a major limitation must be mentioned. Sensitivity is an extremely subjective perception and, therefore, it is difficult to define and evaluate objectively. Moreover, most of the included studies did not provide adequate information, neither on the grade of sensitivity of the NAC before undergoing reduction mammaplasty for gigantomastia, nor on the assessment protocols used (number of raters, experience in sensitivity assessment, reproducibility, method used, timing of assessment, area assessed, and whether patients were asked to close their eyes). However, we underline that the major strength of this systematic review and meta-analysis is the absence of a significant statistical heterogeneity.
Conclusions
This study provides for the first time the evidence of the low risk of sensory loss associated with the NAC-carrying pedicle technique in reduction mammoplasty for gigantomastia. Based on these findings, by combining the safety assurances with outstanding functional outcomes, the NAC-carrying pedicle technique emerges as the preferred choice for reduction mammoplasty for gigantomastia. However, detailed surgical planning and execution remain crucial. The capacity to convert to an FNG approach during surgery should serve as “salvage procedure” in case of insufficiently perfused NAC, preserving the overall safety of the patient and ultimate success of the proscedure.
Acknowledgments
Funding
None.
Conflicts of interest
None declared.
Ethical approval
Not required.
References
- 1.Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136:531–544. doi: 10.1097/PRS.0000000000001622. [DOI] [PubMed] [Google Scholar]
- 2.Sarwer DB, Bartlett SP, Bucky LP, et al. Bigger is not always better: Body image dissatisfaction in breast reduction and breast augmentation patients. Plast Reconstr Surg. 1998;101:1956–1961. doi: 10.1097/00006534-199806000-00028. [DOI] [PubMed] [Google Scholar]
- 3.Glatt BS, Sarwer DB, O'Hara DE, Hamori C, Bucky LP, LaRossa D. A retrospective study of changes in physical symptoms and body image after reduction mammaplasty. Plast Reconstr Surg. 1999;103:76–82. doi: 10.1097/00006534-199901000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Sabino Neto M, Demattê MF, Freire M, Garcia EB, Quaresma M, Ferreira LM. Self-esteem and functional capacity outcomes following reduction mammaplasty. Aesthet Surg J. 2008;28:417–420. doi: 10.1016/j.asj.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Wettstein R, Christofides E, Pittet B, Psaras G, Harder Y. Superior pedicle breast reduction for hypertrophy with massive ptosis. J Plast Reconstr Aesthetic Surg. 2011;64:500–507. doi: 10.1016/j.bjps.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 6.Dafydd H, Roehl KR, Phillips LG, Dancey A, Peart F, Shokrollahi K. Redefining gigantomastia. J Plast Reconstr Aesthetic Surg. 2011;64:160–163. doi: 10.1016/j.bjps.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 7.Kalliainen LK. ASPS Health Policy Committee. ASPS clinical practice guideline summary on reduction mammaplasty. Plast Reconstr Surg. 2012;130:785–789. doi: 10.1097/PRS.0b013e318262f0c0. [DOI] [PubMed] [Google Scholar]
- 8.Dancey A, Khan M, Dawson J, Peart F. Gigantomastia–A classification and review of the literature. J Plast Reconstr Aesthetic Surg. 2008;61:493–502. doi: 10.1016/j.bjps.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 9.Moio M, Schonauer F. Correlation between nipple elevation and breast resection weight: How to preoperatively plan breast reduction. J Plast Reconstr Aesthet Surg. 2015;68:1127–1131. doi: 10.1016/j.bjps.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Thorek M. Possibilities in the reconstruction of the human form 1922. Aesthetic Plast Surg. 1989;13:55–58. doi: 10.1007/BF01570326. [DOI] [PubMed] [Google Scholar]
- 11.Al-Shaham A. Pedicle viability as the determinant factor for conversion to free nipple graft. Can J Plast Surg. 2010;18:e1–e4. doi: 10.4172/plastic-surgery.1000643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonomi F, Harder Y, Treglia G, De Monti M, Parodi C. Is free nipple grafting necessary in patients undergoing reduction mammoplasty for gigantomastia? A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2024;89:144–153. doi: 10.1016/j.bjps.2023.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Talwar AA, Copeland-Halperin LR, Walsh LR, et al. Outcomes of extended pedicle technique vs free nipple graft reduction mammoplasty for patients with gigantomastia. Aesthet Surg J. 2023;43:N91–NP99. doi: 10.1093/asj/sjac258. [DOI] [PubMed] [Google Scholar]
- 14.Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59:500–507. [PubMed] [Google Scholar]
- 15.Lugo LM, Prada M, Kohanzadeh S, Mesa JM, Long JN, de la Torre J. Surgical outcomes of gigantomastia breast reduction superomedial pedicle technique: A 12-year retrospective study. Ann Plast Surg. 2013;70:533–537. doi: 10.1097/SAP.0b013e31827c7909. [DOI] [PubMed] [Google Scholar]
- 16.Kraut RY, Brown E, Korownyk C, Katz LS, Vandermeer B, Babenko O, et al. The impact of breast reduction surgery on breastfeeding: Systematic review of observational studies. PloS One. 2017;12 doi: 10.1371/journal.pone.0186591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Copeland-Halperin LR, Smith L, Copeland M. Re-evaluating the Lejour technique for breast reduction in patients with macromastia. Plast Reconstr Surg Glob Open. 2018;6:e1783. doi: 10.1097/GOX.0000000000001783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bilgen F, Ural A, Bekerecioğlu M. Inferior and central mound pedicle breast reduction in gigantomastia: A safe alternative? J Investig Surg Off J Acad Surg Res. 2021;34:401–407. doi: 10.1080/08941939.2019.1648609. [DOI] [PubMed] [Google Scholar]
- 19.Zelko I, DeLeonibus A, Haidar J, Bahat D, Bishop SN. Nipple-Sparing gigantomastia breast reduction: A systematic review. Ann Plast Surg. 2023;90:267–272. doi: 10.1097/SAP.0000000000003415. [DOI] [PubMed] [Google Scholar]
- 20.Koussayer B, Taylor J, Warner J, Alkaelani MT, Blount T, Wainwright D, et al. Breastfeeding ability after breast reductions: What does the literature tell us in 2023? Aesthet Plast Surg. 2024;48:1142–1155. doi: 10.1007/s00266-023-03690-8. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 22.Sadeghi R, Treglia G. Systematic reviews and meta-analyses of diagnostic studies: A practical guideline. Clin Transl Imaging. 2017;5:83–87. [Google Scholar]
- 23.Chang P, Shaaban AF, Canady JW, Ricciardelli EJ, Cram AE. Reduction mammaplasty: The results of avoiding nipple-areolar amputation in cases of extreme hypertrophy. Ann Plast Surg. 1996;37:585–591. [PubMed] [Google Scholar]
- 24.Lacerna M, Spears J, Mitra A, Medina C, McCampbell E, Kiran R, al et. Avoiding free nipple grafts during reduction mammaplasty in patients with gigantomastia. Ann Plast Surg. 2005;55:21–24. doi: 10.1097/01.sap.0000168249.09491.21. [DOI] [PubMed] [Google Scholar]
- 25.Ashour T, Khachaba Y, El Naggar A. Supero-medial reduction mammaplasty: A safe and reliable technique in gigantomastia and severe breast ptosis. Electron Physician. 2018;10:7230–7234. doi: 10.19082/7230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Başaran K, Ucar A, Guven E, Arinci A, Yazar M, Kuvat SV. Ultrasonographically determined pedicled breast reduction in severe gigantomastia. Plast Reconstr Surg. 2011;128:252e–259e. doi: 10.1097/PRS.0b013e3182268bb1. [DOI] [PubMed] [Google Scholar]
- 27.Oneal RM, Goldstein JA, Rohrich R, Izenberg PH, Pollock RA. Reduction mammoplasty with free-nipple transplantation: Indications and technical refinements. Ann Plast Surg. 1991;26:117–121. doi: 10.1097/00000637-199102000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Koger KE, Sunde D, Press BH, Hovey LM. Reduction mammaplasty for gigantomastia using inferiorly based pedicle and free nipple transplantation. Ann Plast Surg. 1994;33:561–564. doi: 10.1097/00000637-199411000-00017. [DOI] [PubMed] [Google Scholar]
- 29.Colen SR. Breast reduction with use of the free nipple graft technique. Aesthet Surg J. 2001;21:261–271. doi: 10.1067/maj.2001.116439. [DOI] [PubMed] [Google Scholar]
- 30.Georgiade NG, Lewis EC. Reconstructive breast surgery. Plast Reconstr Surg. 1977;59:741. [Google Scholar]
- 31.Hawtof DB, Levine M, Kapetansky DI, Pieper D. Complications of reduction mammaplasty: Comparison of nipple-areolar graft and pedicle. Ann Plast Surg. 1989;23:3–10. doi: 10.1097/00000637-198907000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Griffiths M, Chae MP, Rozen WM. Indocyanine green-based fluorescent angiography in breast reconstruction. Gland Surg. 2016;5:133–149. doi: 10.3978/j.issn.2227-684X.2016.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nguyen CL, Barry N, Lindsay A, et al. Indocyanine green angiography in breast reconstruction surgery: A systematic review of cost-analysis studies. J Plast Reconstr Aesthetic Surg. 2021;74:3196–3211. doi: 10.1016/j.bjps.2021.08.013. [DOI] [PubMed] [Google Scholar]
- 34.Yoshimatsu H, Karakawa R, Scaglioni MF, Fuse Y, Yano T. Use of intraoperative indocyanine green angiography for detection and prediction of congestion in pedicled island flaps. Microsurgery. 2023;43:452–459. doi: 10.1002/micr.31009. [DOI] [PubMed] [Google Scholar]
- 35.Wechselberger G, Stoß S, Schoeller T, Oehlbauer M, Piza-Katzer H. An analysis of breast sensation following inferior pedicle mammaplasty and the effect of the volume of resected tissue. Aesthetic Plast Surg. 2001;25:443–446. doi: 10.1007/s002660010156. [DOI] [PubMed] [Google Scholar]
- 36.Santanelli F, Paolini G, Bittarelli D, Nofroni I. Computer-assisted evaluation of nipple-areola complex sensibility in macromastia and following superolateral pedicle reduction mammaplasty: A statistical analysis. Plast Reconstr Surg. 2007;119:1679–1683. doi: 10.1097/01.prs.0000258828.84107.59. [DOI] [PubMed] [Google Scholar]
- 37.Chiari A, Jr, Nunes TA, Grotting JC, Cotta FB, Gomes RC. Breast sensitivity before and after the L short-scar mammaplasty. Aesthet Plast Surg. 2012;36:105–114. doi: 10.1007/s00266-011-9756-2. [DOI] [PubMed] [Google Scholar]
- 38.Smeele HP, Bijkerk E, van Kuijk SMJ, Lataster A, van der Hulst RRWJ, Tuinder SMH. Innervation of the female breast and nipple: a systematic review and meta-analysis of anatomical dissection studies. Plast Reconstr Surg. 2022;150:243–255. doi: 10.1097/PRS.0000000000009306. [DOI] [PubMed] [Google Scholar]
- 39.Rancati AO, Angrigiani C, Nahabedian MY, Rancati A, White KP. Fluorescence imaging to identify and preserve fifth intercostal sensory nerves during bilateral nipple-sparing mastectomies. Plast Reconstr Surg Glob Open. 2023;11:e5048. doi: 10.1097/GOX.0000000000005048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Torresetti M, Andrenelli E, Peltristo B, Zavalloni Y, Capecci M, Ceravolo MG, Di Benedetto G. The impact of reduction mammaplasty on breast sensation: A systematic review. Aesthet Surg J. 2023;43:NP847–NP854. doi: 10.1093/asj/sjad234. [DOI] [PubMed] [Google Scholar]
- 41.Amini P, Stasch T, Theodorou P, Altintas AA, Phan V, Spilker G. Vertical reduction mammaplasty combined with a superomedial pedicle in gigantomastia. Ann Plast Surg. 2010;64:279–285. doi: 10.1097/SAP.0b013e3181b0a5d8. [DOI] [PubMed] [Google Scholar]
- 42.Bucaria V, Elia R, Maruccia M, Annoscia P, Boccuzzi A, Giudice G. Why choose the septum-supero-medial (SSM)-based mammaplasty in patients with severe breast ptosis: An anatomical point of view. Aesthet Plast Surg. 2018;42:1439–1446. doi: 10.1007/s00266-018-1189-8. [DOI] [PubMed] [Google Scholar]
- 43.Chetty V, Ndobe E. Macromastia and gigantomastia: Efficacy of the superomedial pedicle pattern for breast reduction surgery. S Afr J Surg. 2016;54:46–50. [PubMed] [Google Scholar]
- 44.Elmelegy NG, Sadaka MS, Hegazy AM, Abdeldaim DE. Treatment of gigantomastia using a medial-lateral bipedicle reduction mammoplasty: The role of Doppler-assisted preoperative perforator identification. Aesthet Plast Surg. 2018;42:73–79. doi: 10.1007/s00266-017-1049-y. [DOI] [PubMed] [Google Scholar]
- 45.Karacaoglu E, Zienowicz RJ. Septum-Inferior-Medial (SIM)-based pedicle: A safe pedicle with well-preserved nipple sensation for reduction in gigantomastia. Aesthet Plast Surg. 2017;41:1–9. doi: 10.1007/s00266-016-0763-1. [DOI] [PubMed] [Google Scholar]
- 46.Karacor-Altuntas Z, Dadaci M, Ince B, Karamese M, Savaci N. Central pedicle reduction in gigantomastia without free nipple graft. Ann Plast Surg. 2016;76:383–387. doi: 10.1097/SAP.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 47.Kemaloğlu CA, Özocak H. Comparative outcomes of inferior pedicle and superomedial pedicle technique with wise pattern reduction in gigantomastic patients. Ann Plast Surg. 2018;80:217–222. doi: 10.1097/SAP.0000000000001231. [DOI] [PubMed] [Google Scholar]
- 48.Lacerna M, Spears J, Mitra A, Medina C, McCampbell E, Kiran R, et al. Avoiding free nipple grafts during reduction mammaplasty in patients with gigantomastia. Ann Plast Surg. 2005;55:21–24. doi: 10.1097/01.sap.0000168249.09491.21. [DOI] [PubMed] [Google Scholar]
- 49.Letertre P, Lasserre G, Ricbourg B. Traitement des hypertrophies mammaires très importantes et des gigantomasties par la technique de réduction dite à pédicule postéro-inférieur. A propos de 20 cas [Large breast hypertrophy and gigantomastia management by postero-inferior pedicle reduction technique. About 20 cases] Ann Chir Plast Esthet. 2009;54:331–339. doi: 10.1016/j.anplas.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 50.Mojallal A, Moutran M, Shipkov C, Saint-Cyr M, Rohrich RJ, Braye F. Breast reduction in gigantomastia using the posterosuperior pedicle: an alternative technique, based on preservation of the anterior intercostal artery perforators. Plast Reconstr Surg. 2010;125:32–43. doi: 10.1097/PRS.0b013e3181c49561. [DOI] [PubMed] [Google Scholar]
- 51.Nahabedian MY, McGibbon BM, Manson PN. Medial pedicle reduction mammaplasty for severe mammary hypertrophy. Plast Reconstr Surg. 2000;105:896–904. doi: 10.1097/00006534-200003000-00011. [DOI] [PubMed] [Google Scholar]