Abstract
DNA methylation is crucial for chromatin structure, transcription regulation and genome stability, defining cellular identity. Aberrant hypermethylation of CpG-rich regions is common in cancer, influencing gene expression. However, the specific contributions of individual epigenetic modifications to tumorigenesis remain under investigation. In hepatocellular carcinoma (HCC), DNA methylation alterations are documented as in other tumor types. We aimed to identify hypermethylated CpGs in HCC, assess their specificity across other tumor types, and investigate their impact on gene expression. To this end, public methylomes from HCC, other liver diseases, and 27 tumor types as well as expression data from TCGA-LIHC and GTEx were analyzed. This study identified 39 CpG sites that were hypermethylated in HCC compared to control liver tissue, and were located within promoter, gene bodies, and intergenic CpG islands. Notably, these CpGs were predominantly unmethylated in healthy liver tissue and other normal tissues. Comparative analysis with 27 other tumors revealed both common and HCC-specific hypermethylated CpGs. Interestingly, the HCC-hypermethylated genes showed minimal expression in the different healthy tissues, with marginal changes in the level of expression in the corresponding tumors. These findings confirm previous evidence on the limited influence of DNA hypermethylation on gene expression regulation in cancer. It also highlights the existence of mechanisms that allow the selection of tissue-specific methylation marks in normally unexpressed genes during carcinogenesis. Overall, our study contributes to demonstrate the complexity of cancer epigenetics, emphasizing the need of better understanding the interplay between DNA methylation, gene expression dynamics, and tumorigenesis.
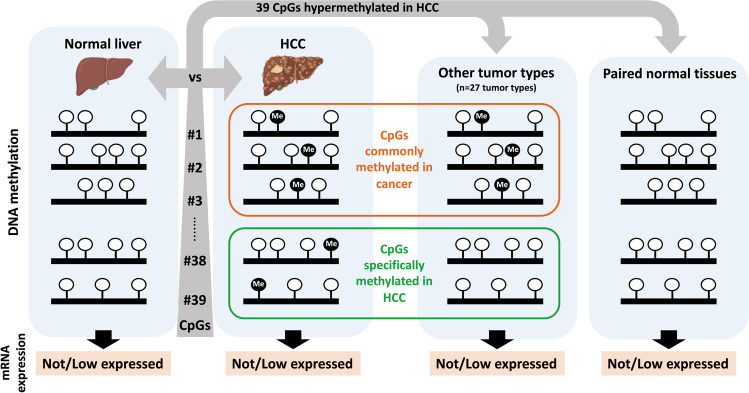
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s13105-024-01045-8.
Keywords: DNA methylation, Liver cancer, Gene expression, Tumor-specific markers
Introduction
DNA methylation, which consists on the addition of a methyl group at carbon 5 of cytosine in cytosine-guanine dinucleotides (CpG), is an essential epigenetic mechanism influencing chromatin structure, regulation of transcription and genome stability [26, 43]. In healthy cells, the bulk of the genome is CpG-deficient and predominantly methylated, while discrete regions called CpG islands (CGIs) are CpG-rich and usually unmethylated [24]. CGIs are located in the promoter region of approximately 60% of genes [24] and promoter-CGI methylation is associated with gene silencing [26, 43]. However approximately half of the annotated CGI are distributed between gene bodies and intergenic regions [24]. Increased CGI gene body methylation positively correlates with transcriptional activation [6, 25, 55], regulates tissue-specific promoter usage [39] or alternative splicing [38]. Therefore, methylation of CpG sites is an essential component of cell type-specific gene regulation, a fundamental mark of cell identity [12, 16, 41], and therefore the unique methylation profile of cells can be used to identify their tissue of origin [33, 59].
Importantly, alterations of methylation patterns are associated with disease development and allow to distinguish healthy from diseased states, including cancer [8, 12, 31]. In fact, an epigenetic reprogramming, including abnormal DNA methylation patterns, is a common alteration in the tumorigenic process, independently of the cell of origin [17]. It has been widely described that during the process of carcinogenesis a global hypomethylation of DNA occurs in parallel with the hypermethylation of CGIs in the promoter regions [26, 43]. Thus, although DNA methylation is considered a tissue-specific mark, many tumor suppressor genes are silenced by aberrant promoter methylation in different types of cancer [14, 26]. For instance, promoter hypermethylation of the DNA-repair gene O6-methylguanine-DNA methyltransferase (MGMT) is a common event in human neoplasia [13], including glioblastoma multiforme, colorectal or breast cancer or of RASSF1A has been observed in several types of cancer others [36], including HCC, breast, pancreatic or lung cancer, among others. However, in line with the relationship between methylation patterns and cellular identity [12, 16, 41], it has also been described that some DNA methylation patterns are associated with specific types of cancers and therefore can be used to differentiate between various tumor types [56, 59].
During the last decades, the use of high-throughput sequencing analyses has considerably contributed to our understanding of how epigenetic modifications contribute to the tumorigenic process [14]. However, an open question remains as to which of all the DNA methylation modifications that occur during malignant transformation are common across different types of tumors (how many and which types of tumors) or specific to a single tumor type. This includes not only the CpGs within promoter CGIs but also those located in gene bodies and intergenic regions, even outside of CGIs. Furthermore, it is critical to determine the impact of such hypermethylation on gene expression and the tumorigenic process, distinguishing between modifications that act as tumorigenic drivers and those that are merely passenger events [10, 27].
Hepatocellular carcinoma (HCC), the most frequent form of liver cancer, ranks as the sixth most common neoplasm and the fourth leading cause of cancer-related death [32]. HCC development and progression consists in a multistep and complex process with sequential genetic and epigenetic alterations [15, 32]. Several previous studies have reported human DNA methylome data on HCC tissue samples and their non-tumoral liver tissue counterparts [3, 20, 30, 40, 44, 50].
Here, using publicly available methylomes, we identified a set of 39 CpGs hypermethylated in HCC compared to control liver that were located not only in promoter but also in gene bodies and intergenic CGIs. These CpGs were predominantly unmethylated in control liver and other extrahepatic healthy tissues, allowing us to identify CpGs that were hypermethylated exclusively in HCC or in several other tumors. Importantly, we observed that DNA hypermethylation in tumors occurs in genes either not expressed or minimally expressed in healthy tissues, suggesting a potential role of DNA methylation in gene expression regulation and cancer development.
Methods
Human samples
The study was approved by the Human Research Review Committee of the University of Navarra (CEI 47/2015). Samples from tumoral (n = 19) and non-tumoral (n = 5) tissues were obtained from HCC patients treated with liver resection. Healthy liver tissues (n = 5) were obtained from surgical resections performed to patients with colon cancer metastasis with normal or minimal liver changes. Samples and data from patients included in the study were provided by the Biobank of the University of Navarra and were processed following standard operating procedures approved by the Ethical and Scientific Committees and by Dr. A Casadei-Gardini (Colection ref.IRST-BO24). Informed consent was obtained from each patient and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Public methylome datasets
All methylomes used were carried out with the Illumina's Infinium HumanMethylation450 (HM450) BeadChip array that analyze around 450.000 CpGs. The CpG candidate lists were identified from: GSE56588 [50], GSE54503 [44], TCGA-LIHC [3], and GSE40279 [18]. For non-tumor liver diseases, we utilized datasets GSE61258 [22], GSE48325 [1], and GSE60753 [20]. To validate findings in human HCC tissue samples, we used datasets GSE60753 [20], GSE89852 [30], and GSE157341 [40]; and GSE60753 [20] for primary hepatocytes and HCC cell lines (FLNEO, H801, HCO2, Hep3B, Huh75, LH86, SNU423, SNU449). Methylation data from 28 tumor types from the TCGA database (including TCGA-LIHC; Supplementary Table S4), comprising 8706 tumor and 759 non-tumor samples, were included.
Identification of differentially methylated CpGs
For identifying hypermethylated CpGs in HCC, 485.512 single CpG sites, present in all samples from GSE56588 [50], GSE54503 [44] and TCGA-LIHC [3] were analyzed. Of these, 144,543 CpGs located within a CGI were retained. β-value ranged from 0 (unmethylated) to 1 (fully methylated). The methylation difference per CpG was calculated as the mean β-value of tumors minus controls. CpGs with a mean methylation difference > 0.2 and an FDR < 0.05 (Student’s two-sided T-test and Benjamini–Hochberg False Discovery Rate) were retained. CpGs are classified as “hypomethylated” with a difference is < − 0.2 and as “hypermethylated” with a difference > 0.2.
For each study, the β-value of the 39 CpGs of interest was extracted from their database. A CpG was considered unmethylated when its β-value was < 0.2 and methylated when its β-value was > 0.2. Each figure includes a color scale indicating the β-value. Additionally, where indicated, the methylation difference between groups was calculated as explained above. Hypermethylation was considered when the difference was > 0.2.
Expression in databases
The expression of the genes was analyzed in HCC and non-tumoral liver samples from the TCGA-LIHC dataset (raw RNA-Seq data downloaded from the GDC Data Portal) and in normal tissues from GTEx.
Hierarchical clustering
Unsupervised hierarchical clustering was performed using the linkage function from the Python Scipy library with Ward distance and plotted using the dendogram function.
Dimensionality reduction analyses
Uniform Manifold Approximation and Projection (UMAP) of patients CGI methylation across studies using umap Python library.
Total DNA Isolation
Total DNA from frozen tissues was isolated using the Maxwell® RSC Cultured Cells DNA Purification Kit with a Maxwell® RSC 48 instrument (Promega, Madison, WI, USA; AS1620). DNA purity and concentration were measured using a NanoDrop spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA).
PCR and Sanger sequencing
Genomic DNA (1 µg) was bisulfite converted using the EZ DNA Methylation Gold Kit (Zymo Research; D5005) according to the manufacturer’s instructions. PCRs of fragments containing the CpG candidates in bisulfite-converted DNA were performed using 5 ng of bisulfite-converted DNA, the Phusion U Hot Start DNA Polymerase kit (F-555S, Thermo Fisher Scientific), and specific primers. PCR products were electrophoresed and visualized in GelRed Nucleic Acid (Biotium, Fremont, CA, USA) stained gels (2% agarose) under UV light. The resulting bands were sequenced by Sanger and quantified by a modified version of EditR [29]. Primers will be provided upon request.
Statistical analysis
Statistical analysis was performed using GraphPad Prism software. A descriptive analysis was done to analyze the sample distribution with a D’Agostino normality test. A two-sided unpaired Student’s t-test or Mann–Whitney U-test were used according to sample distribution.
Results
In silico identification of CpGs hypermethylated in HCC
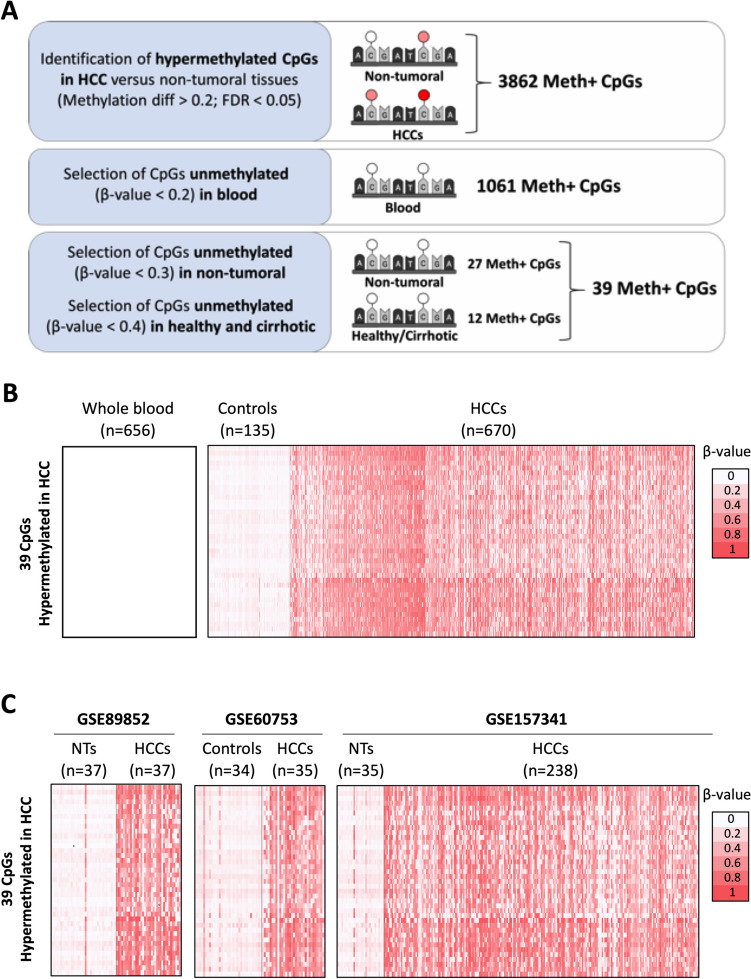
To identify CpGs differentially methylated in HCC, we used three available liver tissue methylomes: GSE56588 (224 HCC, 9 cirrhotic livers, 10 controls), GSE54503 (66 HCC, 66 peritumoral liver samples), and TCGA-LIHC (380 HCC and 50 peritumoral liver samples), all analyzed using Illumina's Infinium HumanMethylation450 BeadChip array (Supplementary Figure S1A). Hierarchical clustering distinguished two groups, separating controls from patients across all studies (Supplementary Figure S1B). UMAP dimensionality reduction similarly clustered HCC and control liver samples together (Supplementary Figure S1C), indicating minimal batch effect. We therefore decided to integrate the methylome data of the three datasets resulting in 670 HCCs and 135 controls. Focusing on CGIs, and consistent with the literature [15], we observed global hypermethylation enrichment in HCC patients versus controls (p-value = 4.31E-28; Supplementary Figure S1D). We identified 3862 CpGs hypermethylated in HCC compared to controls, with a mean methylation difference > 0.2 and FDR < 0.05 (Student's two-sided T-test with Benjamini–Hochberg correction; Fig. 1A, Supplementary Table S1).
Fig. 1.
In silico identification of CpGs hypermethylated in HCC. A Schematic representation of the workflow followed to identify the list of 39 CpGs hypermethylated in HCC but unmethylated in control liver, cirrhotic tissue or whole blood. B, Heatmaps reporting the methylation levels of the 39 CpGs across GSE56588, GSE54503, TCGA-LIHC, GSE40279 datasets, involving 656 healthy individuals' whole blood, 135 liver controls, and 670 HCCs. The 39 CpGs are ranked from the highest to lowest mean methylation difference. C Validation datasets GSE89852, GSE60753 and GSE157341. The CpGs are ranked as in panel B. Color scale bar is shown for reference
To identify those CpGs methylated mainly in HCC cells we eliminated marks potentially originating from circulating blood cells. We excluded all CpGs methylated (β-value > 0.2) in the whole blood of at least one of the 656 healthy individuals covering a wide age range (aged 19 to 101) analyzed in GSE40279. The resulting list was reduced to 1061 CpGs methylated in HCC tissues but not in any of the blood samples (Fig. 1A, Supplementary Table S2). Moreover, none of these 1061 CpGs were part of the 353 CpG sites constituting the aging clock [21], ruling out the possibility of an age-related methylation effect in the identified CpGs.
From the 1061 CpGs hypermethylated in hepatic cells, we identified (a) 27 CpGs unmethylated (β-value < 0.2) in all 135 non-tumoral samples (healthy, cirrhotic and adjacent non-tumoral tissue) with a methylation difference > 0.3 in HCC; moreover, (b) 12 CpGs unmethylated (β-value < 0.2) in livers not harboring a tumor (all the healthy and cirrhotic patients) and methylated in liver tissue adjacent to HCC and in HCC, with a difference > 0.4. Finally, we selected a set of 39 CpGs that were hypermethylated (β-value > 0.3) in HCC but unmethylated (β-value < 0.2) in control liver, cirrhotic tissue or whole blood (Fig. 1B, Supplementary Table S3).
Supporting an association with malignant transformation rather than with liver damage development, none of the 39 CpGs were hypermethylated in livers from obese, NAFLD, NASH, primary biliary cirrhosis, primary sclerosing cholangitis, or cirrhotic patients (GSE61258, GSE48325 and GSE60753; Supplementary Figure S2A).
Accordingly, using independent available methylomes (GSE60753, GSE89852 and GSE157341) we confirmed that all 39 CpGs were hypermethylated in HCC tissues compared to non-tumoral samples (Fig. 1C). Indeed, each CpGs was methylated in at least 54% of the 977 HCC tissues analyzed, ranging from 54.70% to 84.25% (Supplementary Figure S2B).
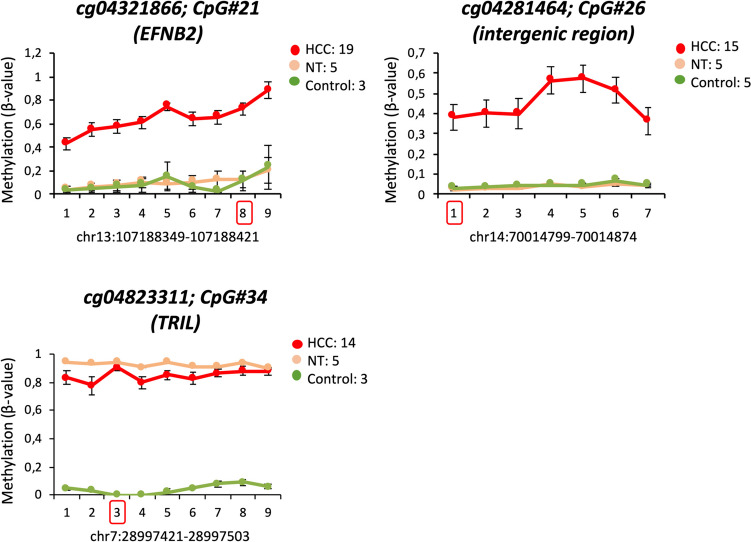
Moreover, we experimentally confirmed the higher methylation level of three selected CpGs in different HCC samples compared to control liver and paired non-tumoral tissues. Consistent with our criteria, two CpGs (cg04321866 and cg04281464) were hypermethylated in HCC compared to both healthy liver and non-tumoral tissue, while the third CpG (cg04823311) was hypermethylated in both HCC and non-tumoral tissue but not in healthy liver samples (Fig. 2). Interestingly, this validation revealed that not only the CpG interrogated in the Infinium array and selected in silico, but all CpGs within each PCR-amplified fragment were hypermethylated in HCC samples (Fig. 2). This result suggests that hypermethylation of these CpGs may play a role in HCC development.
Fig. 2.
Hypermethylation of three candidate CpGs in human HCC and control liver tissues. Graphs show β-values of cg04321866 (CpG#21; EFNB2), cg04281464 (CpG#26; intergenic region), and cg04823311 (CpG#34; TRIL) across HCC samples (n = 19), non-tumoral tissues (NT, n = 5), and control livers (n = 5). PCR amplification and Sanger sequencing were used to analyze methylation across all CpGs within the DNA fragment, with the candidate CpG indicated by a red square
Differential methylation of the CpGs hypermethylated in HCC in other tumors
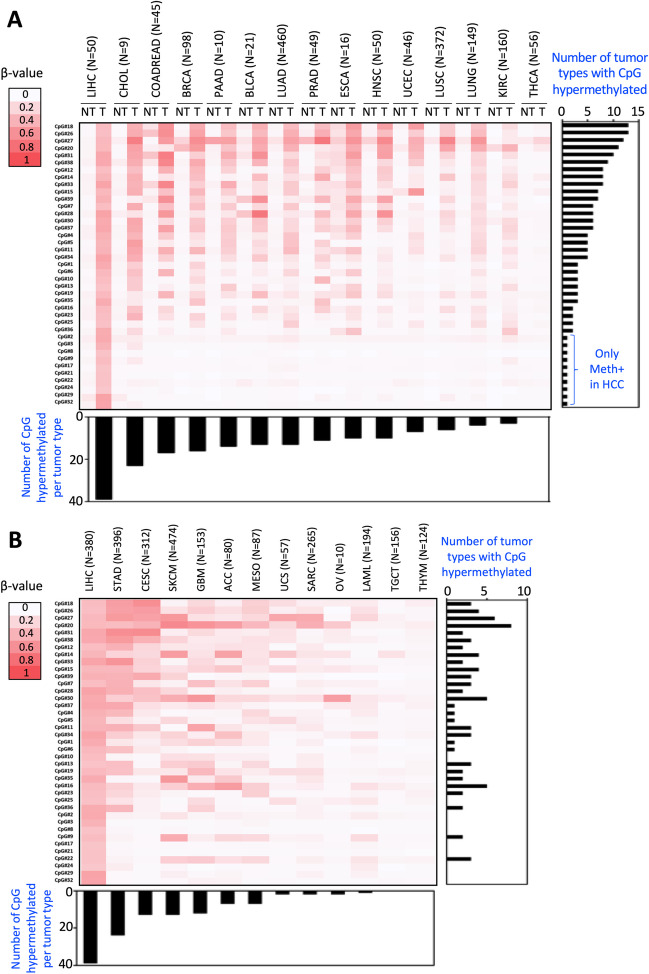
At this point we wondered whether the methylation of these CpGs was a specific feature of HCC cells (Supplementary Figure S2C), or a general characteristic of cancer cells. To address this issue, we first examined the methylation status of the 39 CpGs in healthy tissues to establish their baseline physiological methylation status. We took advantage of 14 TCGA methylomes with more than 5 peritumoral samples (759 non-tumoral samples distributed across 12 different tissues, in addition to liver; Supplementary Table S4). Thirty-two of the 39 CpGs showed no methylation (mean β-value < 0.2) in any of the tissues examined (Fig. 3A). Additionally, six CpGs (CpG#20, CpG#26, CpG#28, CpG#31, CpG#33, and CpG#39) exhibited methylation (mean β-value > 0.2) in only one of the analyzed tissues, while one CpG (CpG#27) was methylated (mean β-value > 0.2) in five tissues (Fig. 3A). These results suggest that, similar to liver and whole blood, these CpGs are predominantly unmethylated in healthy tissues.
Fig. 3.
Methylation levels of the identified hypermethylated CpGs in HCC across various non-tumoral and tumoral samples from different tumor types. A Heatmap displays the mean methylation levels of the 39 CpGs in non-tumoral (NT) and tumoral tissues (T) from TCGA datasets, including LIHC (Hepatocellular Carcinoma), CHOL (Cholangiocarcinoma), COADREAD (Colorectal Adenocarcinoma), BRCA (Breast Invasive Carcinoma), PAAD (Pancreatic Adenocarcinoma), BLCA (Bladder Urothelial Carcinoma), LUAD (Lung Adenocarcinoma), PRAD (Prostate Adenocarcinoma), ESCA (Esophageal Carcinoma), HNSC (Head and Neck Squamous Cell Carcinoma), UCEC (Uterine Corpus Endometrial Carcinoma), LUSC (Lung Squamous Cell Carcinoma), LUNG (Pan-Lung Cancer), KIRC (Kidney Renal Clear Cell Carcinoma), and THCA (Thyroid Carcinoma). CpGs are ranked by the number of tumors showing a mean methylation difference greater than 0.2 (from most to least), and tumors are organized from left to right based on the number of CpGs hypermethylated (from most to least). B Heatmap reporting the mean methylation level of the same CpGs in 13 tumor types with only methylation data of the tumoral tissues (T) from TCGA: LIHC, STAD (Stomach Adenomarcinoma), CESC (Cervical Squamous Cell Carcinoma and Endocervical Adenocarcinoma), SKCM (Skin Cutaneous Melanoma), GBM (Glioblastoma Multiforme), ACC (Adrenocortical Carcinoma), MESO (Mesothelioma), UCS (Uterine Carcinosarcoma), SARC (Sarcoma), OV (Ovarian Serous Cystadenocarcinoma), LAML (Acute Myeloid Leukemia), TGCT (Testicular Germ Cell Tumors) and THYM (Thymoma). CpGs are ranked as in panel A, and tumors are arranged based on the number of hypermethylated CpGs (from most to least) from left to right. The color scale bar is provided on the left side
Considering that these CpGs were practically unmethylated in healthy tissues, we further examined whether these CpGs were hypermethylated in their corresponding tumor tissues. Our analysis revealed that five CpGs (CpG#18, CpG#26, CpG#27, CpG#20 and CpG#31) were hypermethylated in 10 or more tumor types compared to their corresponding control tissues (Fig. 3A). This suggests that the methylation of these CpGs may be a widespread change in carcinogenesis. Conversely, ten CpGs (CpG#2, CpG#3, CpG#8, CpG#9, CpG#17, CpG#21, CpG#22, CpG#24, CpG#29, and CpG#32) showed differential methylation exclusively in HCC (Fig. 3A), suggesting that they represent a specific methylation signature of HCC.
In terms of tumor types, cholangiocarcinoma, followed by colorectal adenocarcinoma, breast carcinoma, and pancreatic adenocarcinoma, exhibited the highest number of hypermethylated CpGs compared to their corresponding controls (23, 17, 16 and 14 CpGs out of the 39, respectively; Fig. 3A). In contrast, lung squamous cell carcinoma, lung adenocarcinoma, and kidney renal clear cell carcinoma were the tumors with fewer hypermethylated CpGs compared to control samples (6, 4 and 3, respectively; Fig. 3A). Notably, thyroid carcinoma did not show hypermethylation of any of the examined CpGs (Fig. 3A).
Additionally, the methylation status of these 39 CpGs was assessed across 13 tumor types from TCGA database where non-tumor sample methylation data were unavailable (Supplementary Table S4). While differential methylation compared to controls could not be confirmed, their methylation status in tumor tissues was established. The five CpGs identified as hypermethylated in more than ten tumors (CpG#18, CpG#26, CpG#27, CpG#20 and CpG#31; Fig. 3A) were methylated in three, four, six, eight and two of these tumor types, respectively (Fig. 3B). Importantly, among the ten CpGs exclusively hypermethylated in HCC (CpG#2, CpG#3, CpG#8, CpG#9, CpG#17, CpG#21, CpG#22, CpG#24, CpG#29, and CpG#32; Fig. 3A), eight (CpG#2, CpG#3, CpG#8, CpG#17, CpG#21, CpG#24, CpG#29, and CpG#32) were not methylated in any of the 13 tumor types analyzed (Fig. 3B), reinforcing their specific methylation pattern in HCC. The remaining two CpGs (CpG#9 and CpG#22) were methylated (mean β-value > 0.2) in two and three tumors, respectively (Fig. 3B).
In terms of tumor types, stomach adenocarcinoma, cervical squamous cell carcinoma and endocervical adenocarcinoma, skin cutaneous melanoma, and glioblastoma multiforme showed methylation (mean β-value > 0.2) in more than ten CpG sites (Fig. 3B). Conversely, uterine carcinosarcoma, sarcoma, ovarian serous cystadenocarcinoma, and acute myeloid leukemia exhibited methylation in only two CpG sites, while testicular germ cell tumors and thymoma did not display methylation in any of the CpG sites analyzed (Fig. 3B).
In summary, our results indicate that most of the CpGs hypermethylated in HCC are predominantly unmethylated not only in the normal liver and blood but in the majority of healthy tissues. Additionally, we identified a subset of CpGs specifically hypermethylated in HCC, while many others are hypermethylated across multiple tumor types. Particularly noteworthy are five CpGs hypermethylated in 10 or more tumor types, indicating a non-random mechanism potentially involved in carcinogenesis.
HCC hypermethylated CpGs and gene expression
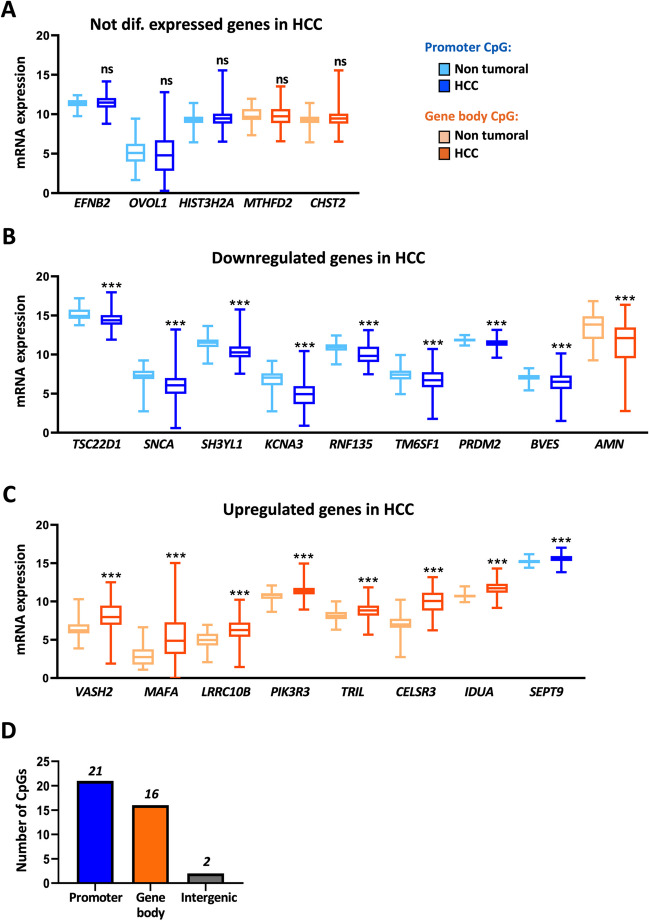
In order to have a general view of the impact of CpG hypermethylation on gene expression, we decided to examine the expression levels of the genes containing the selected CpGs in tumor HCC samples and adjacent control liver tissues from the TCGA-LIHC database. The 39 CpG sites were located in 32 distinct genes and two intergenic regions not uniformly distributed across the genome (Supplementary Table S3), as they were predominantly found on the larger chromosomes, with six of them in chromosome 1 (Supplementary Figure S3). Out of the 32 genes, ten genes (MIXL1, INSM2, HIST1H3F, INA, PYY, MIR129-2, HOXA11, PITX3, CELF6 and MCIDAS) were not expressed in either control liver or HCC tissue samples and five genes (EFNB2, MTHFD2, OVOL1, HIST3H2A and CHST2) showed no differences in expression between HCC and non-tumoral samples (Fig. 4A). However, the other 17 genes were significantly differentially expressed (Fig. 4B-C). The expression of nine genes (TSC22D1, SNCA, SH3YL1, KCNA3, RNF135, TM6SF1, PRDM2, BVES and AMN) was reduced (Fig. 4B), while that of eight genes (VASH2, MAFA, LRRC10B, PIK3R3, TRIL, CELSR3, IDUA and SEPT9) was increased (Fig. 4C) in HCC compared to control livers. Of note, although these changes were statistically significant, in most cases the differences in the expression levels between control livers and HCC tissues were really small, questioning their biological relevance.
Fig. 4.
Correlation of DNA methylation, CpG location and gene expression. A-C Graphs show gene expression levels (log CPM from RNA-seq data) of genes that are not differentially expressed (A), downregulated (B), or upregulated (C) in hepatocellular carcinoma (HCC) compared to non-tumoral tissue, based on TCGA-LIHC data (50 NT and 380 HCC samples). Statistical significance (***p < 0.001) is indicated for each comparison. (D) Distribution of the 39 CpGs categorized by their location in promoters (blue), gene bodies (orange), or intergenic regions (grey) within CpG islands (CGIs). The promoter region includes 1500 nucleotides upstream of the transcription start site (TSS1500) to 300 nucleotides downstream of the TSS
In order to gain mechanistic insight regarding these seemingly arbitrary patterns of gene expression modulation, we decided to examine the location of the CpG sites along the respective gene sequence. It is well-known that promoter CGI hypermethylation represses transcription [43, 45], whereas hypermethylation at gene body CGIs activates gene expression [6, 55]. We found that in addition to the two CpGs located in intergenic regions, 21 CpGs were located within promoter CGIs, while the remaining 16 were within gene body CGIs (Fig. 4D, Supplementary Table S3). In agreement with the literature, genes whose expression was downregulated in HCC had the hypermethylated CpGs located in promoter CGIs, whereas the upregulated genes had hypermethylated CpGs located in gene body CGIs. We observed two exceptions, AMN and SEPT9, whose CpGs were located in the gene body and the promoter CGIs respectively but their expression was reduced and induced (Fig. 4B-C, Table 1). Remarkably, within the genes that were not expressed and those that showed no difference in expression between non tumoral and HCC samples, we found CpG sites in CGIs located in both promoter and gene body regions (Fig. 4A, Table 1). This result highlights a complex interplay between DNA methylation, gene expression, and tumorigenesis in HCC, suggesting that other regulatory mechanisms may influence the expression of these genes and that the role of differential methylation in these regions remains to be determined.
Table 1.
Table reporting the number of CpGs and genes hypermethylated in HCC versus non-tumoral tissue from the TCGA-LIHC database
| Nº genes expressed | ||||||
|---|---|---|---|---|---|---|
| Nº CpGs | Nº genes | Nº genes not expressed in liver & HCC | Not diff exp HCC/Liver |
Downreg HCC/Liver |
Upreg HCC/Liver |
|
| Total | 39 | 32 | 10 | 5 | 9 | 8 |
| Promoter | 21 | 17 | 5 | 3 | 8 | 1 |
| Gene body | 16 | 15 | 5 | 2 | 1 | 7 |
| Intergenic | 2 | 0 | ||||
Genes specifically hypermethylated in HCC were not expressed, or were expressed at low levels, in the normal liver
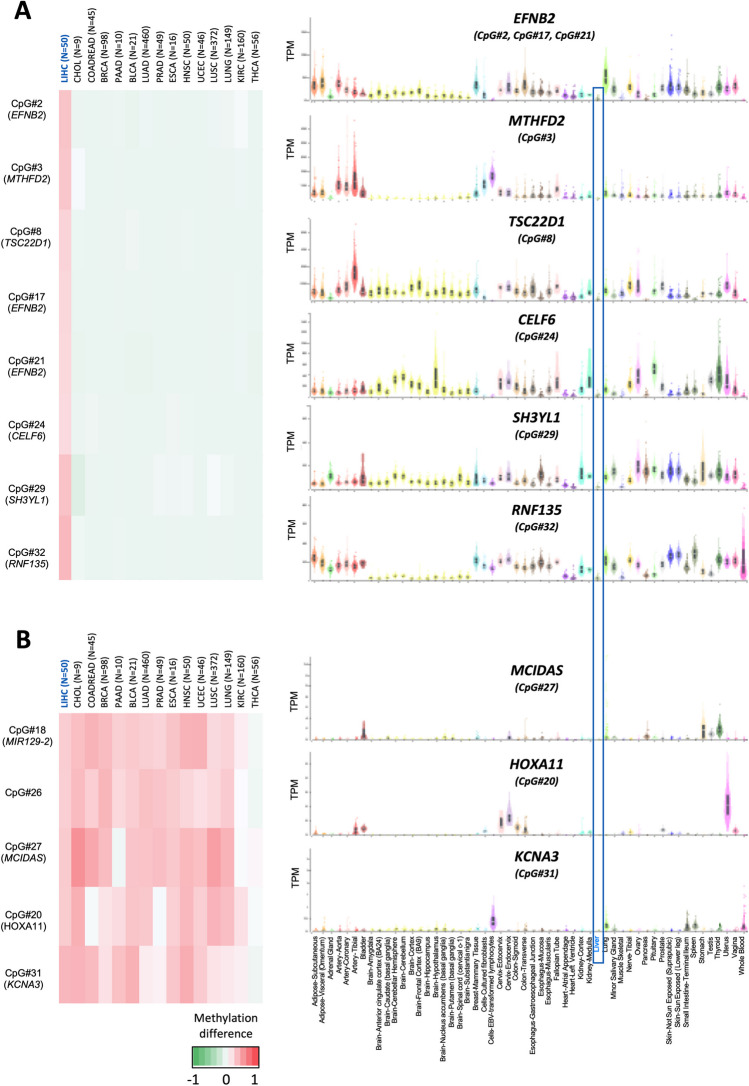
At this point, focusing on the six genes that are specifically hypermethylated in HCC (Fig. 5A-right), and noting that one of them is not expressed in either liver or HCC (CELF6), two others are not associated with changes in expression (EFNB2 and MTHFD2), and the remaining three are slightly downregulated in HCC (TSC22D1, SH3YL1 and RNF135), we questioned whether this hypermethylation status may indeed have an impact on gene expression. In this regard, while a substantial body of literature supports the association of DNA methylation with the regulation of gene expression and its implication in tumor progression [6, 26, 45, 55], it has also been proposed that the majority of hypermethylated genes in cancer are genes already transcriptionally repressed in the pre-cancerous tissue [48, 49]. Moreover, it has been shown that genes specifically repressed in one tissue are prone to be hypermethylated in the corresponding tumor, which may help distinguishing the tissue of origin of the tumor [48, 49]. To investigate this, we examined the expression of these genes in control liver tissue and compared it with their expression in other tissues using the GTEx database. We found that the expression of the genes hypermethylated in HCC (Fig. 5A-right) was markedly lower in liver tissue compared to other healthy tissues (Fig. 5A-left), suggesting that these genes specifically hypermethylated in HCC are also specifically repressed in the normal liver.
Fig. 5.
Methylation and expression of genes specifically hypermethylated in HCC or in 10 or more tumors. (Right) Heatmap showing the mean methylation difference of the eight CpGs specifically hypermethylated in HCC (EFNB2, MTHFD2, TSC22D1, CELF6, SH3YL1 and RNF135) (A) or the five CpGs hypermethylated in 10 or more tumors (MIR129-2, intergenic region, MCIDAS, HOXA11 and KCNA3) (B) The color scale bar is provided below. (Left) Tissue-wide gene expression profiles across 54 tissues from GTEx are shown in TPM, with the liver highlighted by a blue square
To confirm if as proposed genes hypermethylated in cancer correspond to genes little expressed in the corresponding non-tumoral tissue [48, 49], we decided to examine the expression of the five genes that were hypermethylated in 10 or more tumors (Fig. 5B-right) in different healthy tissues (Fig. 5B-left). Among the five CpGs hypermethylated in 10 or more tumors, only three correspond to coding genes (MCIDAS, HOXA11 and KCNA3). We found that, in agreement with the correlation found in the genes specifically methylated in HCC, these three genes are generally not expressed in healthy tissues (Fig. 5B-left). Interestingly, as mentioned above these three genes are not hypermethylated in thyroid carcinoma (THCA) and at least two of them are expressed in the normal thyroid tissue. Altogether, these findings are in line with the emerging notion that genes normally repressed in a healthy tissue become hypermethylated in the corresponding tumor, a situation that would be at odds with the commonly recognized role of DNA hypermethylation in gene expression regulation.
Discussion
DNA methylation is a key epigenetic modification that regulates gene expression and plays an essential role in cancer development [17, 26]. The explosion of high-throughput analyses in recent decades, including methylome studies, has generated massive amount of data from numerous patients across centers and countries [4]. In oncology, these data have significantly enhanced our understanding on the mechanisms underlying tumorigenesis and facilitated the identification of new therapeutic targets and diagnostic biomarkers [4]. Moreover, the free availability of these datasets enables further analyses, helping to increase our knowledge. However, in general, studies are focused on events within a particular tumor type, leaving uncertainty about whether these changes are specific to that tumor or associated with the general carcinogenesis process. Additionally, DNA methylation changes have been typically studied in gene promoters in association with gene expression alterations, rather than considering a broader view of differential DNA methylation at any CpG site across the genome.
In this study, we identify a set of 39 CpGs located within CGIs in promoter, gene body and intergenic regions that are hypermethylated in HCC. Importantly, our analysis revealed that the 39 CpGs were unmethylated not only in the normal liver and blood, but in hepatic tissues from different liver diseases, supporting the association of these methylation marks with the malignant transformation of the liver rather than with the development of liver damage. We evaluated whether the hypermethylation of the 39 CpGs was common to different tumor types or if it was HCC-specific. The TCGA project includes methylation data on 28 tumor types, with more than 8500 tumor and 750 peritumoral samples, allowing to study whether the methylation patterns identified are tissue-specific, cancer-related or cancer-specific. This analysis firstly revealed that the 39 CpGs were also unmethylated in most non-tumoral tissues, being therefore ubiquitously unmethylated CpGs in physiological conditions. When we analyzed whether these 39 CpGs were methylated in other tumors, we identified a group of methylation sites that were common to many tumor types, while others were specific to HCC. Of the CpGs methylated in numerous tumors, five (CpG#18, CpG#26, CpG#27, CpG#20 and CpG#31) were notably hypermethylated in ten or more tumor types analyzed. CpG#26 was located in an intergenic region and the other four CpGs were located in the MIR129-2, MCIDAS, HOXA11/HOXA11-AS and KCNA3 genes. In agreement with our findings, MIR-129–2 has been reported as hypermethylated not only in HCC [34], but also in gastric [2], breast [37] or esophageal cancer [35]. HOXA-11 was found hypermethylated in HCC [23] and also in lung [57], glioblastoma [46], or endometrial [53] carcinoma. Similarly, KCNA3 was shown as hypermethylated in esophageal squamous cell carcinoma [9], colorectal cancer [7] or oropharyngeal squamous cell carcinoma [42]. However, MCIDAS methylation has been only associated with colorectal cancer, being shown hypermethylated in serrated polyps, likely colorectal cancer precursors [5], and identified as one of the 23 DNA-methylation sites proposed to predict progression in patients with colorectal cancer [11]. In our analysis, we found hypermethylation of MCIDAS in HCC, cholangiocarcinoma, and colorectal, breast, prostate, pancreas, lung, esophagus or head and neck carcinomas, among others.
Additionally, our study reveals eight CpGs specifically hypermethylated in HCC and located in six genes, EFNB2 (CpG#2, CpG#17, CpG#21), MTHFD2 (CpG#3), TSC22D1 (CpG#8), CELF6 (CpG#24), SH3YL1 (CpG#29) and RNF135 (CpG#32). All these genes, except CELF6, were also identified as hypermethylated in HCC by Song et al. [47]. Moreover, EFNB2 [19] and RNF135 [51] were described hypermethylated in HCC in two additional studies. In contrast, in another study CELF6 was found hypomethylated instead of hypermethylated in HCC [54]. However, and according to our data, there are no studies describing the methylation of these genes in other tumors, with the exception of one publication describing the hypermethylation of CELF6 in oral squamous cell carcinoma [28] and that of MTHFD2 in esophageal carcinoma [52]. Altogether, and in agreement with previous reports [58], our analysis identified common and tumor-specific epigenetic events.
Another aim of our study was to assess the impact of these methylation changes on gene expression. Importantly, although we selected 39 single CpGs, our validation process revealed that hypermethylation in HCC occurs not only in the selected CpG, but also in the surrounding CpGs within the amplified PCR fragments suggesting a role in gene expression regulation. In this regard, it is widely accepted that the level of methylation in the regions known as CGI regulates gene expression, and that the location of these CGIs determines the direction of this regulation [6, 43, 45, 55]. As expected, and in agreement with the literature [6, 43, 45, 55], we found hypermethylated CpGs located within promoter CGIs that correlated with downregulation of gene expression and hypermethylated CpGs located in gene body CGIs associated with gene transcription activation. However, the changes in gene expression were really small. Moreover, and unexpectedly, among the 32 hypermethylated genes, we found ten that were not expressed in either liver or HCC, and five that despite being hypermethylated did not show any change in expression in HCC. In fact, it has been described that aberrant DNA methylation in cancer occurs in genes normally repressed in the corresponding normal tissues [48, 49], and importantly, that genes repressed in a specific tissue are prone to hypermethylation in cancers derived from that tissue [48, 49]. Our results are in line with these notions, as we found that the genes hypermethylated in several tumors were either not expressed or minimally expressed in control livers and other healthy tissues. However, the expression of the six genes (EFNB2, MTHFD2, TSC22D1, CELF6, SH3YL1, and RNF135) which exhibited DNA hypermethylation exclusively in HCC and not in other tumor types, was markedly low in liver tissue compared to other extrahepatic healthy tissues, suggesting a specific transcriptional repression in the liver.
All these findings raise intriguing questions about the role of DNA methylation in gene expression regulation and its implication in cancer development. They support the hypothesis that hypermethylation may be a “passenger” event, reflecting epigenetic dysregulation in cancer rather than contributing to its development [48, 49]. While it appears that hypermethylation does not have a significant impact on gene expression, particularly in genes that are already transcriptionally repressed, another question arises as to whether this methylation occurs randomly across CpG sites. However, in line with previous studies [14, 26] our results support that hypermethylation across multiple tumor types occurs predominantly in genes that are specifically repressed in the tissue of origin, suggesting a non-random pattern of methylation and a possible role in the epigenetic regulation of cancer. For instance, we cannot exclude that these marks remain as passengers reflecting other epigenetic changes in the tumor. Moreover, those marks could also impact the expression of distant genes through the modulation of chromatin architecture or the recruitment of chromatin and gene expression modulators. Finally, we can speculate a mechanistic role in transformation, and this hypermethylation could be required to ensure the repression of normally not expressed genes, which might otherwise interfere with the malignant transformation process if activated. Irrespective of their function, tumor hypermethylation marks may provide insights into their tissue of origin, and therefore have implications for the development of tissue-specific biomarkers, liquid biopsy approaches and targeted therapies.
In summary, further to the identification of CpGs specifically hypermethylated in HCC our study provides new data concerning the complex interplay between DNA methylation, gene expression, and tumorigenesis. This work underscores the need for further studies aimed at elucidating the underlying mechanisms and functional consequences of cancer-wide and tumor type-specific epigenetic alterations in cancer.
It categorizes these findings based on gene expression status (not expressed, not differentially expressed, downregulated, upregulated) and the location within CpG islands (CGIs).
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We particularly acknowledge the patients for their participation and the Biobank of the University of Navarra for its collaboration.
Abbreviations
- BRCA
Breast carcinoma
- CESC
Cervical squamous cell carcinoma and endocervical adenocarcinoma
- CGI
CpG Island
- COADREAD
Colorectal adenocarcinoma
- FDR
False discovery rate
- GBM
Glioblastoma multiforme
- GTEx
Genotype-Tissue Expression
- HCC
Hepatocellular carcinoma
- HM450
HumanMethylation450 BeadChip array
- KIRC
Kidney renal clear cell carcinoma
- LIHC
Liver hepatocellular carcinoma
- LAML
Acute myeloid leukemia
- LUNG
Lung adenocarcinoma
- LUSC
Lung squamous cell carcinoma
- NAFLD
Non-alcoholic fatty liver disease
- NASH
Non-alcoholic steatohepatitis
- OV
Ovarian serous cystadenocarcinoma
- PCR
Polymerase Chain Reaction
- SARC
Sarcoma
- SKCM
Skin cutaneous melanoma
- STAD
Stomach adenocarcinoma
- TCGA
The Cancer Genome Atlas
- THCA
Thyroid carcinoma
- THYM
Thymoma
- TGCT
Testicular germ cell tumors
- UCS
Uterine carcinosarcoma
- UMAP
Uniform manifold approximation and projection
Authors’ contribution
Conceptualization: C.B., M.A.; Bioinformatics: I.B., M.R, F.D, J.M.H, M.A.; Tissue collection: M.I., M.C., A.C-G., B.S.; DNA extraction and PCR: I.B., M.R., M.E.; Data analysis and interpretation: I.B, M.R, M.F.L., C.B., M.A; Drafting the article: C.B., M.A. Review & editing: I.B, M.R, M.G.F-B., B.S., M.A.A., M.F.L. All authors reviewed and approved the final manuscript for submission. The authors declare that all data were generated in-house and that no paper mill was used.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. Grants PI22/00471 funded by Instituto de Salud Carlos III (ISCIII) and co-funded by the European Union, PI19/00613 funded by Instituto de Salud Carlos III (ISCIII) cofinanced by ‘Fondo Europeo de Desarrollo Regional’ (FEDER) ‘Una Manera de Hacer Europa’ and AECC investigador fellowship INVES223049AREC to MA; MCIN FPI fellowship to MR (BES-2017–079883); Ramón y Cajal Program contract RYC2018-024475–1 from the Spanish Ministry of Science, Innovation and University-co-funded by ESF to MGF-B.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Human ethics and consent to participate declarations
Not applicable.
Conflict of interest
BS reports consultancy fees from Adaptimmune, Astra Zeneca, Bayer, BMS, Boston Scientific, Eisai, Eli Lilly, Incyte, Ipsen, Novartis, MSD, Roche, Sanofi, Sirtex Medical, Terumo; speaker fees from Astra Zeneca, Bayer, BMS, Eisai, Eli Lilly, Incyte, Ipsen, Novartis, Roche, Sirtex Medical, Terumo; research grants (to the Institution) from BMS and Sirtex Medical. Rest of the authors have nothing to declare.
Footnotes
Keypoints
1. We identified 39 CpGs specifically hypermethylated in HCC compared to normal liver tissues and other liver diseases.
2. Among them, a subset of CpGs were commonly hypermethylated in several tumor types, while others were specific to HCC, highlighting a possible role as biomarkers.
3. DNA hypermethylation has no effect or minimally impacts gene expression.
4. DNA hypermethylation predominantly occurs in genes specifically repressed in the normal tissue of origin.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Carmen Berasain, Email: cberasain@unav.es.
María Arechederra, Email: macalderon@unav.es.
References
- 1.Ahrens M, Ammerpohl O, von Schönfels W, Kolarova J, Bens S, Itzel T, Teufel A, Herrmann A, Brosch M, Hinrichsen H, Erhart W, Egberts J, Sipos B, Schreiber S, Häsler R, Stickel F, Becker T, Krawczak M, Röcken C, Siebert R, Schafmayer C, Hampe J (2013) DNA Methylation Analysis in Nonalcoholic Fatty Liver Disease Suggests Distinct Disease-Specific and Remodeling Signatures after Bariatric Surgery. Cell Metab 18:296–302. 10.1016/j.cmet.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 2.Alizadeh N, Asadi M, Shanehbandi D, Zafari V, Shomali N, Asvadi T, Sepehri B (2020) Evaluation of the Methylation of MIR129-2 Gene in Gastric Cancer. J Gastrointest Cancer 51:267–270. 10.1007/s12029-019-00239-4 [DOI] [PubMed] [Google Scholar]
- 3.Ally A, Balasundaram M, Carlsen R, Chuah E, Clarke A, Dhalla N, Holt RA, Jones SJM, Lee D, Ma Y, Marra MA, Mayo M, Moore RA, Mungall AJ, Schein JE, Sipahimalani P, Tam A, Thiessen N, Cheung D, Wong T, Brooks D, Robertson AG, Bowlby R, Mungall K, Sadeghi S, Xi L, Covington K, Shinbrot E, Wheeler DA, Gibbs RA, Donehower LA, Wang L, Bowen J, Gastier-Foster JM, Gerken M, Helsel C, Leraas KM, Lichtenberg TM, Ramirez NC, Wise L, Zmuda E, Gabriel SB, Meyerson M, Cibulskis C, Murray BA, Shih J, Beroukhim R, Cherniack AD, Schumacher SE, Saksena G, Pedamallu CS, Chin L, Getz G, Noble M, Zhang H, Heiman D, Cho J, Gehlenborg N, Saksena G, Voet D, Lin P, Frazer S, Defreitas T, Meier S, Lawrence M, Kim J, Creighton CJ, Muzny D, Doddapaneni H, Hu J, Wang M, Morton D, Korchina V, Han Y, Dinh H, Lewis L, Bellair M, Liu X, Santibanez J, Glenn R, Lee S, Hale W, Parker JS, Wilkerson MD, Hayes DN, Reynolds SM, Shmulevich I, Zhang W, Liu Y, Iype L, Makhlouf H, Torbenson MS, Kakar S, Yeh MM, Jain D, Kleiner DE, Jain D, Dhanasekaran R, El-Serag HB, Yim SY, Weinstein JN, Mishra L, Zhang J, Akbani R, Ling S, Ju Z, Su X, Hegde AM, Mills GB, Lu Y, Chen J, Lee J-S, Sohn BH, Shim JJ, Tong P, Aburatani H, Yamamoto S, Tatsuno K, Li W, Xia Z, Stransky N, Seiser E, Innocenti F, Gao J, Kundra R, Zhang H, Heins Z, Ochoa A, Sander C, Ladanyi M, Shen R, Arora A, Sanchez-Vega F, Schultz N, Kasaian K, Radenbaugh A, Bissig K-D, Moore DD, Totoki Y, Nakamura H, Shibata T, Yau C, Graim K, Stuart J, Haussler D, Slagle BL, Ojesina AI, Katsonis P, Koire A, Lichtarge O, Hsu T-K, Ferguson ML, Demchok JA, Felau I, Sheth M, Tarnuzzer R, Wang Z, Yang L, Zenklusen JC, Zhang J, Hutter CM, Sofia HJ, Verhaak RGW, Zheng S, Lang F, Chudamani S, Liu J, Lolla L, Wu Y, Naresh R, Pihl T, Sun C, Wan Y, Benz C, Perou AH, Thorne LB, Boice L, Huang M, Rathmell WK, Noushmehr H, Saggioro FP, Tirapelli DP da C, Junior CGC, Mente ED, Silva O de C, Trevisan FA, Kang KJ, Ahn KS, Giama NH, Moser CD, Giordano TJ, Vinco M, Welling TH, Crain D, Curley E, Gardner J, Mallery D, Morris S, Paulauskis J, Penny R, Shelton C, Shelton T, Kelley R, Park J-W, Chandan VS, Roberts LR, Bathe OF, Hagedorn CH, Auman JT, O’Brien DR, Kocher J-PA, Jones CD, Mieczkowski PA, Perou CM, Skelly T, Tan D, Veluvolu U, Balu S, Bodenheimer T, Hoyle AP, Jefferys SR, Meng S, Mose LE, Shi Y, Simons JV, Soloway MG, Roach J, Hoadley KA, Baylin SB, Shen H, Hinoue T, Bootwalla MS, Berg DJVD, Weisenberger DJ, Lai PH, Holbrook A, Berrios M, Laird PW (2017) Comprehensive and Integrative Genomic Characterization of Hepatocellular Carcinoma. Cell 169:1327-1341.e23. 10.1016/j.cell.2017.05.046 [DOI] [PMC free article] [PubMed]
- 4.Alyass A, Turcotte M, Meyre D (2015) From big data analysis to personalized medicine for all: challenges and opportunities. BMC Méd Genom 8:33. 10.1186/s12920-015-0108-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andrew A, Baron J, Butterly L, Suriawinata A, Tsongalis G, Robinson C, Amos C (2017) Hyper-Methylated Loci Persisting from Sessile Serrated Polyps to Serrated Cancers. Int J Mol Sci 18:535. 10.3390/ijms18030535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arechederra M, Daian F, Yim A, Bazai SK, Richelme S, Dono R, Saurin AJ, Habermann BH, Maina F (2018) Hypermethylation of gene body CpG islands predicts high dosage of functional oncogenes in liver cancer. Nat Commun 9:3164. 10.1038/s41467-018-05550-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bacolod MD, Mirza AH, Huang J, Giardina SF, Feinberg PB, Soper SA, Barany F (2020) Application of Multiplex Bisulfite PCR–Ligase Detection Reaction–Real-Time Quantitative PCR Assay in Interrogating Bioinformatically Identified, Blood-Based Methylation Markers for Colorectal Cancer. J Mol Diagn 22:885–900. 10.1016/j.jmoldx.2020.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergman Y, Cedar H (2013) DNA methylation dynamics in health and disease. Nat Struct Mol Biol 20:274–281. 10.1038/nsmb.2518 [DOI] [PubMed] [Google Scholar]
- 9.Bian Y, Gao Y, Lu C, Tian B, Xin L, Lin H, Zhang Y, Zhang X, Zhou S, Wan K, Zhou J, Li Z, Chen H, Wang L (2023) Genome-wide methylation profiling identified methylated KCNA3 and OTOP2 as promising diagnostic markers for esophageal squamous cell carcinoma. Chin Méd J. 10.1097/cm9.0000000000002832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Carvalho DD, Sharma S, You JS, Su S-F, Taberlay PC, Kelly TK, Yang X, Liang G, Jones PA (2012) DNA Methylation Screening Identifies Driver Epigenetic Events of Cancer Cell Survival. Cancer Cell 21:655–667. 10.1016/j.ccr.2012.03.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deng Y, Wan H, Tian J, Cheng X, Rao M, Li J, Zhang H, Zhang M, Cai Y, Lu Z, Li Y, Niu S, Shen N, Chang J, Fang Z, Zhong R (2020) CpG-methylation-based risk score predicts progression in colorectal cancer. Epigenomics 12:605–615. 10.2217/epi-2019-0300 [DOI] [PubMed] [Google Scholar]
- 12.Dor Y, Cedar H (2018) Principles of DNA methylation and their implications for biology and medicine. Lancet 392:777–786. 10.1016/s0140-6736(18)31268-6 [DOI] [PubMed] [Google Scholar]
- 13.Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG (1999) Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59:793–797 [PubMed] [Google Scholar]
- 14.Fan S, Tang J, Li N, Zhao Y, Ai R, Zhang K, Wang M, Du W, Wang W (2019) Integrative analysis with expanded DNA methylation data reveals common key regulators and pathways in cancers. npj Genom Med 4:2. 10.1038/s41525-019-0077-8 [DOI] [PMC free article] [PubMed]
- 15.Fernández-Barrena MG, Arechederra M, Colyn L, Berasain C, Avila MA (2020) Epigenetics in hepatocellular carcinoma development and therapy: The tip of the iceberg. Jhep Reports 2:100167. 10.1016/j.jhepr.2020.100167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gifford CA, Ziller MJ, Gu H, Trapnell C, Donaghey J, Tsankov A, Shalek AK, Kelley DR, Shishkin AA, Issner R, Zhang X, Coyne M, Fostel JL, Holmes L, Meldrim J, Guttman M, Epstein C, Park H, Kohlbacher O, Rinn J, Gnirke A, Lander ES, Bernstein BE, Meissner A (2013) Transcriptional and Epigenetic Dynamics during Specification of Human Embryonic Stem Cells. Cell 153:1149–1163. 10.1016/j.cell.2013.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanahan D (2022) Hallmarks of Cancer: New Dimensions. Cancer Discov 12:31–46. 10.1158/2159-8290.cd-21-1059 [DOI] [PubMed] [Google Scholar]
- 18.Hannum G, Guinney J, Zhao L, Zhang L, Hughes G, Sadda S, Klotzle B, Bibikova M, Fan J-B, Gao Y, Deconde R, Chen M, Rajapakse I, Friend S, Ideker T, Zhang K (2013) Genome-wide Methylation Profiles Reveal Quantitative Views of Human Aging Rates. Mol Cell 49:359–367. 10.1016/j.molcel.2012.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hernandez-Meza G, Felden J, Gonzalez-Kozlova EE, Garcia-Lezana T, Peix J, Portela A, Craig AJ, Sayols S, Schwartz M, Losic B, Mazzaferro V, Esteller M, Llovet JM, Villanueva A (2021) DNA Methylation Profiling of Human Hepatocarcinogenesis. Hepatology 74:183–199. 10.1002/hep.31659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hlady RA, Tiedemann RL, Puszyk W, Zendejas I, Roberts LR, Choi J-H, Liu C, Robertson KD (2014) Epigenetic signatures of alcohol abuse and hepatitis infection during human hepatocarcinogenesis. Oncotarget 5:9425–9443. 10.18632/oncotarget.2444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Horvath S (2013) DNA methylation age of human tissues and cell types. Genome Biol 14:3156. 10.1186/gb-2013-14-10-r115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horvath S, Erhart W, Brosch M, Ammerpohl O, von Schönfels W, Ahrens M, Heits N, Bell JT, Tsai P-C, Spector TD, Deloukas P, Siebert R, Sipos B, Becker T, Röcken C, Schafmayer C, Hampe J (2014) Obesity accelerates epigenetic aging of human liver. Proc Natl Acad Sci 111:15538–15543. 10.1073/pnas.1412759111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hou X, Peng J-X, Hao X-Y, Cai J-P, Liang L-J, Zhai J-M, Zhang K-S, Lai J-M, Yin X-Y (2014) DNA Methylation Profiling Identifies EYA4 Gene as a Prognostic Molecular Marker in Hepatocellular Carcinoma. Ann Surg Oncol 21:3891–3899. 10.1245/s10434-013-3401-z [DOI] [PubMed] [Google Scholar]
- 24.Illingworth RS, Gruenewald-Schneider U, Webb S, Kerr ARW, James KD, Turner DJ, Smith C, Harrison DJ, Andrews R, Bird AP (2010) Orphan CpG islands identify numerous conserved promoters in the mammalian genome. Plos Genet 6:e1001134. 10.1371/journal.pgen.1001134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones PA (2012) Functions of DNA methylation: islands, start sites, gene bodies and beyond. Nat Rev Genet 13:484–492. 10.1038/nrg3230 [DOI] [PubMed] [Google Scholar]
- 26.Jones PA, Baylin SB (2002) The fundamental role of epigenetic events in cancer. Nat Rev Genet 3:415–428. 10.1038/nrg816 [DOI] [PubMed] [Google Scholar]
- 27.Kalari S, Pfeifer GP (2010) 10 Identification of Driver and Passenger DNA Methylation in Cancer by Epigenomic Analysis. Adv Genet 70:277–308. 10.1016/b978-0-12-380866-0.60010-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khor GH, Froemming GRA, Zain RB, Abraham TM, Lin TK (2016) Involvement of CELSR3 Hypermethylation in Primary Oral Squamous Cell Carcinoma. Asian Pac J Cancer Prev 17:219–223. 10.7314/apjcp.2016.17.1.219 [DOI] [PubMed] [Google Scholar]
- 29.Kluesner MG, Nedveck DA, Lahr WS, Garbe JR, Abrahante JE, Webber BR, Moriarity BS (2018) EditR: A Method to Quantify Base Editing from Sanger Sequencing. CRISPR J 1:239–250. 10.1089/crispr.2018.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuramoto J, Arai E, Tian Y, Funahashi N, Hiramoto M, Nammo T, Nozaki Y, Takahashi Y, Ito N, Shibuya A, Ojima H, Sukeda A, Seki Y, Kasama K, Yasuda K, Kanai Y (2017) Genome-wide DNA methylation analysis during non-alcoholic steatohepatitis-related multistage hepatocarcinogenesis: comparison with hepatitis virus-related carcinogenesis. Carcinogenesis 38:261–270. 10.1093/carcin/bgx005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liang W-W, Lu RJ-H, Jayasinghe RG, Foltz SM, Porta-Pardo E, Geffen Y, Wendl MC, Lazcano R, Kolodziejczak I, Song Y, Govindan A, Demicco EG, Li X, Li Y, Sethuraman S, Payne SH, Fenyö D, Rodriguez H, Wiznerowicz M, Shen H, Mani DR, Rodland KD, Lazar AJ, Robles AI, Ding L, Consortium CPTA, Aguet F, Akiyama Y, An E, Anand S, Anurag M, Babur O, Bavarva J, Birger C, Birrer M, Calinawan A, Cantley LC, Cao S, Carr S, Ceccarelli M, Chan D, Chinnaiyan A, Cho H, Chowdhury S, Cieslik M, Clauser K, Colaprico A, Zhou DC, Leprevost F da V, Day C, Dhanasekaran M, Domagalski M, Dou Y, Druker B, Edwards N, Ellis M, Selvan ME, Francis A, Getz G, Gillette MA, Robles TG, Gosline S, Gümüş Z, Heiman D, Hiltke T, Hong R, Hostetter G, Hu Y, Huang C, Huntsman E, Iavarone A, Jaehnig E, Jewel S, Ji J, Jiang W, Johnson JL, Katsnelson L, Ketchum K, Krug K, Kumar-Sinha C, Lei J, Liao Y, Lindgren C, Liu T, Liu W, Ma W, Rodrigues FM, McKerrow W, Mesri M, Nesvizhskii AI, Newton C, Oldroyd R, Omenn G, Paulovich A, Petralia F, Pugliese P, Reva B, Ruggles K, Rykunov D, Satpathy S, Savage S, Schadt E, Schnaubelt M, Schraink T, Shi Z, Smith D, Song X, Stathias V, Storrs E, Tan J, Terekhanova N, Thangudu R, Thiagarajan M, Tignor N, Wang J, Wang L-B, Wang P, Wang Y (Cindy), Wen B, Wu Y, Yao L, Yaron TM, Yi X, Zhang B, Zhang H, Zhang Q, Zhang X, Zhang Z, Chan DW, Dhanasekaran SM, Schürer S, Smith RD, Wyczalkowski MA (2023) Integrative multi-omic cancer profiling reveals DNA methylation patterns associated with therapeutic vulnerability and cell-of-origin. Cancer Cell 41:1567-1585.e7. 10.1016/j.ccell.2023.07.013 [DOI] [PMC free article] [PubMed]
- 32.Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J, Finn RS (2021) Hepatocellular carcinoma Nat Rev Dis Primers 7:6. 10.1038/s41572-020-00240-3 [DOI] [PubMed] [Google Scholar]
- 33.Loyfer N, Magenheim J, Peretz A, Cann G, Bredno J, Klochendler A, Fox-Fisher I, Shabi-Porat S, Hecht M, Pelet T, Moss J, Drawshy Z, Amini H, Moradi P, Nagaraju S, Bauman D, Shveiky D, Porat S, Dior U, Rivkin G, Or O, Hirshoren N, Carmon E, Pikarsky A, Khalaileh A, Zamir G, Grinbaum R, Gazala MA, Mizrahi I, Shussman N, Korach A, Wald O, Izhar U, Erez E, Yutkin V, Samet Y, Golinkin DR, Spalding KL, Druid H, Arner P, Shapiro AMJ, Grompe M, Aravanis A, Venn O, Jamshidi A, Shemer R, Dor Y, Glaser B, Kaplan T (2023) A DNA methylation atlas of normal human cell types. Nature 613:355–364. 10.1038/s41586-022-05580-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lu C, Lin K, Tien M, Wu C, Uen Y, Tseng T (2013) Frequent DNA methylation of MiR-129-2 and its potential clinical implication in hepatocellular carcinoma. Genes, Chromosom Cancer 52:636–643. 10.1002/gcc.22059 [DOI] [PubMed] [Google Scholar]
- 35.Macedo-Silva C, Constâncio V, Miranda-Gonçalves V, Leite-Silva P, Salta S, Lobo J, Guimarães R, Carvalho-Maia C, Gigliano D, Farinha M, Sousa O, Henrique R, Jerónimo C (2023) DNA methylation biomarkers accurately detect esophageal cancer prior and post neoadjuvant chemoradiation. Cancer Med 12:8777–8788. 10.1002/cam4.5623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Malpeli G, Innamorati G, Decimo I, Bencivenga M, Kamdje AHN, Perris R, Bassi C (2019) Methylation Dynamics of RASSF1A and Its Impact on Cancer. Cancers 11:959. 10.3390/cancers11070959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mao X, Ye Q, Zhang G, Jiang J, Zhao H, Shao Y, Ye Z, Xuan Z, Huang P (2021) Identification of differentially methylated genes as diagnostic and prognostic biomarkers of breast cancer. World J Surg Oncol 19:29. 10.1186/s12957-021-02124-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maor G, Yearim A, Ast G (2015) The alternative role of DNA methylation in splicing regulation. Trends Genet 31:274–280. 10.1016/j.tig.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 39.Maunakea AK, Nagarajan RP, Bilenky M, Ballinger TJ, D’Souza C, Fouse SD, Johnson BE, Hong C, Nielsen C, Zhao Y, Turecki G, Delaney A, Varhol R, Thiessen N, Shchors K, Heine VM, Rowitch DH, Xing X, Fiore C, Schillebeeckx M, Jones SJM, Haussler D, Marra MA, Hirst M, Wang T, Costello JF (2010) Conserved role of intragenic DNA methylation in regulating alternative promoters. Nature 466:253–257. 10.1038/nature09165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meunier L, Hirsch TZ, Caruso S, Imbeaud S, Bayard Q, Roehrig A, Couchy G, Nault J, Llovet JM, Blanc J, Calderaro J, Zucman-Rossi J, Letouzé E (2021) DNA Methylation Signatures Reveal the Diversity of Processes Remodeling Hepatocellular Carcinoma Methylomes. Hepatology 74:816–834. 10.1002/hep.31796 [DOI] [PubMed] [Google Scholar]
- 41.Recalde M, Gárate-Rascón M, Herranz JM, Elizalde M, Azkona M, Unfried JP, Boix L, Reig M, Sangro B, Fernández-Barrena MG, Fortes P, Ávila MA, Berasain C, Arechederra M (2022) DNA Methylation Regulates a Set of Long Non-Coding RNAs Compromising Hepatic Identity during Hepatocarcinogenesis. Cancers 14:2048. 10.3390/cancers14092048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ren S, Gaykalova D, Wang J, Guo T, Danilova L, Favorov A, Fertig E, Bishop J, Khan Z, Flam E, Wysocki PT, DeJong P, Ando M, Liu C, Sakai A, Fukusumi T, Haft S, Sadat S, Califano JA (2018) Discovery and development of differentially methylated regions in human papillomavirus-related oropharyngeal squamous cell carcinoma. Int J Cancer 143:2425–2436. 10.1002/ijc.31778 [DOI] [PubMed] [Google Scholar]
- 43.Robertson KD (2005) DNA methylation and human disease. Nat Rev Genet 6:597–610. 10.1038/nrg1655 [DOI] [PubMed] [Google Scholar]
- 44.Shen J, Wang S, Zhang Y-J, Wu H-C, Kibriya MG, Jasmine F, Ahsan H, Wu D, Siegel AB, Remotti H, Santella RM (2013) Exploring genome-wide DNA methylation profiles altered in hepatocellular carcinoma using Infinium HumanMethylation 450 BeadChips. Epigenetics 8:34–43. 10.4161/epi.23062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Siegfried Z, Eden S, Mendelsohn M, Feng X, Tsuberi B-Z, Cedar H (1999) DNA methylation represses transcription in vivo. Nat Genet 22:203–206. 10.1038/9727 [DOI] [PubMed] [Google Scholar]
- 46.Skiriutė D, Vaitkienė P, Ašmonienė V, Steponaitis G, Deltuva VP, Tamašauskas A (2013) Promoter methylation of AREG, HOXA11, hMLH1, NDRG2, NPTX2 and Tes genes in glioblastoma. J Neuro-Oncol 113:441–449. 10.1007/s11060-013-1133-3 [DOI] [PubMed] [Google Scholar]
- 47.Song M-A, Tiirikainen M, Kwee S, Okimoto G, Yu H, Wong LL (2013) Elucidating the Landscape of Aberrant DNA Methylation in Hepatocellular Carcinoma. PLoS ONE 8:e55761. 10.1371/journal.pone.0055761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sproul D, Kitchen RR, Nestor CE, Dixon JM, Sims AH, Harrison DJ, Ramsahoye BH, Meehan RR (2012) Tissue of origin determines cancer-associated CpG island promoter hypermethylation patterns. Genome Biol 13:R84. 10.1186/gb-2012-13-10-r84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sproul D, Nestor C, Culley J, Dickson JH, Dixon JM, Harrison DJ, Meehan RR, Sims AH, Ramsahoye BH (2011) Transcriptionally repressed genes become aberrantly methylated and distinguish tumors of different lineages in breast cancer. Proc Natl Acad Sci 108:4364–4369. 10.1073/pnas.1013224108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Villanueva A, Portela A, Sayols S, Battiston C, Hoshida Y, Méndez-González J, Imbeaud S, Letouzé E, Hernandez-Gea V, Cornella H, Pinyol R, Solé M, Fuster J, Zucman-Rossi J, Mazzaferro V, Esteller M, Llovet JM, Consortium H (2015) DNA methylation-based prognosis and epidrivers in hepatocellular carcinoma: HEPATOLOGY, Vol. XX, No. X, 2015. Hepatology 61:1945–1956. 10.1002/hep.27732 [DOI] [PubMed]
- 51.Wang X, Chen M, Liang X, Bai Y, Zeng J, Xu X, Li H, Wang J, Fan K, Zhao G (2022) RNF135 Promoter Methylation Is Associated With Immune Infiltration and Prognosis in Hepatocellular Carcinoma. Front Oncol 11:752511. 10.3389/fonc.2021.752511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang J, Luo J, Sun Z, Sun F, Kong Z, Yu J (2020) Identification of MTHFD2 as a novel prognosis biomarker in esophageal carcinoma patients based on transcriptomic data and methylation profiling. Medicine 99:e22194. 10.1097/md.0000000000022194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Whitcomb BP, Mutch DG, Herzog TJ, Rader JS, Gibb RK, Goodfellow PJ (2003) Frequent HOXA11 and THBS2 promoter methylation, and a methylator phenotype in endometrial adenocarcinoma. Clin cancer Res : Off J Am Assoc Cancer Res 9:2277–2287 [PubMed] [Google Scholar]
- 54.Xie Z, Dang Y, Wu H, He R, Ma J, Peng Z, Rong M, Li Z, Yang J, Jiang Y, Chen G, Yang L (2020) Effect of CELSR3 on the Cell Cycle and Apoptosis of Hepatocellular Carcinoma Cells. J Cancer 11:2830–2844. 10.7150/jca.39328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang X, Han H, De Carvalho DD, Lay FD, Jones PA, Liang G (2014) Gene Body Methylation Can Alter Gene Expression and Is a Therapeutic Target in Cancer. Cancer Cell 26:577–590. 10.1016/j.ccr.2014.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang S, He S, Zhu X, Wang Y, Xie Q, Song X, Xu C, Wang W, Xing L, Xia C, Wang Q, Li W, Zhang X, Yu J, Ma S, Shi J, Gu H (2023) DNA methylation profiling to determine the primary sites of metastatic cancers using formalin-fixed paraffin-embedded tissues. Nat Commun 14:5686. 10.1038/s41467-023-41015-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang Y, Yuan Y, Li Y, Zhang P, Chen P, Sun S (2019) An inverse interaction between HOXA11 and HOXA11-AS is associated with cisplatin resistance in lung adenocarcinoma. Epigenetics 14:949–960. 10.1080/15592294.2019.1625673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang C, Zhao H, Li J, Liu H, Wang F, Wei Y, Su J, Zhang D, Liu T, Zhang Y (2015) The Identification of Specific Methylation Patterns across Different Cancers. PLoS ONE 10:e0120361. 10.1371/journal.pone.0120361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu T, Liu J, Beck S, Pan S, Capper D, Lechner M, Thirlwell C, Breeze CE, Teschendorff AE (2022) A pan-tissue DNA methylation atlas enables in silico decomposition of human tissue methylomes at cell-type resolution. Nat Methods 19:296–306. 10.1038/s41592-022-01412-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.