Abstract
Objective
This study aims to perform a meta-analysis that integrates multiple literature sources to evaluate the clinical efficacy of oblique lumbar interbody fusion (OLIF) versus minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for treating lumbar degenerative diseases (LDD).
Methods
A systematic search was conducted across various databases, including CNKI, VIP, WANFANG DATA, SinoMed, PubMed, Cochrane Library, Embase, and Web of Science, for clinical comparative studies on OLIF and MIS-TLIF for treating LDD, covering the time frame from the inception of the databases to September 2024. Following PRISMA guidelines, studies were screened, assessed, and data were extracted rigorously. Indicators extracted included operative time, intraoperative blood loss, hospital stay, visual analog scale (VAS) scores, Oswestry Disability Index (ODI), disc height (DH), segmental lordotic angle (SLA), lumbar lordosis angle (LLA), postoperative JOA scores, patient satisfaction, complication rates, and fusion rates. Meta-analysis was performed using Review Manager 5.4 software.
Results
A total of 24 studies were included, comprising 11 randomized controlled trials and 13 retrospective cohort studies. The total population consisted of 1785 patients, with 898 in the OLIF group and 887 in the MIS-TLIF group. The meta-analysis indicated that, compared to the MIS-TLIF group, the OLIF group exhibited significantly lower intraoperative blood loss, shorter hospital stays, improved postoperative DH, shorter operative time, reduced postoperative VAS scores, lower postoperative ODI scores, and improved postoperative SLA and LLA. No significant differences were observed between the groups in postoperative JOA scores, fusion rates, complication rates, or patient satisfaction. The OLIF group exhibited advantages such as lower blood loss, shorter hospital stays, higher postoperative fusion rates, and improved recovery of disc and foraminal heights.
Conclusion
Compared to MIS-TLIF, OLIF is associated with a shorter operative time and less intraoperative blood loss, potentially leading to better relief of leg pain, restoration of DH, and prevention of subsidence. These findings offer valuable insights for clinical practice.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-024-05422-3.
Keywords: Lumbar degenerative disease, Oblique lumbar interbody fusion, Minimally invasive transforaminal lumbar interbody fusion, Meta-analysis
Introduction
Lumbar degenerative disease (LDD) primarily encompasses lumbar spinal stenosis (LSS), lumbar spondylolisthesis (LS), and lumbar instability (LI). These conditions are significant contributors to lower back and leg pain among middle-aged and elderly individuals, with rising incidence rates [1], resulting in substantial burdens on families and society. For patients unresponsive to long-term conservative treatment, surgical intervention is necessary [2]. Lumbar interbody fusion is widely acknowledged as an effective treatment for LDD [3]. With the advancement of minimally invasive techniques, minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has emerged as a common surgical option for LDD due to its benefits, including minimal trauma, reduced blood loss, less posterior column damage, lower infection rates, and quicker recovery [4]. Conversely, oblique lumbar interbody fusion (OLIF) is a newer minimally invasive surgical technique [5]. This technique employs an anatomical corridor between the retroperitoneal vascular sheath and the psoas major muscle, facilitating indirect decompression, reducing muscle injury, decreasing blood loss, shortening operative times, and preserving posterior column structure. These advantages contribute to effective clinical outcomes and increasing adoption [5, 6]. Both surgical approaches can achieve favorable outcomes in treating LDD. However, OLIF is a technically challenging procedure that presents a steeper learning curve than MIS-TLIF. Consequently, it remains uncertain whether the less invasive OLIF results in superior recovery outcomes for patients. This study aims to perform a meta-analysis to inform clinical decision-making regarding surgical techniques.
Methods
Search strategy
We conducted a search across seven databases: PubMed, CNKI (China National Knowledge Infrastructure), Wanfang Data, VIP Database, Sinomed, Embase, and Cochrane Library. Additionally, we expanded our search to include relevant references from identified studies. The search strategy employed a combination of subject headings and free-text keywords. The Chinese search terms were "斜外侧椎间融合术," "微创经椎间孔入路椎间融合术," and "腰椎退行性疾病." The English search terms comprised "Oblique lumbar interbody fusion," "OLIF," "minimally invasive transforaminal lumbar interbody fusion," "MIS-TLIF," "MI-TLIF," "degenerative disease of the lumbar spine," "lumbar degenerative spondylosis," and "spinal fusion." The search timeframe spanned from the establishment of the databases to September 2024.
Inclusion and exclusion criteria
Inclusion Criteria: (1) Studies comparing OLIF and MIS-TLIF for treating lumbar degenerative diseases; (2) Studies providing clinical and radiographic efficacy information, including at least one of the following: operative time, intraoperative blood loss, hospital stay, visual analog scale (VAS), Oswestry Disability Index (ODI), JOA score, complications, disc height, lumbar lordosis, and fusion rate; (3) Studies involving patients aged 18–80 years; (4) Studies published in English or Chinese.
Exclusion Criteria: (1) Literature lacking evidence confirming cases as lumbar degenerative diseases; (2) Poorly designed studies or those with insufficient data; (3) Duplicated literature, reviews, systematic evaluations, animal studies, model studies, case reports, or studies lacking full texts; (4) Studies involving patients with deformities, spinal infections, spinal fractures, benign or malignant tumors, revision surgeries at the same level, or cervical or thoracic lesions; (5) Studies with a follow-up period of less than 6 months or a loss to follow-up rate exceeding 20%.
Quality assessment of the literature
The Cochrane risk assessment tool and the Newcastle–Ottawa Scale (NOS) were utilized to assess the quality of the identified studies. For randomized controlled trials, the Cochrane risk assessment tool was employed, and studies meeting three or more criteria were included in the analysis. For retrospective cohort studies, the NOS was utilized, and studies scoring six stars or higher were included in the analysis.
Data extraction and statistical analysis
Two researchers independently screened the literature and extracted data based on the inclusion and exclusion criteria. Discrepancies were resolved through discussion. A standardized Excel spreadsheet was developed to capture the following information: publication year, first author, study design type, blinding (if applicable), OLIF surgical method, MIS-TLIF surgical method, sample size, sex ratio, age, follow-up duration, postoperative JOA score, ODI score, hospital stay, operative time, fusion rate, patient outcomes, VAS score, segmental lordotic angle (SLA), lumbar lordosis angle (LLA), disc height (DH), postoperative complications, and intraoperative blood loss. Statistical analysis was performed using RevMan Manager 5.4 software provided by the Cochrane Collaboration. When I2 < 50% and the Q test p-value ≥ 0.1, studies were deemed to have no statistically significant heterogeneity, and a fixed-effects model was employed for analysis. When I2 ≥ 50% or the Q test p-value < 0.1, significant heterogeneity was assumed, necessitating sensitivity or subgroup analyses to address this heterogeneity prior to employing a fixed-effects model. For studies where heterogeneity could not be resolved, a random-effects model was utilized.
Results
Literature search results
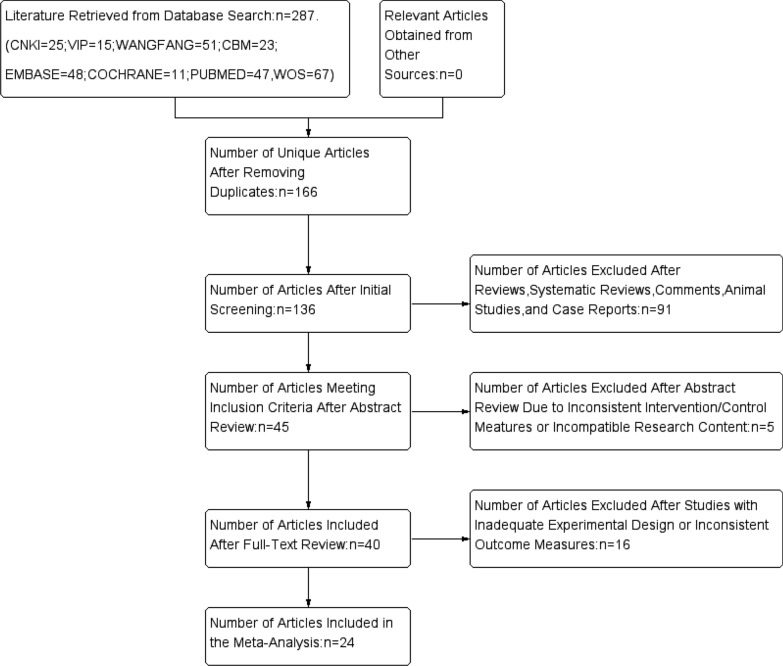
A total of 287 relevant articles were identified. After excluding duplicates and screening titles, abstracts, and full texts, 24 studies were ultimately included in the analysis [8–31]. The detailed screening process is depicted in Fig. 1.
Fig. 1.
Study flow diagram
Basic characteristics and quality assessment of included studies
Of the 24 included studies, 8 were in Chinese [7–14] and 16 in English [15–30], comprising 3 randomized controlled trials [8, 9, 12] and 21 cohort studies [7, 10, 11, 13–30]. A total of 1785 patients were included, with 898 undergoing OLIF and 887 undergoing MIS-TLIF procedures. Basic characteristics of the included studies are summarized in Table 1. The Cochrane risk assessment for bias in randomized controlled trials indicated that 11 study scored 4 points or higher. The NOS quality evaluation indicated that 13 study scored 6 points or higher. (See Supplementary Material 1 for a summary table of basic information on the literature, risk assessment graph, risk assessment summary, and NOS quality assessment table).
Table 1.
Incorporating the meta-analysis results of the included research literature
| Outcome measures | RCSs | RCTs | OLIF cases | MIS-TLIF cases | Heterogeneity test (I2%) | Text model | Combined statistic | Combined statistic value (95%CI) | P-value |
|---|---|---|---|---|---|---|---|---|---|
| Hospital stay [7–10, 12, 14–18, 20, 25–30] | 14 | 3 | 633 | 650 | 82 | Random effects | MD | − 1.91 [− 2.38, − 1.43] | < 0.00001 |
| Introoperative blood loss [7–22, 24–30] | 20 | 3 | 806 | 837 | 99 | Random effects | MD | − 82.69 [− 104.33, − 61.05] | < 0.00001 |
| Surgical time [7–18, 20–30] | 20 | 3 | 862 | 842 | 97 | Random effects | MD | − 21.06 [− 30.99, − 11.33] | < 0.0001 |
| Patient satisfaction [7, 9, 11, 18, 19, 26] | 5 | 1 | 166 | 179 | 0 | Fixed effects | RR | 1.05 [− 0.98, 1.13] | 0.16 |
| Fusion rate [7, 10, 11, 15, 16, 18–20, 24, 26] | 10 | 0 | 265 | 300 | 0 | Fixed effects | RR | 1.06 [1.00, 1.13] | 0.06 |
| Postoperative back pain VAS Scores [7, 10, 11, 13, 14, 16–21, 25–30] | 17 | 0 | 449 | 452 | 0 | Fixed effects | MD | − 0.18 [− 0.22, − 0.13] | < 0.00001 |
| Postoperative leg pain VAS Scores [7, 11, 17–20, 25–30] | 12 | 0 | 392 | 404 | 7 | Fixed effects | MD | − 0.09 [− 0.18, − 0.01] | 0.04 |
| Postoperative ODI Scores [7–10, 12–14, 16–21, 25–30] | 16 | 3 | 687 | 703 | 82 | Random effects | MD | − 1.54 [− 2.44, − 0.64] | 0.0008 |
| Postoperative SLA [12, 20, 25, 26, 29, 30] | 5 | 1 | 178 | 204 | 22 | Fixed effects | MD | 1.37 [0.85, 1.89] | < 0.00001 |
| Postoperative LLA [7, 12, 13, 25, 26, 28–30] | 7 | 1 | 338 | 335 | 38 | Fixed effects | MD | 2.29 [1.63, 2.95] | < 0.00001 |
| Postoperative JOA scores [7, 8, 11, 13, 16, 17] | 5 | 1 | 172 | 180 | 19 | Fixed effects | MD | − 0.03 [− 0.24, − 0.17] | 0.75 |
| Postoperative disc height [7, 10, 12, 15–23, 25, 26, 28, 30] | 15 | 1 | 659 | 648 | 87 | Random effects | MD | 1.22 [0.69, 1.74] | < 0.00001 |
| Postoperative complications [7–10, 12–14, 16–19, 21, 23, 25–30] | 16 | 3 | 758 | 712 | 22 | Fixed effects | RR | 0.95 [0.76, 1.18] | 0.61 |
Conclusion
Perioperative indicators include duration of hospitalization, intraoperative blood loss, and surgery time. Seventeen studies [7–10, 12, 14–18, 20, 25–30] compared the duration of hospitalization between the two surgical approaches. The results demonstrated that the duration of hospitalization in the OLIF group was significantly shorter than that in the MIS-TLIF group, with statistically significant differences (P < 0.05). Twenty-three studies [7–22, 24–30] compared intraoperative blood loss between the two surgical techniques. The analysis indicated that the OLIF group experienced significantly less blood loss than the MIS-TLIF group (P < 0.05). Additionally, twenty-three studies [7–18, 20–30] evaluated the duration of surgery between patients undergoing OLIF and MIS-TLIF. The overall results indicated that the duration of surgery in the OLIF group was significantly shorter than that in the MIS-TLIF group (P < 0.05).
Patient satisfaction was classified into four levels: very satisfied, somewhat satisfied, somewhat dissatisfied, and very dissatisfied. Patients who reported being very satisfied or somewhat satisfied were grouped as satisfied, whereas those who reported being somewhat dissatisfied or very dissatisfied were categorized as dissatisfied. Six studies involving 345 patients [7, 9, 11, 18, 19, 26] compared patient satisfaction between the OLIF and MIS-TLIF groups. The overall results indicated that no significant difference in patient satisfaction between the two groups (P > 0.05).
Ten studies [7, 10, 11, 15, 16, 18–20, 24, 26] reported postoperative fusion rates. The overall results indicated that no significant difference in fusion rates between the two groups (P > 0.05).
Seventeen studies [7, 10, 11, 13, 14, 16–21, 25–30] reported back pain VAS scores, while twelve studies [7, 11, 17–20, 25–30] reported lower limb pain VAS scores. The overall comparison of VAS scores indicated a significant difference between the two groups (P < 0.05), suggesting that the postoperative VAS score in the OLIF group was significantly less than that in the MIS-TLIF group.
Nineteen studies [7–10, 12–14, 16–21, 25–30] reported postoperative ODI scores. The overall results indicated a significant difference between the two groups (P = 0.0008).
Six studies [12, 20, 25, 26, 29, 30] reported improvements in the SLA. The overall comparison of SLA indicated a significant difference between the two groups (P < 0.05), suggesting that the postoperative SLE in the OLIF group was significantly better than that in the MIS-TLIF group.
Eight studies [7, 12, 13, 25, 26, 28–30] reported improvements in the LLA. The overall results indicated that a significant difference between the two groups (P < 0.05), suggesting that the postoperative LLA in the OLIF group was significantly better than that in the MIS-TLIF group.
Six studies [7, 8, 11, 13, 16, 17] reported on the comparison of postoperative JOA scores. The overall results indicated no significant difference between the two groups (P > 0.05).
Sixteen studies [7, 10, 12, 15–23, 25, 26, 28, 30] reported on postoperative disc height. The overall results indicated a significant difference between the two groups (P < 0.05).
Nineteen studies [7–10, 12–14, 16–19, 21, 23, 25–30] reported the occurrence and rates of postoperative complications. The overall results indicated no significant differences between the two groups (Fig. 15, 95% CI 0.76–1.18, P = 0.61), as shown in Table 1 (See Supplementary Material 2 for meta-analysis forest plots, funnel plots, sensitivity analysis and publication bias and the analysis process).
Discussion
Lumbar decompression and fusion surgery is a common procedure for treating lumbar degenerative disease (LDD) [31]. In recent years, minimally invasive lumbar fusion surgery has achieved favorable clinical outcomes while ensuring procedural safety and effectiveness. Advances in surgical techniques and medical instruments have led to methods that minimize trauma and promote faster recovery. In 2002, Foley et al. [4] introduced the minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) technique, which achieves nerve decompression and bone graft fusion using a specialized working channel and corresponding minimally invasive spinal instruments. This approach results in less damage to the posterior structures of the spine and minimizes bleeding; however, it still necessitates retraction of the paravertebral muscles and excision of portions of the facet joints, laminae, and ligaments, which may compromise the stability of the posterior column. This may lead to chronic low back pain and postoperative weakness of the back muscles. Additionally, the confined working space in the channel restricts the use of larger fusion devices, limiting the recovery of intervertebral height and lumbar lordosis, and increasing the risk of nerve injury.
The oblique lumbar interbody fusion (OLIF) surgical technique was officially named by Silvestre et al. in 2012 [5]. This approach utilizes a natural corridor for indirect decompression, preserving the structures of the posterior column and minimizing muscle damage. It facilitates the placement of larger interbody fusion devices, enhancing fusion rates, restoring intervertebral height, and effectively correcting lumbar lordosis, while also promoting faster recovery and confirmed efficacy. However, OLIF also carries risks of vascular and sympathetic nerve injury, and its effectiveness in cases of severe lumbar spondylolisthesis, significant spinal canal stenosis, or large disc herniations remains uncertain [32].
This meta-analysis indicates that, compared to the MIS-TLIF group, the OLIF group experienced shorter surgical times, reduced blood loss, and shorter hospital stays. Of the 24 studies included that reported surgical times, one involved OLIF combined with lateral screw fixation, one was a stand-alone procedure, and the remaining 22 involved OLIF combined with posterior pedicle screw fixation. This suggests that, even with intraoperative position changes, the OLIF group outperformed the MIS-TLIF group in terms of surgical time. This advantage may arise from the smaller operating space in MIS-TLIF, which leads to longer operational times and necessitates multiple fluoroscopic adjustments for positioning. Blood loss is influenced by various factors. Excluding individual patient characteristics, OLIF does not require retraction of the posterior paravertebral muscles. It employs blunt dissection through a natural corridor to access the intervertebral space, directly addresses the endplates, and causes minimal damage to small muscle blood vessels. This results in less blood loss [33], shorter time to ambulation, and faster postoperative recovery.
The OLIF group demonstrated a clear advantage in pain relief and functional improvement. The MIS-TLIF technique necessitates resection of part of the lamina and facet joints [34], while the OLIF technique does not involve such resection. The posterior approach through the muscle interval focuses exclusively on screw placement, leading to less muscle retraction and reduced retraction time, which diminishes surgical trauma for the patient. Consequently, patients in the OLIF group reported lower pain scores and greater postoperative improvements [35]. This suggests that both direct and indirect decompression can effectively relieve nerve compression and alleviate pain. However, OLIF results in less tissue damage during the procedure, preserving the posterior muscles, ligament complex, and bony structures of the lumbar spine. This leads to reduced postoperative trauma and improved functional recovery.
The OLIF group also demonstrated superiority in restoring intervertebral height and improving lumbar lordosis. In contrast to MIS-TLIF, which damages some posterior structures, OLIF effectively expands the intervertebral space via the tension band effect of the posterior longitudinal ligament. Furthermore, OLIF accesses the intervertebral space through a natural corridor, avoiding interference with the spinal canal and nerve roots, which permits a larger operative space. This facilitates the placement of larger interbody fusion devices positioned more anteriorly, which inherently possess a degree of lordotic angle. This effectively distributes load stress on the endplates of the anterior and middle columns, thereby providing improved mechanical stability [36].
Sato et al. [37] conducted a retrospective analysis of 20 patients who underwent OLIF surgery for degenerative lumbar spondylolisthesis, evaluating preoperative and 6-month postoperative MRI and CT images. MRI assessed the cross-sectional area of the spinal canal, while CT evaluated intervertebral disc height and the cross-sectional area of the intervertebral foramen. The results indicated significant postoperative improvements in the cross-sectional area of the spinal canal, intervertebral height, and size of the intervertebral foramen, with a 32% increase in the anteroposterior diameter of the spinal canal and increases of 39% and 21% in the areas of the left and right intervertebral foramina, respectively. Zhu et al. [30] demonstrated through a prospective cohort study that disc height (DH) and lumbar lordosis (LL) in the OLIF group significantly improved at 1 day, 1 month, and 12 months postoperatively.
The results of this study indicate no significant differences in complication rates and fusion rates between the two surgical techniques. Additionally, no notable differences were found in postoperative JOA scores and patient satisfaction between the groups. Common complications in the MIS-TLIF group included dural tears, cerebrospinal fluid leaks, nerve root injuries, and neurological symptoms in the lower limbs. Wong et al. [38] conducted a retrospective analysis of clinical data from 513 patients who underwent MIS-TLIF, reporting an overall complication rate of 15.6%, with dural tears being the most common complication (5.1%); only 0.2% of patients experienced wound infections. These findings are consistent with previous literature, suggesting that nerve root traction during surgery may lead to nerve damage due to local inflammation and adhesions.
In the OLIF group, common complications included hip flexor weakness, anterior-lateral thigh pain and numbness, sympathetic nerve damage, and segmental vascular injuries, consistent with earlier reports [39]. The anterolateral approach necessitates retraction of the psoas major and surrounding tissues, significantly increasing the risk of damage to the lumbar plexus and sympathetic nerves. However, such injuries are usually transient and improve with appropriate postoperative rehabilitation. Both groups reported instances of interbody device subsidence, potentially related to the patients' bone quality; early weight-bearing may also contribute to this subsidence. Neither group reported instances of implant loosening or fracture, indicating that both OLIF and MIS-TLIF provide stable structural support. Generally, the interbody fusion devices used in OLIF are larger than those used in MIS-TLIF, resulting in a greater contact area. Theoretically, the OLIF group should achieve a higher fusion rate. However, in clinical practice, the MIS-TLIF group achieved comparable fusion rates due to the load-sharing effect of the posterior pedicle screw system, leading to satisfactory postoperative recovery and high levels of patient satisfaction. The JOA scores were relatively similar, with no significant differences between the two surgical approaches.
Limitations
This meta-analysis, based on the limited clinical literature available, suggests that OLIF outperforms MIS-TLIF in surgical time, hospital stay, time to ambulation, and intraoperative blood loss. Additionally, OLIF is superior in alleviating pain in patients with LDD, improving functionality, and enhancing intervertebral height and lumbar lordosis; however, there are no significant differences in complication rates and fusion rates between the two groups.
This meta-analysis has several limitations: (1) A total of 13 studies were included, with a lack of randomized controlled trials, resulting in moderate evidence quality; (2) Surgical personnel varied between studies for OLIF and MIS-TLIF, which may impact outcomes; (3) There is a potential for publication bias related to authors' tendencies to publish positive results; (4) Additionally, due to language constraints, this study included only Chinese and English literature, potentially omitting high-quality research in other languages and introducing a risk of language bias.
Supplementary Information
Supplementary Material 1: Summary table of basic information on the literature, risk assessment graph, risk assessment summary, and NOS quality assessment table.
Supplementary Material 2: Meta-analysis forest plots, funnel plots, publication bias and the sensitivity analysis process.
Acknowledgements
We would like to thank all authors of the included studies for providing the data necessary for this meta-analysis.
Author contributions
LD contributed to the study design and data analysis; HX and ZC was responsible for literature search and data extraction; WQ assisted in statistical analysis and manuscript preparation; JH served as the corresponding author, overseeing the research and finalizing the manuscript.
Funding
This study did not receive any funding from external sources.
Availability of data and materials
The data analyzed in this meta-analysis are derived from publicly available databases and published studies, which can be accessed through the following platforms: PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure, Wanfang Data, Sinomed, Chongqing VIP Database, and Web of Science (WOS).
Declarations
Ethics approval and consent to participate
This meta-analysis uses data from published studies; therefore, ethical approval and individual consent to participate were not required. All included studies were conducted in accordance with ethical standards.
Consent for publication
Not applicable, as this meta-analysis does not include individual patient data.
Competing interests
The authors declare that they have no competing interests related to this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Khechen B, Haws BF, Patel DV, Narain AS, Hijji FY, Guntin JA, Cardinal KL, et al. Comparison of postoperative outcomes between primary MIS TLIF and MIS TLIF with revision decompression. (1528-1159 (Electronic)). [DOI] [PubMed]
- 2.Ge DH, Stekas NF, Varlotta CG, Fischer CR, Petrizzo A, Protopsaltis TS, Passias PG, et al. Comparative analysis of two transforaminal lumbar interbody fusion techniques: open TLIF versus Wiltse MIS TLIF (1528-1159 (Electronic)). [DOI] [PubMed]
- 3.Reid P, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. (1547-5646 (Electronic)). [DOI] [PubMed]
- 4.Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. (0069-4827 (Print)). [PubMed]
- 5.Silvestre C, Mac-Thiong J, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. (1976-7846 (Electronic)). [DOI] [PMC free article] [PubMed]
- 6.Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen LL. Analysis of clinical efficacy of OLIF, MIS-TLIF, and Open-TLIF in the treatment of degenerative diseases of a single lumbar segment. Kunming, Yunnan: Kunming University of Science and Technology, 2023.
- 8.Lin J, Hong Y, Chen Z, Lü S. Clinical efficacy of lateral extraforaminal interbody fusion surgery vs. minimally invasive transforaminal interbody fusion surgery for degenerative lumbar scoliosis with lumbar stenosis. Chin J Med Guid. 2023;20(21):97–100. [Google Scholar]
- 9.Liu S. Comparison of the efficacy of lateral extraforaminal lumbar interbody fusion surgery vs. minimally invasive transforaminal lumbar interbody fusion surgery in the treatment of patients with degenerative lumbar spondylolisthesis. Chin J Minkang Med. 2023;35(18):152–5. [Google Scholar]
- 10.Lü F, Tang M, Guo J. Lateral extraforaminal interbody fusion with internal fixation for the treatment of lumbar spinal stenosis. J Neck Low Back Pain. 2021;42(03):326–9. [Google Scholar]
- 11.Pan X, Lu H, Dai J, Chen B, Yu Y, Zhou X. Comparison of the efficacy of lateral extraforaminal lumbar interbody fusion combined with robot-assisted percutaneous internal fixation vs. minimally invasive transforaminal interbody fusion for the initial treatment of single-segment lumbar spondylolisthesis in the same position. Zhejiang Pract Med. 2023;28(04):297–302. [Google Scholar]
- 12.Xu Y, Sang L, Cao Z, Chi K, Chen X, Wu J. Analysis of the efficacy of OLIF and MI-TLIF in the treatment of grade I and II single-segment degenerative lumbar spondylolisthesis. Chin J Trauma Disabil Med. 2022;14:30–4. [Google Scholar]
- 13.Yu Y, Jia Q, Wang L, Guo W, Cheng X. Comparison of the efficacy of two interbody fusion surgeries for the treatment of single-segment degenerative lumbar disease. J Clin Orthop. 2023;26(04):495–9. [Google Scholar]
- 14.Zhang W, Lü L, Wang Z, Lin Z. Clinical efficacy of lateral extraforaminal interbody fusion vs. minimally invasive transforaminal interbody fusion in the treatment of single-segment mild to moderate lumbar spondylolisthesis. J Spin Surg. 2023;21(01):26–31. [Google Scholar]
- 15.Chandra VVR, Prasad BCM, Hanu TG, Kale PG. Comparison between oblique lumbar interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MISTLIF) for lumbar spondylolisthesis. Neurol India. 2022;70(1):127–34. [DOI] [PubMed] [Google Scholar]
- 16.Deng C, Feng H, Ma X, Chen C, Mei J, Sun L. Comparing oblique lumbar interbody fusion with lateral screw fixation and percutaneous endoscopic transforaminal discectomy (OLIF-PETD) and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for the treatment of lumbar disc herniation complicated with lumbar instability. BMC Musculoskelet Disord. 2022;23(1):1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao QY, Wei FL, Li T, Zhu KL, Du MR, Heng W, et al. Oblique lateral interbody fusion vs. minimally invasive transforaminal lumbar interbody fusion for lumbar spinal stenosis: a retrospective cohort study. Front Med (Lausanne). 2022;9:829426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han XG, Tang GQ, Han X, Xing YG, Zhang Q, He D, et al. Comparison of outcomes between robot-assisted minimally invasive transforaminal lumbar interbody fusion and oblique lumbar interbody fusion in single-level lumbar spondylolisthesis. Orthop Surg. 2021;13(7):2093–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.He D, He W, Tian W, Liu B, Liu Y, Sun Y, et al. Clinical and radiographic comparison of oblique lateral lumbar interbody fusion and minimally invasive transforaminal lumbar interbody fusion in patients with L4/5 grade-1 degenerative spondylolisthesis. Orthop Surg. 2023;15(6):1477–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hung SF, Liao JC, Tsai TT, Li YD, Chiu PY, Hsieh MK, et al. Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci Rep. 2021;11(1):12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jun L, Zou T, Wei JJ, Huo T, Min W, Wei C, et al. Comparison of the effects between oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal interbody fusion (MIS-TLIF) in the treatment of adult degenerative lumbar scoliosis. J Orthop. 2024;58:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koike Y, Kotani Y, Terao H, Iwasaki N. Comparison of outcomes of oblique lateral interbody fusion with percutaneous posterior fixation in lateral position and minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis. Asian Spine J. 2021;15(1):97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotani Y, Ikeura A, Tokunaga H, Saito T. Single-level controlled comparison of OLIF51 and percutaneous screw in lateral position versus MIS-TLIF for lumbosacral degenerative disorders: clinical and radiologic study. J Orthop Sci. 2021;26(5):756–64. [DOI] [PubMed] [Google Scholar]
- 24.Kotani Y, Koike Y, Ikeura A, Tokunaga H, Saito T. Clinical and radiologic comparison of anterior–posterior single-position lateral surgery versus MIS-TLIF for degenerative lumbar spondylolisthesis. J Orthop Sci. 2021;26(6):992–8. [DOI] [PubMed] [Google Scholar]
- 25.Li S, Yang Z, Yan W, Da C, Niu W, Qu T. Comparing OLIF combined with lateral screw fixation versus minimally invasive TLIF for treating single-level degenerative lumbar spondylolisthesis: a retrospective cohort study. J Neurol Surg Part A Cent Eur Neurosurg. 2024. 10.1055/a-2297-4416. [DOI] [PubMed]
- 26.Lin GX, Akbary K, Kotheeranurak V, Quillo-Olvera J, Jo HJ, Yang XW, et al. Clinical and radiologic outcomes of direct versus indirect decompression with lumbar interbody fusion: a matched-pair comparison analysis. World Neurosurg. 2018;119:e898–909. [DOI] [PubMed] [Google Scholar]
- 27.Liu L, Xue H, Han Z, Jiang L, Chen L, Wang D. Comparison between OLIF and MISTLIF in degenerative lumbar stenosis: an age-, sex-, and segment-matched cohort study. Sci Rep. 2023;13(1):13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Song Z, Zhang Z, Zheng J, Zhang K, Wang F, Ran M, et al. Short-term and mid-term evaluation of three types of minimally invasive lumbar fusion surgery for treatment of L4/L5 degenerative spondylolisthesis. Sci Rep. 2024;14(1):4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou T, Fan W, Gu Y, Che W, Zhang L, Wang Y. Percutaneous transforaminal endoscopic surgery combined with mini-incision OLIF and anterolateral screws rod fixation vs. MIS-TLIF for surgical treatment of single-level lumbar spondylolisthesis. Front Surg. 2022;9:1049448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhu HF, Fang XQ, Zhao FD, Zhang JF, Zhao X, Hu ZJ, et al. Comparison of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for treatment of lumbar degeneration disease: a prospective cohort study. Spine. 2022;47(6):E233–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiaqi Li, Linfeng W, Xianda G, Baoyang Z, Bingyi Z, Yong S. Research progress on MIS-TLIF in the treatment of lumbar degenerative diseases. Chin J Orthop Surg. 2018;26(07):631–4. [Google Scholar]
- 32.Wu M, Li J, Zhang M, Ding X, Qi D, Li G, et al. Efficacy and radiographic analysis of oblique lumbar interbody fusion for degenerative lumbar spondylolisthesis. (1749-799X (Electronic)). [DOI] [PMC free article] [PubMed]
- 33.Deng D, Wu R, Zhao X, Yang L, Huang X, Liao X. Early efficacy observation of lateral lumbar interbody fusion surgery for the treatment of lumbar degenerative diseases. Chin J Bone Joint Injury. 2018;33(9):966–8. [Google Scholar]
- 34.Kunadt MA-O, Barleben L, Büttner-Janz K. One-level open vs. minimally invasive transforaminal lumbar interbody fusion: a systematic review and advanced meta-analytic assessment of prospective studies with at least two years follow-up. (1432-0932 (Electronic)). [DOI] [PubMed]
- 35.Sun WA-O, Liu HN, Chen MT, Lin YP, Wang HS, Chen BL. Meta-analysis of the clinical efficacy and safety of oblique lateral interbody fusion and transforaminal interbody fusion in the treatment of degenerative lumbar spondylolisthesis. (2058-5241 (Print)). [DOI] [PMC free article] [PubMed]
- 36.Wu R, Deng D, Huang X, Shi C, Zhou Y, Liang D, et al. Comparison of short-term efficacy of OLIF vs. TLIF surgery for the treatment of lumbar spondylolisthesis. Chin J Bone Joint Injury. 2019;34(11):1140–4. [Google Scholar]
- 37.Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. (1432-0932 (Electronic)). [DOI] [PubMed]
- 38.Wong AP, Smith Z, Nixon AT, Lawton CD, Dahdaleh NS, Wong RH, Auffinger B, et al. Intraoperative and perioperative complications in minimally invasive transforaminal lumbar interbody fusion: a review of 513 patients. (1547-5646 (Electronic)). [DOI] [PubMed]
- 39.Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. (1749-799X (Electronic)). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Summary table of basic information on the literature, risk assessment graph, risk assessment summary, and NOS quality assessment table.
Supplementary Material 2: Meta-analysis forest plots, funnel plots, publication bias and the sensitivity analysis process.
Data Availability Statement
The data analyzed in this meta-analysis are derived from publicly available databases and published studies, which can be accessed through the following platforms: PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure, Wanfang Data, Sinomed, Chongqing VIP Database, and Web of Science (WOS).