Abstract
Background
Today, malnutrition is one of the biggest health crises for children in the world. Access to accurate and high-quality data is very important to establish policies to deal with it. Registries are considered valuable tools for data collection and management of child malnutrition. Designing a dataset is the first step toward developing a registry system.
Objective
This study aimed to determine the minimum data elements for the Child Malnutrition Registry System (CMRS).
Methods
In this descriptive and cross-sectional study, firstly, data elements were extracted from reviewing scientific papers, reviewing existing systems, and conducting interviews with experts. Then, the extracted data elements were validated using an expert panel and Delphi technique. The criterion for accepting the final data elements in the registry system was based on a collective agreement, and it was when 75% of the experts collectively agreed upon a particular data element.
Results
A dataset was designed using the determined minimum data elements, including administrative data elements with three sub-categories (demographic, socioeconomic, and healthcare providers) and clinical data elements with 11 sub-categories (medical history, anthropometric indicators, clinical examination, nutritional data, physical activity and sleep, lab tests, para-clinical tests, diagnosis, complications, care procedures, life status, and follow-up). The number of final data elements in administrative and clinical categories were 47 and 251, respectively.
Conclusion
A comprehensive and accurate dataset provides conceptual structures that are the basis for developing the children’s malnutrition registry system. The result of this study can fill the existing gaps in collecting, storing, and analyzing child malnutrition data. Furthermore, it can play an effective role in creating a successful strategic plan for improving child malnutrition.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12911-024-02771-1.
Keywords: Dataset, Malnutrition, Children, Registry system, Delphi technique
Introduction
Child malnutrition is considered a key contributor to the global disease burden [1]. Based on the latest key findings and joint document 2023 Edition by UNICEF/World Health Organization/World Bank Group, One hundred forty-eight million children under five years (22/3%) have been globally stunted, 45 million (6/8%) of which were wasted. Furthermore, there were 37 million (5/6%) children suffering from overweight in 2022; this number has surged by eight million since 2000 [2]. Nearly half of deaths among children under five years of age are linked to undernutrition. These mostly occur in low- and middle-income countries (LMICs), with a notable prevalence in Sub-Saharan Africa and Southern Asia. More than three-quarters of all children with severe wasting live in Asia, and another 22% live in Africa. Almost all of the impacted stunted children were from Asia (52% of the global share) and Africa (43% of the global share). In Asia, specifically, 76.6 million children under the age of five experience stunted growth; of these numbers, 30.5% is related to Southern Asia [2].
In Iran, although malnutrition prevalence has decreased in recent years [3, 4], various studies indicate the high prevalence of malnutrition in some geographical areas in Iran [5–9]. Therefore, malnutrition still remains a significant challenge for the healthcare sector in Iran [10].
The global burden of malnutrition has serious and long-term consequences for individuals and their families, communities, and countries [2], including growth retardation, cognitive and functional impairment, social and academic development deficiency, immunodeficiency, increased morbidity, and mortality [11, 12].
Malnutrition is defined as “an imbalance between nutrient requirement and intake, resulting in the cumulative deficits of energy, protein, or micronutrients which may negatively affect growth, development, and other outcomes” [13]. Malnutrition includes undernutrition and overnutrition. The former defines growth failure as being dependent on macronutrient and micronutrient deficiencies resulting from negligible nutrition [11]. On the other hand, overnutrition is induced by an excess of nutrients in the diet, leading to the accumulation of body fat detrimental to one’s health (i.e., overweight/obesity) [2].
Despite the economic progress in developing countries, malnutrition remains an important issue in these countries [14]. Moreover, the COVID-19 pandemic has deteriorated the nutritional status of the world. During the pandemic, several poor and developing countries have been facing food and nutritional shortages; also, governments were forced to cut social services that the poorest people depend on, such as school nutrition programs [15]. Along the same line, studies show that the COVID-19 pandemic and its consequences have led to a significant increase in malnutrition prevalence [4, 15, 16]. For example, it was shown in a small region in Pakistan that stunting and underweight increased by 17.26% and 12.29% during the COVID-19 [17]. The pandemic has worsened malnutrition through reduced household wealth, Limited access to nutritious food, disrupted nutrition services, and decreased physical activity. Stunting (chronic malnutrition) increased gradually and persisted long after the pandemic due to prolonged economic and health system challenges. Maternal malnutrition during the pandemic led to low birth weight and stunted growth in children. Wasting and severe wasting (acute malnutrition) could see a short-term spike, with estimates suggesting a potential 15% increase in prevalence in 2020 [18].
Nutritional surveillance and intervention programs in different countries can reduce the number of malnourished children [19, 20]. Child malnutrition should be identified as soon as possible to initiate the interventions and treatments in order to prevent any complications [21–23]. Having adequate and accurate data about the patient and their precision transmission is critical to providing high-quality care and malnutrition management [24]. Unfortunately, malnutrition data or data related to its risk are neither not appropriately reported nor reported at all [25, 26] Lack of reporting malnutrition or inaccurate reports downgrade management and interventions’ importance at the national or regional levels [27]. Besides, at lower levels, inadequate information about patients’ nutritional status may jeopardize childeren’s health status [24].
Malnutrition management is complex and multifaceted; meanwhile, there is a need to collect lots of relevant, accurate, and sufficient data about the nutritional status of patients, which further imposes a challenge on healthcare providers and professionals [28]. In this way, disease registries are valuable tools for data collection and management. The disease registry system is an organized system to collect, store, retrieve, analyze, and disseminate information about people with a specific disease [29]. The number of registries is continuously growing, and their use in recent years has been prevalent for various purposes such as public health, epidemiology, quality management, clinical registries, and disease-specific registries [30, 31].
From a certain perspective, registration systems can be categorized into three types: hospital registration, central registration, and population registration. These categories increase in scale in the order mentioned [32].
The value of a registry system strongly depends on the quality of data [31]. In disease registry systems, high-quality data plays a critical role in decision-making and planning; conversely, inaccurate data could increase the number of mistakes and wrong decisions [33]. One of the basic principles contributing to the quality of data is preparing a dataset (DS), which helps identify the data needed for specific purposes and provides clear definitions for integrating the data into the data set [34].
In the field of nutrition, the DS improves nutritional care by creating standard nutritional care pathways in which care roles and responsibilities are clearly defined [35]. A well-designed DS as a clinical tool is vital to ensure providing high-quality care to patients and to facilitate the collection of high-value clinical data [36, 37] A nutrition DS progresses the healthcare documentation level by allowing practitioners to regularly share information about the patient’s nutritional needs and facilitate inter- and intra-disciplinary communication [38]. Poor communication significantly leads to various side effects and endangers patient safety and care effectiveness [19, 24]; therefore, the standardization of nutritional data collection through a registry system is essential to improve the efficacy and safety of patient care [39].
In several studies, designing datasets for malnutrition was reported. They were used with different age groups, such as nutritional care for adults in primary healthcare [24, 28] or elderly nutrition in nursing homes [40–42]. Håkonsen et al. [24] presented the minimum data set in support of nurses in daily documentation in the field of nutrition. In this study, minimum data such as 1) comprehensive assessment of geriatrics, b) use of valid nutrition screening tool, and 3) They provided history and clinical diagnosis, physical examination and dietary assessment when evaluating the nutritional status of the elderly in primary health. Håkonsen et al. [28], in another study, developed a nutrition minimum data set for primary health care professionals. In this study, a total of 32 data items were identified, which were grouped into five categories: (1) physiological measurements, (2) ability to eat, (3) intake, ( 4) stress factors and (5) factors that indirectly affect intake and needs.
Given the critical role of the registry systems in child malnutrition management, we initially intended to develop a child malnutrition registry system (CMRS). Based on previous discussions about registries, this study was conducted at the national level and focused on Iran. However, we were aware that developing a CMRS requires a standard dataset. Due to the lack of a standard dataset for child malnutrition, we decided to design a dataset that considered the minimum data elements in this study. This study is a part of a larger research project aiming at developing a CMRS.
Materials and methods
This research is a mixed method study (a qualitative and quantitative study) that was conducted in 2020–2022 through the following stages:
Stage 1: identification of the data elements
This stage was done in three steps.
In the first step, we conducted a literature review. Based on the framework used in developing the minimum clinical datasets, this literature review ensures that the set of data elements is considered for inclusion in the comprehensive set of elements, not just the commonly or widely used set of elements [36].
The literature review was conducted in electronic databases, including the Persian language databases: Scientific Information Database (SID) in Persian, PubMed, Scopus, Web of Science Medline, and Google Scholar in English, to identify appropriate related sources. Moreover, we searched institutional websites including World Health Organization (WHO), United Nations International Children’s Emergency Fund (UNICEF), the World Bank, Centers for Disease Control and Prevention (CDC), National Health Service (NHS), the International Food Policy Research Institute (IFPRI), Food and Agriculture Organization (FAO), and Food and Nutrition Technical Assistance (FANTA).
The resources we used were articles, guidelines, forms, and reports available on the internet. Keywords in this study include the words related to the concepts of MDS or registry systems and words relating to malnutrition. The keywords used while performing database searches are as follows:
(dataset OR “data set” OR “minimum data set” OR “data element” OR “common data element” OR MDS OR registries OR “registry system” OR “surveillance system” OR “information system” OR database) AND (malnutrition OR undernutrition OR emaciation OR undernourish OR “protein-energy malnutrition” OR “protein-calorie malnutrition” OR “protein deficiency” OR subnutrition OR malnourished OR underweight OR stunting OR “wasting overnutrition” OR obesity OR overweight).
Inclusion criteria: We used full-text papers with the keywords in the title and abstracts. Also, we included the full text of papers in English and Persian, published until November 2022. Furthermore, the population up to 18 years old (according to UNICEF) was included in this study [39].
Exclusion criteria: In this study, we followed the following exclusion criteria: studies with the target group of only adults and the elderly, studies about food, papers published in languages other than Persian and English, and papers whose full-text were impossible to find.
Two reviewers separately reviewed the papers in this study to check the inclusion and exclusion criteria. Only full-text papers marked as important were evaluated. A third reviewer examined any disagreement between the two reviewers. Then, the data elements were extracted from the included articles.
In the second step, data elements of the Ministry of Health and Medical Education (MOHME) sources and the national electronic health records system were searched. The sources were continuously checked until the data elements were saturated and no new data elements appeared from the sources. Finally, a list of extracted data elements was prepared.
In the third step, face-to-face semi-structured interviews with the experts were conducted. A group of multidisciplinary experts, including nutritionists and pediatricians, were interviewed. Each interview lasted approximately 50 min. The potential participants were also informed about the goals of this research study (Appendix 1). After the first round of interviews, we used the snowball sampling method to recruit the remainder of the sample. Since the exact number of interviewees could not be determined before analysis [43], we continued to interview until the data saturation was reached. In this study, we reached data saturation after nine interviews (Table 1). Interviews were recorded and transcribed in Micro Soft Word document files; then, analysis was done in MAXQDA software (ver. 12). This study used a qualitative content analysis approach to analyze the interview transcripts. This involved systematically coding and categorizing the data to identify key themes and patterns. This method allowed for a deep understanding of the participants’ perspectives and the identification of specific requirements.
Table 1.
Demographic characteristics of experts who participated in the interview
| Category | Subcategory | Numbers | Percent (%) |
|---|---|---|---|
| Gender | Male | 8 | 61/5 |
| Female | 5 | 38/5 | |
|
Age category (Year) |
35–39 | 3 | 23 |
| 40–49 | 5 | 38/5 | |
| 50–59 | 5 | 38/5 | |
| Grade |
Masters Sciences(MS) |
5 | 38/5 |
| PhD | 4 | 30/75 | |
| Clinical Specialist | 4 | 30/75 | |
| Field of Study | Nutritionist | 9 | 69/25 |
| Pediatrician | 4 | 30/75 | |
| Work experience | 7–10 | 3 | 23 |
| 11–15 | 5 | 38/5 | |
| 26–30 | 5 | 38/5 |
Finally, extracted data elements of all the steps of this stage were merged, and a list of extracted data elements was prepared.
Stage 2: validation of the data elements
In this stage, the validity of the data elements was examined in two steps.
In the first step, an expert panel was held to evaluate the data elements and finalize the questionnaire of four members, including two Nutritionists, one Pediatrician, and one health information management in this panel. These experts have the required knowledge and experience related to child malnutrition and registry systems and were different from those who participated in the interview stage.
In the second step, the Delphi technique was used as a formal collaborative technique involving experts to answer the questionnaires in two or more rounds [44]. A group of nutritionists and pediatrician experts was chosen based on their expertise and experience in child malnutrition or malnutrition recording. These experts were different from those who participated in the interview and panel. Experts were asked to review and score the initial data elements based on their importance in the Delphi technique rounds. The data elements were validated using the Delphi technique in two rounds.
In the questionnaire, experts were asked about the necessity of data elements, such as Yes or No. If the experts agreed with the presence of a data element, they were also asked to specify whether it was optional or mandatory. A blank row was provided with respondents to add required data elements at the end of the questionnaire. (Appendix 2)
The criterion for accepting the final data elements in the registry system was based on a collective agreement of experts. In the first round, data elements with an agreement of less than 50% were removed; however, data elements receiving 50–75% agreement were thus transferred to the second round, and elements with more than 75% agreement in the first round of the Delphi technique were accepted. This process continued until we reached convergence and collective agreement on the dataset. The criterion to accept the final data elements was a collective agreement to achieve a level of 75% or more. The final data elements of the dataset were collected at the end of the Delphi technique rounds.
Results
Stage 1: identification of the data elements
In this stage, a large number of potential studies were identified. Through a rigorous screening process, this number was narrowed down to a final set of articles that met all inclusion criteria.
Final retrieved resources included Vitamin and Mineral Nutrition Information System (VMNIS) of WHO [45], Birbhum HDSS of India [46], China National Health Survey (CNHS) of China [47], National Nutrition Surveillance System (NNSS) of Vietnam [48], Helping to Outline Pediatric Eating Disorders (HOPE) in Australia [49], the Food and Nutrition Surveillance System (Sistema Nacional de Vigilância Alimentar Nutricional; SISVAN) in Brazil [50], Nutritional Surveillance Project (NSP) in Bangladesh [51] review of “Save and Children” [52] guideline WHO [37], and guideline of Ministry of Health and Medical Education (MOHME) of Iran [53].
After extracting the data from the first and second steps (literature review and MOHME sources), the required dataset to develop a CMRS was identified and inserted into the list, and 125 data elements were identified.
Stage 2: validation of the data elements
Based on the opinions obtained in the interviews with experts (Table 1), we determined two main themes: administrative and clinical data. Also, sub-themes were divided as follows: demographic (17 sections), socioeconomic (11 sections), health care providers (7 sections), medical history (8 sections), anthropometric indicators (9 sections), clinical examination (2 sections), nutritional data (8 sections), physical activity (3 sections), sleep status (2 sections), lab tests (6 sections), para-clinical tests (8 sections), diagnosis (8 sections), complications (2 sections), nutritional interventions (4 sections), pharmacotherapy (2 sections), surgery procedures (5 sections), life status, and follow-up (5 sections).
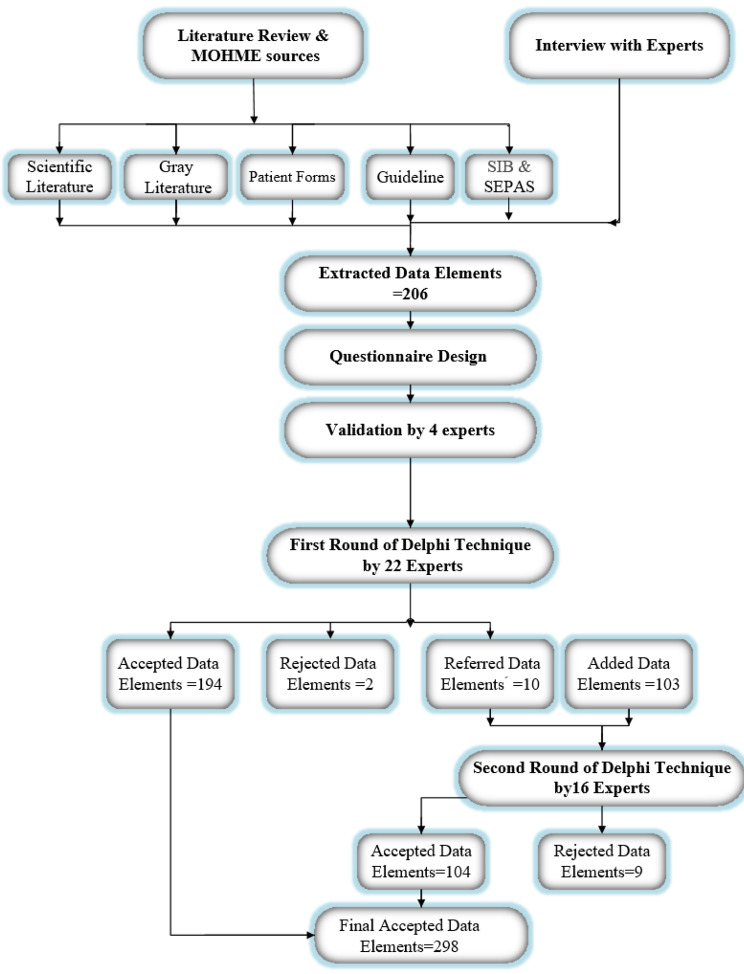
The data elements extracted from the first stage were merged, duplicated, and placed in a questionnaire. After reviewing the data elements of this questionnaire in the expert panel, 206 data elements remained in the questionnaire. These experts (Table 2) also assessed the content validity of this questionnaire. Figure 1 contains a flowchart that shows the research process and the number of data elements during the various stages. Furthermore, after organizing the sub-categories, 15 sub-categories were entered in the first round of Delphi; three sub-categories were in the administrative category, and 12 were in the clinical category. In the first round of the Delphi technique, 22 experts participated, but six of them did not return the questionnaires in the second round (See Table 3).
Table 2.
Demographic characteristics of experts who participated in the expert panel
| Category | Subcategory | Numbers | Percent (%) |
|---|---|---|---|
| Gender | Male | 2 | 50 |
| Female | 2 | 50 | |
|
Age category (Year) |
40–49 | 3 | 75 |
| 50–59 | 1 | 15 | |
| Grade | PhD | 3 | 75 |
| Clinical Specialist | 1 | 15 | |
| Field of Study | Nutritionist | 2 | 50 |
| Pediatrician | 1 | 25 | |
| Health Information Management | 1 | 25 | |
| Work experience | 5–10 | 3 | 75 |
| 11–16 | 1 | 15 |
Fig. 1.
Flowchart of data set extraction process
Table 3.
Demographic characteristics of experts who participated in the Delphi technique
| Category | Subcategory | Numbers | Percent (%) | ||
|---|---|---|---|---|---|
| First Round of Delphi | Second Round of Delphi | The first round of Delphi | The second round of Delphi | ||
| Gender | Male | 12 | 10 | 54/5 | 62/5 |
| Female | 10 | 6 | 45/5 | 37/5 | |
|
Age category (Year) |
30–34 | 4 | 2 | 18 | 12/5 |
| 35–39 | 4 | 2 | 18 | 12/5 | |
| 40–44 | 5 | 3 | 23 | 18/75 | |
| 45–49 | 3 | 4 | 14 | 25 | |
| 50> | 6 | 5 | 27 | 31/25 | |
| Grade |
Masters Sciences(MS) |
5 | 5 | 23 | 31/3 |
| PhD | 13 | 9 | 59 | 56/3 | |
| Clinical Specialist | 3 | 1 | 13 | 6/3 | |
| Fellowship | 1 | 1 | 5 | 6/3 | |
| Field of Study | Nutritionist | 18 | 14 | 82 | 87/5 |
| Pediatrician | 4 | 2 | 18 | 12/5 | |
| Work experience | > 5 | 3 | 1 | 13 | 6/25 |
| 5–10 | 6 | 4 | 27 | 25 | |
| 11–15 | 6 | 4 | 27 | 25 | |
| 16–20 | 2 | 2 | 10 | 12/5 | |
| 25–29 | 5 | 5 | 23 | 31/25 | |
The findings of the first round showed that 193 data elements were approved, and the data element “The patient’s main language” was rejected. Moreover, there was a 50–75% agreement on 10 data elements (see Tables 4 and 5). The experts suggested that the sub-category of clinical examination should be excluded from the general field. They also recommend that all the details of patients’ symptoms should be added to this sub-category. Therefore, this data element was removed (rejected), and 103 data elements of symptoms were then entered in the second stage of Delphi. There were two and 111 data elements in the administrative and clinical categories, respectively, in the second-round questionnaire.
Table 4.
Administrative data category of Data Set
| Data sections | The first round of Delphi | The second round of Delphi | The final number of data elements | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of data elements | < 50% | 50–75% | > 75% | Number of data elements | < 50% | 50–75% | > 75% | ||
| Demographic | 22 | 1 | 1 | 19 | 1 | 0 | 0 | 1 | 21 |
| Socioeconomic | 18 | 0 | 1 | 17 | 1 | 1 | 0 | 0 | 17 |
| Healthcare Providers | 9 | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 9 |
| 49 | 1 | 2 | 45 | 2 | 1 | 0 | 1 | 47 | |
Table 5.
Clinical data category of data set
| Data sections | The first round of Delphi | The second round of Delphi | Final number of data elements | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of data elements | < 50% | 50–75% | > 75% | Number of data elements | < 50% | 50–75% | > 75% | ||
| Medical History | 12 | 0 | 0 | 12 | 0 | 0 | 0 | 0 | 12 |
| Anthropometric indicators | 12 | 0 | 0 | 12 | 0 | 0 | 0 | 0 | 12 |
| Clinical examination | 2 | 1 | 0 | 1 | 103 | 0 | 0 | 103 | 104 |
| Vaccination | 4 | 0 | 4 | 0 | 4 | 4 | 0 | 0 | 0 |
| Nutritional data | 9 | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 9 |
| Physical activity and sleep | 9 | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 9 |
| Lab Tests | 62 | 0 | 4 | 58 | 4 | 4 | 0 | 0 | 58 |
| Paraclinical Tests | 8 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 8 |
| Diagnosis | 14 | 0 | 0 | 14 | 0 | 0 | 0 | 0 | 14 |
| Complications | 3 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 3 |
| Care Plan | 17 | 0 | 0 | 17 | 0 | 0 | 0 | 0 | 17 |
| life status and follow-up | 5 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 5 |
| 157 | 1 | 8 | 148 | 111 | 8 | 0 | 103 | 251 | |
The results obtained from the second round of the Delphi technique show that the “child’s educational status” was finalized from the demographic data sub-category with 75% agreement. However, one data element (type of parents’ marriage) from the socioeconomic sub-category did not receive the collective agreement, which was later removed. The vaccination sub-category with four data elements and laboratory test sub-category with another four data elements (PT/ INR, PTT, PCO2, PH/ Cl) were not approved and eliminated. All 103 data elements added in the second round of the Delphi technique were approved and finalized (see Tables 6 and 7).
Table 6.
Administrative data elements for a data set of CMRS
| Section name | Data elements |
|---|---|
| Demographic |
Mandatory Patient name and surname- Father name -National identity number- Sex- Date of birth- Type of birth- How many pregnancy weeks was he/she born?- Mobile Phone Number |
|
Optional Parental consent- Province of birth- Country of birth- City of Birth –Religion- Ethnicity -Educational status of the child (kindergarten, elementary …)- Type of insurance / supplementary insurance- Blood group- Residence address- Residence zip code- Home phone number | |
| Socioeconomic |
Mandatory -Dependent (parents /only father due to mother’s death / only father due to divorce / only mother due to father’s death / only mother due to divorce/grandparents / legal guardian) - Family income level- residence (urban, rural, …) |
|
Optional - Father’s job- Mother’s job- Where does the child come in his/her family?- Number of sisters- Number of brothers- Father educational status- Mother educational status- Having a caregiver or babysitter- Babysitter educational status - Maternal substance abuse (drugs, smoking, alcohol…)- Time? (in pregnancy/ in postnatal period/every time)-severity and amount of consumption -substance abuse by the father (drugs, smoking, alcohol…)-severity and amount of consumption | |
| Healthcare Providers |
Mandatory Name and surname of the nutritionist- Name and surname of the Attending physician- Acceptance date- Encounter reason- length of stay (LOS)- Patient discharge status |
|
Optional Medical center Name- Type of medical center- Medical record number |
Table 7.
Clinical data elements for a data set of CMRS
| Section name | Data elements |
|---|---|
| Medical History |
Mandatory Weight loss or no weight gain in the last three months- History of a specific disease in the child (mentioning the type of disease) |
|
Optional History of burns(Yes/No)/ Burn site/date- History of surgery- History of individual allergies- Drug sensitivity/drug name- Food allergy/food name- History of a specific disease in family and close relatives (mentioning the type of disease) | |
| Anthropometric indicators |
Mandatory weight at admission - Height at admission –Age- BMI for age |
|
Optional Birth weight- Birth height- Head circumference- Birth Z score- Z score weight for height- Z score height for age- Z score Weight for age- MUAC | |
| Clinical examination |
Mandatory Digestion and liver: Diarrhea- Vomiting skin and hair: Edema- Dermatitis |
|
Optional Digestion and liver: bloody diarrhea- nausea- Bloody vomiting- Bloody stools- Cough- Chronic cough- Constipation- Swallowing disorder- Anorexia- Fever- Chronic abdominal pain- Acute abdominal pain- Flatulence- Abdominal tenderness- Abdominal mass- hypoglycemia- Hypothermia Kidney and urinary tract: Kidney failure- Dehydration Brain and Nervous: Mental retardation- Hyperactive- Decreased consciousness- Convulsions- Tremor- Headache- Ataxia Skin and hair: Eczema- Paleness- Seborrhea around the lips and nose- Cellulite- Dermatitis caused by photosensitivity- Acrodermatitis- Follicular hyperkeratosis (such as sandpaper)- Skin without pigment- Purpura- Scrotal and vaginal dermatitis- Perinatal abscess- Hair loss- Coin hair loss- Alopecia- Unpigmented and dull hair that is easily pulled out- Hirsuitism- Recent hair color change- Dandruff- skin itching- skin dryness- Yellowing of the skin- Urticaria- Hyperhidrosis Subcutaneous tissue: Tissue Reduction Sight test and eye examination: Adaptation to darkness- Sensitivity to light- Color differentiation- Bitot spots, xerophthalmia, keratomalacia- Conjunctival pallor Face, mouth and neck: Corner stomatitis- Cheilosis- Bleeding from the gums- Papules atrophy- Soft language- Glossitis- Cavities(Tooth Decay)- Dysgeusia(Decreased taste sensitivity)- Goiter- Hypogonadism- Rosary bead- Bleeding under the skin- Skull bulge- Wide Fontanelle- Cranial softness- Painful bones to the touch- Painful head vertex in touch- Spoon nails (koilonychia)- Sensorimotor neuropathy- Ocular muscle paralysis- Tetany Pulmonary: Atelectasis- Pneumothorax- Emphysema- Pleural effusion- Pulmonary abscess- Bronchopulmonary- Dysplasia Cardiovascular: Heart failure- Dilated- Cardiomyopathy- Atrial arrhythmia- Ventricular arrhythmia- Endocarditis- Tetralogy of Fallot- Dextrocardia Musculoskeletal: Joint pain- Muscle pain- Dry joint- Arthritis- Movement restrictions Psychiatry: Schizophrenia- Anxiety- Depression Duration of symptoms | |
| Nutritional data |
Mandatory Type of feeding (Breast milk/formula or both / family food / complementary nutrition)- Nutrition Supplements and vitamins in use- Daily consumption of vegetables and fruits- Drinks frequency and amount |
|
Optional Age to start complementary feeding of infant-Feeding method (Oral / NPO / TPN / Intestinal feeding by gavage or EN / Part of feeding intravenously or PPN / Other)- Food habits- Junk Food- Water source and its health status (protected or not) | |
| Physical activity and sleep |
Mandatory Sleep quality (good/average / …)- Physical activity and its duration in the day- Average walking per day (for example, from school to home or Conversely)- Average daily time spent watching TV- Average daily time spent playing mobile phone games and using computer |
|
Optional Duration of sleep- Delay in falling asleep and its rate- Waking up in the middle of the night (yes/no)/ its rate | |
| Lab Tests |
Mandatory Hematology: Hb- ESR Biochemistry: Total Protein- Albumin Serum- Pre Albumin- retinol-binding protein- Globulin- TG- Cholesterol- HDL- LDL- AlP- ALT(SGPT)- AST(SGOT)- FBS/ Glucose- Hb (Hemoglobin) A1C- Serum Iron- Ferritin- K- Mg- Na- Folic acid- BUN- Creatinine- Uric Acid- Vit.B12- Vit.B1- Vit.B2- Vit. A- Vit.D- Zn- Selenium- Iodine- Calcium- Phosphate- Urin: Urine- analysis/ UC Stool: Stool analysis/ SC hormone levels: TSH Test time |
|
Optional Hematology: WBC- RBC- HCT- MCV- MCH- MCHC- Platelet- MPV- PMN- Lymph- Mono- EOS- Retic count Biochemistry: VLDL- T.Bil- D.Bil -PT/ INR- PTT Sweat: Sweat Chloride test(CI) hormone levels: T3- T4 | |
| Other Paraclinical Tests |
Mandatory Medical Imaging: Type of medical imaging (MRI, CT scan, ultrasound, …)- Anatomical location- Date of medical imaging- Result |
|
Optional Pathology: Biopsy site- Date of receiving the specimen – Result- Date of receipt of the result | |
| Diagnosis |
Mandatory Undernutrition- Wasted- Severely Wasted- Stunted- Severely Stunted- Underweight- Severely Underweight- Mineral deficiency- Overweight- obesity |
|
Optional Refeeding syndrome- Kwashiorkor- Nutritional marasmus- Diagnosis code in ICD-10 | |
| complications |
Mandatory Complication(yes / no)- Complication name |
|
Optional Date of onset of Complication | |
| Care Procedures |
Mandatory Nutritional interventions: Recommended dietary supplement (drug supplement / natural supplement)- Vitamin intake (yes/no)/Vitamin type- Micronutrients (yes / no)/Type of micronutrients Pharmacotherapy: Need to get medication (yes/no)- medicine name- Dose Surgery: Surgery (yes/no)- Name of surgery- Result |
|
Optional Nutritional interventions: Other recommendations Pharmacotherapy: Date of Start taking- End of use Surgery: Date of surgery- Anesthesia medication received Action code in ICD-9-CM | |
| life status and follow-up |
Mandatory Status (improvement / no improvement/referral / non-response / death /other)- Need to get food parcels -Next follow-up date |
|
Optional Death (intermediate cause / underlying cause/date/relationship between death and malnutrition / …) Source or method of follow-up (telephone contact with family/patient file / HIS /SIB system / other) |
Note
MUAC: (Mid-Upper Arm Circumference)
LOS: (length of stay)
SIB : Health Ministry’s Comprehensive Network is entitled SIB (an abbreviation for the Persian equivalent of ‘integrated health system’), which is the EHR system
Discussion
In the present study, we created a dataset. As an essential part of a registry system, this dataset can provide sufficient, relevant, and high-quality data for child malnutrition care and management. Svensson-Ranallo et al. proposed a framework for the development of clinical MDS called MCDS. Furthermore, these researchers argue that this framework is a coherent method to create high-quality MCDS for individuals and organizations [36]. Our study adopted a similar approach to the proposed framework; moreover, we conducted interviews with experts to find out their opinions on the dataset.
The dataset was categorized into administrative (demographic, socioeconomic, healthcare providers) and clinical (11 sub-categories) data. The demographic and socioeconomic data elements were comparable to those in Koletzko et al.‘s dataset on nutrition infancy [54] including mother’s education, ethnicity, country of birth, and maternal substance abuse.
In child malnutrition, due to the nature of this disease, administrative data elements such as demographics and socioeconomics also play an essential role in the dataset. The demographic sub-category and its data elements such as location and contact number, can help track child malnutrition. Furthermore, the demographic data elements can assess the prevalence of this disease in various cities and provinces. Every child has the right to equal opportunity, and each society has a role to ensure that no one is denied these opportunities [55]. Having prevalence information on child malnutrition in various provinces can help managers make decisions accurately, distribute budgets equitably, and allocate more resources to less privileged and more malnourished regions.
The clinical category was finalized with 11 sub-categories, namely medical history, anthropometric indicators, clinical examination, nutritional data, physical activity and sleep, lab tests, para-clinical tests, diagnosis and type of malnutrition, complications, care procedures, life status, and follow-up treatment.
Meanwhile, the availability of a parent’s medical history is critical to making the appropriate clinical decisions. As a type of clinical data, follow-up data is required to evaluate the efficacy of nutritional interventions and therapeutic outcomes. In this regard, Tuffery’s study also confirms the importance of a patient’s medical history [52].
The vaccination sub-category and related data elements were not approved in the second round of Delphi, and they were eventually removed from the dataset. Global Vaccine Action Plan 2011–2020 (GVAP), approved by the World Health Assembly in 2012, calls on all countries to achieve ≥ 90% national coverage for all vaccines in their regular immunization schedules by 2020 [56].
Studies conducted in Iran show that the country has reached vaccination coverage of more than 98% [57], and even in some areas, it was very close to 100% [58]. On the other hand, all information related to vaccination, dates and doses about all infants from birth to 6 years of age is collected in the Health Ministry’s Comprehensive Network, entitled SIB (an abbreviation for the Persian equivalent of ‘integrated health system’). Perhaps for these reasons, the experts did not consider vaccination information necessary in the Data Set.
In the second round of Delphi, 103 data elements were added. In the first round of Delphi, we defined the clinical examination category as a whole with two data elements. We think that the nature of the dataset [36] should have a minimal number of data elements. Therefore, we believe that the sub-category of the clinical examination is better if a smaller amount of data is included in the general field. However, the experts suggested that clinical examinations provide us with more details about the importance of malnutrition symptoms; therefore, they added it to the second round.
We addressed all indicators of malnutrition, namely birth weight, birth height, admission weight, admission height, head circumference, birth Z score, BMI for age, Z score weight for height, Z score height for age, Z score weight for age, and MUAC (Mid-Upper Arm Circumference) in the dataset. Also, these indicators are similar to WHO guidelines [37]. There is no established standard for assessing wasting in children’s medicine. Children under the age of five can be diagnosed through two anthropometric indicators: the weightfor-height z-score (WHZ) or the mid-upper arm circumference (MUAC) The World Health Organization currently recommends using both criteria for screening and admission to treat severe and moderate cases [59, 60].
As an inclusion criteria in this study, we considered children up to 18 years old [61]; in some studies, however, 10 to 18 years old is considered adolescent; therefore, some anthropometric indicators of child age cannot be used for these adolescents [37]. We thus attempted to consider all indicators up to 18 years, such as BMI for age.
By relying on the WHO definition of malnutrition [62], we attempted to address all various forms of malnutrition, namely wasting, stunting, underweight, micronutrient deficiencies, overweight, and obesity. Since obesity is a relatively new problem that needs more attention [63], we thus decided to consider the sub-category of physical activity and sleep with data elements related to overweight and obesity. These data elements can be very helpful in the treatment and intervention programs. Results of Bel-Serrat et al.‘s study indicated that physical activity, sedentary behaviors, and diet should be paid more attention [64]. Furthermore, in our Data Set, there is a sub-category of nutritional data with data elements such as food habits, junk food, daily consumption of vegetables, fruits and drinks frequency and amount, and water source. These data elements are similar to the data elements in the WHO guideline [37] and Bel-Serrat et al.‘s study as well [64].
As the World Health Organization has pointed out, the medical history of parents is important in children’s malnutrition; for example, the intergenerational cycle of malnutrition is exacerbated by the fact that small women are at greater risk of delivering an infant with low birth weight [65], and this data element was also included in our end list.
The Data Set will help clarify the concept of malnutrition. It also helps collect accurate and comprehensive data about children with malnutrition to be used in planning, policymaking, and health care delivery to these children. To the best of our knowledge, this pioneering study in Iran developed the Data Set, which focuses on child malnutrition. However, this study has some limitations. First, the parents of malnourished children, who are one of the main beneficiaries of the Data Set, have not been involved in this study. Hence, the patients’ and their families’ perspectives and voices have been missed from our Data Set. Second, data were subjective and based on participants’ availability, experience, and knowledge; thus, data elements were finalized based on a limited number of experts.
Also in the second round of the Delphi technique, a number of experts from the first stage did not participate, potentially limiting the comprehensiveness of the final expert consensus.
Conclusion
A comprehensive and accurate dataset for child malnutrition provides a standard structure of concepts that are the basis for the development of a registry system. In this study, we developed a dataset to standardize the data in order to be used for developing a CRMS (Child Malnutrition Registry System). We think that this dataset can demonstrate low-quality malnutrition data by providing consistent, complete, and uniform data elements and improving communications among healthcare providers. Furthermore, the dataset can fill the existing gaps in collecting, storing, and analyzing child malnutrition data. Moreover, it can play an effective role in developing a successful strategic plan in order to improve child malnutrition. Finally, creating a national registry system based on the data obtained from this research is a practical and essential proposal that will be addressed in the next step of this project. The design and implementation of this system will be the focus of future efforts.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the Iran University of Medical Sciences, Pediatric Gastroenterology Liver and Nutrition Research Center, and all study participants.
Author contributions
Conceptualization, M.S. and M.L. ; Methodology, M.S., M.L., B.O, A.SH ; Validation, M.S., MJ.S.; Formal analysis, M.S.; Investigation, M.L.; Data curation, M.S.; Writing—original draft, M.S.; Supervision, M.S, B.O, A.SH.; All authors have read and agreed to the published version of the manuscript.
Funding
There were no funding sources for this study.
Data availability
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval for the study was obtained from the Ethical Committee of Iran University of Medical Sciences (IR.IUMS.REC.1397.1083). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Malihe Sadeghi, Email: sadeghiii.m@gmail.com.
Mostafa Langarizadeh, Email: langarizade.m@iums.ac.ir.
Beheshteh Olang, Email: beheshteholang@gmail.com.
References
- 1.Chilot D, Belay DG, Merid MW, Kibret AA, Alem AZ, Asratie MH, et al. Triple burden of malnutrition among mother–child pairs in low-income and middle-income countries: a cross-sectional study. BMJ open. 2023;13(5):e070978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levels and trends in child malnutrition: UNICEF/WHO/World Bank Group joint child. malnutrition estimates: key findings of the 2023 edition. World Health Organization [internet].[cited 2023 November 11]. https://www.who.int/publications/i/item/9789240073791
- 3.Ghodsi D, Rasekhi H, Yari Z, Roustaee R, Nikooyeh B, Faramarzi A, et al. Prediction and analysis of trends in the nutritional status of children under 5 years in Iran: reanalysis of the results of national surveys conducted between 1998 and 2020. Front Nutr. 2023;10:1083318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zar HJ, Dawa J, Fischer GB, Castro-Rodriguez JA. Challenges of COVID-19 in children in low-and middle-income countries. Paediatr Respir Rev. 2020. [DOI] [PMC free article] [PubMed]
- 5.Moradi Y, Shadmani FK, Mansori K, Hanis SM, Khateri R, Mirzaei H. Prevalence of underweight and wasting in Iranian children aged below 5 years: a systematic review and meta-analysis. Korean J Pediatr. 2018;61(8):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Veghari G. The comparison of under-five-children’s nutrition status among ethnic groups in north of Iran, 1998–2013; results of a three stages cross-sectional study. Iran J Pediatr. 2015;25(4). [DOI] [PMC free article] [PubMed]
- 7.Dehghan Haghighi J, Ayubi E, Sadeghi-Bojd S, Narouei B. Malnutrition and its related factors among children under five years of age. Int J Pediatr. 2022;10(2):15412–25. [Google Scholar]
- 8.Manoochehri S, Faradmal J, Poorolajal J, Asadi FT, Soltanian AR. Risk factors associated with underweight in children aged one to two years: a longitudinal study. BMC Public Health. 2024;24(1):1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nikooyeh B, Rasekhi H, Rabiei S, Ghodsi D, Amini M, Yari Z et al. Alarming High Prevalence of Various Forms of Malnutrition in 24–60 M Children in Sistan-Baluchestan: Needing of Urgent Actions, Tomorrow is Too Late! National Food and Nutrition Surveillance. Iran J Nutr Sci Food Technol. 2024:23–32.
- 10.Mansori K, Shadmani FK, Mirzaei H, Azad RV, Khateri S, Hanis SM, et al. Prevalence of stunting in Iranian children under five years of age: systematic review and meta-analysis. Med J Islamic Repub Iran. 2018;32:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bharaniidharan J, Reshmi S. Review on malnutrition: impact and prevention. Int J Adv Res Innov. 2019;7:240–3. [Google Scholar]
- 12.Carter LE, Shoyele G, Southon S, Farmer A, Persad R, Mazurak VC, et al. Screening for pediatric malnutrition at hospital admission: which screening tool is best? Nutr Clin Pract. 2020;35(5):951–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta NM, Corkins MR, Lyman B, et al. Defining pediatric malnutrition: a paradigm shift toward etiology-related definitions. JPEN J Parenter Enter Nutr. 2013;37(4):460–81. [DOI] [PubMed] [Google Scholar]
- 14.Mohseni M, Arian A, Kalantari N. Factors associated with malnutrition among under five-year-old children in Iran: a systematic review. Ann Trop Med Public Health. 2017;10:1147–58. [Google Scholar]
- 15.Micha R, Mannar V, Afshin A, Allemandi L, Baker P, Battersby J et al. Global Nutrition Report 2020: action on equity to end malnutrition. Bristol, UK: Development Initiatives. https://globalnutritionreport.org/reports/2020-glo
- 16.Headey D, Heidkamp R, Osendarp S, Ruel M, Scott N, Black R, et al. Impacts of COVID-19 on childhood malnutrition and nutrition-related mortality. Lancet. 2020;396(10250):519–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alam MB, Shahid M, Alzghoul BI, Yang J, Zakar R, Malik NI, et al. The effects of Financial stress and Household Socio-Economic Deprivation on the Malnutrition Statuses of Children under five during the COVID-19 Lockdown in a Marginalized Region of South Punjab, Pakistan. Children. 2022;10(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levels and trends in child malnutrition: UNICEF/WHO/The World Bank Group. joint child malnutrition estimates: key findings of the 2021 edition [internet].[cited 2024 May 2]. https://www.who.int/publications/i/item/9789240025257
- 19.Penny ME, Creed-Kanashiro HM, Robert RC, Narro MR, Caulfield LE, Black RE, et al. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster-randomised controlled trial. Lancet. 2005;365:1863–72. [DOI] [PubMed] [Google Scholar]
- 20.Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health. 2011;11(Suppl 3):S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salvà A, Corman B, Andrieu S, Salas J, Vellas B. Minimum data set for nutritional intervention studies in elderly people. Journals Gerontol Ser A: Biol Sci Med Sci. 2004;59(7):M724–9. [DOI] [PubMed] [Google Scholar]
- 22.McGrath CJ, Arndt MB, Walson JL. Biomarkers to stratify risk groups among children with malnutrition in resource-limited settings and to monitor response to intervention. Hormone Res Paediatrics. 2017;88(1):111–7. [DOI] [PubMed] [Google Scholar]
- 23.Landi M, Swakin E, Minijihau C, Welch H, Tefuarani N, Duke T. Severe malnutrition in children in Papua New Guinea: effect of a multi-faceted intervention to improve quality of care and nutritional outcomes. Paediatrics Int Child Health. 2017;37(1):21–8. [DOI] [PubMed] [Google Scholar]
- 24.Håkonsen SJ, Pedersen PU, Bjerrum M, Bygholm A, Peters MD. Nursing minimum data sets for documenting nutritional care for adults in primary healthcare: a scoping review. JBI Evid Synthesis. 2018;16(1):117–39. [DOI] [PubMed] [Google Scholar]
- 25.Khalatbari-Soltani S, Waeber G, Marques-Vidal P. Estimation of malnutrition prevalence using administrative data: not as simple as it seems. Clin Nutr. 2015;34(6):1276–7. [DOI] [PubMed] [Google Scholar]
- 26.Meijers JMM, Halfens RJG, van Bokhorst-de MAE, Dassen T, Schols JMGA. Malnutrition in Dutch health care: prevalence, prevention, treatment, and quality indicators. Nutrition. 2009;25(5):512–9. [DOI] [PubMed] [Google Scholar]
- 27.Khalatbari-Soltani S, Waeber G, Marques-Vidal P. Diagnostic accuracy of undernutrition codes in hospital administrative discharge database: improvements needed. Nutrition. 2018;55:111–5. [DOI] [PubMed] [Google Scholar]
- 28.Håkonsen SJ, Pedersen PU, Bygholm A, Peters MD, Bjerrum M. Speaking the same language: development of a nutrition minimum data set for healthcare professionals in primary healthcare. Health Inf J. 2020;26(1):248–63. [DOI] [PubMed] [Google Scholar]
- 29.Gliklich RE, Dreyer NA, Leavy MB. Registries for Evaluating Patient Outcomes: A User’s Guide. Third edition. Two volumes. (Prepared by the Outcome DEcIDE Center [Outcome Sciences, Inc., a Quintiles company] under Contract No. 290 2005 00351 TO7. AHRQ publication No. 13(14)-EHC111. Rockville, MD: Agency for Healthcare Research and Quality; April 2014. http://www.effectivehealthcare.ahrq.gov/registries-guide-3.cfm.
- 30.Lindoerfer D, Mansmann U. A comprehensive assessment tool for patient Registry Software systems: the CIPROS checklist. Methods Inf Med. 2015;54(5):447–54. [DOI] [PubMed] [Google Scholar]
- 31.Lindoerfer D, Mansmann U. Enhancing requirements engineering for patient registry software systems with evidence-based components. J Biomed Inf. 2017;71:147–53. [DOI] [PubMed] [Google Scholar]
- 32.Sadeghi M. Development of child malnutrition registry system in Iran. Iran University of Medical Sciences. Tehran, Iran, Ph.D Thesis. Nonember. 2021. [In persian].
- 33.Davis NA, LaCour M. Foundations of Health Information Management-E-Book. Elsevier Health Sciences; 2016.
- 34.Ogarek JA, McCreedy EM, Thomas KS, Teno JM, Gozalo PL. Minimum data set changes in health, end-stage disease and symptoms and signs scale: a revised measure to predict mortality in nursing home residents. J Am Geriatr Soc. 2018;66(5):976–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin L, de van der Schueren MA, Blauwhoff-Buskermolen S, Baracos V, Gramlich L. Identifying the barriers and enablers to nutrition care in head and neck and esophageal cancers: an international qualitative study. J Parenter Enter Nutr. 2016;40(3):355–66. [DOI] [PubMed] [Google Scholar]
- 36.Svensson-Ranallo PA, Adam TJSF. A framework and standardized methodology for developing minimum clinical datasets. AMIA Jt Summits Transl Sci Proc. 2011;2011:54–58. [PMC free article] [PubMed]
- 37.Al Jawaldeh A, Osman D, Tawfik A. Food and nutrition surveillance systems: a manual for policy-makers and programme managers / World Health Organization. Regional Office for the Eastern Mediterranean. 2014. ISBN: 978-92-9021-840-1. 2014.
- 38.Håkonsen SJ. Design and Development Process of a Nutrition Minimum Data Set for Primary Health Care-A User Centered Approach. Aalborg University Denmark. Ph.d Dissertation. 2019. 10.5278/vbn.phd.med.00123
- 39.Ireton-Jones C, DeLegge M. Home parenteral nutrition registry: a five-year retrospective evaluation of outcomes of patients receiving home parenteral nutrition support. Nutrition. 2005;21(2):156–60. [DOI] [PubMed] [Google Scholar]
- 40.Saliba D, Jones M, Streim J, Ouslander J, Berlowitz D, Buchanan J. Overview of significant changes in the Minimum Data Set for nursing homes version 3.0. J Am Med Dir Assoc. 2012;13(7):595–601. [DOI] [PubMed] [Google Scholar]
- 41.Luo H, Lum TY, Wong GH, Kwan JS, Tang JY, Chi I. Predicting adverse health outcomes in nursing homes: a 9-year longitudinal study and development of the FRAIL-minimum data set (MDS) quick screening tool. J Am Med Dir Assoc. 2015;16(12):1042–7. [DOI] [PubMed] [Google Scholar]
- 42.Crogan NL, Corbett CF. Predicting malnutrition in nursing home residents using the minimum data set. Geriatr Nurs. 2002;23(4):224–6. [DOI] [PubMed] [Google Scholar]
- 43.Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative Res Sport Exerc Health. 2019:1–16.
- 44.Davey CJ, Slade SV, Shickle D. A proposed minimum data set for international primary care optometry: a modified Delphi study. Ophthalmic Physiol Opt. 2017;37(4):428–39. [DOI] [PubMed] [Google Scholar]
- 45.Aburto NJ, Rogers L, De-Regil LM, Kuruchittham V, Grace R, Arif R et al. An evaluation of a global vitamin and mineral nutrition surveillance system. Arch Latinoam Nutr. 2013;63(2). [PubMed]
- 46.Ghosh S, Barik A, Majumder S, Gorain A, Mukherjee S, Mazumdar S, et al. Health & demographic surveillance system profile: the Birbhum population project (Birbhum HDSS). Int J Epidemiol. 2015;44(1):98–107. [DOI] [PubMed] [Google Scholar]
- 47.Gong W, Liu A, Yao Y, Ma Y, Ding C, Song C, et al. Nutrient supplement use among the Chinese population: a cross-sectional study of the 2010–2012 China nutrition and health surveillance. Nutrients. 2018;10(11):1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hajeebhoy N, Nguyen PH, Tran DT, de Onis M. Introducing infant and young child feeding indicators into national nutrition surveillance systems: lessons from V ietnam. Matern Child Nutr. 2013;9:131–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Watson HJ, McCormack J, Hoiles KJ, Forbes D, Potts J. The HOPE (helping to Outline Paediatric Eating disorders) project: development and debut of a paediatric clinical eating disorder registry. J Eat Disorders. 2013;1(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Coelho LC, Asakura L, Sachs A, Erbert I, Novaes CdRL SGAG. Food and Nutrition Surveillance System/SISVAN: getting to know the feeding habits of infants under 24 months of age. Ciencia Saude Coletiva. 2015;20:727–38. [DOI] [PubMed] [Google Scholar]
- 51.Akhter N, Haselow N. Using data from a nationally representative nutrition surveillance system to assess trends and influence nutrition programs and policy. Field Actions Sci Rep J Field Actions. 2010;4.
- 52.Tuffrey V. Nutrition surveillance systems: their use and value. London: Save the Children and Transform Nutrition. 2016. Available frome: https://resourcecentre.savethechildren.net/library/nutrition-surveillance-systems-their-use-and-value
- 53.Guidelines and forms of nutritional assessment for children and adolescents Hospitalization. Ministry of Health and Medical Education. The treatment deputy of Health Department. Office of Hospital Management and Clinical Services Excellence. 2019. [In persian]. http://vct.qums.ac.ir/Portal/home/?217776/%D9%81%D8%B1%D9%85-%D9%87%D8%A7-%D9%88-%DA%86%DA%A9-%D9%84%DB%8C%D8%B3%D8%AA-%D9%87%D8%A7
- 54.Koletzko B, Fewtrell M, Gibson R, Van Goudoever JB, Hernell O, Shamir R, et al. Core data necessary for reporting clinical trials on nutrition in infancy. Annals Nutr Metabolism. 2015;66(1):31–5. [DOI] [PubMed] [Google Scholar]
- 55.Mohseni M, Aryankhesal A, Kalantari N. Prevention of malnutrition among children under 5 years old in Iran: a policy analysis. PLoS ONE. 2019;14(3):e0213136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Feldstein LR, Mariat S, Gacic-Dobo M, Diallo MS, Conklin LM, Wallace AS. Global routine vaccination coverage, 2016. MMWR Morbidity Mortal Wkly Rep. 2017;66(45):1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nikfarjam A, Shamshiri A, Hasanpour Z, Khalili M. Status of vaccination coverage in children 24 months to 6 years in urban and high risk areas covered by Tehran University of Medical Sciences. Iran J Epidemiol. 2016;11(4):10–9. [Google Scholar]
- 58.Mirahmadizadeh AR, Zahmatkesh S, Kashfi nezhad MS, Sayadi M, Tabatabaee HR, Mokhtari AM, et al. Vaccination Coverage in Children of Fars Province, 2017: achievement of Global Vaccine Action Plan goals. SADRA Med Sci J. 2018;6(4):251–60. [Google Scholar]
- 59.López-Ejeda N, Medialdea L, Vargas A, Coronado J, García-Arias MÁ, Marrodán MD. Public Health Implications of Wasting and Stunting Relationship in children under five years highly vulnerable to Undernutrition in Guatemala: the REDAC study. Nutrients. 2022;14(19):3945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.https://www.who.int/publications/i/item/9789241506328WHOGUotMoSAMiIaCAo
- 61.Unicef. The convention on the rights of the child. Guiding principles: General requirements for all rights [internet]. 2021 [cited 14 December 2021]. https://www.unicef.org/media/60981/file/convention-rights-child-text-child-friendly-version.pdf
- 62.https://www.who.int/health-topics/malnutrition#tab=tab_1 MWHOIAcJAf.
- 63.Daga S, Mhatre S, Kasbe A, Dsouza E. Double burden of malnutrition among Indian schoolchildren and its measurement: a cross-sectional study in a single school. BMJ Paediatrics open. 2020;4(1). [DOI] [PMC free article] [PubMed]
- 64.Bel-Serrat S, Huybrechts I, Thumann BF, Hebestreit A, Abuja PM, De Henauw S, et al. Inventory of surveillance systems assessing dietary, physical activity and sedentary behaviours in Europe: a DEDIPAC study. Eur J Public Health. 2017;27(4):747–55. [DOI] [PubMed] [Google Scholar]
- 65.https://https://who.int/data/nutrition/nlis/info/malnutrition-in-childrenWHOMicAi
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.