Abstract
The initial six months following HIV infection have a high viral load. Nonspecific presentations might lead to the missing primary HIV diagnosis. Multiorgan and multisystem diagnosis is a rare presentation of primary HIV.
A 40-year-old male patient with no documented comorbidities presented with bilateral flank pain. The onset of the pain was gradual, characterized as dull and aching, with radiation toward the groin. The patient also had severe pain in the left shoulder and left ankle region. Per-abdominal examination revealed bilateral flank tenderness, with the right side being more tender than the left. Swelling of the left shoulder and ankle was observed, accompanied by tenderness and a restricted range of motion.
Contrast-enhanced computed tomography of the chest and abdomen revealed bilateral pyelonephritis multiple renal abscesses and liver abscesses. Left shoulder septic arthritis was also present. Pus culture and blood culture were positive for methicillin-sensitive Staphylococcus aureus. Antibiotics, according to the culture sensitivity, were given, and retroviral therapy was started from the antiretroviral clinic.
Primary HIV infection can present with a variety of signs and symptoms. This case demonstrates that AIDS can affect any organ and mimic other disease processes. The initial clinical picture might be confused with individually occurring diseases; therefore, we should consider AIDS in patients presenting with multiorgan failure. Early initiation of empiric and then culture-specific antibiotics along with antiretroviral therapy helps in the rapid improvement of the patient and controls the high viremia. The infected patient also needs appropriate counseling on ways to avoid high-risk behavior, which may prevent transmission of HIV.
Keywords: abscess, hiv-infected patients, immunocompromised patient, multiorgan, renal abscess
Introduction
Primary HIV infection (PHI) in the acute setting presents nonspecific symptoms and complicates the diagnosis [1]. The typical clinical presentation of PHI usually occurs two to four weeks after exposure to the virus and most commonly presents as fever, pharyngitis, and adenopathy. Therefore, the early diagnosis might be missed by the clinical picture, given these nonspecific symptoms [2]. Rapid diagnosis of PHI prevents unknowing virus transmission during periods of high viral load [1]. Establishing an early diagnosis is crucial for the individual and public health. Herein, we present a case of PHI with multiorgan and multisystem involvement. This article was previously presented at the 2021 Urological Society of India Annual Conference on February 12, 2021.
Case presentation
A 40-year-old male patient with no documented comorbidities presented with bilateral flank pain. The onset of the pain was gradual, characterized as dull and aching, with radiation toward the groin. The patient also had severe pain in the left shoulder and ankle region. There was a history of occasional smoking and drinking. There was no history of fever, chills, hematuria, previous surgery, respiratory complaints, or decreased urine output. The patient and relatives denied any history of illicit drug abuse.
General physical examinations were within normal limits. Per-abdominal investigation revealed bilateral flank tenderness, more on the right than on the left. Left shoulder and ankle swelling were present, with tenderness and a restricted range of motion. No apparent enlarged lymph nodes were present.
Blood tests showed hemoglobin of 7.3 g/dL and a total leukocyte count of 5,200/mm3. Liver and kidney function tests were within normal limits. Hepatitis B surface antigen and hepatitis C virus serology were negative. However, HIV serology came to be positive. On further evaluation, the absolute CD4 count was 68 cells/mm3, and the percentage of T helper cells CD4 was 9.2%, respectively.
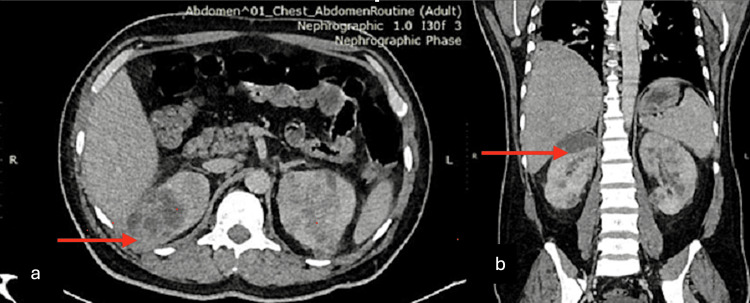
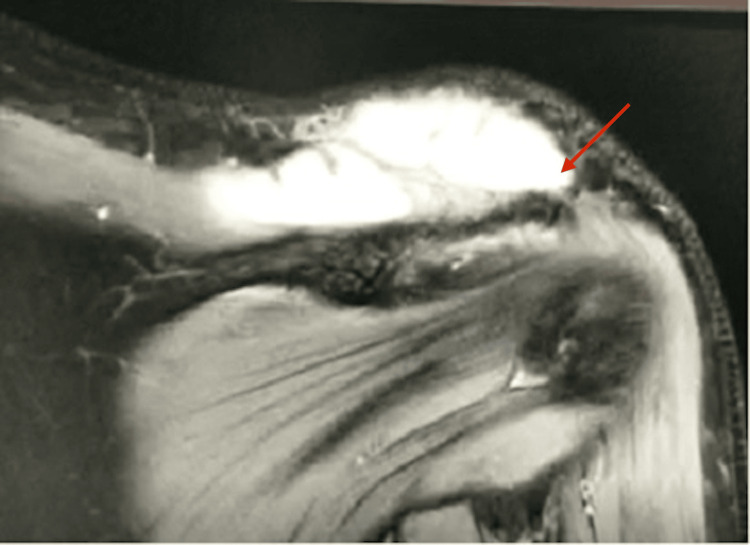
Contrast-enhanced computed tomography of the chest and abdomen revealed bilateral pyelonephritis and multiple renal abscesses with the largest size, 7.2 x 4.3 x 2.4 cm, at the upper pole of the right kidney (Figure 1). It also showed an enlarged liver (23.4 cm in craniocaudal) with few peripherally enhancing hypodense lesions suggestive of abscesses and mild right-sided pleural with fissural extension with underlying basal atelectasis. Ultrasound of the left shoulder joint depicted an ill-defined heteroechoic collection with free-floating internal echoes in the acromioclavicular joint, causing significant joint space widening. The left ankle showed multifocal ill-defined hypoechoic intramuscular groups with internal echoes involving the deep muscles of the ankle, the largest measuring 10 x 5 cm along the medial aspect. MRI was done for the left shoulder and ankle, which further revealed irregular multiloculated peripherally enhancing collections measuring 7.7 x 9.1 x 3.3 cm with epicenter at the acromioclavicular joint with superior extension up to the subcutaneous plane, causing a focal bulge (Figure 2). Inferior-medial extension into the intramuscular plane between the trapezius and supraspinatus muscle and anteroinferior extension into the clavicular part of the deltoid muscle were also noticed.
Figure 1. CECT abdomen. Axial (a) and coronal (b) images showing right upper pole renal abscess and multiple other renal abscesses in bilateral kidneys (arrows represent the areas of abscesses).
CECT: contrast-enhanced computed tomography
Figure 2. MRI of the left shoulder, showing an irregular collection in the left acromioclavicular joint (arrow represents the area of collection).
The patient was started on broad-spectrum antibiotics. USG-guided aspiration of pus from the right renal abscess, liver abscess, and left shoulder joint was done. Pus culture and blood culture were positive for methicillin-sensitive Staphylococcus aureus sensitive to amoxiclav, tetracycline, linezolid, and vancomycin. Tuberculosis acid-fast bacillus and cartridge-based nucleic acid amplification tests were negative. Fungal culture was also negative. Repeat aspiration of residual abscesses in the upper pole of the right kidney and left ankle joint was done. Vancomycin was started empirically, which was continued following the culture sensitivity report. Antiretroviral therapy (ART) was started with a fixed drug combination of tenofovir /lamivudine/dolutegravir. Echocardiography was also done, which showed a normal study. No vegetation was found. A prophylactic antibiotic (trimethoprim-sulfamethoxazole combination) was created because of a low CD4 count. After aspiration, with culture-sensitive antibiotics and ART, the patient continued to improve and was discharged on day 12. The patient is on regular follow-ups in the ART clinic, orthopedics, and urology.
Discussion
The first six months following HIV exposure is the PHI period [3]. The initial six months have a high viral load, which the host immune system subsequently limits. Without ART, there is a gradual decline in CD4 T cells. Viral dissemination is rapid in this period, and viral reservoirs form throughout the body. This is why ART cannot cure HIV infection [3]. Symptoms take two to six weeks to appear.
The presentations of primary HIV can be the following:
1) the most common is a flu-like illness, including fever, cough, lymphadenopathy, and myalgias [4], which occurs in 65%-95%;
2) neurological presentations, including aseptic meningitis and facial nerve paresis [4];
3) multiorgan involvement, including renal infarcts, renal failure, myocarditis, and pancreatitis [2];
4) multiorgan abscess and septic arthritis as in this index case.
The acute presentations may be nonspecific, making the diagnosis challenging [1]. A delay in diagnosis results in a higher rate of disease progression and rapid fall in CD4 T cells. This also increases the chances of opportunistic infections. The Strategic Timing of the Antiretroviral Treatment trial concluded that immediate initiation of ART benefits all patients [5].
PHI can have a bizarre clinical presentation. Paño-Pardo et al. presented a case of a 19-year-old female patient with PHI with an unusual presentation of fever, rhabdomyolysis, myocarditis, pancreatitis, bilateral renal infarcts, anemia, and acute kidney injury. The patient improved on antibiotics [2]. Tattevin et al. reported a case of a 16-year-old woman with an unusual presentation of sepsis, leukopenia, myocarditis, and rhabdomyolysis during PHI [6].
This index patient presented with multiorgan and multisystem abscesses. Renal and liver abscesses with septic arthritis of the left acromioclavicular joint and left ankle were seen in the index patient and managed. The entire presentation may be due to PHI, as no other predisposing factors existed. S. aureus bacteremia has a higher incidence among patients with HIV. The risk is related to the CD4+T cell counts and is highest in patients with CD4 counts <200 cells/mm3. Bacteremia can be classified as complicated or noncomplicated, particularly in patients with metastatic sites of infection, as was present in this index patient having both renal and liver abscesses. Patients may also present with persistent systemic inflammatory response syndrome and cardiovascular dysfunction [7].
Patients who develop AIDS are at increased risk of unusual kidney infections with agents like Candida, Mycobacteria, Salmonella, and Pneumocystis pneumonia. Renal Candida infections can result in fungal ball formation in the collecting system, leading to hydronephrosis. A staphylococcal renal abscess can also be present and repeatedly occur, leading to nephrectomy. Renal tuberculosis can also be seen in 6%-23% of cases of patients with HIV and may require antituberculosis agents for six to nine months. Therefore, the patient should undergo testing for tuberculosis and fungal infections to rule out additional conditions [8].
A retrospective analysis of 18 patients with septic arthritis with HIV showed that three patients in their study were diagnosed with HIV after admission for septic arthritis. The mean CD4+T cell count was 154/mm3. S. aureus cultures were present in seven patients, streptococcal in six patients, coagulase-negative Staphylococcus in two patients, Neisseria gonorrhoeae in one patient, and Mycobacterium tuberculosis in three patients. The culture was monomicrobial in 17 patients and polymicrobial in one patient. Fever was present in 18 patients in this study. Three patients who had adjacent osteomyelitis with septic arthritis underwent debridement and drainage procedures [9]. The index patient in this study had polyarticular septic arthritis, which should also be suspected in patients having a CD4+T cell count of less than 200 cells/mm3. The patient also had cultures positive for S. aureus.
These microbiological data show that S. aureus is a common pathogen in HIV patients and should always be covered in initial empiric antibiotic therapy. Although the index patient in this study has methicillin-sensitive S. aureus, many studies have reported an increased incidence of methicillin-resistant S. aureus in HIV-infected patients [10,11]. A high index of suspicion should be present for opportunistic pathogens. Therefore, any purulent aspirated material should be sent for mycobacterial and fungal cultures. This is necessary for patients having a CD4+T cell count of less than 200 cells/mm3 [9].
Early diagnosis is crucial to prevent virus transmission to uninfected sexual partners. Knowledge of HIV also limits transmission with more frequent use of condoms. The principle of treatment-as-prevention refers to using ART to reduce the viral load and decrease the chances of transmission [12].
Conclusions
PHI can present with a variety of signs and symptoms. It should be kept in the differential diagnosis of patients with multiorgan and multisystem involvement. Primary HIV should be differential for such presentation besides tuberculosis, autoimmune pathology, etc. Early initiation of broad-spectrum empiric (based on local hospital antibiotic policy) and then culture-specific antibiotics along with ART helps in the rapid improvement of the patient and controls the high viremia. The infected patient also needs appropriate counseling on ways to avoid high-risk behavior, which may prevent the transmission of HIV.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Deepak Kumar, Gurpremjit J. Singh, Ankur Mittal, Harshit Agarwal
Acquisition, analysis, or interpretation of data: Deepak Kumar, Vikas Panwar
Drafting of the manuscript: Deepak Kumar, Gurpremjit J. Singh, Vikas Panwar
Critical review of the manuscript for important intellectual content: Ankur Mittal, Harshit Agarwal
References
- 1.Primary HIV type 1 infection. Kassutto S, Rosenberg ES. Clin Infect Dis. 2004;38:1447–1453. doi: 10.1086/420745. [DOI] [PubMed] [Google Scholar]
- 2.Primary HIV infection with multisystemic presentation. Paño-Pardo JR, Alcaide ML, Abbo L, Dickinson G. Int J Infect Dis. 2009;13:0–80. doi: 10.1016/j.ijid.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Primary HIV infection: a medical and public health emergency requiring rapid specialist management. Fidler S, Fox J. Clin Med Lond Engl. 2016;16:180–183. doi: 10.7861/clinmedicine.16-2-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Primary HIV infection: clinical presentation, testing, and treatment. Henn A, Flateau C, Gallien S. Curr Infect Dis Rep. 2017;19:37. doi: 10.1007/s11908-017-0588-3. [DOI] [PubMed] [Google Scholar]
- 5.Initiation of antiretroviral therapy in early asymptomatic HIV infection. Lundgren JD, Babiker AG, Gordin F, et al. N Engl J Med. 2015;373:795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Multiple organ failure during primary HIV infection. Tattevin P, Camus C, Arvieux C, Ruffault A, Michelet C. Clin Infect Dis. 2007;44:0–9. doi: 10.1086/510683. [DOI] [PubMed] [Google Scholar]
- 7.Septic pulmonary emboli and renal abscess caused by Staphylococcus aureus in an HIV-infected patient. Medina-Piñón I, Reyes-Mondragón AL, Martínez-Reséndez MF, Camacho-Ortiz A. Case Rep Infect Dis. 2018;2018:1460283. doi: 10.1155/2018/1460283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The urological management of the patient with acquired immunodeficiency syndrome. Heyns CF, Fisher M. BJU Int. 2005;95:709–716. doi: 10.1111/j.1464-410X.2004.05435.x. [DOI] [PubMed] [Google Scholar]
- 9.Septic arthritis in patients with human immunodeficiency virus. Zalavras CG, Dellamaggiora R, Patzakis MJ, Bava E, Holtom PD. Clin Orthop Relat Res. 2006;451:46–49. doi: 10.1097/01.blo.0000229305.97888.17. [DOI] [PubMed] [Google Scholar]
- 10.The incidence of and risk factors for MRSA bacteraemia in an HIV-infected cohort in the HAART era. Burkey MD, Wilson LE, Moore RD, Lucas GM, Francis J, Gebo KA. HIV Med. 2008;9:858–862. doi: 10.1111/j.1468-1293.2008.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Staphylococcus aureus colonization in a community sample of HIV-infected and HIV-uninfected drug users. Miller M, Cespedes C, Vavagiakis P, Klein RS, Lowy FD. Eur J Clin Microbiol Infect Dis. 2003;22:463–469. doi: 10.1007/s10096-003-0969-4. [DOI] [PubMed] [Google Scholar]
- 12.Antiretroviral treatment of HIV-1 prevents transmission of HIV-1: where do we go from here? Cohen MS, Smith MK, Muessig KE, Hallett TB, Powers KA, Kashuba AD. Lancet. 2013;382:1515–1524. doi: 10.1016/S0140-6736(13)61998-4. [DOI] [PMC free article] [PubMed] [Google Scholar]