Abstract
Abstract
Objectives
To investigate the social support status and associated factors among Vietnamese methadone maintenance patients during the COVID-19 pandemic.
Design
Cross-sectional study.
Setting
Three methadone clinics.
Participants
540 patients.
Primary and secondary outcome measures
The Medical Outcomes Study—Social Support Survey questionnaire was employed to measure patients’ social support. Factors associated with the social support status of patients were determined through multivariate linear regression models. Variables in these models were selected using the Bayesian model averaging method.
Results
The average social support score of patients was 63.50±26.54 (ranger: 0–100). The average social support scores of patients living in mountainous areas (Dien Bien: 63.74±23.67, Son La: 46.15±20.31) were significantly lower than that of patients residing in metropolitan areas (Hanoi: 80.61±23.47) (p<0.001). The likelihood of gaining high social support was 1.31 times more likely among patients living with at least one person (64.21±26.25) in comparison with those living alone (48.84±28.69) (p=0.013). The higher the number of family members living with the patient and close friends/relatives, the higher the social support score. Factors significantly associated with patients’ social support included the place of residence, the patient’s occupation, the family’s monthly income, the number of people living with the patients, and the number of close friends/relatives (p<0.001).
Conclusion
Methadone maintenance patients in Vietnam received a moderate level of social support during the COVID-19 pandemic. In the context of pandemics, not only the authorities but also family members and the community should give succour and strength to the patients, thereby contributing to the success of methadone treatment and the recovery of patients.
Keywords: Behavior, Health Services, MENTAL HEALTH, Patients, PUBLIC HEALTH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This multicentre study included a large number of methadone maintenance patients.
We selected variables in the multivariate linear regression model via the Bayesian model averaging method.
Causal relationships between independent factors and patients’ social support cannot be determined because this is only a cross-sectional study.
Employing a convenience sampling method for recruiting patients can give rise to some biases and lower the ability of generalisation.
Background
Illicit drug use is one of the major global public health issues. Misusing drugs can result in many pernicious effects on users’ health, such as increasing the risk of suffering from drug use disorders.1 People with drug use disorders must face numerous issues, such as mental health disorders (depression and anxiety), socioeconomic disadvantages, increased difficulties in finding and remaining in employment, financial instability and indigence.2,5 In recent years, online sales have made access to illicit drugs simpler than ever.6 Despite proven dangers and detrimental effects on health, illicit use of drugs still has persisted and proliferated recently.
In 2020, it was estimated that 284 million people aged from 15 to 64 years old worldwide used drugs at least once and 38.6 million people suffered from drug use disorders. About 11.2 million people injected drugs, including half of them living with hepatitis C, 1.4 million cases living with HIV and 1.2 million cases living with both. The number of people using illicit drugs in 2019 rose by 22% from 2010 and was forecast to increase by 11% in 2030, especially in Africa (increased by 40%). Notably, illicit drug use was the rationale behind the deaths of about 494 000 people and the loss of 30.9 million years of healthy life in 2019.1 7 In Vietnam, as of December 2020, there were more than 235 000 drug users and most of them used amphetamine-type stimulants (about 70–80%).8 Methadone maintenance treatment, a long-term medication, can help reduce criminal activities and improve drug users’ social well-being.9 According to the statistics of the Ministry of Health, as of 2023, roughly 50 353 patients used methadone to treat opioid dependence in 343 methadone clinics in Vietnam.10
Methadone maintenance patients usually have to face numerous difficulties and challenges during their treatment process, such as retention, psychological distress and high levels of stigma and discrimination from other people.11,13 High rates of treatment non-adherence, dropout and opioid relapse were found among these patients in previous studies.14 15 More importantly, in the context of the COVID-19 pandemic, frequent in-person clinic visits can make a contribution to putting patients at risk of COVID-19 exposure.16 If offered to take methadone home without any comprehensive monitoring plans, they also can face some issues such as overdose, non-adherence and illegal drug trade.17 Social support, which plays a key role in maintaining good physical and mental health, is a crucial factor contributing to the success of methadone treatment and the recovery of patients.1418,22 During the COVID-19 outbreaks, lockdowns and self-isolation may hinder family members, healthcare workers and other people from supporting patients, especially those living alone. This research was carried out to measure the social support status and associated factors among methadone maintenance patients in a metropolis and two mountainous provinces of Vietnam in the context of the COVID-19 pandemic.
Methods
Setting and participants
This study is a part of a larger project conducted to investigate social support and its influences among methadone maintenance patients from various perspectives.14 18 This cross-sectional study was conducted in three methadone clinics in Vietnam (including one clinic in the Hanoi capital—a metropolitan area and two clinics in Dien Bien and Son La provinces—two mountainous areas). These health facilities were selected on purpose. Participants were recruited using a convenience sampling method. The inclusion criteria included patients aged 18 and above, having the capacity to listen and speak Vietnamese, and not contracting mental disorders or severe diseases. The minimum sample size was computed using the formula n=Z21−α/2. σ2/d2. With Z=1.96 (5% significance level), σ (SD) of 22.9,23 and d (an absolute precision) of 2; the minimum sample size was 504. It was estimated that there were approximately 1013 patients in three selected clinics. From December 2021 to March 2022, the research team approached 556 patients. Sixteen patients refused to engage in this study. A total of 540 patients (180 in each clinic) were included in the final analysis (response rate: 97.1%).
Patient and public involvement
Patients and the public were not involved in the design, conduct, reporting or dissemination plans of this study.
Procedures and measurements
With the support of the medical personnel working in the three clinics above, patients were invited to participate in this research when they came to clinics to take methadone. Data collectors (the authors and master’s students from the Hanoi University of Pharmacy) introduced the study’s aim and objectives to patients. Then, voluntary participants had face-to-face interviews with data collectors (a paper-based survey). After finishing the interview with each patient, the data collectors would check all questions in the data collection form to avoid missing values.
The questionnaire consisted of two main parts: (1) the general demographic characteristics of patients and (2) the Medical Outcomes Study—Social Support Survey (MOS-SSS) Questionnaire. The former (independent variables) included questions involving patients’ age, sex, highest level of education, place of residence, family members, occupation, financial autonomy and the monthly income of the patient and his/her family. The latter (dependent variable) consisted of one question about the number of close friends/relatives the patient felt at ease with and could talk to about what was on his/her mind and 19 other questions (items) measuring the functional aspects of social support. The main part of the MOS-SSS Questionnaire comprises four domains of social support (including tangible support: 4 items, emotional-information support: 8 items, positive social interaction: 3 items and affectionate support: 3 items) and one additional item.24 For each item, patients could choose one of five following answers: (1) none of the time/never, (2) a little of the time/rarely, (3) some of the time/sometimes, (4) most of the time/usually and (5) all of the time/always (a 5-point Likert rating scale). The MOS-SSS Questionnaire was translated into Vietnamese. The reliability and validity of this Vietnamese version were demonstrated in a previous study.23 In our study, with the data of 540 patients, Cronbach’s alpha of 0.96 for the overall scale (0.92 for emotional-information support, 0.89 for tangible support, 0.88 for affectionate support and 0.83 for positive social interaction) demonstrated good internal consistency of this instrument.
Data analysis
The data were analysed using R V.4.4.0.25 Frequencies and percentages were used to summarise the data about categorical variables (such as sex and place of residence), while means (SD) and medians (25th–75th/min–max) were employed to summarise the data involving numeric variables (such as age and monthly income). The normal distribution of quantitative variables was assessed using histograms and the Shapiro-Wilk test (p value>0.05 indicated a normally distributed continuous variable). Because of the non-normal distribution of data, the differences in social support scores were analysed using the Wilcoxon rank-sum test (between two patient groups) and the Kruskal-Wallis test/Dunn test for multiple comparisons (among three patient groups or more). The social support score for each patient was calculated using the equation (1):
| (1) |
Including:
Observed scores were assigned following the answers of patients (none of the time/never=1, a little of the time/rarely=2, some of the time/sometimes=3, most of the time/usually=4 and all of the time/always=5).
Minimum possible score=1.
Maximum possible score=5.26
The social support average scores were computed for the overall MOS-SSS Scale (19 items) and four subscales. The higher scores indicated more social support. Factors associated with the social support status of patients were determined through univariate and multivariate linear regression models. For the multivariate linear regression, variables in this model were selected using the Bayesian model averaging method, which is a widely used method for variable selection. In addition, the least absolute shrinkage and selection operator regression was also reported. These models were the modifications of linear regression to minimise the complexity of models, be more resistant to outliers and the spread of data, and prevent overfitting and multicollinearity. A p value lower than 0.001 was considered statistical significance.
Results
Participants’ characteristics
A total of 540 patients concurred to take part in this research. Most of them were men (98.89%) and individuals aged from 31 to 60 years old (86.30%). Three-quarters graduated from a secondary or high school and then stopped studying. Almost a quarter of the participants did not work. A third were entirely economically dependent on their family members or relatives. On average, the monthly income of patients and their families was approximately 2.98 million Vietnam dongs (US$130.39) and 7.47 million Vietnam dongs (US$326.84), respectively. A majority of patients (95.37%) were living with at least one person (mainly their spouses and offspring). Commonly, a patient lived with from 2 to 3 family members and had from 2 to 4 close friends/relatives whom he/she felt at ease with and could talk about what was on his/her mind (table 1).
Table 1. Baseline characteristics of participants (n=540 patients).
| Patients’ characteristics | Summary statistics | |||
| Categorical variables | Number | Percentage | ||
| Sex | Male | 534 | 98.89 | |
| Female | 6 | 1.11 | ||
| Highest level of education | Illiterate | 19 | 3.52 | |
| Primary school | 52 | 9.63 | ||
| Secondary school | 219 | 40.56 | ||
| High school | 194 | 35.93 | ||
| Intermediate/college | 38 | 7.04 | ||
| University or higher | 18 | 3.33 | ||
| Place of residence (province) | Dien Bien | 180 | 33.33 | |
| Hanoi | 180 | 33.33 | ||
| Son La | 180 | 33.33 | ||
| Living with somebody | No | 25 | 4.63 | |
| Yes | Wife/husband | 302 | 55.93 | |
| Father | 194 | 35.93 | ||
| Mother | 285 | 52.78 | ||
| Son/daughter | 283 | 52.41 | ||
| Others | 22 | 4.07 | ||
| Working | No | 128 | 23.70 | |
| Yes | Farmer | 123 | 22.78 | |
| Freelancer | 175 | 32.41 | ||
| Trader | 40 | 7.41 | ||
| Other occupations | 74 | 13.70 | ||
| Financial autonomy | Dependent | 174 | 32.22 | |
| Partial | 239 | 44.26 | ||
| Full | 127 | 23.52 | ||
| Type of occupation | Non-working | 128 | 23.70 | |
| Seasonal/part-time | 258 | 47.78 | ||
| Full-time | 154 | 28.52 | ||
| Numeric variables | Mean (SD) | Median (25th–75th) | ||
| Age | 42.01 (9.41) | 42 (36–49) | ||
| Number of family members living with the patient | 2.47 (1.39) | 2 (2–3) | ||
| Patient’s monthly income (million VNDs) | 2.98 (3.27) | 2.00 (0.00–4.78) | ||
| Family’s monthly income (million VNDs) | 7.47 (6.62) | 5.00 (4.00–10.00) | ||
| Number of close friends/relatives | 3.39 (2.97) | 3 (2–4) | ||
Exchange rate: 1 million Vietnam dongs (VNDs)=US$43.7541.
The social support status of methadone maintenance patients
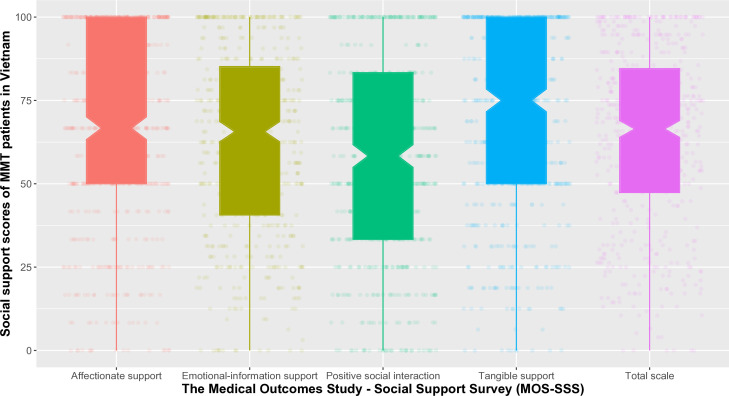
The social support average score of all 540 patients was 63.50±26.54 (out of 100). Only 162 patients (30.00%) had a social support score of 80 or higher. Among four subscales, the average score of the ‘Tangible support’ subscale was the highest (68.77±29.27), while that of the ‘Positive social interaction’ subscale was the lowest (56.93±30.58) (figure 1). The average scores of all MOS-SSS items were higher than 50.00, ranging from 51.53 to 71.67. Among 19 items, nearly half of the patients always had somebody to take them to the doctor (46.85%) and prepare meals for them (46.85%). In addition, 43.70% of patients had at least one person who always showed them love and affection. These items were the three with the highest average scores (71.67±32.49, 70.23±33.11 and 70.65±31.97, respectively). Furthermore, a fifth of patients said they did not have anyone to get together with for relaxation (18.52%) or do something enjoyable with them (17.22%). The average scores of these two items were also the lowest (51.53±35.34 and 55.97±36.39, respectively) (table 2).
Figure 1. The distribution of the social support scores of methadone maintenance patients. The average social support score of patients was 63.50±26.54 for the total scale. Regarding four domains, the average score of the ‘Tangible support’ subscale, the ‘Positive social interaction’ subscale, the ‘Emotional-Informational support’ scale and the ‘Affectionate support’ was 68.77±29.27, 56.93±30.58, 62.87±27.66 and 66.06±29.91, respectively. MMT, methadone maintenance treatment.
Table 2. The responses of patients to MOS-SSS items and the scores for each item.
| MOS-SSS items | Answers (n (%)) | Social support scores | |||||
| Never | Rarely | Sometimes | Usually | Always | Mean (SD) | Median (25th–75th) | |
| Tangible support | 68.77(29.27) | 75.00 (50.00–100.00) | |||||
| Help you if you are confined to bed | 75 (13.89) | 33 (6.11) | 130 (24.07) | 84 (15.56) | 218 (40.37) | 65.60 (35.37) | 75 (50–100) |
| Take you to the doctor | 40 (7.41) | 51 (9.44) | 103 (19.07) | 93 (17.22) | 253 (46.85) | 71.67 (32.49) | 75 (50–100) |
| Prepare meals for you | 39 (7.22) | 61 (11.30) | 117 (21.67) | 70 (12.96) | 253 (46.85) | 70.23 (33.11) | 75 (50–100) |
| Help you with daily chores | 35 (6.48) | 94 (17.41) | 107 (19.81) | 64 (11.85) | 240 (44.44) | 67.59 (33.89) | 75 (50–100) |
| Emotional-informational support | 62.87(27.66) | 65.63 (40.63–85.16) | |||||
| Listen to you | 35 (6.48) | 72 (13.33) | 134 (24.81) | 85 (15.74) | 214 (39.63) | 67.18 (32.27) | 75 (50–100) |
| Give you good advice | 38 (7.04) | 54 (10.00) | 136 (25.19) | 104 (19.26) | 208 (38.52) | 68.06 (31.58) | 75 (50–100) |
| Give you information | 60 (11.11) | 78 (14.44) | 128 (23.70) | 98 (18.15) | 176 (32.59) | 61.67 (34.09) | 75 (25–100) |
| Someone to confide in | 59 (10.93) | 69 (12.78) | 121 (22.41) | 99 (18.33) | 192 (35.56) | 63.70 (34.22) | 75 (50–100) |
| Give advice you want | 66 (12.22) | 79 (14.63) | 123 (22.78) | 92 (17.04) | 180 (33.33) | 61.16 (34.85) | 75 (25–100) |
| Share worries with you | 90 (16.67) | 80 (14.81) | 116 (21.48) | 91 (16.85) | 163 (30.19) | 57.27 (36.32) | 50 (25–100) |
| Turn to for suggestions | 66 (12.22) | 71 (13.15) | 107 (19.81) | 96 (17.78) | 200 (37.04) | 63.56 (35.26) | 75 (25–100) |
| Understand your problems | 76 (14.07) | 71 (13.15) | 130 (24.07) | 80 (14.81) | 183 (33.89) | 60.32 (35.63) | 50 (25–100) |
| Positive social interaction | 56.93(30.58) | 58.33(33.33–83.33) | |||||
| Have a good time with you | 57 (10.56) | 70 (12.96) | 135 (25.00) | 85 (15.74) | 193 (35.74) | 63.29 (34.09) | 75 (50–100) |
| Get together for relaxation | 100 (18.52) | 91 (16.85) | 157 (29.07) | 60 (11.11) | 132 (24.44) | 51.53 (35.34) | 50 (25–75) |
| Do something enjoyable with you | 93 (17.22) | 86 (15.93) | 117 (21.67) | 87 (16.11) | 157 (29.07) | 55.97 (36.39) | 50 (25–100) |
| Affectionate support | 66.06(29.91) | 66.67(50.00–100.00) | |||||
| Show you love and affection | 36 (6.67) | 58 (10.74) | 106 (19.63) | 104 (19.26) | 236 (43.70) | 70.65 (31.97) | 75 (50–100) |
| Give you comforting gestures | 58 (10.74) | 70 (12.96) | 162 (30.00) | 57 (10.56) | 193 (35.74) | 61.90 (34.20) | 50 (50–100) |
| Love and make you feel wanted | 49 (9.07) | 74 (13.70) | 115 (21.30) | 94 (17.41) | 208 (38.52) | 65.65 (33.79) | 75 (50–100) |
| Additional item | |||||||
| Help you get your mind off things | 72 (13.33) | 79 (14.63) | 126 (23.33) | 98 (18.15) | 165 (30.56) | 59.49 (34.85) | 50 (25–100) |
| Total | 63.50 (26.54) | 66.45 (47.37–84.54) | |||||
MOS-SSSMedical Outcomes Study—Social Support Survey
Comparing the social support average scores among patient groups
The social support average score of female patients (81.14±17.59) was higher than that of male patients (63.30±26.57). University graduates had an average score higher than other groups. However, these differences were not statistically significant (p=0.116 and p=0.334, respectively). Among three provinces, the average score of patients living in Hanoi (80.61±23.47) was significantly higher than that of patients residing in mountainous areas, including Dien Bien (63.74±23.67, p<0.001) and Son La (46.15±20.31, p<0.001). Regarding types of occupation, the average score of full-timers (72.75±18.72) was significantly higher than that of part-timers/people with seasonal jobs (57.93±28.04, p<0.001) and patients not working (63.59±28.44, p=0.031). In addition, patients who led a solitary life (48.84±28.69) had an average score significantly lower than individuals living with at least one person (64.21±26.25) (p=0.013). More importantly, the higher the number of family members living with the patient and his/her close friends/relatives, the higher the average social support score (table 3).
Table 3. The comparisons of social support average scores among patient groups.
| Patients’ characteristics (n) | Average score (SD) | Median (min, max) | P value | |
| Sex | Male (534) | 63.30 (26.57) | 65.79 (0, 100.0) | 0.116 |
| Female (6) | 81.14 (17.59) | 86.84 (50.0, 94.74) | ||
| Age | 30 and under (61) | 53.45 (24.14) | 61.84 (13.16, 100.0) | 0.007 |
| 31–40 (177) | 63.04 (27.12) | 65.79 (0, 100.0) | ||
| 41–50 (201) | 65.47 (27.13) | 68.42 (0, 100.0) | ||
| 50 and above (101) | 66.45 (24.53) | 68.42 (0, 100.0) | ||
| Highest level of education | Illiterate (19) | 64.82 (13.39) | 64.47 (28.95, 89.47) | 0.334 |
| Primary school (52) | 69.00 (21.05) | 68.42 (0, 100.0) | ||
| Secondary school (219) | 61.13 (27.06) | 63.16 (0, 100.0) | ||
| High school (194) | 63.31 (28.55) | 69.08 (0, 100.0) | ||
| Intermediate/college (38) | 66.03 (24.45) | 72.37 (3.95, 100.0) | ||
| University or higher (18) | 71.71 (24.81) | 76.32 (10.53, 100.0) | ||
| Place of residence (province) | Dien Bien (180) | 63.74 (23.67) | 67.11 (0, 100.0) | <0.001 |
| Hanoi (180) | 80.61 (23.47) | 89.47 (0, 100.0) | ||
| Son La (180) | 46.15 (20.31) | 50.00 (6.58, 80.26) | ||
| Living with somebody | No (25) | 48.84 (28.69) | 42.11 (0, 100.0) | 0.013 |
| Yes (515) | 64.21 (26.25) | 67.11 (0, 100.0) | ||
| Number of family members living with the patient | 0 (25) | 48.84 (28.69) | 42.11 (0, 100.0) | <0.001 |
| 1 (108) | 55.62 (26.01) | 57.90 (0, 100.0) | ||
| 2 (166) | 59.12 (28.19) | 61.84 (0, 100.0) | ||
| 3 (131) | 68.27 (25.29) | 69.74 (0, 100.0) | ||
| 4 (70) | 71.82 (17.65) | 68.42 (25.00, 100.0) | ||
| >4 (40) | 81.91 (19.68) | 84.87 (0, 100.0) | ||
| Occupation | Non-working (128) | 63.59 (28.44) | 68.42 (0, 100.0) | <0.001 |
| Farmer (123) | 64.22 (15.90) | 64.47 (22.37, 100.0) | ||
| Freelancer (175) | 56.73 (30.14) | 55.26 (0, 100.0) | ||
| Trader (40) | 63.49 (29.13) | 63.82 (13.16, 100.0) | ||
| Other occupations (74) | 78.16 (20.59) | 80.26 (0, 100.0) | ||
| Type of occupation | Non-working (128) | 63.59 (28.44) | 68.42 (0, 100.0) | <0.001 |
| Seasonal/part-time (258) | 57.93 (28.04) | 57.90 (0, 100.0) | ||
| Full-time (154) | 72.75 (18.72) | 71.05 (0, 100.0) | ||
| Financial autonomy | Dependent (174) | 64.25 (26.02) | 67.11 (0, 100.0) | <0.001 |
| Partial (239) | 59.67 (25.99) | 63.16 (0, 100.0) | ||
| Full (127) | 69.67 (27.21) | 73.68 (0, 100.0) | ||
| Number of close friends/relatives | 0 (22) | 25.90 (23.43) | 21.05 (0, 76.32) | <0.001 |
| 1 (74) | 36.49 (22.90) | 27.63 (3.95, 96.05) | ||
| 2 (155) | 55.65 (25.19) | 53.95 (0, 100.0) | ||
| 3 (114) | 69.39 (15.05) | 66.45 (42.11, 100.0) | ||
| 4 (52) | 73.20 (13.47) | 72.37 (32.90, 100.0) | ||
| 5 (63) | 78.72 (16.19) | 78.95 (31.58, 100.0) | ||
| >5 (60) | 95.31 (6.149) | 97.37 (76.32, 100.0) | ||
| Patient’s income per month(million VNDs) | No income (143) | 64.79 (27.95) | 69.74 (0, 100.0) | <0.001 |
| 0.01–2.00 (129) | 61.53 (18.62) | 64.47 (0, 100.0) | ||
| 2.01–4.00 (131) | 52.84 (27.80) | 53.95 (0, 100.0) | ||
| 4.01–6.00 (79) | 65.41 (27.49) | 71.05 (14.47, 100.0) | ||
| >6.00 (58) | 86.18 (18.34) | 94.74 (17.11, 100.0) | ||
| Family’s income per month(million VNDs) | 0–3.33 (111) | 50.64 (26.38) | 53.95 (0, 100.0) | <0.001 |
| 3.34–6.67 (227) | 57.22 (24.79) | 61.84 (0, 100.0) | ||
| 6.68–10.00 (123) | 70.75 (22.93) | 73.68 (0, 100.0) | ||
| >10.00 (79) | 88.32 (15.03) | 94.74 (27.63, 100.0) | ||
Exchange rate: 1 million Vietnam dongs (VNDs)=US$43.7541.
Factors associated with the social support of methadone maintenance patients
The results from the multivariate linear regression analyses showed that factors associated with the social support scores of methadone maintenance patients included the place of residence (p<0.001), patient’s occupation (p<0.001), the type of occupation (p=0.001), family income per month (p<0.001), the number of people living with the patients (p<0.001) and the number of close friends/relatives (p<0.001). Strongly positively associated with higher social support scores were the three last factors mentioned above. In comparison with patients living in Dien Bien, living in Hanoi was significantly associated with a higher level of social support (p=0.004), while residing in Son La was highly associated with lower social support scores (p<0.001). Patients with full-time occupations were also strongly associated with a higher level of social support when compared with those with seasonal/part-time jobs and non-working individuals. In addition, based on the univariate linear regression models, the patient’s age and monthly income can be two other factors positively associated with the social support scores (p<0.001 and p<0.001, respectively) (table 4).
Table 4. Factors associated with the social support status of methadone maintenance patients in Vietnam.
| Independent variables | Univariate linear regression | Multivariate linear regression | |||||
| LASSO | BMA | ||||||
| Coef | P value | Coef | P value | Coef | P value | ||
| Sex (ref: female) | Male | −17.84 | 0.102 | ||||
| Age | 0.417 | <0.001 | |||||
| Place of residence (ref: Dien Bien) | Hanoi | 16.864 | <0.001 | 5.191 | 0.019 | 6.129 | 0.004 |
| Son La | −17.595 | <0.001 | −20.417 | <0.001 | −23.662 | <0.001 | |
| Education level (ref: high school) | Illiterate | 1.513 | 0.812 | ||||
| Primary school | 5.696 | 0.169 | |||||
| Secondary school | −2.174 | 0.406 | |||||
| Intermediate/college | 2.725 | 0.563 | |||||
| University/higher | 8.403 | 0.199 | |||||
| Occupation (ref: farmer) | Non-working | −0.627 | 0.847 | −21.103 | <0.001 | ||
| Freelancer | −7.488 | 0.014 | −14.744 | <0.001 | |||
| Trader | −0.730 | 0.876 | −14.931 | <0.001 | |||
| Others | 13.948 | <0.001 | −15.381 | <0.001 | |||
| Type of occupation (ref: full-time) | Non-working | −9.163 | 0.003 | −11.372 | <0.001 | ||
| Seasonal/part-time | −14.822 | <0.001 | −10.432 | <0.001 | −7.686 | 0.001 | |
| Financial autonomy (ref: dependent) | Partial | −4.574 | 0.081 | ||||
| Full | 5.428 | 0.078 | |||||
| Living with somebody (ref: no) | Yes | 15.368 | 0.005 | ||||
| Number of family members living with the patient | 5.817 | <0.001 | 3.046 | <0.001 | 2.277 | <0.001 | |
| Patient’s income per month (million VNDs) | 1.632 | <0.001 | |||||
| Family’s income per month (million VNDs) | 1.614 | <0.001 | 0.309 | 0.034 | 0.528 | <0.001 | |
| Number of close friends/relatives | 4.939 | <0.001 | 2.818 | <0.001 | 2.854 | <0.001 | |
| Multiple R2 | 0.5029 | 0.5406 | |||||
| Adjusted R2 | 0.4963 | 0.5319 | |||||
Exchange rate: 1 million Vietnam dongs (VNDs)=US$43.7541. Variance Inflation Factors (VIFs) of all independent variables in two multivariate linear models are lower than 3.8.
BMABayesian model averagingCoefcoefficientLASSOleast absolute shrinkage and selection operatorrefreference
Discussion
This is the first study conducted in multiple methadone clinics to evaluate the social support status and its associated factors among methadone maintenance patients in Vietnam during the COVID-19 pandemic. The results showed that a majority of participants were men aged from 31 to 60. Numerous patients had a low level of education, did not work, had no or negligible income per month, and had to live dependently on other family members. Furthermore, patients received a moderate level of social support, with only a third having a score of 80 and above. Higher social support scores were witnessed among patients living in a metropolitan area, full-timers, and those living with somebody (in comparison with patients residing in mountainous areas, part-timers/non-working patients, and those living alone, respectively). Besides the place of residence and patients’ occupation, the number of family members living with the patients, the number of close friends/relatives, and the total monthly income of their families were three other factors significantly associated with their social support status. The correlation between social support and these three factors was positive.
The place of residence was a significant factor associated with social support. The social support average score of those living in metropolitan areas was significantly higher than that of those living in mountainous areas. The population density can be a reason for this finding. In 2021, according to the statistics of the Vietnam General Statistics Office, the population density in Hanoi was 2480 people/km2, while the figures for Dien Bien and Son La were only 66 and 91 people/km2, respectively.27 People living in densely populated areas have many chances of making friends and expanding relationships, thereby contributing to increasing their social support status. In fact, the average number of close friends/relatives of patients living in Hanoi (mean=5.14, median=5) was significantly higher than that of those living in Dien Bien (mean=2.71, median=2) and Son La (mean=2.32, median=2) (p<0.001). In the context of the COVID-19 pandemic, patients living in cities could have a higher risk of contracting this virus in the light of high population density. However, when necessary, patients still may easily receive support from their neighbours. By contrast, in mountainous areas, difficulties involving transportation may affect patients living alone, especially during lockdowns and self-isolation. As a result, the government needs to have practical solutions to support patients living in remote areas during plagues.
Another important factor associated with the social support status was the patient and family’s monthly income. It is noted that there was a strong relationship between family income and patient income per month (p<0.001). A patient with a higher personal/family income can cover cost-of-living expenses, pay the cost of methadone therapy, and have a better physical and mental health status. Monthly income was also a factor associated with objective support (p=0.005) and social support (p=0.047) among people living with HIV in China.28 In Vietnam, healthcare expenditure usually burdens methadone maintenance patients, especially those living under the breadline.29 The COVID-19 pandemic may have exacerbated this situation because patients could not work and earn a living, especially during the lockdown. To ameliorate this problem, giving succour to patients with financial difficulties is of great note.
The results from this study also demonstrated the crucial roles and influences of family members living with methadone maintenance patients and close friends/relatives on their social support status. The correlation between the social support scores of patients and the number of family members living with the patients and their close friends/relatives was positive. In common, family members, especially spouses or partners, are the main sources of social support for married people. For single, widowed, or divorced patients, the roles of family members, relatives, and close friends are of paramount importance and should be an area of greater focus. A study in the USA highlighted that social support and personal social networks (including family members and friends) played a crucial role in disseminating health information for Korean-American adults in 2013.30 The family was the most important support that Iranian men on methadone maintenance therapy needed to overcome stigmatisation.31 Social support from family, friends, and specialists also made a contribution to reducing stress in patients with substance use disorders.20
In our study, the social support average score of female participants was higher than that of male participants. An important rationale behind the high score of the former is that they are more likely to share their unpleasant feelings and experiences with others, such as friends and coworkers, to reduce their psychological burdens and difficulties in life. Meanwhile, by reason of restrictive emotionality and self-reliance, a majority of male participants seemingly tend to repress their emotions and feelings. They usually endeavour to overcome difficulties and psychological pressure through their own efforts.28 32 In this study, the difference in social support scores between male participants and female participants was not statistically significant and sex was not associated with social support. Although researchers strived to involve as many female participants as possible, only six female participants enrolled in this study. This is because the number of female participants using opioids and participating in methadone maintenance treatment was negligible in Vietnam. The low number of female participants can affect statistical analyses and the reproducibility of the results involving sex. There is a need to study the association between sex and social support for methadone maintenance patients in the future.
In Vietnam, methadone maintenance patients still perceived high levels of stigma and discrimination from other people. These issues were linked to patients’ mental health disorders and unemployment.3 5 33 In Iran, women undergoing methadone maintenance treatment received a low level of social support.34 Findings from a study conducted in Michigan demonstrated the role of social support in reducing shame and stigma for individuals receiving methadone maintenance treatment.35 Perceived and received social support can influence the health-related quality of life among patients36 37 and reduce the risk of treatment non-adherence, opioid relapse, and depression.14 18 38 39 However, the level of social support for Vietnamese patients was moderate. In this study, social support was related to factors involving patients’ occupation, residence, income, family members, and close friends/relatives. As a result, they should be properly and carefully considered if the government and the authorities plan to launch campaigns to enhance social support for this patient population in the future.
Limitations
This study has several following limitations. First and foremost, this is only a cross-sectional study, and therefore, findings cannot confirm the causal relationships between social support and independent factors. Second, the high prevalence of male patients can affect the reproducibility of findings involving patients’ sex. In addition, by virtue of difficulties in transportation during the outbreaks of the COVID-19 pandemic and the paucity of funding, we had to use a convenience sampling method to recruit patients, which can give rise to several potential biases. With only 540 participants in three clinics, the results may not be representative of methadone maintenance patients in Vietnam and limit the ability of generalisation.
Conclusions
During the COVID-19 pandemic, Vietnamese methadone maintenance patients only received a moderate level of social support. Factors associated with their social support status included the place of residence, occupation, age, patient/family’s monthly income, the number of family members living with the patient, and the number of close friends/relatives. In the context of pandemics, not only the authorities but also family members and the community should give succour and strength to the patients, thereby contributing to the success of methadone treatment and the recovery of patients.
Acknowledgements
The authors would like to thank the medical personnel and colleagues who were working in methadone clinics and assisted us in the process of data collection. We also appreciate the enthusiastic participation of all 540 patients in this study.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial, or not-for-profit sectors.
Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-081519).
Data availability free text: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by the ethical committee of Hanoi University of Pharmacy (reference number: 21-12/PTC-HĐĐĐ). Written informed consent was obtained from all 540 patients. Participants gave informed consent to participate in the study before taking part.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Huong Thi Thanh Nguyen, Email: huongnguyenthanh@hup.edu.vn.
Dien Quang Tran, Email: dylantran.phar@gmail.com.
Dai Xuan Dinh, Email: daidinh.hup@gmail.com.
Data availability statement
Data are available on reasonable request.
References
- 1.United Nations Office on Drugs and Crime . United Nations Publication; 2022. World drug report 2022. [Google Scholar]
- 2.Momen NC, Plana-Ripoll O, Agerbo E, et al. Association between Mental Disorders and Subsequent Medical Conditions. N Engl J Med. 2020;382:1721–31. doi: 10.1056/NEJMoa1915784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tran BX, Boggiano VL, Thi Nguyen HL, et al. Concurrent drug use among methadone maintenance patients in mountainous areas in northern Vietnam. BMJ Open. 2018;8:e015875. doi: 10.1136/bmjopen-2017-015875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plana-Ripoll O, Pedersen CB, Holtz Y, et al. Exploring Comorbidity Within Mental Disorders Among a Danish National Population. JAMA Psychiatry. 2019;76:259–70. doi: 10.1001/jamapsychiatry.2018.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nong VM, Boggiano VL, Nguyen LHT, et al. Ability to join the workforce and work productivity among drug users under methadone maintenance treatment in a mountainous area of Northern Vietnam: a cross-sectional study. BMJ Open. 2017;7:e016153. doi: 10.1136/bmjopen-2017-016153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations Office on Drugs and Crime . United Nations Publication; 2023. World drug report 2023. [Google Scholar]
- 7.United Nations Office on Drugs and Crime . United Nations publication; 2021. World drug report 2021. [Google Scholar]
- 8.Vietnam Ministry of Labour . War Invalids and Social Affairs; 2021. Report on the situation and results of the prevention and control of prostitution and drug addiction treatment in 2020 and orientations, tasks in 2021. [Google Scholar]
- 9.Sun H-M, Li X-Y, Chow EPF, et al. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open. 2015;5:e005997. doi: 10.1136/bmjopen-2014-005997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vietnam Ministry of Health HIV/aids prevention plan for 2024 number /QĐ370 BYT. 2024
- 11.Zhang L, Chow EPF, Zhuang X, et al. Methadone Maintenance Treatment Participant Retention and Behavioural Effectiveness in China: A Systematic Review and Meta-Analysis. PLoS ONE. 2013;8:e68906. doi: 10.1371/journal.pone.0068906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen LH, Tran BX, Nguyen HLT, et al. Psychological Distress Among Methadone Maintenance Patients in Vietnamese Mountainous Areas. AIDS Behav. 2017;21:3228–37. doi: 10.1007/s10461-017-1779-5. [DOI] [PubMed] [Google Scholar]
- 13.Le TA, Le MQT, Dang AD, et al. Multi-level predictors of psychological problems among methadone maintenance treatment patients in difference types of settings in Vietnam. Subst Abuse Treat Prev Policy. 2019;14:39. doi: 10.1186/s13011-019-0223-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen HTT, Dinh DX. Opioid relapse and its predictors among methadone maintenance patients: a multicenter, cross-sectional study in Vietnam. Harm Reduct J. 2023;20:136. doi: 10.1186/s12954-023-00872-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chao E, Hung C-C, Lin C-P, et al. Adherence among HIV-positive injection drug users undergoing methadone treatment in Taiwan. BMC Psychiatry. 2020;20:346. doi: 10.1186/s12888-020-02764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brothers S, Palayew A, Simon C, et al. Patient experiences of methadone treatment changes during the first wave of COVID-19: a national community-driven survey. Harm Reduct J. 2023;20:31. doi: 10.1186/s12954-023-00756-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang H, Su H, Zhang C, et al. Challenges of methadone maintenance treatment during the COVID-19 epidemic in China: Policy and service recommendations. Eur Neuropsychopharmacol. 2020;35:136–7. doi: 10.1016/j.euroneuro.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen HTT, Dinh DX. Treatment non-adherence among methadone maintenance patients and associated factors: a multicenter, cross-sectional study in Vietnam. Harm Reduct J. 2024;21:129. doi: 10.1186/s12954-024-01040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quyen BTT, Nguyen LT, Phuong VTV, et al. Quality of life in methadone maintenance treated patients in Long An, a southern province of Vietnam. Health Psychol Open. 2020;7:2055102920953053. doi: 10.1177/2055102920953053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang C, Xia M, Li T, et al. How Do Specific Social Supports (Family, Friend, and Specialist) Reduce Stress in Patients With Substance Use Disorders: A Multiple Mediation Analysis. Front Psychiatry. 2021;12:618576. doi: 10.3389/fpsyt.2021.618576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laudet AB, Morgen K, White WL. The Role of Social Supports, Spirituality, Religiousness, Life Meaning and Affiliation with 12-Step Fellowships in Quality of Life Satisfaction Among Individuals in Recovery from Alcohol and Drug Problems. Alcohol Treat Q. 2006;24:33–73. doi: 10.1300/J020v24n01_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin C, Wu Z, Detels R. Family support, quality of life and concurrent substance use among methadone maintenance therapy clients in China. Public Health. 2011;125:269–74. doi: 10.1016/j.puhe.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khuong LQ, Vu T-VT, Huynh V-AN, et al. Psychometric properties of the medical outcomes study: social support survey among methadone maintenance patients in Ho Chi Minh City, Vietnam: a validation study. Subst Abuse Treat Prev Policy. 2018;13:8. doi: 10.1186/s13011-018-0147-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 25.R Core Team . Vienna, Austria: R Foundation 415 for Statistical Computing, Vienna, Austria; 2021. [30-Oct-2023]. R: a language and environment for statistical computing.https://www.R-project.org Available. accessed. [Google Scholar]
- 26.The RAND Corporation Social support survey instrument scoring instructions. 2023. [30-Oct-2023]. https://www.rand.org/health-care/surveys_tools/mos/social-support/scoring.html Available. Accessed.
- 27.Vietnam General Statistics Office Area, population and population density by province. 2023. [30-Oct-2023]. https://www.gso.gov.vn/en/px-web/?pxid=E0201&theme=Population%20and%20Employment Available. Accessed.
- 28.Li Y, Zhang X-W, Liao B, et al. Social support status and associated factors among people living with HIV/AIDS in Kunming city, China. BMC Public Health. 2021;21:1413. doi: 10.1186/s12889-021-11253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tran BX, Phan HTT, Nguyen LH, et al. Economic vulnerability of methadone maintenance patients: Implications for policies on co-payment services. Int J Drug Policy. 2016;31:131–7. doi: 10.1016/j.drugpo.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 30.Kim W, Kreps GL, Shin CN. The role of social support and social networks in health information-seeking behavior among Korean Americans: a qualitative study. Int J Equity Health. 2015;14:40. doi: 10.1186/s12939-015-0169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aghakhani N, Lopez V, Cleary M. Experiences and Perceived Social Support among Iranian Men on Methadone Maintenance Therapy: A Qualitative Study. Issues Ment Health Nurs. 2017;38:692–7. doi: 10.1080/01612840.2017.1341586. [DOI] [PubMed] [Google Scholar]
- 32.Gough B, Robertson S, Luck H. Engendered Expressions of Anxiety: Men’s Emotional Communications With Women and Other Men. Front Sociol . 2021;6:697356. doi: 10.3389/fsoc.2021.697356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Nguyen H, Nguyen HLT, Mai HT, et al. Stigmatization among methadone maintenance treatment patients in mountainous areas in northern Vietnam. Harm Reduct J. 2017;14:1. doi: 10.1186/s12954-016-0127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rahimi S, Raheimi S, Jalali A, et al. Social Support Among Women Undergoing Methadone Maintenance Treatment in Iran. J Addict Nurs. 2018;29:179–87. doi: 10.1097/JAN.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 35.Broman MJ, Pasman E, Brown S, et al. Social support is associated with reduced stigma and shame in a sample of rural and small urban adults in methadone treatment. Addict Res Theory. 2023;31:37–44. doi: 10.1080/16066359.2022.2101640. [DOI] [Google Scholar]
- 36.Zhou K, Li H, Wei X, et al. Relationships between received and perceived social support and health-related quality of life among patients receiving methadone maintenance treatment in Mainland China. Subst Abuse Treat Prev Policy. 2017;12:33. doi: 10.1186/s13011-017-0116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chou Y-C, Shih S-F, Tsai W-D, et al. Improvement of quality of life in methadone treatment patients in northern Taiwan: a follow-up study. BMC Psychiatry. 2013;13:190. doi: 10.1186/1471-244X-13-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wahab S, Chun Keat T, Azmi AD, et al. Risk of Depression Among MMT Patients: Does Coping Strategies and Perceived Social Support Play a Role? Subst Abuse. 2021;15:11782218211049407. doi: 10.1177/11782218211049407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X, Xu H, Gu J, et al. Depression, suicidal ideation, and related factors of methadone maintenance treatment users in Guangzhou, China. AIDS Care. 2016;28:851–6. doi: 10.1080/09540121.2015.1124981. [DOI] [PMC free article] [PubMed] [Google Scholar]