Abstract
Glaucoma is a pathologically irreversible eye illness in the realm of ophthalmic diseases. Because it is difficult to detect concealed and non-obvious progressive changes, clinical diagnosis and treatment of glaucoma is extremely challenging. At the same time, screening and monitoring for glaucoma disease progression are crucial. Artificial intelligence technology has advanced rapidly in all fields, particularly medicine, thanks to ongoing in-depth study and algorithm extension. Simultaneously, research and applications of machine learning and deep learning in the field of glaucoma are fast evolving. Artificial intelligence, with its numerous advantages, will raise the accuracy and efficiency of glaucoma screening and diagnosis to new heights, as well as significantly cut the cost of diagnosis and treatment for the majority of patients. This review summarizes the relevant applications of artificial intelligence in the screening and diagnosis of glaucoma, as well as reflects deeply on the limitations and difficulties of the current application of artificial intelligence in the field of glaucoma, and presents promising prospects and expectations for the application of artificial intelligence in other eye diseases such as glaucoma.
Keywords: glaucoma, artificial intelligence, screening, diagnosis, optical coherence tomography
Introduction
Glaucoma is a disease characterized by optic nerve damage and visual field defect, and it is also the world’s first irreversible blinding eye disease (1–3). The main cause of glaucoma is the development of blockage and obstruction of the circulation process of aqueous humor in the eyeball, which leads to increased intraocular pressure (1). Glaucoma is different from other eye diseases in that it has insidious onset and no obvious clinical manifestations and signs in the early stage (4). Therefore, once glaucoma shows the related symptoms, the eye has suffered irreversible and harmful vision reduction and vision loss, and may even lead to blindness, which seriously has a huge impact on the life and health of the population (5, 6). Glaucoma can also lead to many complications that further aggravate eye vision damage, such as infection, fear of light and so on (7, 8). It has to be said that with the increase of many disadvantageous factors including refraction and bad living habits, the prevalence and risk of glaucoma are also gradually increasing (9). Therefore, the screening, diagnosis and treatment of glaucoma are of great significance to human eye health.
In the past, artificial intelligence (AI) was only defined as a kind of science and engineering that made only machines (10, 11). However, with the development of science and technology, artificial intelligence has gradually become the representative word of machine learning and deep learning (12–14). Due to the continuous innovation of deep learning and machine learning technologies, artificial intelligence has made significant progress and has been applied in ophthalmology, cancer diagnosis, drug synthesis, molecular targeting, genomic medicine, proteomics medicine and other fields, especially in image recognition and image diagnosis, and has achieved mature clinical applications (15–17).
The application of artificial intelligence in the field of ophthalmology is very broad, including the diagnosis and screening of a variety of eye diseases (18). This review summarizes the relevant applications of artificial intelligence in the screening and diagnosis of glaucoma, and provides a reliable basis and theory for further clinicians to better formulate treatment plans for glaucoma. At the same time, we have also deeply reflected on the limitations and difficulties of the current application of artificial intelligence in the field of glaucoma. Finally, we put forward good prospects and expectations for the application of artificial intelligence to other eye diseases such as glaucoma.
Application of AI in glaucoma screening
As the prevalence of glaucoma increases, screening for glaucoma in the population is also critical (19). The application of AI-assisted diagnosis technology to realize early screening of glaucoma can avoid visual impairment of glaucoma patients due to early misdiagnosis or missed diagnosis, and reduce the incidence of glaucoma blindness (20, 21). The screening criteria for glaucoma have always emphasized three principles, which are early detection, early diagnosis and early treatment (22). The traditional screening of glaucoma is a diagnosis by means of tonometer and fundus photography combined with clinical experience (23). This model has the disadvantages of low diagnosis pursuit rate and high screening cost (24). A general procedure of screening for glaucoma in Figure 1. The current AI screening system will provide an efficient and fast algorithm mode, which has a higher detection rate and accuracy rate than the traditional glaucoma screening mode. In addition, the AI screening system can also reduce the cost of examination, greatly easing the financial burden of glaucoma patients.
Figure 1.
A general procedure of screening for glaucoma.
At present, the main screening techniques for glaucoma include intraocular pressure examination and fundus photography. In the early screening of glaucoma, AI is mainly combined with fundus photography (25). Fundus photography is the most rapid and simple examination method to determine the optic nerve damage in glaucoma (26). Meanwhile, Intraocular pressure (IOP), as the gold standard for glaucoma screening, can also serve as an important auxiliary diagnostic basis for fundus photography (27). In recent years, great progress has been made in the identification of glaucoma by fundus photography. A recent study suggests that improved artificial intelligence could make screening for glaucoma easier by analyzing color fundus photos in a cost-effective way (28). This study proposes a solution for robust glaucoma screening in response to the difficulty of uneven image distribution and low-quality images and their significant degradation of real-world performance (28). At the same time, a study of a large labeled dataset of fundus photo glaucoma screening conducted by AI from the Netherlands also showed that some of the specific features of glaucoma can be recognized and prepared to be captured by AI (29). In the field of glaucoma screening, the development of AI has greatly improved the safety and effectiveness of glaucoma surgery, but AI still needs to continue to overcome shortcomings in terms of targeting, quantification and accuracy. In order to broaden the application of AI in glaucoma or other eye diseases, current researchers and clinicians can make more efforts to improve the targeting accuracy of AI technology.
Application of AI in glaucoma diagnosis
After screening with AI fundus photography, glaucoma patients need to be referred for further diagnosis (30). Fundus photography is very convenient and economical, which is suitable for assisting large-scale glaucoma screening in areas with backward primary medical system (31). However, further accurate diagnosis still requires the combination of optical coherence tomography (OCT) technology and perimetry results, both of which are objective criteria for determining glaucoma damage (32).
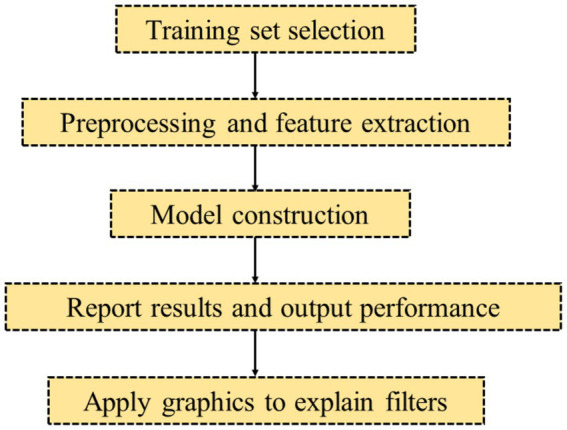
OCT is a retinal and choroidal imaging technology used to diagnose and monitor eye diseases (33). The principle of OCT is to use interferometry to produce the corresponding real-time correct image in Figure 2. At the same time, this lower power diode laser can correctly hit the emitted infrared light on the tissue to a certain extent, and then return it to the fiber interferometer according to the principle of light reflection (34). By adjusting the time of use and the intensity of the backscattered light, OCT can, in some ways, render a two-dimensional image similar to ultrasound (35). In recent years, the research and application of AI in OCT and perimetry have become more in-depth, which has greatly improved the diagnostic efficiency and accuracy of glaucoma. At the same time, there are also studies that combine the diagnosis of OCT and perimetry to analyze the function and structure, respectively, and propose objective criteria for the diagnosis of glaucoma from the structure and function, so as to obtain more reasonable and accurate diagnosis results. Color fundus image data is enhanced by using histogram equalization (HE) and contrast-limited adaptive HE (CLAHE) image processing. Giancarlo Fortino et al. demonstrated that AI can develop hybrid solutions with image processing and deep learning to ensure the best and most appropriate decisions for glaucoma diagnosis (36). Satish K Panda et al. trained a deep learning network to segment 3 neural tissues and 4 connective tissue layers of the optic papilla of glaucoma, confirming that AI can recognize new biomarkers of the optic papilla of glaucoma for the diagnosis of glaucoma to achieve the diagnosis accuracy of glaucoma (37). The diagnosis of glaucoma by OCT combined with AI still needs a long time to be applied to clinical practice, so it still needs more efforts by the majority of scientific researchers to carry out some interdisciplinary work.
Figure 2.
OCT in AI for glaucoma diagnosis.
In addition to not only combining with OCT, AI can also be combined with other technologies and detection methods to achieve the purpose of steadily improving the accuracy of glaucoma diagnosis (38, 39). Previous studies have shown that the application of artificial intelligence has a significant effect on the change pattern of the subbasal nerve and corneal aberrations in patients with glaucoma (40). A recent study from Japan shows that artificial intelligence science estimates the time of tear film rupture and effectively diagnoses the occurrence of glaucoma (41). Moreover, artificial intelligence eyeball biomechanical technology can also be used in the diagnose of glaucoma (42). In the future, the research of AI in glaucoma diagnosis needs to be further developed with multi-modal algorithms, because the multi-modal data makes use of more complete inspection parameters and is more comprehensive, and the use of multi-modal data can make a more accurate diagnosis of glaucoma.
Large language models in the field of glaucoma
The application of large language models (LLM) in the field of glaucoma marks an emerging trend in AI technology in the field of medicine (43). Through deep learning technology, LLM can understand and process a large number of medical text data, such as medical literature, medical records, research reports, etc., thus playing an important role in the diagnosis, treatment and patient management of glaucoma (44). In glaucoma diagnosis, the LLM is able to analyze the patient’s symptoms, history, and test results to provide initial diagnostic recommendations. This helps doctors to judge the condition more accurately, especially in the early identification of high-risk glaucoma patients, the application of LLM has significant value (45). By integrating with electronic medical record system, LLM can automatically extract and analyze medical record data to assist doctors to make more timely diagnosis. In terms of treatment, LLM is able to recommend the appropriate treatment plan for doctors according to the specific situation of patients, combined with the latest medical research results and clinical experience. This not only increases the degree of personalization of treatment plans, but also helps to optimize treatment outcomes and reduce the risk of complications (46). In addition, LLM also plays an important role in the management of glaucoma patients. By building a glaucoma intelligent knowledge base question-and-answer system, LLM is able to provide patients with comprehensive and accurate disease information and self-management recommendations (47). This helps patients to better understand the condition, master self-monitoring and management methods, which can alleviate anxiety to a certain extent and improve the quality of life.
In conclusion, the application of large language models in the field of glaucoma provides a powerful auxiliary tool for doctors, improves the accuracy of diagnosis and the personalized degree of treatment, and provides patients with more convenient and efficient disease management services. With the continuous development and improvement of the technology, the application prospect of LLM in the field of glaucoma will be broader.
Difficulties and challenges in the application of AI in glaucoma
Currently, AI is being used in the screening and diagnosis of glaucoma (48). To some extent, AI can really improve the screening rate and diagnostic accuracy of glaucoma (49). However, there are still many limitations to the full application of AI in glaucoma. First, the vast majority of hospital-based prospective studies enroll a small number of glaucoma subjects and have limited image integration and segmentation for model development (50, 51). The number of subjects is too small for the AI model to overfit the diagnosis and clinical data of glaucoma patients (52). Therefore, before considering the real clinical application of AI and glaucoma, it is necessary to test on more glaucoma patients to calculate the best model, so that later glaucoma-related research can be carried out more smoothly. Most hospitals have different databases for the combination of AI and glaucoma patients (53).
The number of glaucoma patients in each hospital is limited. Due to the differences in the database including available clinical features, it is difficult to improve the screening rate and diagnostic accuracy of glaucoma by using AI in cross-hospital cooperation (54). Therefore, the field of artificial intelligence for glaucoma urgently needs to develop a universal, publicly available database for further research. If such a database is established, data from glaucoma patients worldwide can be used, reducing the limitations and objectivity associated with a limited number of subjects. In addition, the current acceptance of artificial intelligence for disease management is still limited to a small portion of the population, which is also consistent with the small number of subjects (55, 56). Therefore, in order to mature the application of artificial intelligence in the treatment of glaucoma, promoting the development of artificial intelligence has also become a necessary step and process.
It must be emphasized once again that in the application of artificial intelligence in the diagnosis and treatment of eye diseases such as glaucoma, how to ensure the privacy and security of patient data has also become a hot problem that needs to be solved and solutions need to be found (57, 58). The high cost and low throughput of multimodal diagnostics, as well as the need to consider accuracy and specificity while controlling detection costs, are also issues that will require significant time and effort to address in the future. Finally, in the process of clinical screening and diagnosis of glaucoma, the quality of images obtained will be uneven, which to some extent brings unnecessary difficulties to image processing and integration. Therefore, setting a standard for image output is also conducive to the mature application of artificial intelligence in glaucoma screening and treatment.
Further advancement and conclusion
The diagnostic ability of AI in glaucoma has been adequately reflected, and the clinical research has gradually become relatively mature. The establishment of an effective AI combined with fundus photography applied in glaucoma screening mode, supplemented by intraocular pressure detection, can greatly improve its screening efficiency and accuracy, and can widely carry out glaucoma screening in various regions (59, 60). In the future, the AI-guided glaucoma screening model will have many advantages, such as high accuracy, high efficiency, high performance and low cost (61). High-quality databases will also be established in various regions, and high-quality databases can simultaneously feed AI to conduct high-quality training tests to improve the performance of AI algorithms and form a benign closed loop (62, 63). In terms of the realization of AI glaucoma screening and AI-assisted diagnosis of glaucoma, the research on single-mode OCT and perimetry has been gradually improved, but the research based on multi-mode data needs to be developed to improve the efficiency and comprehensiveness of AI in diagnosing glaucoma (64, 65). At the same time, the generalization ability of AI needs to be further improved, and the input of invalid data and parameters needs to be reduced (66). In the future, it is necessary to explore a reasonable standard to compare the heterogeneity of different AI in glaucoma, and comprehensively consider gender, age, number of data sets, and concurrent diseases.
AI is also an important part of the prediction of future glaucoma. It has made some progress in the prediction of glaucoma, and will accurately predict the progress of glaucoma patients in the future (67). At the same time, it also has certain application prospects in the humanized treatment of clinical patients. The collection of sufficient longitudinal data can help doctors design personalized treatment plans for glaucoma patients, such as personalized drug courses or surgical recommendations, and control the IOP of patients at safe target IOP through treatment (68, 69). Finally, through the follow-up results adjustment program, the progress of the disease can be controlled, which brings great help to the prognosis of the disease (70). In the future, A will use its ability to detect characteristic patterns in large data sets to select more suitable therapeutic drugs and surgical methods for patients, so as to better humanized intervention and prognosis of glaucoma progression.
To summarize, by combining fundus imaging, OCT, perimetry, and other technologies, AI has demonstrated significant performance in glaucoma early screening, clinical diagnosis, progression prediction, individualized treatment, and prognosis. However, there are certain limits. The era of intelligent diagnosis and treatment is approaching, owing to advances in science and technology, as well as economic strength. It will be popularized in the field of ophthalmology to promote the reduction of the prevalence of glaucoma in the world, bring benefits to patients with glaucoma, and achieve greater social benefits.
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Natural Science Foundation of China (Nos 82274589, 81973912, China); Beijing Administration of Traditional Chinese Medicine Major Difficult Diseases Traditional Chinese and Western Medicine Collaborative Research Project (No. 2023BJSAYNJBXTGG-010, China); the Science and Technology Innovation Project of China Academy of Chinese Medical Sciences (No. CI2021A02602, China); China Center for Evidence-based Medicine of Traditional Chinese Medicine (No. 2020YJSZX-2, China); and the High level Traditional Chinese Medicine Hospital Project of Eye hospital, China Academy of Chinese Medical Sciences (Nos GSP5-82, GSP4-02-5).
Author contributions
YJ: Conceptualization, Writing – original draft. LL: Conceptualization, Supervision, Writing – review & editing. JL: Writing – original draft. KX: Writing – original draft. WZ: Supervision, Writing – original draft. YL: Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S. Glaucoma. Lancet. (2017) 390:2183–93. doi: 10.1016/S0140-6736(17)31469-1 [DOI] [PubMed] [Google Scholar]
- 2.Ferro Desideri L, Rutigliani C, Corazza P, Nastasi A, Roda M, Nicolo M, et al. The upcoming role of artificial intelligence (AI) for retinal and glaucomatous diseases. J Opt. (2022) 15:S50–7. doi: 10.1016/j.optom.2022.08.001, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang X, Raja H, Madadi Y, Delsoz M, Poursoroush A, Kahook MY, et al. Predicting Glaucoma before onset using a large language model Chatbot. Am J Ophthalmol. (2024) 266:289–99. doi: 10.1016/j.ajo.2024.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiggs JL, Pasquale LR. Genetics of glaucoma. Hum Mol Genet. (2017) 26:R21–7. doi: 10.1093/hmg/ddx184, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chun YS, Sung KR, Park CK, Kim HK, Yoo C, Kim YY, et al. Factors influencing vision-related quality of life according to glaucoma severity. Acta Ophthalmol. (2018) 97:13918. doi: 10.1111/aos.13918 [DOI] [PubMed] [Google Scholar]
- 6.Safa BN, Wong CA, Ha J, Ethier CR. Glaucoma and biomechanics. Curr Opin Ophthalmol. (2022) 33:80–90. doi: 10.1097/ICU.0000000000000829, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aldaas K, Challa P, Weber DJ, Fleischman D. Infections and glaucoma. Surv Ophthalmol. (2021) 67:637–58. doi: 10.1016/j.survophthal.2021.08.009 [DOI] [PubMed] [Google Scholar]
- 8.Vishwaraj CR, Kavitha S, Venkatesh R, Shukla AG, Chandran P, Tripathi S. Neuroprotection in glaucoma. Indian J Ophthalmol. (2022) 70:380–5. doi: 10.4103/ijo.IJO_1158_21, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khawaja AP, Sherratt MA, Sparrow JM, Royal College of Ophthalmologists Glaucoma Commissioning Guidance Development Group . The Royal College of ophthalmologists’ Glaucoma commissioning guidance: executive summary. Eye. (2017) 31:818–22. doi: 10.1038/eye.2017.11, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connor CW. Artificial intelligence and machine learning in anesthesiology. Anesthesiology. (2019) 131:1346–59. doi: 10.1097/ALN.0000000000002694, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mintz Y, Brodie R. Introduction to artificial intelligence in medicine. Minim Invasive Ther Allied Technol. (2019) 28:73–81. doi: 10.1080/13645706.2019.1575882 [DOI] [PubMed] [Google Scholar]
- 12.Gore JC. Artificial intelligence in medical imaging. Magn Reson Imaging. (2020) 68:A1–a4. doi: 10.1016/j.mri.2019.12.006 [DOI] [PubMed] [Google Scholar]
- 13.Gupta R, Srivastava D, Sahu M, Tiwari S, Ambasta RK, Kumar P. Artificial intelligence to deep learning: machine intelligence approach for drug discovery. Mol Divers. (2021) 25:1315–60. doi: 10.1007/s11030-021-10217-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nensa F, Demircioglu A, Rischpler C. Artificial intelligence in nuclear medicine. J Nucl Med. (2019) 60:29s–37s. doi: 10.2967/jnumed.118.220590 [DOI] [PubMed] [Google Scholar]
- 15.Hashimoto DA, Witkowski E, Gao L, Meireles O, Rosman G. Artificial intelligence in anesthesiology: current techniques, clinical applications, and limitations. Anesthesiology. (2020) 132:379–94. doi: 10.1097/ALN.0000000000002960, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiang Y, Yang M, Wang S, Li X, Sun Y. Emerging role of deep learning-based artificial intelligence in tumor pathology. Cancer Commun (Lond). (2020) 40:154–66. doi: 10.1002/cac2.12012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keskinbora K, Güven F. Artificial intelligence and ophthalmology. Turk J Ophthalmol. (2020) 50:37–43. doi: 10.4274/tjo.galenos.2020.78989, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauren C, Bryan W, Krishna Adithya V, Swati U, Silvester C, Rengaraj V, et al. Automatic detection of glaucoma via fundus imaging and artificial intelligence: A review. Surv Ophthalmol. (2022) 68:17–41. doi: 10.1016/j.survophthal.2022.08.005 [DOI] [PubMed] [Google Scholar]
- 19.Tan NYQ, Friedman DS, Stalmans I, Ahmed IIK, Sng CCA. Glaucoma screening: where are we and where do we need to go? Curr Opin Ophthalmol. (2020) 31:91–100. doi: 10.1097/ICU.0000000000000649, PMID: [DOI] [PubMed] [Google Scholar]
- 20.Brandão-de-Resende C, Alcântara LAR, Vasconcelos-Santos DV, Diniz-Filho A. Glaucoma and telemedicine. J Glaucoma. (2023) 32:327–32. doi: 10.1097/IJG.0000000000002200 [DOI] [PubMed] [Google Scholar]
- 21.Girard MJA, Schmetterer L. Artificial intelligence and deep learning in glaucoma: current state and future prospects. Prog Brain Res. (2020) 257:37–64. doi: 10.1016/bs.pbr.2020.07.002 [DOI] [PubMed] [Google Scholar]
- 22.Camara J, Neto A, Pires IM, Villasana MV, Zdravevski E, Cunha A. Literature review on artificial intelligence methods for Glaucoma screening, segmentation, and classification. Journal of. Imaging. (2022) 8:19. doi: 10.3390/jimaging8020019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaurasia AK, Greatbatch CJ, Hewitt AW. Diagnostic accuracy of artificial intelligence in Glaucoma screening and clinical practice. J Glaucoma. (2022) 31:285–99. doi: 10.1097/IJG.0000000000002015, PMID: [DOI] [PubMed] [Google Scholar]
- 24.Zapata MA, Royo-Fibla D, Font O, Vela JI, Marcantonio I, Moya-Sanchez EU, et al. Artificial intelligence to identify retinal fundus images, quality validation, laterality evaluation, macular degeneration, and suspected Glaucoma. Clin Ophthalmol. (2020) 14:419–29. doi: 10.2147/OPTH.S235751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bellows DA, Chan NCY, Chen JJ, Cheng H-C, MacIntosh PW, Nij Bijvank JA, et al. Neuro-ophthalmic literature review. Neuro-Ophthalmology. (2020) 44:415–21. doi: 10.1080/01658107.2020.1828705 [DOI] [Google Scholar]
- 26.Ng WY, Zhang S, Wang Z, Ong CJT, Gunasekeran DV, Lim GYS, et al. Updates in deep learning research in ophthalmology. Clin Sci. (2021) 135:2357–76. doi: 10.1042/CS20210207, PMID: [DOI] [PubMed] [Google Scholar]
- 27.Timothy YYL. Ocular imaging at the cutting-edge. Eye. (2020) 35:1–3. doi: 10.1038/s41433-020-01268-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coen de V, Koenraad AV, Nicolas J, He W, Hongyi S, Firas K, et al. AIROGS: artificial intelligence for RObust Glaucoma screening challenge. arXiv. (2023) 2023:1738. doi: 10.48550/arXiv.2302.01738 [DOI] [Google Scholar]
- 29.Lemij HG, Vente C, Sánchez CI, Vermeer KA. Characteristics of a large, labeled data set for the training of artificial intelligence for Glaucoma screening with fundus photographs. Ophthalmology. Science. (2023) 3:100300. doi: 10.1016/j.xops.2023.100300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schuman JS, De Los Angeles Ramos Cadena M, McGee R, Al-Aswad LA, Medeiros FA. A case for the use of artificial intelligence in Glaucoma assessment. Ophthalmol Glaucoma. (2021) 5:e3–e13. doi: 10.1016/j.ogla.2021.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nunez R, Harris A, Ibrahim O, Keller J, Wikle CK, Robinson E, et al. Artificial intelligence to aid Glaucoma diagnosis and monitoring: state of the art and new directions. Photo-Dermatology. (2022) 9:810. doi: 10.3390/photonics9110810, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gong D, Hu M, Yin Y, Zhao T, Ding T, Meng F, et al. Practical application of artificial intelligence Technology in Glaucoma Diagnosis. J Ophthalmol. (2022) 2022:1–12. doi: 10.1155/2022/5212128, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chalkias I-N, Bakirtzis C, Pirounides D, Boziki MK, Grigoriadis N. Optical coherence tomography and optical coherence tomography with angiography in multiple sclerosis. Healthcare. (2022) 10:1386. doi: 10.3390/healthcare10081386, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Psomadakis CE, Marghoob N, Bleicher B, Markowitz O. Optical coherence tomography. Clin Dermatol. (2021) 39:624–34. doi: 10.1016/j.clindermatol.2021.03.008 [DOI] [PubMed] [Google Scholar]
- 35.Invernizzi A, Cozzi M, Staurenghi G. Optical coherence tomography and optical coherence tomography angiography in uveitis: a review. Clin Experiment Ophthalmol. (2019) 47:357–71. doi: 10.1111/ceo.13470 [DOI] [PubMed] [Google Scholar]
- 36.Omer D, Utku K, Deepak G, Ashish K, Fabio G, Giancarlo F. Explainable framework for Glaucoma diagnosis by image processing and convolutional neural network synergy: analysis with doctor evaluation. Futur Gener Comput Syst. (2021) 129:152–69. doi: 10.1016/j.future.2021.11.018 [DOI] [Google Scholar]
- 37.Panda SK, Cheong H, Tun TA, Devella SK, Senthil V, Krishnadas R, et al. Describing the structural phenotype of the glaucomatous optic nerve head using artificial intelligence. Am J Ophthalmol. (2021) 236:172–82. doi: 10.1016/j.ajo.2021.06.010 [DOI] [PubMed] [Google Scholar]
- 38.Fu H, Li F, Sun X, Cao X, Liao J, Orlando JI, et al. AGE challenge: angle closure Glaucoma evaluation in anterior segment optical coherence tomography. Med Image Anal. (2020) 66:101798. doi: 10.1016/j.media.2020.101798, PMID: [DOI] [PubMed] [Google Scholar]
- 39.Mardin CY. Are there static-structural biomarkers for Glaucoma with OCT? Klin Monatsbl Augenheilkd. (2022) 239:149–57. doi: 10.1055/a-1688-1601 [DOI] [PubMed] [Google Scholar]
- 40.Bragança CP, Torres JM, Macedo LO, Soares CPA. Advancements in Glaucoma diagnosis: the role of AI in medical imaging. Diagnostics. (2024) 14:530. doi: 10.3390/diagnostics14050530, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li F, Wang D, Yang Z, Zhang Y, Jiang J, Liu X, et al. The AI revolution in glaucoma: bridging challenges with opportunities. Prog Retin Eye Res. (2024) 103:101291. doi: 10.1016/j.preteyeres.2024.101291, PMID: [DOI] [PubMed] [Google Scholar]
- 42.Wang Y, Shan G, Li H, Wang L. A wearable-sensor system with AI Technology for Real-Time Biomechanical Feedback Training in hammer throw. Sensors. (2022) 23:425. doi: 10.3390/s23010425, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carlà MM, Gambini G, Baldascino A, Boselli F, Giannuzzi F, Margollicci F, et al. Large language models as assistance for glaucoma surgical cases: a ChatGPT vs. Google Gemini comparison. Graefe's archive for. Clin Exp Ophthalmol. (2024) 262:2945–59. doi: 10.1007/s00417-024-06470-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dihan Q, Chauhan MZ, Eleiwa TK, Hassan AK, Sallam AB, Khouri AS, et al. Using large language models to generate educational materials on childhood Glaucoma. Am J Ophthalmol. (2024) 265:28–38. doi: 10.1016/j.ajo.2024.04.004, PMID: [DOI] [PubMed] [Google Scholar]
- 45.Huang AS, Hirabayashi K, Barna L, Parikh D, Pasquale LR. Assessment of a large language Model’s responses to questions and cases about Glaucoma and retina management. JAMA. Ophthalmology. (2024) 142:371. doi: 10.1001/jamaophthalmol.2023.6917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abid A, Baxter SL. Breaking barriers in behavioral change: the potential of AI-driven motivational interviewing. J Glaucoma. (2024) 33:473–7. doi: 10.1097/IJG.0000000000002382, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Daniel B, Omri Z, Leah A, Zaki N, Ariela K, Joseph P, et al. Gemini AI vs. ChatGPT: a comprehensive examination alongside ophthalmology residents in medical knowledge. Graefes Arch Clin Exp Ophthalmol. (2024) 2024:625. doi: 10.1007/s00417-024-06625-4 [DOI] [PubMed] [Google Scholar]
- 48.Aretha Z, Isis Z, Priya T, Rashika V, Catherine Y, Eric K, et al. Deep learning artificial intelligence in vision-threatening disease in clinical and community screenings. Invest Ophthalmol Vis Sci. (2022) 2022:1381. Available at: https://iovs.arvojournals.org/article.aspx?articleid=2782173&resultClick=1 (Accessed December 4, 2024). [Google Scholar]
- 49.Christopher M, Nakahara K, Bowd C, Proudfoot JA, Belghith A, Goldbaum MH, et al. Effects of study population, labeling and training on Glaucoma detection using deep learning algorithms. Transl Vis Sci Technol. (2020) 9:27. doi: 10.1167/tvst.9.2.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghanchi F, Bourne R, Downes SM, Gale R, Rennie C, Tapply I, et al. An update on long-acting therapies in chronic sight-threatening eye diseases of the posterior segment: AMD, DMO, RVO, uveitis and glaucoma. Eye. (2022) 36:1154–67. doi: 10.1038/s41433-021-01766-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agboola HA, Zaccheus JE. Wavelet image scattering based glaucoma detection. BMC Biomed Eng. (2023) 5:1. doi: 10.1186/s42490-023-00067-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gupta K, Reddy S. Heart, eye, and artificial intelligence: a review. Cardiol Res. (2021) 12:132–9. doi: 10.14740/cr1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hood DC, La Bruna S, Tsamis E, Thakoor KA, Rai A, Leshno A, et al. Detecting glaucoma with only OCT: implications for the clinic, research, screening, and AI development. Prog Retin Eye Res. (2022) 90:101052. doi: 10.1016/j.preteyeres.2022.101052, PMID: [DOI] [PubMed] [Google Scholar]
- 54.Hood DC, Zemborain ZZ, Tsamis E, De Moraes CG. Improving the detection of Glaucoma and its progression: a topographical approach. J Glaucoma. (2020) 29:613–21. doi: 10.1097/IJG.0000000000001553, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jalamangala Shivananjaiah SK, Kumari S, Majid I, Wang SY. Predicting near-term glaucoma progression: an artificial intelligence approach using clinical free-text notes and data from electronic health records. Front Med. (2023) 10:16. doi: 10.3389/fmed.2023.1157016, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li Z, Keel S, Liu C, He M. Can artificial intelligence make screening faster, more accurate, and more accessible? Asia-Pacific. J Ophthalmol. (2018) 7:436–41. doi: 10.22608/APO.2018438 [DOI] [PubMed] [Google Scholar]
- 57.Srikanth T, Ranjith C, Ruoming J, Robert JC, Minzhong Y. Identifying the edges of the optic cup and the optic disc in Glaucoma patients by segmentation. Sensors. (2023) 23:4668. doi: 10.3390/s23104668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Elmoufidi A, Skouta A, Jai-Andaloussi S, Ouchetto O. CNN with multiple inputs for automatic Glaucoma assessment using fundus images. Int J Image Graph. (2022) 23:2350012. doi: 10.1142/S0219467823500122 [DOI] [Google Scholar]
- 59.Abdullah YI, Schuman JS, Shabsigh R, Caplan A, Al-Aswad LA. Ethics of artificial intelligence in medicine and ophthalmology. Asia-Pacific. J Ophthalmol. (2021) 10:289–98. doi: 10.1097/APO.0000000000000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anton N, Dragoi EN, Tarcoveanu F, Ciuntu RE, Lisa C, Curteanu S, et al. Assessing changes in diabetic retinopathy caused by diabetes mellitus and Glaucoma using support vector Machines in Combination with differential evolution algorithm. Appl Sci. (2021) 11:944. doi: 10.3390/app11093944 [DOI] [Google Scholar]
- 61.Chang J, Lee J, Ha A, Han YS, Bak E, Choi S, et al. Explaining the rationale of deep learning Glaucoma decisions with adversarial examples. Ophthalmology. (2020) 128:78–88. doi: 10.1016/j.ophtha.2020.06.036 [DOI] [PubMed] [Google Scholar]
- 62.Kamalipour A, Moghimi S. Macular optical coherence tomography imaging in Glaucoma. J Ophthalmic Vision Res. (2021) 16:478–89. doi: 10.18502/jovr.v16i3.9442, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee EB, Wang SY, Chang RT. Interpreting deep learning studies in Glaucoma: unresolved challenges. Asia-Pacific. J Ophthalmol. (2021) 10:261–7. doi: 10.1097/APO.0000000000000395 [DOI] [PubMed] [Google Scholar]
- 64.Mahmoudi S, Feroui A, Lazouni MEA. A new intelligent system for Glaucoma disease detection. Int J Comput Aided Eng Technol. (2019) 11:613. doi: 10.1504/IJCAET.2019.100457 [DOI] [Google Scholar]
- 65.Medeiros FA, Lee T, Jammal AA, Al-Aswad LA, Eydelman MB, Schuman JS, et al. The definition of glaucomatous optic neuropathy in artificial intelligence research and clinical applications. Ophthalmol Glaucoma. (2023) 6:432–8. doi: 10.1016/j.ogla.2023.01.007, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oh S, Park Y, Cho KJ, Kim SJ. Explainable machine learning model for Glaucoma diagnosis and its interpretation. Diagnostics. (2021) 11:510. doi: 10.3390/diagnostics11030510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zain K, Ronald Z, Eitan S, Lei Z, Vivek T, Hiroshi I, et al. Relationships between the optic nerve head in optical coherence tomography and optic nerve volume in magnetic resonance imaging in Glaucoma. Invest Ophthalmol Vis Sci. (2022) 2022:11. Available at: https://iovs.arvojournals.org/article.aspx?articleid=2783316&resultClick=1(Accessed December 4, 2024). [Google Scholar]
- 68.Ruamviboonsuk P, Cheung CY, Zhang X, Raman R, Park SJ, Ting DSW. Artificial intelligence in ophthalmology: evolutions in Asia. Asia-Pacific. J Ophthalmol. (2020) 9:78–84. doi: 10.1097/01.APO.0000656980.41190.bf [DOI] [PubMed] [Google Scholar]
- 69.Young SL, Jain N, Tatham AJ. The application of advanced imaging techniques in glaucoma. Expert. Rev Ophthalmol. (2022) 17:183–97. doi: 10.1080/17469899.2022.2101449 [DOI] [Google Scholar]
- 70.Siesky B, Harris A, Vercellin ACV, Guidoboni G, Tsai JC. Ocular blood flow as it relates to race and disease on glaucoma. Adv Ophthalmol Optom. (2021) 6:245–62. doi: 10.1016/j.yaoo.2021.04.016, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]