Abstract
Background
The burden of ST-segment elevation myocardial infarction (STEMI) worldwide is increasing as the leading cause of death; there are scant data on system-based initiatives and performance metrics relative to its management in low- and middle-income countries where resources are frequently limited.
Objectives
The Global Heart Attack Treatment Initiative (GHATI) ultimate aim is improving evidence-based STEMI care, adherence to guidelines, and tracking of clinical and institutional indicators in low- and middle-income countries. To achieve that goal, the process of care and outcomes of STEMI patients in those nations will be studied.
Methods
In this initial phase of GHATI (2019-2021), prospective analyses of selected STEMI metrics derived from the American College of Cardiology Chest Pain MI Registry were undertaken in 18 international hospitals, most located in developing countries unfamiliar with quality improvement metrics.
Results
Of 4,092 patients enrolled, complete data were available in 3,914 consecutive STEMIs included here: 80.5% male; 35.5% smokers; shock on arrival in 10%; and 5.1% with cardiac arrest before intervention. Overall, a 2% improvement on combined endpoints (shock; arrest before or after intervention; final ejection fraction <40%; survival at discharge) was observed over time, and survivorship also increased by 2% (P = 0.003). First medical contact to device time <90 minutes occurred in 74.8%; reperfusion therapy in 94.2%; and adherence to guidelines in 91.8%.
Conclusions
This global contemporary registry successfully enrolled STEMI patients in nations generally unfamiliar with quality improvement metrics; trends of improvement in their care were observed. GHATI may facilitate implementation of policies aimed at enhancing outcomes of cardiovascular disease worldwide, particularly in countries with evolving economies.
Key words: AMI registry, international, STEMI
Central Illustration
Over 20 million deaths attributed to cardiovascular disease occur every year worldwide, one-half due to coronary heart disease (CHD); of those, over 80% are estimated to take place in developing nations where most of the world population resides. ST-segment elevation myocardial infarction (STEMI) remains an important cause of morbidity and mortality as it is the predominant acute manifestation of CHD with a global prevalence of over 3 million cases a year.1, 2, 3 Recent reports show increasing rates of STEMI in countries like China and India, accounting for 60% to 80% of acute myocardial infarction hospitalizations.4, 5, 6, 7, 8
This humanitarian and financial burden resulting from CHD, formerly considered a “first world” disease, is increasing due to a multiplicity of factors including the transformation of previously agricultural societies into urban industrialized cities with their ensuing unhealthy dietary habits, pollution, stress, and sedentary lifestyles. Other contributing issues such as relatively fast economic growth widening the gap between the rich and the poor; lack of CV risk factors and lifestyle modification initiatives; important educational challenges; and social and cultural disparities may also be present.7
Meanwhile, significant improvements in STEMI care and outcomes have been achieved in countries with strong economies as the result of timely reperfusion, evidence-based pharmacological interventions, and implementation of quality improvement (QI) and system-based protocols. Initiatives such as the Mission: Lifeline and STEMI Accelerator Programs are largely responsible for many of these advancements in the United States, clinical registries such as the National Cardiovascular Disease Registry program and similar ones in Western Europe are key resources that provide ongoing measurement, track important processes, and identify opportunities for improvement.9, 10, 11, 12, 13, 14, 15
Unfortunately, many countries lack such registries or systematic resources for data gathering on STEMI, a fact also present in most low- and middle-income countries (LMICs) where some have even indicated they are virtually nonexistent.4,16,17 Surveys conducted by the American College of Cardiology (ACC) have supported those considerations showing unacceptably low rates of reperfusion, widespread lack of local or national STEMI registries, and logistical limitations to adherence to ACC/AHA/ESC guidelines internationally.18
Recognizing the significant global burden of STEMI and the paucity of data on system-based initiatives and performance metrics outside the United States and Western Europe, the ACC launched the Global Heart Attack Treatment Initiative (GHATI) primarily with the goal of collecting useful information in the understanding of how LMICs care for STEMI patients and their outcomes. With the ultimate aim of promoting the implementation of QI efforts, this initiative will enhance evidence-based CV care in LMICs and improve cardiovascular disease mortality worldwide.19
Methods
Program implementation
Chest Pain Myocardial Infarction (CPMI) is an ACC National Cardiovascular Disease Registry that gathers data from 772 institutions in the United States on subjects with suspected acute coronary syndrome (ACS) extending from low-risk chest pain to acute myocardial infarction, focusing on patient characteristics, guideline-based therapies and processes, and in-hospital outcomes. GHATI is an ACC initiative launched in 2019 involving countries and sites outside the United States that applies a subset of CPMI registry data specifically focused on STEMI patients.
Table 1 describes the select data elements and performance metrics tracked in this international effort including adherence to guideline-directed medical therapies (GDMTs) administered: aspirin upon arrival, P2Y12 inhibitor between first medical contact and catheterization, aspirin, beta-blocker, and statin at discharge, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers for final left ventricular ejection fraction (EF) <40%, and P2Y12 inhibitor at discharge. In addition to these measures, in-hospital mortality, and a composite endpoint of shock on arrival, cardiac arrest before/after intervention, final EF <40% and survival at discharge were obtained and followed quarterly. While GHATI did not implement specific interventions prior to launching and recruitment, investigators felt that assessing both system-related characteristics before clinical presentation as well as hospital processes were important undertakings if an accurate depiction of the status of STEMI care in LMICs was to be obtained.
Table 1.
CPMI-Derived Performance Metrics and Data Points Used in GHATI
| Elements | Description |
|---|---|
| E1 | Reason for delay at facility |
| E2 | Transportation time |
| E3 | Mean and median time: first medical contact to ECG |
| E4 | Mean and median time: arrival to ECG |
| E5 | Mean and median time: arrival to cath lab |
| E6 | Mean and median time: arrival to fibrinolytic therapy |
| E7 | Mean and median time: arrival to device time |
| E8 | Proportion of patients with LVEF <40% |
| E9 | Proportion of patients discharged alive |
| E11 | Proportion of patients receiving P2Y12 inhibitor between first medical contact and catheterization |
| E12 | Proportion of patients received at facility in cardiogenic shock |
| E13 | Patients who experienced cardiac arrest before intervention |
| E14 | Patients who experienced cardiac arrest after intervention |
| E15 | Patients who are current smokers |
| E16 | Patients who are female |
| Performance metrics | Description |
| PM1 | Aspirin upon arrival |
| PM2 | Aspirin prescribed at discharge |
| PM3 | Beta-blocker at discharge |
| PM4 | Statin at discharge |
| PM5 | Evaluation of LVEF |
| PM6 | ACE-I or ARB for LVSD (LVEF <40%) at discharge |
| PM7 | Door-to-needle time (fibrinolytic therapy) |
| PM8 | STEMI patients receiving primary PCI within 90 min |
| PM9 | Reperfusion therapy |
| PM13 | P2Y12 inhibitor at discharge |
ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin II receptor blocker; GHATI = Global Heart Attack Treatment Initiative; LVEF = left ventricular ejection fraction; LVSD = left ventricular systolic dysfunction; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Participation in GHATI was voluntary, free of charge, and required the following: identification and commitment of site champions, reporting of results collected in a timely manner, agreement to share aggregated data, adherence to privacy and ethical standards described in the participation agreement, and in accordance with the local individual Institutional Review Board requirements. Recognizing the financial restrictions present at many sites where no budget allocation for the establishment of QI efforts existed, investigators secured a modest stipend from the ACC with the specific intention of facilitating GHATI’s participation. Lastly, institutions were allowed to engage independently in QI initiatives based on the analysis of their own data.
Data collection
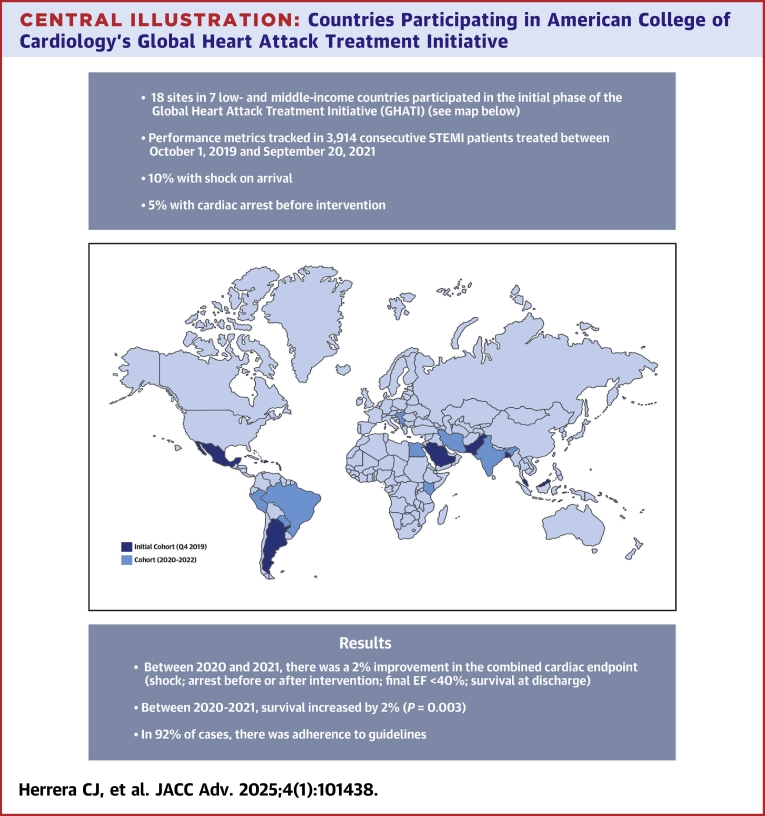
As shown in the Central Illustration, GHATI began enrolling sites from 7 countries but within 24 months, the registry had grown to 39 sites in 20 countries across 5 continents. Table 2 depicts the characteristics of those hospitals: most were tertiary care centers located in largely populated urban areas, equipped with catheterization laboratories, had fewer than 300 beds, were not part of a STEMI network, and had no prior experience in registries or QI programs.
Central Illustration.
Countries Participating in American College of Cardiology’s Global Heart Attack Treatment Initiative
EF = ejection fraction; STEMI = ST-segment elevation myocardial infarction.
Table 2.
Characteristics of 18 Hospitals Enrolled in GHATI’s Initial Phase
| Population living in city served | Average 10 million (range 1-24) |
| Number of hospitals in said city | Average 42 (range 14-100) |
| Type of hospital | Tertiary 85%; community 15% |
| Number of beds | <300 (76%) |
| Part of STEMI network | 57% |
| Cath lab available | 98% |
| STEMI local protocol implemented during GHATI | 41.6% |
Abbreviations as in Table 1.
During the initial pilot phase, centers were required to report 20 consecutive patients per quarter. Subsequently, they were expected to submit all consecutive STEMIs. Deidentified patient and hospital information were aggregated by each site and reported quarterly to GHATI. Those data were then compared over time and sent back to participating facilities with site anonymity. Information was summarized by quarter and averaged over the “rolling four-quarters” for each available data point. An internal audit protocol was also applied to centers quarterly, so accuracy and completeness of information was assured. Shortly after GHATI was launched, the SARS-CoV-2 pandemic spread throughout most of the nations involved. Understanding the potential impact this crisis could create in the care of STEMI patients, additional metrics were implemented and tracked including COVID-19 diagnostic algorithms prior to reperfusion therapy; delays in interventions (pharmacologic or percutaneous); coronary findings during cardiac catheterization; and final diagnosis reached. Since these indicators are currently being collected, they will not be reported here.
Statistical analysis
All STEMI metrics were calculated using a rolling 4-quarter mean difference for both GHATI and CPMI; the values were reported in aggregate by hospitals, averaged over 4 sequential quarters. Where a difference was calculated, the window of the date range is then moved forward by one-quarter and the values compared. This is done to smooth seasonal values while allowing for detail at the quarter level (vs comparing year to year).
Survivorship was calculated by site averaged over 4 quarters compared to the following 4 quarters; for example, the average proportion of patients discharged alive for site A between Q4 2019 and Q3 2020 is compared to the average proportion of patients discharged alive for site A between Q1 2020 and Q4 2020.
Since the composite outcomes included metrics with different directions of improvement, the averages were calculated as a sum of the proportion of patients discharged alive and the complementary percentage (the 1-metric value) for proportion of patients received in shock, who arrested before or after the intervention, and with residual EF <40%.
Adherence to GDMTs by hospital and all other metrics were compared between time points and groups using the Mann-Whitney (Wilcoxon rank sum) test since the data were not normally distributed as determined by Shapiro-Wilk analysis. All analyses were developed in R (version 4.4.0).20
Results
Between October 1, 2019 (Q4 2019), and September 30, 2021 (Q3 2021), information on 4,092 patients with STEMI treated at 22 sites was sent to GHATI investigators; data corresponding to the rolling four-quarters between Q4 2019 and Q3 2021 obtained at 18 sites included 3,914 patients (reflecting all sites with 4+ consecutive quarters reported) are analyzed here. The participating countries in GHATI’s initial phase were Argentina, Bangladesh, Dominican Republic, Malaysia, Mexico, Pakistan, and Saudi Arabia. Subsequently, sites from Brazil, Costa Rica, Cuba, Egypt, India, Iran, Kenya, North Macedonia, Paraguay, Peru, Serbia, Singapore, and United Arab Emirates were added after initial data collection began.
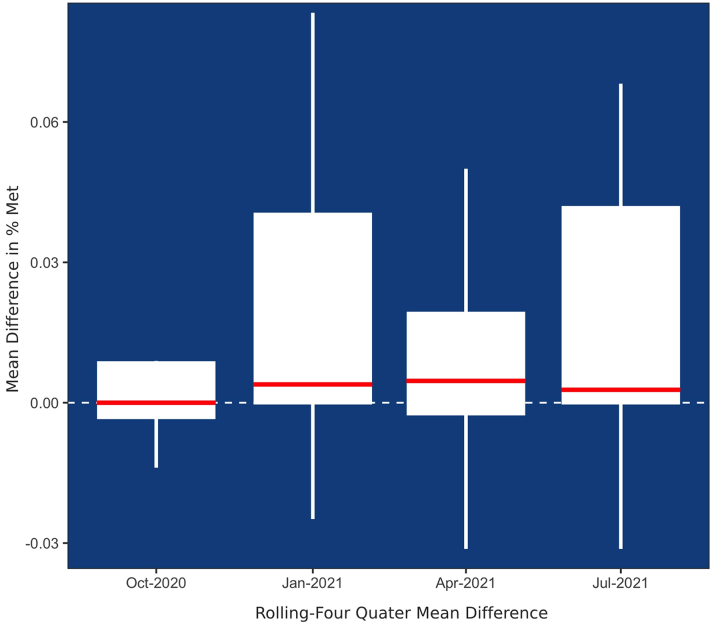
Patient characteristics included 80.5% male, 35.5% current smokers, 10% had cardiogenic shock, and 5.1% cardiac arrest prior to intervention. Figure 1 depicts sustained improvement on the proportion of patients discharged alive over time points with a mean difference averaged across sites of 1.7% ± 3.5%. Table 3 illustrates STEMI metrics from 2020 to 2021 for each CPMI and GHATI including the average percentage receiving any reperfusion, lytic therapy within 30 minutes, and proportion of patients discharged alive.
Figure 1.
Change in Proportion of Patients Discharged Alive Over Time
Table 3.
2-Year Comparison of CPMI vs GHATI STEMI Metrics (2020-2021)
| Metric | 2020-2021 |
|
|---|---|---|
| CPMI | GHATI | |
| Proportion of patients who arrested prior to intervention | 3.6% | 5.1% |
| Proportion of patients with LVEF <40% | 13% | 34.5% |
| Proportion of patients received in cardiogenic shock | 7.8% | 10% |
| Proportion of patients discharged alive | 96% | 93% |
| Proportion of patients with EF documentation | 97% | 96% |
| % of patients receiving lytic Rx <30’ of arrival (door to needle time) | 57% | 28% |
| % of patients with FMC to device time <90’ | 85% | 74.8% |
| % of patients that received (any) reperfusion therapy | 98% | 94.2% |
Data are presented as average.
CPMI = Chest Pain Myocardial Infarction NCDR Registry; FMC = first medical contact; other abbreviations as in Table 1.
Discussion
GHATI is the most contemporary global STEMI registry to date; although difficult at the outset, we observed that implementing QI initiatives is a feasible endeavor in countries generally unfamiliar with the concept. During the study period of this initial 2-year effort, sustained trends of improvement in both clinical and system-based metrics were noted; these included reductions in the combined endpoint of cardiogenic shock on arrival, arrest preintervention and postintervention, final EF < 40%, and survival at discharge. Whether these were the result of random occurrence or of a more focused, rigorous streamlined approach to the care of STEMI patients driven by the process itself or the local coordinators cannot be determined from these data.
Sustained robust adherence to GDMTs and trends toward shorter transportation times were also seen, suggesting that current guidelines have indeed positively impacted patient care even under resource-limited circumstances. The fact that several established metrics of STEMI care measured in GHATI behaved similarly to those of U.S. institutions participating in CPMI supports this concept. We hypothesize that tracking and the frequent internal comparison of individual hospital data may have contributed to improvement in site performance. Although it was not a specific goal or a requirement of GHATI, subsequent selected surveyed sites acknowledged the implementation of STEMI protocols based on their own data analysis.
With over 3 million STEMIs occurring globally each year and more than 20 million cardiovascular fatalities, acute myocardial infarction is a leading cause of death in many nations, including LMICs. The epidemiological transition observed during the past few decades in many of these countries suggests that the prevalence of fatal CHD will continue to rise in years to come, and with it, the significant financial burden created by its impact on societal productivity, including saturation of hospitals and health care systems that will only worsen.21 This is underscored by the disparities in care provided to STEMI patients in various regions of the world given structural system differences with use of medical transportation, paramedic skills, availability of urgent and accurate electrocardiogram interpretation, etc. Consequently, the development of strategies aimed at enhancing public education on signs and symptoms of STEMI and the importance of early response, establishing rapid access and presentation to medical facilities; implementation of effective systems of care, and overall cultural and socioeconomical support for the treatment of patients with STEMI in these regions is urgently needed.
It was not until the end of the 1990s and early 2000s when a handful of STEMI registries began to include and/or focused on LMICs; however, they enrolled all forms of ACS clinical presentations and by design, were primarily intended to gather clinical characteristics and treatment modalities. Between 1999 and 2009, hospitals from North and South America, Europe, Asia, China, Australia, and New Zealand were recruited in GRACE (Global Registry of Acute Coronary Events) with the goal of creating a predictive risk score.22 In the ACCESS (ACute Coronary Events - a multinational Survey of current management Strategies) registry, a more representative sample of LMICs, 11,731 patients with ACS, less than half of STEMIs, were enrolled in this prospective observational study conducted in 19 nations of Africa, Latin America, and the Middle East.23
In China, one of the world’s most populated countries, there were no national representative STEMI registries until the China PEACE-Retrospective Acute Myocardial Infarction Study was published; and similarly to the previously cited studies, while appropriate therapies were used in most patients, significant gaps were evident, including reduced rates of reperfusion and relatively high early mortality.24
More recently, 2 important registries have addressed the status of STEMI in India, a nation where this entity represents a major public health challenge as it has the highest burden of ACS in the world. In the CREATE (Treatment and outcomes of acute coronary syndromes in India), registry, longer delays before medical evaluation and reperfusion therapy, lower use of PCI, strong use of GDMTs, and a significant socioeconomical gradient on mortality so that poorer patients carried the highest death rates independent of risk factors were noted.25 The Kerala ACS registry, India’s largest to date, aimed at gathering prospective data to address treatment and system gaps in management; patients typically presented late, longer than 30 minutes door-to-needle times were observed in nearly a third of the sample, overall rates of reperfusion therapy, either pharmacological or mechanical, were low, discharge medications use was relatively high, and unadjusted mortality was high as well.26
Central and Eastern European patients with ACS have been reported to have worse outcomes than those treated in the United States and Western European centers; the International Survey of Acute Coronary Syndrome in Transitional Countries enrolled patients with STEMI and compared results based on high or low national public health expenditure. The authors highlighted the fact that many STEMI patients in lower-income European nations do not receive reperfusion therapies, are managed conservatively without cardiac catheterization, and suffer unacceptably long delays in presentation and treatment.27
In Latin America, very little contemporary data exist on STEMI outcomes and systems of care, the small Brazilian Registry of STEMI care of Salvador (RESISST) perhaps being the exception. This initiative intended to identify predictors of 30-day mortality and importantly, assess how the use of evidence-based therapies impacted clinical outcomes after the implementation of a regional care integrated STEMI network. Among patients enrolled between 2011 and 2013, significant improvements in the use of antiplatelet therapy and statins, rates of primary reperfusion, and 30-day mortality were noted highlighting the potential beneficial impact of systems of care in regions with limited resources.28,29
As Table 3 demonstrates, it is noteworthy that during the initial 2 years of GHATI’s enrollment, although rates of reperfusion were robust compared with CPMI data, they remained lower. Similarly, the proportion of STEMI patients receiving pharmacologic reperfusion within the therapeutic window and the proportion of those receiving PCI within guideline-mandated time also remained lower in GHATI nations compared with centers in the United States. Ongoing analysis of COVID metrics gathered after GHATI’s start may shed light into this observation, however, it is plausible that these gaps may have been present during the current era of STEMI care and were the result of other factors related to both system-based and institutional-driven limitations.
The observed difference between male and female patients diagnosed and treated for STEMI in the first 2 years of GHATI was a previously noted trend in some European and Australian studies albeit not consistently.30, 31, 32 Sex differences in STEMI occurrence are particularly concerning given the younger age of populations residing in LMICs, nations with already constrained health care expenditures. This subject, however, needs further study in larger populations and across different geographical regions for a better understanding so that specific sex-related corrective interventions can be implemented.
Difficulties encountered in GHATI’s implementation and consolidation included: financial limitations for technology support (computers, software, etc); workforce restrictions; unavailability of appropriately trained personnel capable of running QI programs and acquiring and monitoring data accuracy; and general absence of a QI-driven culture. In addition, other system-related complex challenges were noted as well: lack of advanced cardiac life support-trained Emergency Medical Services personnel; lack of equipped ambulances sometimes without electrocardiogram capabilities; and nearly nonexistent STEMI networks in several countries further hampering timely transportation. While the analysis of these important aspects of STEMI care were not directly related to GHATI’s specific goals, we recognize their critical impact on hospital-related metrics, and since have expanded data collection so transportation-related parameters are tracked. Furthermore, we believe that once these obstacles are overcome, the cost-effectiveness of implementing initiatives like GHATI in LMICs will undoubtedly be demonstrated as long-term savings resulting from improved quality.
It must be acknowledged that GHATI hospitals represented a small proportion of the broad range of institutions serving largely populated cities in LMICs (from tertiary to community). However, this, and the fact that most sites were not previously part of an acute myocardial infarction network illustrate the major challenges encountered in the timely care of STEMI patients in those nations. In this context, several hospitals that were part of the initial cohort had the forethought of structuring QI initiatives of their own.
As with any registry, GHATI’s limitations also include possible selection bias as centers volunteered to participate, as well as variability in consecutive data collection via self-reporting and a relatively small number of participating centers and subjects to assess quality of care. In addition, while it does not reduce or interfere with collection and accuracy, programmed deidentification of patient’s information on sites and countries involved in GHATI driven by required international regulation of data sharing may have hindered detailed analysis of specific clinical and system-based variables locally or regionally.
Lastly, ample evidence exists supporting the notion that the SARS-CoV-2 pandemic negatively impacted STEMI care globally: travel restrictions, patient hesitation, and hospital staff/providers limitations are likely explanations of the significant delays in patient care that ultimately led to increased morbidity and mortality.33 The data gathered in this initial phase of GHATI could well reflect that STEMI care in LMICs may have had a worse impact during the SARS-CoV-2 pandemic as many nations with established disparities did not implement early measures to circumvent these unforeseen circumstances. Subsequent analysis of GHATI’s database and ongoing COVID-related metrics will likely bring clarity into this issue.
Conclusions
The results shown here have significant clinical and public health implications for the future, making it imperative that we study in more detail the dynamics of STEMI presentation and management in LMICs if we are to impact mortality and outcomes of CHD, the leading cause of CV death worldwide. Our results suggest that implementation of QI initiatives in countries with no or minimal prior experience in STEMI systems of care is feasible although larger international registries and longer follow-up times will be required to corroborate our findings.
The information obtained from this observational, nonintervention registry should guide future local and regional initiatives directed at enhancing STEMI care in LMICs by improving system and patient-related obstacles pertinent to their circumstances such as public education on the early recognition of CV symptoms; advanced cardiac life support training of providers; multidisciplinary training of physicians in urgent care centers toward timely diagnosis and therapy of STEMI; strengthening pharmaco-invasive strategies is distant rural areas; and supporting the creation of STEMI networks.
Achieving these goals will require buy-in from governmental bodies, health care personnel, community organizations, and the adoption of a culture change in favor of an “opportunity for improvement” approach when dealing with suboptimal outcomes. Many, including the leadership of the ACC, have recently called for such actions with the specific purpose of improving cardiac health for underserved men and women alike across all regions of the globe.16,34,35 We certainly hope that moving forward, this and future GHATI contributions are of use in achieving successful implementation of local and national initiatives in the fight against CHD.
Perspectives.
COMPETENCY IN PATIENT CARE: Data on the status of contemporary evidence-based STEMI care in LMICs are limited, and little information exists in the implementation and sustainability of Acute Myocardial Infarction QI programs in these nations. In this prospective registry involving several countries across multiple continents, we learned that implementing such efforts is a feasible endeavor.
TRANSLATIONAL OUTLOOK: The implications derived from this ACC initiative suggest that factors related to STEMI care can be successfully tracked and improved globally.
Funding support and author disclosures
Mrs Olsson was an employee at the American College of Cardiology at the time of GHATI development and data collection. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The following investigators and participating institutions were fundamental for the completion of this project: Clinica Bazterrica, Argentina (Carlos Barrero, Lucas Roj, Enrique Fairman); Hospital Aleman, Argentina (Claudio Higa, Omar Tupayachi Villagomez); Sanatorio Britanico, Argentina (Luis Esteban Keller, Gabriel Tissera); National Institute of Cardiovascular Diseases, Bangladesh (Afzalur Rahman, AKM Monwarul); CEDIMAT Centro Cardiovascular, Dominican Republic (Cesar J Herrera, Carlos García Lithgow, Diogenes Cuevas, Ricardo Blanchery); Sarawak Heart Centre, Malaysia (Tiong Kiam Ong, Alan Fong, Khor How Keat); Instituto Nacional de Cardiologia Ignacio Chavez, Mexico (Alexandra Arias-Mendoza, Magdiel Conzalez); Tabba Heart Institute, Pakistan (Bashir Hanif, Rehan Malik); King Abdulaziz Cardiac Center, KA Medical City, Saudi Arabia (Mohammed Balghith, Bandar Al Haddad). The authors thank Yara Guk-Levi, Clinical Data Scientist and NCDR Analytics Associate for her invaluable contributions to this paper. The authors are also indebted to Dr Pamela Piña for her assistance in the preparation of the images.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Global Burden of Disease Study 2013 Mortality and Causes of Death. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yusuf S., Rangarajan K., Teo K., et al. Cardiovascular risk and events in 17 low-middle-and high-income countries. N Engl J Med. 2014;371:818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin E.J., Muntner P., Alonso A., et al. Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation. 2019;139(10):e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 4.Chandrashekhar Y., Narula J. Resource, and infrastructure-appropriate management of ST-segment elevation myocardial infarction in low-and middle-income countries. Circulation. 2020;141:2004–2025. doi: 10.1161/CIRCULATIONAHA.119.041297. [DOI] [PubMed] [Google Scholar]
- 5.Roselló X., Huo Y., Pocock S., et al. Global geographical variations in ST-segment elevation myocardial infarction management and post-discharge mortality. Int J of Cardiol. 2017;245:27–34. doi: 10.1016/j.ijcard.2017.07.039. [DOI] [PubMed] [Google Scholar]
- 6.Yusuf S., Reddy S., Ounpuu S., et al. Global burden of cardiovascular diseases part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 7.Murugiah K., Nuti S.V., Krumholz H.M. STEMI care in LMIC. Obstacles and opportunities. Global Heart. 2014;9(4):429–430. doi: 10.1016/j.gheart.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ranasinghe I., Rong Y., Du X., et al. System barriers to the evidence-based care of acute coronary syndrome in China. Circ Cardiovasc Qual Outcomes. 2014;7:209–216. doi: 10.1161/CIRCOUTCOMES.113.000527. [DOI] [PubMed] [Google Scholar]
- 9.O’Gara P.T., Kushner F.G., Ascheim D.D., et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of cardiology foundation/American heart association task force on practice guidelines. J Am Coll Cardiol. 2013;61:e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 10.Jollis J., Al-Khalidi H.R., Roettig M.L., et al. Impact of regionalization of ST-segment-elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: Mission: Lifeline Accelerator-2. Circulation. 2018;137:376–387. doi: 10.1161/CIRCULATIONAHA.117.032446. [DOI] [PubMed] [Google Scholar]
- 11.Henry T.D. From concept to reality: a decade of progress in regional ST-elevation myocardial infarction systems. Circulation. 2012;126:166–168. doi: 10.1161/CIRCULATIONAHA.112.114140. [DOI] [PubMed] [Google Scholar]
- 12.Cambou J.P., Simon T., Mulak G., et al. The French registry of Acute ST-elevation or non-ST-elevation Myocardial Infarction (FAST-MI): study design and baseline characteristics. Arch Mal Coeur Vaiss. 2007;100:524–534. [PubMed] [Google Scholar]
- 13.Huber K., Gersh B.J., Goldstein P., et al. The organization, function, and outcomes of ST-elevation myocardial infarction networks worldwide: current state, unmet needs and future directions. Eur Heart J. 2014;35:1526–1532. doi: 10.1093/eurheartj/ehu125. [DOI] [PubMed] [Google Scholar]
- 14.Dharma S. Comparison of real-life systems of care for ST-segment elevation myocardial infarction. Global Heart. 2020;15(1):66. doi: 10.5334/gh.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhatt D.L., Drozda J.P., Shahian D.M., et al. ACC/AHA/STS statement on the future of registries and the performance measurement Enterprise: a report of the American College of Cardiology/American Heart Association task force on performance measures and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2015;66:2230–2245. doi: 10.1016/j.jacc.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Hall M., Cenko E., Bueno H., et al. Contemporary roles of registries in clinical cardiology: insights from Western and Eastern European countries. Int J Cardiol. 2016;217:S13–S15. doi: 10.1016/j.ijcard.2016.06.220. [DOI] [PubMed] [Google Scholar]
- 17.Smith F.G., Brogan R.A., Alabas O., et al. Comparative care and outcomes for acute coronary syndromes in Central and Eastern European transitional countries: a review of the literature. Eur Heart J Acute Cardiovasc Care. 2015;4:537–554. doi: 10.1177/2048872614551545. [DOI] [PubMed] [Google Scholar]
- 18.Wilson H., Jollis J., Alexanderson E. Scaling STEMI care internationally. ACC’s global STEMI quality improvement initiative. J Am Coll Cardiol. 2018;72:2528–2530. doi: 10.1016/j.jacc.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 19.Levenson B., Herrera C., Wilson H. New ACC global heart Attack treatment initiative: improving STEMI care worldwide. J Am Coll Cardiol. 2020;75:1605–1608. doi: 10.1016/j.jacc.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 20.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: Accessed October 17, 2024. _R: A Language and Environment for Statistical Computing_.https://www.R-project.org/ [Google Scholar]
- 21.Alexander T., Mullasari A.S., Narula J. Developing a STEMI system of care for low-and middle-income countries. The STEMI India model. Global Heart. 2014;9(4):419–423. doi: 10.1016/j.gheart.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Fox K.A., Eagle K.A., Gore J.M., et al. The global registry of acute coronary events, 1999 to 2009-CRACE. Heart. 2010;96:1095–1101. doi: 10.1136/hrt.2009.190827. [DOI] [PubMed] [Google Scholar]
- 23.The ACCESS Investigators Management of acute coronary syndromes in developing countries: acute Coronary Events-a multinational Survey of current management Strategies. Am Heart J. 2011;162:852–859.e22. doi: 10.1016/j.ahj.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 24.Li J., Wang Q., Hu S., et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2015;385:441–451. doi: 10.1016/S0140-6736(14)60921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xavier D., Pais P., Deveraux P.J., et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 26.Mohanan P.P., Mathew R., Harikrishnan S., et al. Presentation, management, and outcomes of 25, 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bugiardini R., Badimon L., ISACS-TC Investigators and CoordinatorsISACS-TC Investigators and Coordinators The international Survey of acute coronary syndromes in transitional countries (ISACS-TC): 2010-2015. Int J Cardiol. 2016;(217):S1–S6. doi: 10.1016/j.ijcard.2016.06.219. [DOI] [PubMed] [Google Scholar]
- 28.Filgueiras Filho N.M., Feitosa Filho G.S., Solla D.J.F., et al. Implementation of a regional network for ST-segment-elevation myocardial infarction (STEMI) care and 30-day mortality in a low-to middle-income city in Brazil: findings from salvador’s STEMI registry (RESISST) J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.008624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Solla D.J.F., Paiva Filho Ide M., Delisle J.E., et al. Integrated regional networks for ST-segment-elevation myocardial infarction care in developing countries: the experience of Salvador, Bahia, Brazil. Circ Cardiovasc Qual Outcomes. 2013;6:9–17. doi: 10.1161/CIRCOUTCOMES.112.967505. [DOI] [PubMed] [Google Scholar]
- 30.Degano I.R., Salomaa V., Veronesi G., et al. Twenty five-year trends in myocardial infarction mortality rates and case fatality in six European populations. Heart. 2015;101:1413–1421. doi: 10.1136/heartjnl-2014-307310. [DOI] [PubMed] [Google Scholar]
- 31.Randall S.M., Zilkens R., Duke J.M., et al. Western Australia population trends in the incidence of acute myocardial infarction between 1993 and 2012. Int J Cardiol. 2016;222:678–682. doi: 10.1016/j.ijcard.2016.08.066. [DOI] [PubMed] [Google Scholar]
- 32.Gabet A., Danchin N., Juilliere Y., et al. Acute coronary syndrome in women: rising hospitalizations in middle-aged French women, 2004-2014. Eur Heart J. 2017;38(14):1060–1065. doi: 10.1093/eurheartj/ehx097. [DOI] [PubMed] [Google Scholar]
- 33.Kite T.A., Ludman P.F., Gale C.P., et al. International prospective registry of acute coronary syndromes in patients with COVID-19. J Am Coll Cardiol. 2021;77(20):2466–2476. doi: 10.1016/j.jacc.2021.03.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seligman B., Vedanthan R., Fuster V. Acute coronary syndromes in low-and-middle-income countries: moving forward. Int J Cardiol. 2016;(217):S10–S12. doi: 10.1016/j.ijcard.2016.06.213. [DOI] [PubMed] [Google Scholar]
- 35.Poppas A., Masoudi F.A. NCDR: advancing patient care, outcomes, and value through innovation and knowledge. J Am Coll Cardiol. 2021;77:224–226. doi: 10.1016/j.jacc.2020.12.001. [DOI] [PubMed] [Google Scholar]