Abstract
This report describes a medial calcar episiotomy with partial anterior transfemoral osteotomy of the proximal femur to aid in removal of a femoral component in setting of revision total hip arthroplasty through a direct anterior approach. Revision total hip arthroplasty is challenging, labor-intensive, and carries high complication rates. Previously described techniques such as extended trochanteric osteotomies can be utilized to facilitate removal of fixed femoral stems. The technique herein described was performed in an effort to avoid the morbidity of additional dissection and risk of nonunion associated with complete osteotomy of the trochanteric region. We present a novel technique to aid in the removal of a fixed femoral stem in the setting of revision total hip arthroplasty through an anterior approach. This technique has not previously been described specifically in the literature and was performed safely and effectively for this patient. A complication-free outcome with osteotomy union was achieved on a final follow-up of 13 months.
Keywords: Hip, Revision, Extraction, Osteotomy, Direct anterior
Introduction
Total hip arthroplasty (THA) is one of the most common surgical procedures performed by orthopaedic surgeons and has experienced rapid growth in the United States among all surgical procedures. [1] Primary THA can be performed through posterior, lateral, and anterior surgical approaches, and the direct anterior (DA) approach has gained popularity in the past decade. [2] Given the large projected increases in primary THA performed, the increase in necessity for revision procedures is inevitable. As such, the number of cases of revision THA has been projected to increase between 43% and 70% from 2014 to 2030. [3]
Revision total hip arthroplasty can be technically challenging and carries higher complication rates compared to primary THA. Historically, numerous techniques have been described through posterior and lateral approaches to facilitate removal of fixed femoral stems and help to prevent iatrogenic fracture or loss of bone stock. However, until recent years, described DA revision techniques were only cadaveric in nature. Described DA femoral stem revision techniques such as the anterior cortical window and the extended trochanteric osteotomy offer advantages in stem extraction but carry complication risks such as abductor weakness, intraoperative fracture, and nonunion. [[4], [5], [6]]
The purpose of this report is to describe a case of revision THA through the DA approach in which a novel technique involving a medial bone episiotomy and anterior transfemoral osteotomy without breaching of the lateral cortex was used to assist in femoral stem extraction and to describe advantages and disadvantages when compared to previously described DA revision techniques.
Surgical technique
A 65-year-old male presented with left hip pain and mechanical symptoms 1 year following uneventful THA performed through a standard DA approach. Radiographic images (Fig. 1), lab workup, and bone scan confirmed the presence of aseptic loosening of the proximal aspect of the femoral component, and he underwent revision total hip arthroplasty. Written informed consent was obtained for publishing this deidentified surgical technique paper.
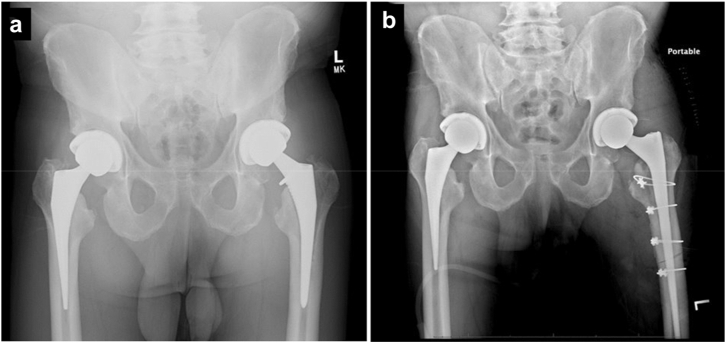
Figure 1.
(a) Preoperative radiographs demonstrating history of bilateral THA with loosening of left femoral component proximally and apparent fixation distally. (b) Immediate postoperative radiographs after revision of femoral component.
The patient was positioned on a Hana table (Mizuho OSI) and draped in normal sterile fashion. The operative surgeon (S.D.) elected the standard DA approach through the previous incision, an approach that has been well-described in the literature, while excising scarred tissue. The hip was then dislocated and the femoral head was removed. The femoral component appeared loose proximally but was found to be well-fixated distally. Several attempts made at stem removal were unsuccessful. Straight, curved, and flexible osteotomes as well as flexible drills and burs were used to loosen the prosthesis without success. It was then decided to perform a medial episiotomy to gain access to the femoral stem.
The incision was extended distally, and the femur was externally rotated to 90 degrees to bring the medial calcar anteriorly in line with the incision. The vastus medialis muscle was carefully peeled off the femur to the tip of the stem distally. Roughly 1 cm below the lesser trochanter, vascular branches to the muscle were encountered during dissection. These branches were protected by carefully lifting them off the femur with a right-angle retractor with blunt edges, as the major blood supply to the vastus medialis muscle comes from distal branches, and smaller vessels were coagulated where required (Fig. 2). Using an oscillating saw with a 2 mm blade, the episiotomy was started proximal and anterior to the lesser trochanter on the medial calcar region, and the episiotomy was extended to the tip of the stem, which was confirmed with fluoroscopic imaging (Fig. 3). We do suggest use of a small-width blade for the oscillating saw to avoid surrounding soft tissue injury when necessary.
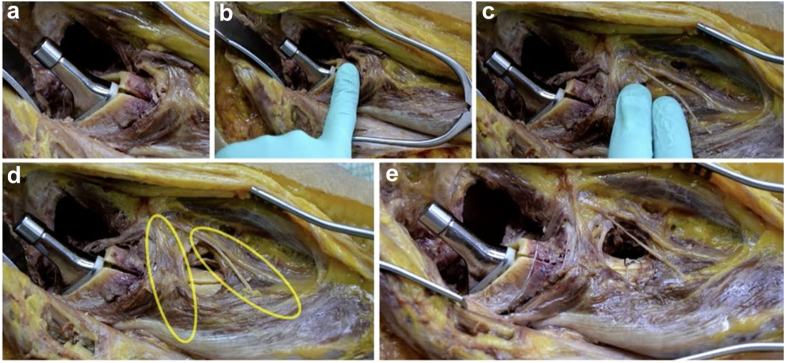
Figure 2.
Vasculature encountered during proposed surgical technique demonstrating proximity to medial calcar demonstrated in a cadaveric specimen.
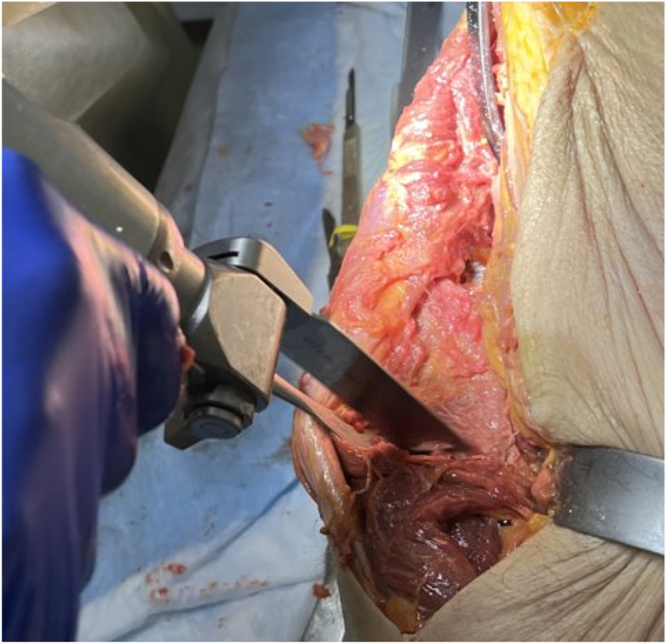
Figure 3.
Medial proximal femoral osteotomy demonstrated in a cadaveric specimen.
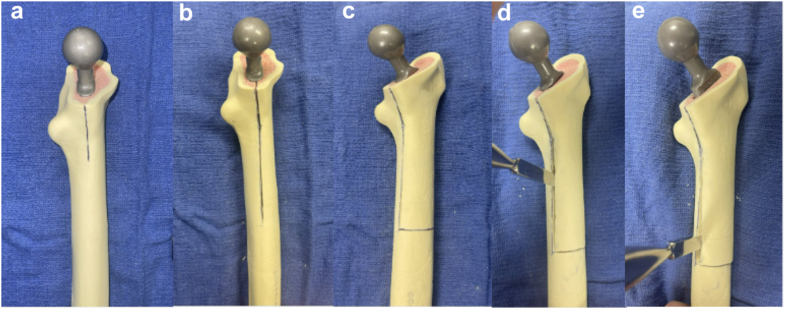
After completion of the episiotomy, attempts at removal remained unsuccessful as the stem remained well-fixed anteriorly and posteriorly. It was then decided to proceed with an anterior transfemoral osteotomy from the medial to lateral direction distally without breaching the lateral cortex, starting from the end of the episiotomy. The leg was then brought back to a neutral position. A Cobra retractor was placed distally on the lateral aspect of the femur to visualize the anterior surface of the femur. The anterior transfemoral osteotomy was then made using the oscillating saw (Fig. 4). The leg was then externally rotated back to 90 degrees, exposing the medial calcar region. Small Kirschner wires (Synthes Holdings, AG) and flexible osteotomes were used anterior and posterior to the stem distally to free up the interface between the stem and bone. As stated previously, our exposure and stem removal did not necessitate the breaching of the lateral cortex (Fig. 5). The stem was then able to be removed by hand in the case described. The osteotomy was fixated with 4 cables (Synthes Holdings, AG), one distal and 3 proximal to the distal osteotomy site. The femoral canal was then reamed, and a long revision femoral stem was used with good intraoperative stability observed.
Figure 4.
Anterior transfemoral osteotomy demonstrated in a cadaveric specimen.
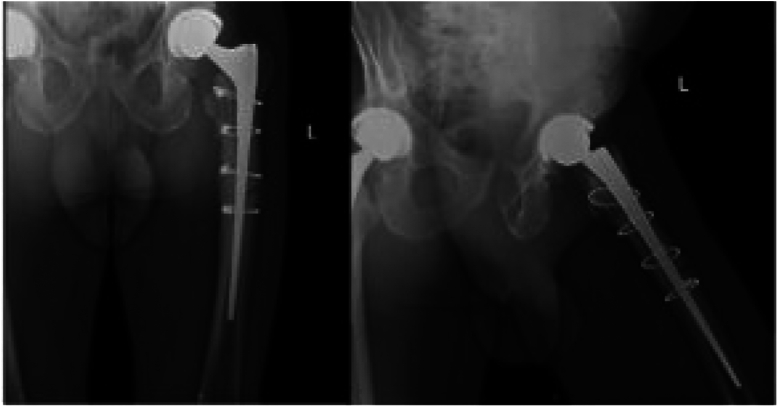
Figure 6.
Thirteen-month follow-up radiographs depicting hardware in optimal alignment with healing of osteotomy site.
Postoperatively, he was made 50% flatfoot weight-bearing on his left lower extremity. He progressed to full weight bearing at 4 weeks and underwent a self-directed home exercise program to maintain strength and range of motion. He was allowed all activities as tolerated at 10 weeks postoperatively. At 13-month follow-up, the patient is progressing well, the incision is well-healed, and radiographic images confirm excellent position of the prosthesis with union at the osteotomy site and without hardware complication (Fig. 6). He has been able to complete his activities of daily living without issue or pain.
Figure 5.
Sawbones example of technique. (a) Proximal planned medial episiotomy. (b) Episiotomy extended distally. (c) Planned anterior transfemoral osteotomy after episiotomy has been completed. (d) Osteotome used to lever osteotomy site open proximally. (e) Osteotome used to lever osteotomy site open distally. Note the lateral most cortex remains intact.
Discussion
There have been numerous techniques and variations of osteotomies described to aid in the removal of a fixed femoral stem in the setting of revision arthroplasty. First described in 1995 by Younger, the extended trochanteric osteotomy (ETO) has become very popular in this setting. [7] Studies have shown this can be a safe and effective technique to aid a difficult problem, but there have been reported complications associated with it. [8] Known complications surrounding the greater trochanteric disruption include nonunion, trochanteric migration, stem subsidence, fracture, abductor weakness, and dislocation. [[9], [10], [11]] This technique and evolved variations have traditionally been described through lateral or posterior approaches. A variation of an ETO through a DA approach has been described in recent years, and studies suggest equivocal results. [12,13] Other osteotomy techniques have been described that avoid disruption of the greater trochanter in an effort to avoid potential complications of nonunion and abductor weakness. [14,15] An anterior cortical window can be performed without disrupting the greater trochanter, and studies have shown satisfactory survivorship at 10-year follow-up. [5] This technique has also been recently described through the DA approach. [6] Mahmood et al recently described an “inside-out” technique; however, that procedure has limitations as well.
By performing the approach described herein, an “outside-in" technique, the trochanteric region is avoided in an effort to prevent known complications that can be difficult to address anteriorly. This approach may have inherently less morbidity than other previously described approaches, and our procedure can be performed in a stepwise fashion. If the longitudinal split is performed medially, it is the belief of these authors that it gives you an advantage in removing the stem with episiotomy alone, as most stems are well-fixed around the medial calcar region. If the stem cannot be safely removed with only an episiotomy, then the anterior transfemoral osteotomy can be performed as described. This may include procedures for tapered stems, while other osteotomy options may be chosen for more well-fixed, full-coated stems, which require stem cutting. It is also thought that without completing the osteotomy and leaving the lateral and posterior cortex intact, there will be a decreased risk of nonunion; however, this would require studies in larger populations with long-term follow-up.
This approach brings the surgeon in closer proximity to the femoral vessels medially. It has been shown that the intra-articular terminal branches of the medial femoral circumflex artery lie approximately 4 cm medially from the medial calcar region [16]. Care should be given to stay in close proximity to the bone medially to avoid iatrogenic injury. However, the perforating vessels that can be encountered in lateral ETO are protected in this approach. Only one muscular branch was encountered proximally feeding the vastus medialis in this patient, which can be protected or electrocauterized.
Summary
We present a novel technique to aid in the removal of a fixed femoral stem in the setting of revision total hip arthroplasty through an anterior approach. This technique has not previously been described in the literature and was performed safely and effectively for this patient. Given the rise in the number of THA and DA surgeons, it is of value to describe new surgical techniques in DA revision arthroplasty. Further research should be conducted involving this technique with longer-term follow-up and a larger patient population.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2024.101583.
CRediT authorship contribution statement
Brian Omslaer: Writing – review & editing, Writing – original draft, Conceptualization. Shaan Sadhwani: Writing – review & editing, Writing – original draft, Conceptualization. Jamie Henzes: Writing – review & editing. Steven Deluca: Writing – review & editing, Writing – original draft, Conceptualization. Muzaffar Ali: Writing – review & editing, Writing – original draft, Conceptualization.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.artd.2024.101583.
Appendix A. Supplementary data
References
- 1.Fingar K.R., Stocks C., Weiss A.J., Steiner C.A. Agency for Healthcare Research and Quality (US); Rockville, MD: 2006. Most frequent operating room procedures performed in U.S. Hospitals, 2003–2012: statistical brief #186, in healthcare cost and utilization project (HCUP) statistical briefs. [PubMed] [Google Scholar]
- 2.Patel N.N., Shah J.A., Erens G.A. Current trends in clinical practice for the direct anterior approach total hip arthroplasty. J Arthroplasty. 2019;34:1987–1993. doi: 10.1016/j.arth.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz A.M., Farley K.X., Guild G.N., Bradbury T.L., Jr. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79–S85. doi: 10.1016/j.arth.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thaler M., Dammerer D., Ban M., Leitner H., Khosravi I., Nogler M. Femoral revision total hip arthroplasty performed through the interval of the direct anterior approach. J Clin Med. 2021;10:337. doi: 10.3390/jcm10020337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park C.H., Yeom J., Park J.W., Won S.H., Lee Y.K., Koo K.H. Anterior cortical window technique instead of extended trochanteric osteotomy in revision total hip arthroplasty: a minimum 10-year follow-up. Clin Orthop Surg. 2019;11:396–402. doi: 10.4055/cios.2019.11.4.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morcos M.W., Decker M.M., Lanting B.A. Direct anterior approach for femoral component revision: surgical technique for extended trochanteric osteotomy and anterior cortical window. J Orthop. 2020;22:274–277. doi: 10.1016/j.jor.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Younger T.I., Bradford M.S., Magnus R.E., Paprosky W.G. Extended proximal femoral osteotomy. A new technique for femoral revision arthroplasty. J Arthroplasty. 1995;10:329–338. doi: 10.1016/s0883-5403(05)80182-2. [DOI] [PubMed] [Google Scholar]
- 8.Hamad K., Konan S. Extended trochanteric osteotomy in revision hip arthroplasty: a case series study and systematic literature review. Arthroplasty. 2022;4:14. doi: 10.1186/s42836-022-00115-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calek A.K., Schöfl T., Zdravkovic V., Zurmühle P., Ladurner A. Aseptic revision of total hip arthroplasty with a single modular femoral stem and a modified extended trochanteric osteotomy-treatment assessment with the forgotten joint score-12. Arthroplast Today. 2022;15:159–166. doi: 10.1016/j.artd.2022.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehra A., Hemmady M.V., Hodgkinson J.P. Trochanteric non-union--does it influence the rate of revision following primary total hip replacement? A minimum of 15 years follow-up. Surgeon. 2008;6:79–82. doi: 10.1016/s1479-666x(08)80069-8. [DOI] [PubMed] [Google Scholar]
- 11.Sundaram K., Siddiqi A., Kamath A.F., Higuera-Rueda C.A. Trochanteric osteotomy in revision total hip arthroplasty. EFORT Open Rev. 2020;5:477–485. doi: 10.1302/2058-5241.5.190063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pan T., Bierowski M.J., King T.S., Mason M.W. Outcomes of revision hip arthroplasty using the supine anterior-based muscle sparing approach. Arthroplast Today. 2022;14:199–203. doi: 10.1016/j.artd.2022.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manrique J., Chen A.F., Heller S., Hozack W.J. Direct anterior approach for revision total hip arthroplasty. Ann Transl Med. 2014;2:100. doi: 10.3978/j.issn.2305-5839.2014.09.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim Y.M., Lim S.T., Yoo J.J., Kim H.J. Removal of a well-fixed cementless femoral stem using a microsagittal saw. J Arthroplasty. 2003;18:511–512. doi: 10.1016/s0883-5403(03)00024-x. [DOI] [PubMed] [Google Scholar]
- 15.Smith E.B. Save the greater trochanter: a novel modification to the extended trochanteric osteotomy. Arthroplast Today. 2022;16:107–111. doi: 10.1016/j.artd.2022.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gadinsky N.E., Klinger C.E., Sculco P.K., Helfet D.L., Lorich D.G., Lazaro L.E. Femoral head vascularity: implications following trauma and surgery about the hip. Orthopedics. 2019;42:250–257. doi: 10.3928/01477447-20190723-03. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.