Abstract
Background
High turnover among the medical professions is detrimental to the healthcare system and population well-being, particularly in low- and middle-income countries (LMICs) with limited financial and human resources. To prevent brain drain, effective strategies are vital to improve the retention of healthcare workers, especially doctors. However, little evidence has been synthesised regarding the effectiveness of these strategies, especially in LMICs. This scoping review aimed to evaluate the retention strategies implemented in LMICs and their effectiveness in mitigating doctor turnover.
Methods
Four databases; MEDLINE (PubMed), Scopus, ScienceDirect, and EBSCOHost were searched using pre-determined keywords to identify articles published between January 1st, 2013 and February 28th, 2023 that evaluated retention strategies for doctors in LMICs. The review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Extension for Scoping Reviews (PRISMA-ScR) guidelines to ensure transparency. Relevant studies were identified, screened, and narratively synthesised.
Results
Thirteen articles were included, representing a diverse range of LMICs. Retention strategies were categorised into educational, financial incentives, regulatory, as well as professional and personal support. Approximately 77% (n = 10) of studies reported positive outcomes, another two did not achieve favourable results, while one showed mixed outcomes. An equal number of studies applying single-strategy (n = 5) and combined-strategy (n = 5) approaches reported successful outcomes, especially when focusing on education and/ or regulatory strategies. More notably, international collaboration in education strategies enhanced success rates while compulsory service enforcement by authorities helped retain doctors in underserved areas to address healthcare worker maldistribution. Efficiency in administrative management, regardless of urban or rural locations, also emerged as a key factor of successful retention.
Conclusions
This review highlighted the effectiveness of different retention strategies for doctors in LMICs and its associated factors. It is imperative to emphasise the lack of a one-size-fits-all solution for this global issue. Thus, a multifaceted, comprehensive approach is essential in producing sustainable health workforce development that ensures optimal health outcomes, especially for populations in underserved areas. Future studies should prioritise pre- and post-intervention comparisons using appropriate indicators to enhance understanding and guide effective interventions for doctor retention.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-12154-x.
Keywords: Medical doctors, LMICs, Recruitment, Retention strategies, Scoping review
Background
The quantity and distribution of the healthcare workforce are critical components of a health system's functionality as they impact healthcare accessibility and quality of care [1]. Achieving a balanced and equitable distribution of healthcare workers is essential for ensuring effective healthcare systems and promoting the well-being of populations in any country. However, in recent years, the issue of brain drain among doctors has become a global problem [2] due to excessive workloads [3], insufficient remuneration [4, 5], limited professional growth [6], suboptimal healthcare infrastructures [7, 8], and concerns about wellbeing and safety [4]. Given the negative impact of brain drain on the healthcare sector [9], collaborative efforts by governmental agencies, healthcare institutions, and professional organisations are needed to enhance working conditions and work-life balance [10, 11]. Retention, in this context, refers to the period spanning from an individual's initial engagement with a healthcare service to their eventual departure, i.e., the duration of an individual's tenure within the healthcare system.
Retention of healthcare professionals (HCPs), especially medical doctors, is a formidable challenge in low- and middle-income countries (LMICs), particularly in remote and rural regions [12], due to various factors such as resource constraints [13], rising disease burdens [14], and attractive job offers from higher-income nations [15, 16]. To address this, investments in healthcare systems are essential in incentivising HCPs to deliver essential healthcare services in areas most in need, leading to improved health outcomes and reduced disparities in healthcare access. Retention strategies in the form of targeted interventions to improve remuneration, infrastructure, career opportunities, and support systems for HCPs are important to mitigate brain drain and retain doctors in their home healthcare systems, especially in underserved regions.
In addition, the implementation of effective retention strategies plays a crucial role in boosting healthcare capacity and attaining universal health coverage, particularly in underserved regions that lack adequate healthcare services. This is especially pertinent to the United Nations' Sustainable Development Goals (SDGs), specifically, Goal 3 which emphasises the importance of ensuring access to quality healthcare and combating major diseases, and Goal 10 which focuses on reducing inequalities within and among countries. Preserving the expertise held by retained doctors is vital in reducing healthcare disparities, particularly between urban and rural areas, and promoting the economic and social inclusion of marginalised populations, aligning with the SGD’s emphasis on quality healthcare and combating major diseases.
This scoping review aimed to provide a comprehensive overview of retention strategies practised in LMICs to address the challenges of retaining medical doctors and preventing brain drain. Commonly applied retention strategies in high-income nations may not be replicable in LMICs as the implementation often depends on local contexts such as more advanced healthcare infrastructure, greater financial resources, and more robust support systems, which are not always present in LMICs. This disparity can make it challenging to implement and sustain similar retention strategies in LMICs. Therefore, this review focused on LMICs to gain input on region-specific challenges and the effectiveness of customised strategies in LMIC settings. By identifying the factors influencing the outcomes of different retention strategies, the findings can guide policymakers and healthcare administrators in developing local-customised interventions and prioritising effective strategies to improve doctor retention in LMICs, aligning with SDG 3 goal of promoting well-being and ensuring healthy lives for all.
We conducted an initial literature search to determine whether the topic of doctor retention had been explored previously and to identify any gaps in the existing research. For preliminary search, we examined three key databases: MEDLINE (PubMed), the Cochrane Database of Systematic Reviews, and JBI Evidence Synthesis. Although several reviews on doctor retention have been published, their focus diverged significantly from ours. Specifically, studies included in Noya et al. [22] and Holloway et al. [23] concentrated primarily on retention in rural and remote areas, while Verma et al. [24] examined strategies aimed at recruiting and retaining primary care physicians. In contrast to these studies, this review seeks not only to identify the spectrum of retention strategies implemented in LMICs but also to critically assess their effectiveness. This represents a shift from previous reviews, which often discussed retention strategies without evaluating their outcomes.
Methods
The protocol for this scoping review has been published [17] which serves as a guiding framework for systematically exploring and mapping the literature about medical doctors' retention strategies in LMICs. The following sections provide a concise overview of the review methodology, outlining key steps and considerations in the data collection and synthesis of relevant information for this review.
This review followed the methodological framework outlined by Arksey and O'Malley [18)] and the Joanna Briggs Institute Manual [19]. In addition, recommendations from Levac, Colquhoun, and O’Brien [20] were also incorporated to improve the quality and rigour of the review process. The following steps were performed in this scoping review: (I) Identifying a research question, (II) Retrieving relevant studies using a systematic search strategy, (III) Selecting appropriate studies for review, (IV) Charting the data, and (V) Collating, summarising and reporting the results. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses—Extension for Scoping Reviews (PRISMA-ScR) guidelines [21] in our reporting.
Stage 1: Identifying the research question
This scoping review aimed to identify strategies or interventions for retaining doctors in healthcare institutions in LMICs and to determine effective strategies for preventing doctors from leaving these institutions. The following research questions were formulated:
What are the retention strategies currently being implemented for doctors in LMICs?
Which of these strategies have been identified as effective in retaining doctors in LMICs?
Stage 2: Retrieving relevant studies
For the identification of relevant studies, a well-defined search strategy was developed, incorporating key terms such as "retention," "retain," "maintain," "doctor," "physician," "general practitioner," and "low- and middle-income countries." Four authors (NJ, IAS, PB and IKA) conducted the search across four databases; MEDLINE (PubMed), EBSCOHost, Scopus, and ScienceDirect, chosen for their comprehensive coverage of health and human services literature. The search strategy was customised for each database’s specific indexing terms and functionalities to ensure optimal retrieval of relevant articles. Details of the MEDLINE search strategy are provided in Additional File 1.
Stage 3: Study selection
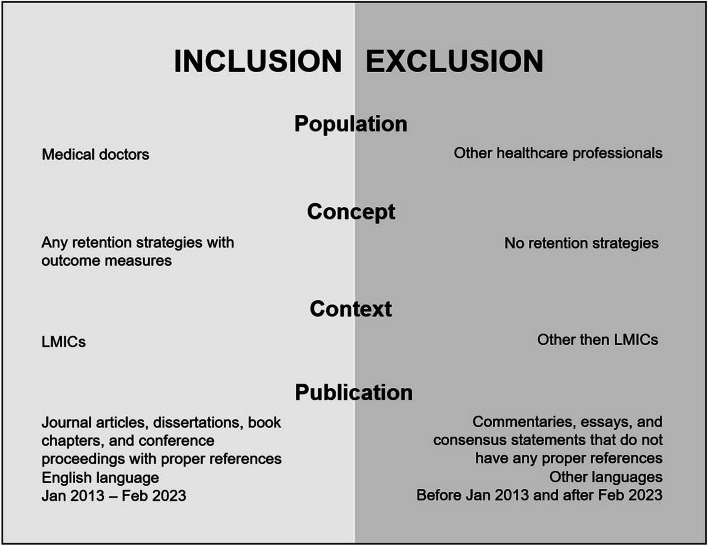
Articles published from January 1st, 2013 to February 28th, 2023 were included if the studies reported strategies that were implemented to retain medical doctors in LMICs. There were no restrictions on study design but only articles published in English were included. Studies without complete access to the full text were also excluded. Figure 1 shows the inclusion and exclusion criteria according to the PCC framework. In this review, retention strategies were treated as both interventions (strategies implemented) and outcomes (effectiveness in reducing turnover). Given the limited studies that measured direct retention outcomes, evaluating retention strategies as both interventions and outcomes offered a broader understanding of their effectiveness. This dual role reflects the scoping review’s objective to synthesise evidence on their effectiveness.
Fig. 1.
Inclusion and exclusion criteria of the study selection process
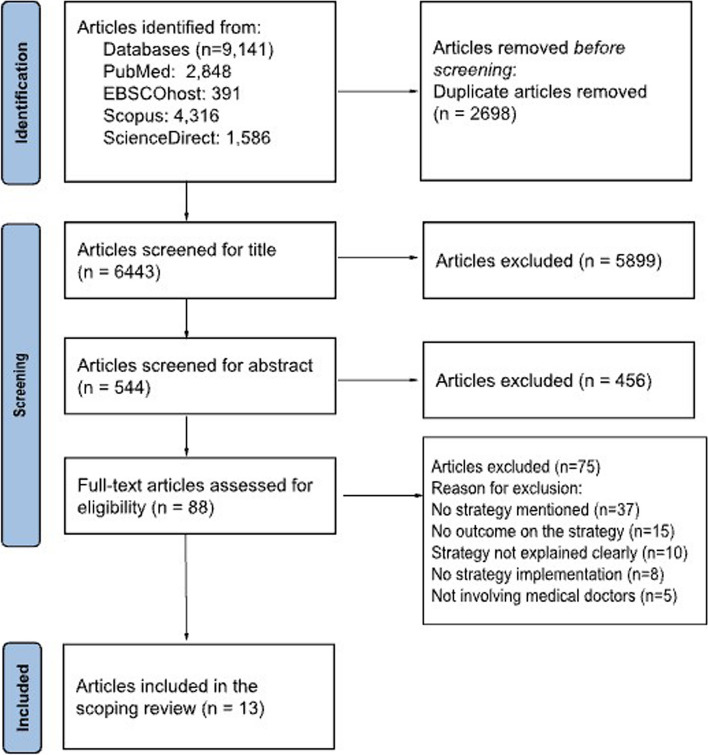
The selection process followed the PRISMA-ScR guidelines [21] and was carried out in three phases: title screening, abstract screening, and full-text evaluation. Two pairs of authors (NJ and IAS; PB and IKA) independently screened of titles and abstracts to exclude studies that did not meet the inclusion criteria. Both pairs then evaluated the full texts of potentially relevant articles, focusing on study characteristics, populations, retention strategies, and outcomes. KYL acted as a third reviewer to resolve disagreements if consensus could not be reached within the pairs. This collaborative and structured approach aimed to minimise selection bias and ensure a transparent and rigorous selection process. The selection process is shown in Fig. 2 via PRISMA flow diagram [25].
Fig. 2.
PRISMA flow diagram
Stage 4: Charting the data
During the data charting phase, relevant information was extracted from the included studies, following a process similar to a systematic review [18]. The extracted information from the full-text articles was systematically organised into a data extraction table in Microsoft Excel to provide a comprehensive overview of the findings based on the objectives of this review. The data extracted encompassed various aspects, including authorship, publication year, country, study design, study population, and location. Additionally, data regarding retention strategies and outcome measures were collected. Factors that influenced the outcomes of the retention strategies were also identified. Four authors independently conducted this process for each included article, and any discrepancies were resolved through in-depth discussions until consensus was achieved.
Stage 5: Collating, summarising, and reporting the results
In the final stage, thematic analysis was performed for all the retention strategies using a dual approach that integrated inductive analysis with the WHO 2010 Global Policy Recommendations [26] on increasing access to health workers in remote and rural areas through improved retention. The four categories in the report included education, regulatory, financial incentives, as well as professional and personal support. Firstly, a narrative synthesis was conducted whereby each retention strategy was qualitatively assessed to understand the context and impact of each strategy. The effectiveness of each strategy was evaluated based on outcome measures reported in the study. The diverse factors associated with each retention strategy were synthesised to comprehend what influenced its success. Thus, this review provided a comprehensive overview of the effectiveness of retention strategies in LMICs through descriptive analysis.
Results
A total of 9,141 articles published between January 1st, 2013 to February 28th, 2023 were retrieved in the initial search. After removing duplicates, there were 6,443 articles left. Following that, another 6,355 papers were excluded after title and abstract screening, leaving 88 articles for full-text evaluation. Another 75 articles were further excluded due to various reasons, leading to 13 articles for final analysis [27–39]. The main reasons for exclusion were the absence of any implemented strategy and the lack of outcome measures linked to those strategies. Figure 2 displays the results of the article selection process based on the PRISMA 2020 flow diagram.
From the 13 included studies, 12 (92%) were single-country studies: one from a low-income country (Malawi), six from lower middle-income countries (India, Nepal, Zambia, Philippines, Iran, Ghana, and Tanzania), and five from upper-middle-income countries (four from Thailand and one from Guyana). In addition, there was a study that featured multinational research that featured seven countries from the African continent (Ethiopia, Malawi, Uganda, Kenya, Rwanda, Zambia, and Zimbabwe). The number of publications peaked in 2017 (n = 4, 31%) and 2023 (n = 3). Most studies employed quantitative (n = 6, 46%), mixed methods (n = 4, 30%), qualitative (n = 1, 8%), case study (n = 1, 8%), and descriptive analysis (n = 1, 8%). The summary characteristics of the included studies with retention strategies targeting medical doctors in LMICs are shown in Table 1.
Table 1.
Characteristics of included studies relating to retention strategies for doctors in LMICs
| Study | Country | Study Design | Study Participants | Retention Strategy | Strategy Category |
|---|---|---|---|---|---|
| Low-income Countries | |||||
|
Addressing Malawi's surgical workforce crisis: A sustainable paradigm for training and collaboration in Africa Qureshi et al. (2013) [28] |
Malawi | Descriptive analysis | Malawian surgical residents in Kamuzu Central Hospital (KCH) |
KCH Surgery Residency Programme • 2-year basic surgical training accredited by COSECSA started in 2009 and expanded to a full 5-year program in 2011 aimed to train Malawian surgical residents locally • Enrolment of three residents annually • Collaboration with surgeons in other countries such as the United States (US) and Norway to enhance general and orthopaedic surgical capacity and research • Establishment of a web-access surgical library, well-trained operation theatre staff, comprehensive equipment and facilities |
Education |
| Lower Middle-income Countries | |||||
|
Strategies for Attraction and Retention of Health Workers in Remote and Difficult-to-Access Areas of Chhattisgarh, India: Do they work? Lisam et al. (2015) [37] |
India | Mixed methods (Document review and interviews) | 57 healthcare workers including specialists, medical officers (MOs), staff nurses, rural medical assistants, programme managers, and government officials from 20 health facilities |
Chhattisgarh Rural Medical Corps (CRMC) Scheme • Launched in 2009 by the Department of Health and Family Welfare, Chhattisgarh, and the National Rural Health Mission to attract and retain health workers including doctors in underserved, remote, and difficult-to-access areas • Monthly financial incentives were provided to HCPs according to the location of the health facilities in three zones with a minimum service period of four years • Eligible MOs with at least two years of service gained extra marks during admission to postgraduate courses against reserved seats by the State Government |
Financial incentives |
|
A staff support programme for rural hospitals in Nepal Zimmerman et al. (2016) [35] |
Nepal | Mixed methods (Document review and interview) | Doctors under the Family Practice Programme from 7 rural hospitals |
The Rural Staff Support Programme • Aimed to improve retention and performance of doctors in rural Nepal hospitals • Rural doctors' compulsory-service scholarship started in 2007 in three hospitals; and expanded to another four more in 2011 • Doctors posted at the participating hospital received salaries three times higher than the standard government rate • Doctors who leave early penalised with twice the scholarship amount, ranging from US$20,000 to US$30,000 • Performance-based incentives given to doctors based on continuous evaluation of hospital performance • Personal, professional, and management support for all staff • Other supports provided comfortable living quarters and internet access, in-service training provided for all staff, and capacity development for hospital management committees |
Professional and personal support Education Regulatory Financial incentives |
|
An evaluation of the effectiveness of the Zambian Health Worker Retention Scheme (ZHWRS) for rural areas Gow et al. (2013) [38] |
Zambia | Mixed methods (Document review and survey) | 234 healthcare workers (doctors (n = 94), nurses, midwives, clinical officers, physiotherapists, pharmacists, and laboratory technicians/technologists) and 3 districts (1 urban, 2 rural) |
Zambian Health Workers Retention Scheme (ZHWRS) • ZHWRS implemented in 2003 intended to retain and recruit Zambian doctors in the rural and remote districts later expanded to other health workers in 2007 • Doctors who served in the rural in three years received monthly rural hardship allowances and annual education allowances per child • Renovation funds available for accommodation improvement • Post-contract expiration, eligible for postgraduate study assistance with eligibility for a loan of 90% of the three-year rural hardship allowance • Doctors were subjected to annual performance reviews and training needs assessments for capacity building • Other benefits offered such as hardship allowance, vehicle loans, housing subsidies, and facility incentives |
Financial incentives Professional and personal support |
|
Experiences from the Philippine grassroots: impact of strengthening primary care systems on health worker satisfaction and intention to stay De Mesa et al. (2023) [39] |
Philippines | Quantitative study (Survey) | 153 healthcare workers consisted of family physicians, nurses, midwives, and community health workers from three sites; urban (n = 36), rural (n = 54), and remote (n = 117) |
Philippine Primary Care Studies (PPCS) Programme • Launched in 2016 to enhance primary healthcare systems in the Philippines • Expanded programme to rural and remote areas in 2019, supporting HWCs through enhanced capacity-building, electronic health records (EHR), and performance-based financial incentives |
Professional and personal support Financial incentives |
|
In-Country Training by the Ghana College of Physicians and Surgeons (GCPS): An Initiative that has Aided Surgeon Retention and Distribution in Ghana Gyedu et al. (2019) [29] |
Ghana | Mixed methods (Survey and interviews) | 117 (80%) of the 146 surgeons in Ghana who were trained through the GCPS |
Ghana College of Physicians and Surgeons (GCPS) Training • Established in 2003 to facilitate the training and credentialing of specialists including surgeons within Ghana • Surgeons being trained at one of the two main training sites • GCPS offered advanced training for subspecialties in surgery |
Education |
|
Retention of medical doctors at the district level: a qualitative study of experiences from Tanzania Sirili et al. (2018) [36] |
Tanzania | Qualitative study (Document review, interview, focus group discussion) | 15 members of the District Health Management teams and MOs working at the 3 district hospitals |
Partial-Centralised Health Sector Administration System • Introduced in 2006 to ensure equitable distribution of doctors in the country focused on deployment and retention in areas with critical shortage • Enabled private practices in district hospitals to boost doctors' income and retention incentives • Career development plans established by the health managers • Introduced a minimum financial incentive package • Implementation of strategies varied in different districts and health managers |
Financial incentives Professional and personal support |
| Mixed Low-income Countries & Lower Middle-income Countries | |||||
|
The Brain Drain Myth: Retention of Specialist Surgical Graduates in East, Central, and Southern Africa, 1974–2013 Hutch et al. (2017) [27] |
Ethiopia, Kenya, Malawi, Rwanda, Tanzania, Uganda, Zambia, Zimbabwe | Quantitative study (Retrospective cohort) | 1,038 surgical graduates from eight African countries |
East, Central, and Southern Africa (ECSA) Postgraduate Surgical Training Programmes • Aimed to train and retain surgeons in ESCA region • Surgical training provided by 24 universities for the Master of Medicine (MMed) programme in surgery and College of Surgeons of East, Central and Southern Africa (COSECSA) for 5-year Surgical Residency Program to Fellowship |
Education |
| Upper Middle-income Countries | |||||
|
Retention of doctors in rural health services in Thailand: impact of a national collaborative approach Arora et al. (2017) [32] |
Thailand | Quantitative study (Retrospective analysis) | 19,338 medical graduates worked in Ministry of Public Health (MOPH) hospitals between 2001 and 2015 |
Collaborative Project to Increase Production of Rural Doctors (CPIRD) and the One District One Doctor (ODOD) Programme • Implemented since 1994, two government initiatives, CPIRD and ODOD, aimed to increase doctors in rural and remote areas • Collaboration between the Ministry of Education, 14 universities, and 37 MOPH hospitals • Strategies include recruiting rural-background students, using existing health services for training, and early rural exposure, followed by regulated placements • CPIRD recruited students from mixed rural–urban provinces • Recruitment of ODOD extended to more remote areas with full scholarships for a 6-year medical program • Regulations on job placement, mandatory service duration, and non-adherence penalties • Mandatory service for CPIRD graduates was to serve three years with a US$11,300 penalty for non-compliance, while ODOD graduates serve 12 years in rural home districts with a US$56,000 penalty for non-compliance |
Education Regulatory |
|
Community-based learning enhances doctor retention Boonluksiri et al. (2018) [33] |
Thailand | Quantitative study (Cohort study) | 10,018 doctors who graduated between 2001–2010 |
Community-Based Learning (CBL) for CPRID track students • Students with a rural background under the CPIRD track were provided with CBL which was an integrated learning in academic courses with community engagement and attachment by rural exposure • CPIRD students followed the standard campus-based preclinical curriculum then rural hospital rotations • Normal-track medical students have mainly done their clinical rotations in urban settings |
Education Regulatory |
|
Rural retention of doctors graduating from the rural medical education project to increase rural doctors in Thailand: a cohort study Pagaiya, Kongkam and Sriratana (2015) [30] |
Thailand | Quantitative (Cohort study) | 7,157 doctors who entered the Ministry of Public Health (MOPH) after graduation between 2000 and 2007 |
Collaborative Project to Increase Rural Doctors (CPIRD) • Aimed to attract and retain doctors in rural areas via collaborative training with MOPH and return-to-home province service • Medical students with rural backgrounds were trained for 6 years near their hometowns [3 years pre-clinical, 3 years in hospitals] • CPIRD doctors posted back to their home provinces; normal track graduates chose the remaining available positions • All graduates were required to work for three years in MOPH rural hospitals after graduation, with a US$12,500 fine for contract breach |
Education Regulatory |
|
Rural retention of new medical graduates from the Collaborative Project to Increase Production of Rural Doctors (CPIRD): a 12-year retrospective study Techakehakij and Arora (2017) [31] |
Thailand | Quantitative (Retrospective study) | New medical graduates who entered MOPH hospitals (Thailand) from January 2003 to October 2014 |
Collaborative Project to Increase Rural Doctors (CPIRD) • Aimed to increase rural doctors’ numbers through special recruitment • Students must reside or be educated in specified rural areas • Pre-clinical training matched normal track students; clinical years in university-affiliated schools near hometowns • Offered four tracks: regular CPIRD program (Regular CPIRD), one-district-one-doctor program (ODOD), regular post-graduate program (Grad), post-graduate program for civil servants (Grad CS) • Graduates from public medical schools had post-graduation contracts for public hospital work • Most graduates, except ODOD, were required to serve three years in MOPH hospitals; non-compliance means a US$11,500 fine • 12 years of compulsory service for ODOD doctors in rural areas; a breach will incur a US$57,300 fine |
Education Regulatory |
|
An examination of Eyal & Hurst's (2008) framework for promoting retention in resource-poor settings through locally relevant training: A case study for the University of Guyana Surgical Training Program Prashad et al. (2017) [34] |
Guyana | Case study (Document review and interviews) | Graduates, trainees, faculty members, and policymakers associated with the UGDS programme in Guyana |
University of Guyana Diploma in Surgery (UGDS) • 2.5-year postgraduate surgery programme by the Canadian Association of General Surgeons and the University of Guyana to train and retain surgical graduates • The training included clinical rotations, structured tutorial modules, written and oral exams, and a six-month rural hospital placement • Trainees were provided with housing benefits, and graduates of the programme have a required return-of-service to the Ministry of Health for four years |
Education |
Retention strategies for doctors in LMICs vary but often revolve around similar scope and context, especially in areas with limited healthcare access. These strategies, categorised by the World Health Organization [26], include education, regulation, financial incentives, as well as professional and personal support. Generally, most of the studies in this review reported that the countries adopted a blended approach of strategies in their efforts to attain favourable outcomes. Educational strategies have emerged as a significant focus of research, with nine studies concentrating on this area [27–35]. Three studies from African countries outlined strategies aimed at developing and preserving a highly skilled and dedicated medical workforce via training programs through collaborations with diverse academic professionals to retain skilled HCPs, especially surgeons [27, 28, 34]. Additionally, membership and fellowship training for various specialties and subspecialties [29] were offered as postgraduate education opportunities.
Five studies concentrated on educational initiatives for rural doctors [30–33, 35]. In Thailand, scholarships incentivised rural students to return post-graduation, while in Nepal, compulsory-service scholarships were linked to secured training spots in family practice programmes [35]. These educational strategies were often supported by regulatory frameworks overseeing job placement, mandatory service duration, and penalties for non-compliance to enhance retention and ensure service provision [30–32, 35]. In addition, despite being nations with economic constraints and limited resources, financial strategies were also opted by several LMICs to attract and retain HCPs in remote, difficult-to-access, and critically underserved areas. India and Tanzania offered monthly incentives [36, 37], Zambia provided rural hardship allowances [38], and the Philippines gave out performance-based incentives [39]. In addition to financial incentives, Nepal offered three times higher salaries for rural doctors [35]. Indirect monetary compensation, like an annual education allowance for staff’s children, was one of the innovative strategies observed in Zambia [38].
Four studies outlined professional and personal support mechanisms to enhance the well-being of doctors and their families, especially in rural areas. These strategies included the provision of conducive living quarters, renovation funds, housing subsidies, and vehicle loans [35, 38]. Additional professional support such as capacity-building initiatives and electronic health record development were also strategies aimed at improving the job satisfaction of doctors to indirectly boost their intentions to work in the rural setting [39]. Apart from that, allowing private practice further enhanced job satisfaction and encouraged doctors to remain in rural district hospitals in Tanzania [36].
Among the 13 included studies, more than two-thirds (n = 10) reported a successful outcome with the strategies employed [27–35, 37], as compared to two studies with unsuccessful outcomes [36, 38] and one with mixed outcomes [39]. It should be noted that the four studies [30–33] from Thailand were all based on the evaluation of the same programme, i.e. Collaborative Project to Increase Production of Rural Doctors (CPIRD) at different time points. In addition, two studies were based on the same programme (COSECSA) but the evaluation was centred in different regions, i.e. in East, Central, and Southern Africa [27] as well as Malawi [28]. The summary of the overall outcomes reported in each study according to the four categories of retention strategies is shown in Table 2.
Table 2.
Overall outcomes based on the categories of retention strategies
| Authors (Year) |
Categories of Retention Strategies | Overall Outcome |
|||
|---|---|---|---|---|---|
| Education | Financial incentives | Regulatory | Professional and personal support | ||
| Arora et al. (2017) [32] | X | X | Successful | ||
| Boonluksiri et al. (2018) [33] | X | X | Successful | ||
| De Mesa et al. (2023) [39] | X | X | Mixed Outcome | ||
| Gow et al. (2013) [38] | X | X | Not Successful | ||
| Gyedu et al. (2019) [29] | X | Successful | |||
| Hutch et al. (2017) [27] | X | Successful | |||
| Lisam et al. (2015) [37] | X | Successful | |||
| Pagaiya, Kongkam and Sriratana (2015) [30] | X | X | Successful | ||
| Prashad et al. (2017) [34] | X | Successful | |||
| Qureshi et al. (2013) [28] | X | Successful | |||
| Sirili et al. (2018) [36] | X | X | Not Successful | ||
| Techakehakij and Arora (2017) [31] | X | X | Successful | ||
| Zimmerman et al. (2016) [35] | X | X | X | X | Successful |
Further observation revealed that all five single-strategy approaches tended to report success, especially those focusing on education (n = 4) or financial incentives (n = 1) [27–29, 34, 37]. In comparison, studies with combined strategies showed various outcomes; five had successful outcomes [30–33, 35], one demonstrated mixed outcomes [39], and two showed unsuccessful outcomes [36, 38] in retaining doctors.
Table 3 outlines the detailed description of outcome measures and the factors influencing the overall outcomes in the included studies. Among the included studies in this review, the retention strategies were evaluated using direct or indirect outcomes. Direct measures included immediate and measurable effects such as retention rates of the doctors following the strategies [27, 29–34]. Other studies reported higher rates of intention to stay [39], recruitment [38], or lower vacancy rates [36, 37] to indicate the success of the approaches. On the other hand, some studies used proxy indicators in the form of indirect and secondary effects to reflect positive outcomes of retention strategies, such as better job satisfaction [38, 39], a higher number of routine and complex operations performed [28, 29], as well as increased hospitalisation and outpatient visits [35]. Notably, three studies reported both direct and indirect outcomes [29, 30, 34], hence providing a more in-depth understanding of the interconnectedness between retention strategies with broader health system goals and community well-being.
Table 3.
Overview of Study Outcomes Relating to Retention Strategies of Doctors in LMICs
| Authors (Year) | Category of strategies | Outcome measured | The main description of outcomes | Factors influencing the outcomes |
|---|---|---|---|---|
| Arora et al. (2017) [32] |
Education Regulatory |
Retention rate Number of doctors Provincial assignment compliance |
• The overall and year-by-year retention of medical graduates under the special recruitment track (CPIRD) was higher than the normal track (overall retention of 78.2% and 52.5% respectively, p < 0.05) between 2001–2016 • Increased production of doctors for rural areas, with a significant rise in graduates from the special recruitment track from eight in 2001 to 883 in 2015 • Among 4,869 medical graduates under the special recruitment track remaining in the MOPH, 90.9% (n = 4425) worked in their primarily assigned provinces |
Not mentioned |
| Boonluksiri et al. (2023) [33] |
Education Regulatory |
Retention rate CBL contact time |
• 5,774 of 10,018 doctors (57.6%) were retained. CPIRD retained at a higher rate (1,514 of 2,098 doctors; 72.1%) than normal track (4,260 of 7,919 doctors; 53.8%; p < 0.001) • Graduate entry CPIRD were retained at a higher rate than normal track; 108 of 128 doctors (84.4%) and 1406 of 1971 doctors (71.3%), respectively (p = 0.001) • More CPIRD doctors worked in rural areas than normal track doctors (62.3% and 49.0%, p < 0.001) • Higher contact time of CBL in the retention group than in the resignation group (305.9 h (2.97%) versus 312.5 h (2.90%), respectively, P = 0.046) |
CBL programmes differed based on the affiliated university, staff preparedness, learning quality, community appeal, engagement level, rural setting, and contact time of rural exposure |
| De Mesa et al. (2023) [39] |
Financial incentives Professional and personal support |
Intention to stay Job satisfaction |
• Urban areas: No change in the intent to stay, with 74% of HCPs intending to stay both at baseline and the end of the study (p-value = 1.000) • Rural areas: Increased in the intent to stay from 75% at baseline to 89%, although this change was not statistically significant (p-value = 0.090) • Remote areas: Significant decrease in the intent to stay from 93% at baseline to 76% (p-value < 0.001) • Baseline: Urban HCPs showed lower work enjoyment (63%) and morale (72%) than those in rural and remote areas, with widespread feelings of under-compensation, especially in remote areas concerning equipment access • Final improvements: Increased satisfaction with compensation fairness at urban (p = 0.001) and rural sites (p = 0.016), and access to medicines in rural areas (p = 0.012), were significant, moving median satisfaction scores from neutral to satisfied • Differences in satisfaction: Urban and rural HCPs maintained satisfaction levels, while remote HCPs experienced significant drops in morale and overall satisfaction (p < 0.001) |
Facilitators: Fair remuneration for HCPs in both urban and rural areas Performance-based incentives, electronic health records adoption, improving diagnostic capabilities and medicine access improved job satisfaction and retention Barriers: Late or irregular salary payments Poor working conditions such as infrastructures and workplace hygiene |
| Gow et al. (2013) [38] |
Financial incentives Professional and personal support |
Recruitment rate Job satisfaction and intentions to quit |
• The ZHWRS did not meet its targets for health worker recruitment • In 2009, the MOH workforce consisted of 627 health workers, representing 3% of the total health workforce, a 24% decrease from 2006, indicating declining attraction and retention capabilities • 40% of health workers have very low or low job satisfaction, contributing to high attrition rates. 48% of the workers showed a desire to quit their current locations, with intentions to join the private sector, migrate outside Zambia, or move to local NGO health facilities |
The "one-size-fits-all" approach overlooked the unique characteristics and requirements of various health cadres Absence of a comprehensive multi-sectoral rural implementation plan Weak human resource management system with health worker distribution biased toward urban areas Lack of non-financial incentives |
| Gyedu et al. (2019) [29] | Education |
Retention rate Health service provision |
• A high retention rate of 87–97% among GCPS-trained surgeons with 44% in the rural and higher-need areas • Surgeons performed 13 weekly operations, with 35% of elective and 77% of emergency operations classified as essential, highlighting the scheme's effectiveness in addressing critical surgical needs • Surgeons in Ghana contributed to medical education and evidence base through their involvement in training (79%) and research (46%) • Surgeons reported improvements in their hospitals, such as expanded surgical services, reduced referrals, enhanced quality of care, and increased patient satisfaction |
Regular engagement in community service, health education, training of other HWCs, advocacy, and collaboration with international organisations |
| Hutch et al. (2017) [27] | Education | Retention rate |
• High retention rates of surgical graduates within their countries of training, 85.1% (883/1038), the ECSA region, 88.3% (917/1038), and Africa, 93.4% (970/1038) • Retention rate by country of graduation within Africa varied from Malawi (100%, 11/11) to Zimbabwe (65.5%, 38/58) • Zambia retained 97.9% (46/47) of graduates in the country, while Ethiopia and Uganda showed lower rates with 77.8% (277/356) and 77.3% (75/97) |
Provision of surgical training via 24 university-affiliated teaching hospitals |
| Lisam et al. (2023) [37] | Financial incentives |
Vacancy rate Financial incentives utilisation |
• In 2010–11, 1,319 health workers joined CRMC, and the vacancy rate reduced from 90 to 45% across facilities, with a further increase to 1,658 in 2011–12 with a 20% increase in the proportion of staff joining CRMC areas • Increase in the budget utilisation for CRMC, from 27% in 2009–10 to 98% in 2011–12 • Doctors expressed that they continued to work in CRMC areas due to financial incentives and extra marks for post-graduate admissions |
Increased budget provisions by the government Delayed and irregular payment of incentives Limited access to training, inadequate supervision, and poor monitoring Inadequate healthcare infrastructures and personal support such as residential accommodation, educational facilities, transportation allowances, and life insurance in CRMC |
| Pagaiya, Kongkam and Sriratana (2015) [30] |
Education Regulatory |
Retention rate Resignation rate Risk of leaving service |
• CPIRD doctors had a higher retention rate in rural areas (29%) compared to non-CPIRD doctors (18%) • Overall median survival time was 4.2 years for CPIRD doctors and 3.4 years for normal track doctors • The survival time decreased for later cohorts, with CPIRD doctors' median survival dropping from 8.0 years (2002 cohort) to 3.9 years (2007 cohort), and normal track doctors from 8.4 years (2000 cohort) to 3.1 years (2007 cohort) • Even though almost half of the doctors (45.9%) left the MOH service during the study period, the rate of leaving was lower among CPRID doctors (33%) than those in the normal track (48%) • The incidence rate of doctors who left the rural areas was lower for CPIRD than for normal track at 14.9% and 18.2% of doctor-years • The rate increased over time, from 2.2% for CPIRD (2001 cohort) to 17.0% (2007 cohort), and from 8.1% for the normal track (2000 cohort) to 28.3% (2007 cohort) • Normal track doctors had a 1.3 times higher risk of leaving rural areas than CPIRD doctors |
Selective admission of students with rural background students Collaborative training with medical schools and the MoH Preferential job placement in their home provinces after graduation |
| Prashad et al. (2017) [34] | Education |
Retention rate Career promotion |
• 11 out of 14 (78.6%) resident graduates practised in Guyana • Mixed experiences from participants about the rural practice environment, with some expressing satisfaction while others expressed frustrations due to overwork and understaffing • Rural training programme improved understanding of challenges in under-resourced areas and made the graduates more inclined to practise there • Participation in the programme led to promotion and senior positions |
Alignment of training with actual country medical practice and training skills relevant to the local community International partnerships with the Canadian Association of General Surgeon Diploma programme were still insufficient for some, resulting in them leaving to pursue higher-level training abroad Inequalities arising from diploma qualification compared to other postgraduate programme Lack of support from important stakeholders |
| Qureshi et al. (2013) [28] | Education |
Staff number Operative case Accreditation and training expansion Integration of surgery residents |
• Increase in physician staff, indicating a bolstered surgical capacity • A marked increase in major operative cases performed from 1,070 in 2007 to 1,573 in 2010, indicating the department's growing capacity and skill level • Accredited programme by COSECSA in 2009 to provide 5 years of basic surgical training to local surgeons, with six more residents joining in 2011 • Surgery residents have replaced the responsibilities traditionally held by Clinical Officers, indicating successful integration and potential for long-term retention |
Integration of local surgical training programme into existing educational and healthcare infrastructure with international collaboration Governmental support from the MOH Career advancement through research, educational resources opportunities and improved hospital facilities Efforts to address and secure funding and resources despite economic challenges |
| Sirili et al. (2018) [36] |
Financial incentives Professional and personal support |
Financial incentive system Working conditions Career development Living environment and social services Implementation challenges Vacancy rate |
• The participants expressed that the non-uniform application of financial incentives across districts may lead to an internal brain drain of doctors seeking better incentives • They highlighted that despite efforts to improve working conditions, under-equipped facilities, and general feeling of being undervalued by the community suggest a need for further improvements to enhance their satisfaction and work environment • The participants mentioned that implemented career development strategies like postgraduate scholarships, but lack of a clear career path in districts discouraged doctors, highlighting the need for a structured approach • The living environment and social services, including housing, education, and recreational facilities, significantly influenced doctors' decisions to stay or leave rural districts, emphasising the need for improved quality of life • Health managers reported that they implemented strategies to retain doctors, including career development plans, financial incentives, and private practices, but faced challenges due to limited resources and rural doctor retention complexity • None of the three districts achieved the recommended minimum number of doctors recommended for their staffing level • District A had a 26.3% shortage (59 out of 80 required doctors). Districts B and C had only 3 out of 8 required doctors, equivalent to a 62.5% shortage |
Unfavourable working conditions, unclear career paths, and a non-uniform financial incentive system across districts Unsupportive community environments like difficulty finding housing, limited income opportunities, lack of community appreciation, and inadequate social services Minimum financial incentives due to financial constraints and competing priorities Weak management capacity across all levels in the country |
| Techakehakij and Arora (2017) [31] |
Education Regulatory |
Retention rate Probability of leaving Resignation rate |
• Rural service retention of normal track doctors was significantly lower than their CPIRD counterparts (p < 0.001) • CPIRD medical graduates were 2.44 times more likely to complete a 3-year rural service compared with their normal track graduates • The 3-year rural retention rate was 286.7% higher in Grad CS doctors compared to Regular CPIRD physicians, while Grad medical graduates showed a 52.9% lower retention rate • CPIRD physicians have a 54.4% lower annual probability of leaving the MoPH hospitals than normal track peers • ODOD and Grad CS physicians were respectively 37.0% and 74.8% less likely to leave rural services each year compared to Regular CPIRD counterparts • Grad doctors had a 63.0% higher annual resignation rate than Regular CPIRD physicians |
Female doctors were more likely to resign from MoPH hospitals Higher resignation rates among physicians from certain regions Compulsory service lengths and penalties for non-compliance differ for different tracks |
| Zimmerman et al. (2016) [35] |
Professional and personal support Education Regulatory Financial incentives |
Recruitment Hospital service delivery |
• Continuous posting of family practice doctors in each of the seven hospitals • Mean annual admissions and outpatient visits per hospital almost doubled, from 832 to 1,592 and 10,585 to 21,341, respectively • Mean deliveries per hospital per year tripled from 152 to 462 • The mean caesarean sections per hospital per year increased from 1.4 to 24.8 |
Compulsory-service scholarships ensure a binding commitment to serve in a rural hospital Performance-based incentives with higher salaries Central personnel management to streamline the recruitment and deployment of hospital staff Personal, professional, and management support to all hospital staff which includes improved living quarters, new hospital equipment, and internet access |
Among the studies implementing retention strategies focusing on a single category, four emphasised educational strategies in African countries [27–29, 34], while another implemented a financial strategy in India [37]. A significant increase in retention rates for surgical graduates [27, 29] and resident graduates [34], as well as decreased vacancy rates [37] were reported. In Thailand, the CPIRD project that incorporated education and regulatory approaches led to higher retention rates of CPIRD graduates compared to the standard track. Additionally, the number of doctors working in rural areas significantly increased by 29%, in sync with a reduction in the resignation rate by 15%.
In Nepal, the consistent placement of family practice doctors gave rise to a two-fold increase in mean annual hospital admissions and outpatient visits, along with a tripling of mean annual deliveries, indicating the effectiveness of the strategies employed [35]. Additionally, compulsory services enforcement in Thailand and Nepal, as described in three studies [30, 31, 35], has proven to be a significant factor in retaining doctors in underserved areas. On the other hand, a study in the Philippines [39] that employed a combination of financial with professional and personal support strategies reported mixed outcomes. Similar combination strategies in Zambia and Tanzania also did not produce successful outcomes [36, 38], prompting a reconsideration of the combination of strategies utilised.
Each of these studies reported different types of barriers but financial insufficiency and infrastructure limitations emerged as major hindrances to the sustainability and success of the strategies. Uneven allocation of financial incentives, under-resourced facilities, ambiguous career progression pathways [36], lack of non-financial rewards [38], and diminished job satisfaction stemming from perceptions of being under-compensated, especially in remote areas [39] were some of the common barriers reported. In contrast, adept human resource management in ensuring an adequate number of doctors in the service and strategic distribution of doctors was the most cited facilitator to a successful strategy, as observed in three studies [29, 30, 35] in Ghana, Thailand, and Nepal respectively.
Discussion
This scoping review provides a comprehensive overview of retention strategies implemented in LMICs in response to the obstacles encountered in retaining doctors. This extensive analysis of various studies highlighted three key outputs: the retention strategies used to retain medical doctors in LMICs, the outcomes of the retention strategies, and the factors influencing these outcomes. Besides, distinct regional and country-specific challenges and variations of customised strategies were analysed. We included 13 studies published between 2013 and 2023 from 14 LMICs. A variety of retention strategies were applied, which can be broadly categorised as educational, regulatory, financial, as well as professional and personal support based on the WHO report [26].
Among these, educational strategies were the most practised retention approach. Addressing doctors' educational needs enhances motivation and contributes to their retention [40]. Such strategies not only address the immediate need for skilled personnel but also ensure the alignment of healthcare practices with contemporary medical standards [41]. Educational strategies are often the focus of interventions for health workforce retention from high-income countries (HICs). For example, in Norway, the retention of primary doctors in rural regions rose to 65% after postgraduate medical training [42]. In this review, the four studies from the African region [27–29, 34], focused on the development and retention of surgeons via collaborative efforts with academic professionals from HICs such as Canada [34], the United States (US), and Norway [28]. HICs generally have more resources to invest in comprehensive educational programmes, including sophisticated simulation training and continuing medical education [43]. Strong international collaboration in resource and knowledge sharing between countries served as the cornerstone of most tailored training programmes aimed at strengthening the ongoing professional development of doctors and ultimately, retaining them in LMICs. The educational approach was associated with successful outcomes in nine studies in this review. Therefore, in line with our review findings, the educational approach presented the highest potential for replication and adaptation in resource-limited contexts in view of its flexibility and proven effectiveness.
Furthermore, these educational strategies were frequently employed in conjunction with other categories. In the Thailand CPIRD programme, the educational strategy was linked to the regulatory strategy in the form of compulsory service post-training. Rural doctors were guaranteed priority access to training opportunities in exchange for subsequent service obligations. Successful outcomes of such a combined approach in mitigating healthcare disparities in underserved areas, regardless of HICs or LMICs, have been reported in Indonesia [44], Australia and Canada [45], and Canada [46]. In the context of CBL in the CPRID programme [33], the effort aligned with Khalil and Alameddine's [12] study which found that community-based training has also been shown to yield higher recruitment and retention of HCPs in rural and remote regions within the Eastern Mediterranean Region.
Financial incentives represent another instrumental retention strategy in attracting and retaining doctors in underserved or remote areas [47, 48]. Willis-Shattuck et al. [13] emphasised the significance of financial incentives such as hardship allowances, regular salary raises, and bonuses based on performance in motivating HCPs. Multiple studies in the literature reported positive outcomes from the financial incentives in HICs. In Israel, about half of all doctors in peripheral hospitals reported that the incentives contributed to their choice of residency location [49]. A study in Australia found that a financial incentive in the form of a locum relief scheme had the most impact on improving rural doctor retention [50]. Meanwhile, a study in the US found that financial incentives also improved healthcare for underserved groups, with the reason being postulated as improved productivity after physicians received variable compensation [51]. All this evidence from HICs highlighted the effectiveness of financial incentives in retaining doctors and addressing healthcare disparities. Nevertheless, the lack of a national budget allocation for long-term human resource planning, reliance on outside funding, and fierce competition from the private sector or foreign recruiting agencies were frequent obstacles faced by LMICs to retain medical doctors [52]. This is echoed by our review findings, whereby Sirili et al. [36], Gow et al. [38], and De Mesa et al. [39] all showed that financial incentives failed to positively impact the retention of doctors working in remote areas in the long-term due to inconsistencies in incentive systems. Hence, it is imperative for LMICs to secure key sources of sustainable financing mechanisms to safeguard health workforce planning and management.
Likewise, strategies that encompassed both professional and personal assistance required some levels of budgetary provision from the governments. Various professional and personal supports, such as conducive living conditions, internet access, renovation funds, and flexible working hours can create an environment where doctors feel valued and supported. It is crucial not to ignore or disregard these incentives, despite their complexities, as they play a role in creating a healthy work environment, indirectly motivating doctors to continue working in challenging areas [53, 54]. This reality called for innovative solutions to navigate budgetary limitations, one of which was integrating financial incentives with other interventions [55], especially regulatory strategies, for example, by exerting compulsory service among the recipients to maximise return on investment.
Apart from that, alternative retention strategies have also been tested in certain countries. Non-financial acknowledgment, such as public recognition for HCPs' contributions, was an additional morale booster [56, 57]. Community engagement, often overlooked, could also be a cost-effective initiative. Programmes integrating doctors into local communities fostered a sense of belonging and contributed to retention [58]. Considering regional differences in LMICs, it is crucial to decentralise healthcare-related decision-making to HCPs at the 'ground zero' to better align with the unique needs of each community [59, 60]. Furthermore, investments in well-equipped healthcare infrastructure, often seen as benefiting marginalised populations in remote areas, could also be a driving force to retain doctors as they could access the latest medication and technology in medical treatment.
Given the findings that emerged from this review, it is clear that no one-size-fits-all approach is available as a solution to the brain drain issue in LMICs. In view of that, it is imperative to conduct regular workforce surveys and evaluations of implemented retention strategies based on real-world outcomes to assess their effectiveness and sustainability among the target groups. In this review, one of the main barriers reported was the lack of comprehensive programme evaluation, particularly in terms of the long-term impacts of retention strategies with direct outcome measures such as retention rates and attrition rates, hence hindering the assessment of its overall effectiveness. A similar barrier was highlighted in a recent review that focused on interventions to improve the retention of health workers in rural and underserved areas of HICs [48]. The evidence gaps in terms of the effectiveness of the various interventions in improving the attraction and retention of HCPs underscores the need for further research, especially in LMICs where the challenges of healthcare workforce retention are most acute.
To date, most studies on retention strategies for HCPs were conducted in HICs. Comparatively, there is a scarcity of reviews on similar topics among HCPs, especially doctors in LMICs. Furthermore, most of the published studies were descriptive in nature and did not perform any formal evaluation of the retention initiatives [12, 22, 61, 62]. Apart from gathering relevant retention strategies for doctors in LMICs, our review also included an in-depth analysis that focused on the evaluation of the strategies. As the global community continues to grapple with healthcare disparities, the lessons learned from LMICs can inform a more nuanced understanding of retention dynamics, offering pathways to sustainable health workforce development and, ultimately, improved health outcomes for underserved populations.
The review highlighted the need for tailored approaches to retention, given the diverse challenges across LMICs. It also emphasised the importance of evaluating retention strategies through measurable outcomes, such as retention rates and long-term impacts, to ensure sustainability and scalability.
Practical implications and future research
This review offers a comprehensive understanding of the practical implications of various retention strategies on the recipients, institutions, and the wider healthcare system. These findings form a critical foundation for targeted policy interventions and refined strategies to address healthcare workforce maldistribution and shortages in LMICs. Policymakers and healthcare administrators can utilise the findings to implement tailored retention strategies that address specific workforce challenges. Educational interventions, such as postgraduate training and international collaborations, offer scalable solutions to improve professional development and align healthcare practices with global standards. When combined with regulatory approaches, such as compulsory service agreements, these strategies can promote the equitable distribution of healthcare professionals in underserved regions. Health facilities must adopt a multi-faceted, context-specific approach to retention, integrating these strategies to address both immediate needs and long-term workforce challenges. Such efforts are essential for reducing brain drain, improving healthcare equity, and enhancing service delivery in LMICs.
This review also highlights significant gaps in the current evidence base for retention strategies targeting medical doctors in LMICs, emphasising the need for further research in several areas. Comprehensive evaluations are required to assess the long-term effectiveness and sustainability of these strategies with robust indicators, particularly through measurable outcomes such as retention rates, attrition rates, and healthcare delivery improvements. Furthermore, future research should also explore innovative and non-financial incentives, such as community engagement and public recognition, as these may serve as cost-effective alternatives, especially in resource-constrained settings. Lastly, the sustainability of retention strategies demands greater focus, with research focusing on their ability to withstand to external pressures, including economic instability and global health crises. Addressing these gaps will provide a stronger evidence base to inform future interventions and strengthen health systems in LMICs.
Limitations
We acknowledged several limitations to this review that may influence the interpretation and applicability of the findings. Firstly, some of the studies encompassed a broader spectrum of HCPs beyond medical doctors, thus possibly affecting the generalisability of the results as the diversity in study populations could potentially dilute the direct applicability of the results to the retention of doctors specifically. Additionally, a few of the studies also did not measure retention directly but rather reported proxy indicators of retention, such as willingness to stay or quantitative measures of healthcare delivery by increased service provision in terms of patients seen or operations conducted. While these proxy indicators may not fully capture the complexity of retention issues, they were considered acceptable and useful approximation alternatives to represent retention strategies' outcomes.
Secondly, the decision to limit our review to English-language publications may narrow the scope of our review by potentially excluding relevant non-English studies in linguistically diverse LMICs. However, the decision to prioritise English was taken to minimise language-related biases in the review process in view of limited translation resources. Even though certain grey literature such as policy documents and theses may contain valuable information not presented in peer-reviewed sources, the decision to exclude grey literature was made because of the challenges of limited accessibility, inconsistent indexing, and difficulties in assessing the quality and reliability of information. Another limitation was the varying methodological rigour such as document review and case study, among the included studies which may potentially affect the overall reliability of the findings. Lastly, the broad approach of this review, while designed to capture a wide array of retention strategies across LMICs for a comprehensive overview, may have resulted in less in-depth analysis compared to focused systematic reviews. Despite these limitations, we were able to generate a holistic understanding of the subject by summarising the diversity of strategies and findings in the field of doctor retention in LMICs. More importantly, future research can strive to generate more nuanced studies based on the preliminary findings presented in this review.
Conclusions
Addressing the specific needs and challenges of the medical workforce is crucial for building a resilient healthcare workforce in LMICs. In the face of brain drain, many LMICs are stepping up the efforts to retain their HCPs, especially medical doctors. While strategies like financial incentives, professional development opportunities, as well as improved working conditions have been promising in improving retention rates, their long-term success remains uncertain due to varying contextual factors and resource limitations. Given the lack of a one-size-fits-all solution, our review highlights the importance of retention strategies that are meticulously tailored to the distinct needs of LMICs. Long-term monitoring and evaluation must be incorporated to ensure sustainability and adaptability over time of the strategies. International collaborations between LMICs and HICs, coupled with innovative solutions, can play a transformative role in overcoming resource constraints and strengthening healthcare systems. By addressing these challenges, LMICs can move closer to achieving equitable healthcare access, improving health outcomes for underserved populations, and contributing to the global goals of health equity and sustainable development under the SDGs.
Supplementary Information
Acknowledgements
The authors extend their gratitude to the Director General of Health Malaysia for granting permission to publish this paper. Additionally, we would like to express our appreciation to the Sector for Evidence-Based in Healthcare, National Institutes of Health, Malaysia for their guidance throughout the review process.
Abbreviations
- CBL
Community-Based Learning
- COSECSA
College of Surgeons of East, Central and Southern Africa
- CPIRD
Collaborative Project to Increase Production of Rural Doctors
- CRMC
Chhattisgarh Rural Medical Corps
- ECSA
East, Central, and Southern Africa
- EHR
Electronic health records
- GCPS
Ghana College of Physicians and Surgeons
- HCPs
Healthcare professionals
- HICs
High-income countries
- KCH
Kamuzu Central Hospital
- LMICs
Low- and middle-income countries
- MOs
Medical officers
- MOH
Ministry of Health
- MOPH
Ministry of Public Health
- ODOD
One District One Doctor
- PPCS
Philippine Primary Care Studies
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Extension for Scoping Reviews
- SDGs
Sustainable Development Goals
- UGDS
University of Guyana Diploma in Surgery
- US
United States
- WHO
World Health Organisation
- ZHWRS
Zambian Health Workers Retention Scheme
Authors’ contributions
All five authors contributed to the conceptualisation of the study. NJ, IAS, PB, and IKA undertook responsibilities for screening and data extraction. All authors were involved in data analysis and drafting of the manuscript. KYL provided critical review for intellectual content and finalised the paper. All authors have reviewed and approved the final manuscript.
Funding
The authors received no specific funding for this work.
Data availability
The data sets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Duckett S. The Australian health workforce:facts and futures. Aust Health Rev. 2000;23(4):60. [DOI] [PubMed] [Google Scholar]
- 2.Atte F. The moral challenges of health care providers brain drain phenomenon. Clin Ethics. 2021;16(2):67–73. [Google Scholar]
- 3.Oberoi SS, Lin V. Brain drain of doctors from southern Africa: brain gain for Australia. Aust Health Rev. 2006;30(1):25. [PubMed] [Google Scholar]
- 4.Tahir MW, Kauser R, Tahir MA. Brain Drain of Doctors; Causes and Consequences in Pakistan. 2011;5(3).
- 5.Shumba A, Mawere D. The Causes and Impact of the Brain Drain in Institutions of Higher Learning in Zimbabwe. Int Migr. 2012;50(4):107–23. [Google Scholar]
- 6.Bazoukis X, Kalampokis N, Papoudou-Bai A, Bazoukis G, Grivas N. The increasing incidence of immigration and information-seeking behaviour of medical doctors in north-western Greece. Rural Remote Health [Internet]. 2020 Mar 23 [cited 2024 Apr 23]; Available from: https://www.rrh.org.au/journal/article/4877 [DOI] [PubMed]
- 7.Adjei-Mensah S. Factors Influencing Brain Drain Among Health Workers in Ghana. Eur J Hum Resour. 2023;7(1):17–30. [Google Scholar]
- 8.Balouch MS, Balouch MM, Balouch MS, Qayyum W, Zeb Z. Career Aspirations Of Junior Doctors In Pakistan: Exploring Reasons Behind The Brain Drain. J Ayub Med Coll Abbottabad. 2022;34(3):500–6. [DOI] [PubMed] [Google Scholar]
- 9.Hooper CR. Adding insult to injury: the healthcare brain drain. J Med Ethics. 2008;34(9):684–7. [DOI] [PubMed] [Google Scholar]
- 10.Najib MNM, Abdullah S, Narresh S, Juni MH. Brain-Drain Phenomenon Among Healthcare Workers. Int J Public Health Clin Sci [Internet]. 2019 Jun 1 [cited 2024 Apr 23];6(3). Available from: http://publichealthmy.org/ejournal/ojs2/index.php/ijphcs/article/view/1015/630
- 11.Akinwale OE, George OJ. Personnel brain-drain syndrome and quality healthcare delivery among public healthcare workforce in Nigeria. Arab Gulf J Sci Res. 2023;41(1):18–39. [Google Scholar]
- 12.Khalil M, Alameddine M. Recruitment and retention strategies, policies, and their barriers: A narrative review in the Eastern Mediterranean Region. Health Sci Rep. 2020;3(4): e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Willis-Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res. 2008;8(1):247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miranda JJ, Barrientos-Gutiérrez T, Corvalan C, Hyder AA, Lazo-Porras M, Oni T, et al. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med. 2019;25(11):1667–79. [DOI] [PubMed] [Google Scholar]
- 15.Adebayo A, Akinyemi OO. “What Are You Really Doing in This Country?”: Emigration Intentions of Nigerian Doctors and Their Policy Implications for Human Resource for Health Management. J Int Migr Integr. 2022;23(3):1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imran N, Azeem Z, Haider II, Amjad N, Bhatti MR. Brain Drain: Post Graduation Migration Intentions and the influencing factors among Medical Graduates from Lahore, Pakistan. BMC Res Notes. 2011;4(1):417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jinah N, Abdullah Sharin I, Bakit P, Adnan IK, Lee KY. Overview of Retention Strategies for Medical Doctors in Low- and Middle-Income Countries and Their Effectiveness: Protocol for a Scoping Review. JMIR Res Protoc. 2024;8(13): e52938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 19.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26. [DOI] [PubMed] [Google Scholar]
- 20.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 22.Noya F, Carr S, Freeman K, Thompson S, Clifford R, Playford D. Strategies to Facilitate Improved Recruitment, Development, and Retention of the Rural and Remote Medical Workforce: A Scoping Review. Int J Health Policy Manag. 2021;15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holloway P, Bain-Donohue S, Moore M. Why do doctors work in rural areas in high-income countries? A qualitative systematic review of recruitment and retention. Aust J Rural Health. 2020;28(6):543–54. [DOI] [PubMed] [Google Scholar]
- 24.Verma P, Ford JA, Stuart A, Howe A, Everington S, Steel N. A systematic review of strategies to recruit and retain primary care doctors. BMC Health Serv Res. 2016;16(1):126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. 2010;71. [PubMed]
- 27.Hutch A, Bekele A, O’Flynn E, Ndonga A, Tierney S, Fualal J, et al. The Brain Drain Myth: Retention of Specialist Surgical Graduates in East, Central and Southern Africa, 1974–2013. World J Surg. 2017;41(12):3046–53. [DOI] [PubMed] [Google Scholar]
- 28.Qureshi JS, Young S, Muyco AP, Borgstein E, Charles AG, Mulwafu W, et al. Addressing Malawi’s surgical workforce crisis: A sustainable paradigm for training and collaboration in Africa. Surgery. 2013;153(2):272–81. [DOI] [PubMed] [Google Scholar]
- 29.Gyedu A, Debrah S, Agbedinu K, Goodman SK, Plange-Rhule J, Donkor P, et al. In-Country Training by the Ghana College of Physicians and Surgeons: An Initiative that has Aided Surgeon Retention and Distribution in Ghana. World J Surg. 2019;43(3):723–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pagaiya N, Kongkam L, Sriratana S. Rural retention of doctors graduating from the rural medical education project to increase rural doctors in Thailand: a cohort study. Hum Resour Health. 2015;13(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Techakehakij W, Arora R. Rural retention of new medical graduates from the Collaborative Project to Increase Production of Rural Doctors (CPIRD): a 12-year retrospective study. Health Policy Plan. 2017;32(6):809–15. [DOI] [PubMed] [Google Scholar]
- 32.Arora R, Chamnan P, Nitiapinyasakul A, Lertsukprasert S. Retention of doctors in rural health services in Thailand: impact of a national collaborative approach. Rural Remote Health [Internet]. 2017 Sep 30 [cited 2024 Apr 23];17(3). Available from: http://www.rrh.org.au/articles/subviewnew.asp?ArticleID=4344 [DOI] [PubMed]
- 33.Boonluksiri P, Tumviriyakul H, Arora R, Techakehakij W, Chamnan P, Umthong N. Community-based learning enhances doctor retention. Educ Health. 2018;31(2):114. [DOI] [PubMed] [Google Scholar]
- 34.Prashad A, Cameron B, McConnell M, Rambaran M, Grierson L. An examination of Eyal & Hurst’s (2008) framework for promoting retention in resource-poor settings through locally-relevant training: A case study for the University of Guyana Surgical Training Program. Can Med Educ J. 2017;8(2):e25-36. [PMC free article] [PubMed] [Google Scholar]
- 35.Zimmerman M, Shah S, Shakya R, SundarChansi B, Shah K, Munday D, et al. A staff support programme for rural hospitals in Nepal. Bull World Health Organ. 2016;94(1):65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sirili N, Frumence G, Kiwara A, Mwangu M, Anaeli A, Nyamhanga T, et al. Retention of medical doctors at the district level: a qualitative study of experiences from Tanzania. BMC Health Serv Res. 2018;18(1):260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lisam S, Nandi S, Kanungo K, Verma P, Mishra J, Mairembam D. Strategies for attraction and retention of health workers in remote and difficult-to-access areas of Chhattisgarh, India: Do they work? Indian J Public Health. 2015;59(3):189. [DOI] [PubMed] [Google Scholar]
- 38.Gow J, George G, Mwamba S, Ingombe L, Mutinta G. An evaluation of the effectiveness of the Zambian Health Worker Retention Scheme (ZHWRS) for rural areas. Afr Health Sci. 2013;13(3):800–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Mesa RYH, Marfori JRA, Fabian NMC, Camiling-Alfonso R, Javelosa MAU, Bernal-Sundiang N, et al. Experiences from the Philippine grassroots: impact of strengthening primary care systems on health worker satisfaction and intention to stay. BMC Health Serv Res. 2023;23(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mosadeghrad AM. Factors Affecting Medical Service Quality. Iran J Public Health. 2014;43(2):210–20. [PMC free article] [PubMed] [Google Scholar]
- 41.Rawal LB, Joarder T, Islam SMS, Uddin A, Ahmed SM. Developing effective policy strategies to retain health workers in rural Bangladesh: a policy analysis. Hum Resour Health. 2015;20(13):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Straume K, Shaw DM. Effective physician retention strategies in Norway’s northernmost county. Bull World Health Organ. 2010;88(5):390–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Almousa O, Zhang R, Dimma M, Yao J, Allen A, Chen L, et al. Virtual Reality Technology and Remote Digital Application for Tele-Simulation and Global Medical Education: An Innovative Hybrid System for Clinical Training. Simul Gaming. 2021;52(5):614–34. [Google Scholar]
- 44.Noya FC, Carr SE, Thompson SC. Attracting, Recruiting, and Retaining Medical Workforce: A Case Study in a Remote Province of Indonesia. Int J Environ Res Public Health. 2023;20(2):1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sendanyoye C, Sebastian S, Petrie S, Carson DB, Peters PA. Recruitment and Retention of Rural Physicians [Internet]. Spatial Determinants of Health Lab, Carleton University; 2019 [cited 2024 Apr 29]. Available from: https://repository.library.carleton.ca/concern/research_works/ff365527s
- 46.Emery A, Hurley S, Williams J, Pougnault S, Mercer A, Tennant M. A seven-year retrospective analysis of students entering medicine via a Rural Student Recruitment program in Western Australia. Aust J Rural Health. 2009;17(6):316–20. [DOI] [PubMed] [Google Scholar]
- 47.Russell D, Mathew S, Fitts M, Liddle Z, Murakami-Gold L, Campbell N, et al. Interventions for health workforce retention in rural and remote areas: a systematic review. Hum Resour Health. 2021;19(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Esu EB, Chibuzor M, Aquaisua E, Udoh E, Sam O, Okoroafor S, et al. Interventions for improving attraction and retention of health workers in rural and underserved areas: a systematic review of systematic reviews. J Public Health. 2021 Apr 13;43(Supplement_1):i54–66. [DOI] [PubMed]
- 49.Ashkenazi Y, Gordon M, Rosen B. Using financial incentives to attract medical residents to the periphery: The Israeli experience. Health Policy. 2019;123(1):80–6. [DOI] [PubMed] [Google Scholar]
- 50.Li J, Scott A, McGrail M, Humphreys J, Witt J. Retaining rural doctors: Doctors’ preferences for rural medical workforce incentives. Soc Sci Med. 2014;121:56–64. [DOI] [PubMed] [Google Scholar]
- 51.Chien AT, Chin MH, Alexander GC, Tang H, Peek ME. Physician financial incentives and care for the underserved in the United States. Am J Manag Care. 2014;20(2):121–9. [PMC free article] [PubMed] [Google Scholar]
- 52.Zurn P, Vujicic M, Lemière C, Juquois M, Stormont L, Campbell J, et al. A technical framework for costing health workforce retention schemes in remote and rural areas. Hum Resour Health. 2011;6(9):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ruisoto P, Ramírez MR, García PA, Paladines-Costa B, Vaca SL, Clemente-Suárez VJ. Social Support Mediates the Effect of Burnout on Health in Health Care Professionals. Front Psychol. 2021;13(11): 623587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schaefer R, Jenkins LS, North Z. Retaining doctors and reducing burnout through a flexible work initiative in a rural South African training hospital. Afr J Prim Health Care Fam Med [Internet]. 2021 [cited 2024 Apr 29];13(1). Available from: http://www.phcfm.org/index.php/PHCFM/article/view/2799 [DOI] [PMC free article] [PubMed]
- 55.World Health Organization. Retention of the health workforce in rural and remote areas: a systematic review. Web Annex A. GRADE evidence profiles. 2020;24.
- 56.Karaferis D, Aletras V, Raikou M, Niakas D. Factors Influencing Motivation and Work Engagement of Healthcare Professionals. Mater Socio Medica. 2022;34(3):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chmielewska M, Stokwiszewski J, Filip J, Hermanowski T. Motivation factors affecting the job attitude of medical doctors and the organizational performance of public hospitals in Warsaw, Poland. BMC Health Serv Res. 2020;20(1):701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mandal A, Phillips S. To stay or not to stay: the role of sense of belonging in the retention of physicians in rural areas. Int J Circumpolar Health. 2022;81(1):2076977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen J, Ssennyonjo A, Wabwire-Mangen F, Kim JH, Bell G, Hirschhorn L. Does decentralization of health systems translate into decentralization of authority? A decision space analysis of Ugandan healthcare facilities. Health Policy Plan. 2021;36(9):1408–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Faguet JP. Does Decentralization Increase Government Responsiveness to Local Needs? Evidence from Bolivia. SSRN Electron J [Internet]. 2001 [cited 2024 Apr 29]; Available from: http://www.ssrn.com/abstract=260579
- 61.Williamson L, Burog W, Taylor RM. A scoping review of strategies used to recruit and retain nurses in the health care workforce. J Nurs Manag. 2022;30(7):2845–53. [DOI] [PubMed] [Google Scholar]
- 62.Naal H, El Koussa M, El Hamouch M, Hneiny L, Saleh S. Evaluation of global health capacity building initiatives in low-and middle-income countries: A systematic review. J Glob Health. 2020;10(2): 020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets used and/or analysed during the current study are available from the corresponding author upon reasonable request.