Abstract
The β domain of streptokinase is required for plasminogen activation and contains a region of sequence diversity associated with infection and disease in group A streptococci. We report that mutagenesis of this polymorphic region does not alter plasminogen activation, which suggests an alternative function for this molecular motif in streptococcal disease.
Streptokinase (SK) is a plasminogen activator secreted by group A, C, and G streptococci. SK contributes to streptococcal virulence by generating plasmin, which leads to bacterial spread from a primary focus of infection by causing fibrinolysis and degradation of extracellular matrix and basement membrane components (6, 16). Plasmin also induces inflammation via complement activation, which may play a role in postinfectious diseases, such as glomerulonephritis (12).
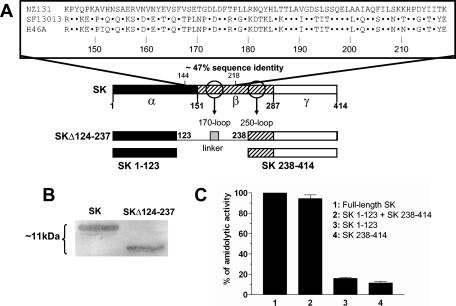
The extent to which SK is involved in streptococcal pathogenesis may depend on structural differences among SKs. SK is a 414-amino-acid (aa) protein composed of three structural domains: α (aa 1 to 150), β (aa 151 to 287), and γ (aa 288 to 414) (19). The highly conserved (≥85% sequence identity) α and γ domains provide most of the contact sites with the plasmin moiety (2, 19) and exhibit a synergistic effect on plasminogen activation (9). The β domain provides no direct contact sites with the plasmin active-site moiety, yet it is required to dock plasminogen via a kringle-binding surface-exposed hairpin loop (termed the 250-loop) between residues 251 and 262 (Fig. 1A) (1, 18). In contrast, a region between amino acids 144 and 218 which spans the second structural loop of the β domain (170-loop) (Fig. 1A) is the major focus of sequence heterogeneity (4), yet its function is unknown. The side chains of nonconserved amino acids within this heterogenous loop are oriented towards the surface, away from the side that faces the plasmin moiety of the activator complex (18).
FIG. 1.
Effect of deletion of the SK polymorphic region on plasminogen activation. (A) Location and alignment of the polymorphic region of the β domain of SK. Domain boundaries and amino acid numbering are based on the crystal structure of SK from S. dysgalactiae subsp. equisimilis H46A (group C) (19); surface-exposed 170- and 250-loops of the β domain are indicated (18). Dots represent identical residues. National Center for Biotechnology Information sequence accession numbers are as follows: for GAS strain NZ131, S04168; for GAS strain SF13013, P10520; and for H46A, CAA51351. (B) Activation of plasminogen on 1% agarose gel overlaid with blots of sodium dodecyl sulfate-polyacrylamide gel electrophoresis-separated full-length SK and SK mutant with aa 124 through 237 deleted (SKΔ124-237) by solid-phase conversion of amidolytic substrate S-2251 according to the method of Kulisek et al. (7). The change in molecular mass is noted on the left. (C) Plasminogen activation by recombinant SK fragments lacking the polymorphic region of SK as measured by release of ρ-nitroanilide from substrate S-2251 after 5 min of incubation. Data were measured in triplicate and results were normalized to percent total activity by full-length SK.
This suggests that SK polymorphism may not be directly engaged in plasminogen binding and activation but instead may determine biological properties related to disease. Previous studies have linked sequence patterns within this polymorphic motif to specific strains of group A streptococci (GAS) that cause acute poststreptococcal glomerulonephritis (APSGN) (10). Also, phylogenetic analysis of β-domain sequences reveals a strong linkage disequilibrium (P ≪ 0.01) with plasminogen-binding group A streptococcal M protein (PAM) in strains that exhibit tissue tropism to the skin (5). Considering the fact that both SK and PAM cooperate to enhance streptococcal virulence through plasminogen activation (15), the specific association between β-domain polymorphism and tissue tropism further supports a role of this motif in disease.
Despite these associations, the biological significance of sequence polymorphism in SK remains unknown. Studies on SK structure and function have focused entirely on therapeutic SK from a nonpathogenic group C streptococcus and have not considered the role of sequence polymorphism of the β domain on plasminogen activation (1, 2, 9, 18, 19). In an attempt to begin addressing the biological importance of structural heterogeneity in SK, we tested whether the removal or exchange of the major polymorphic region in the β domain had any effect on the activation of plasminogen. SK DNA from group A Streptococcus pyogenes strains NZ131 (serotype M49) (3) and SF13013 (serotype M1) (17) and group C Streptococcus dysgalactiae subsp. equisimilis H46A (11) was amplified by PCR, cloned, and expressed in Escherichia coli DH5α as previously described (8). Internal deletion of most of the β domain (aa 124 to 237)-encoding region was achieved by restriction digestion of cloned ska from strain SF13013 with AccI and SplI, followed by ligation with a double-stranded DNA linker encoding an unrelated 14-amino-acid spacer (FADKDDSTHDNDIF). The resulting recombinant protein was tested for plasminogen activation in comparison to that of full-length SK. Proteins (1 μg) were run on sodium dodecyl sulfate-polyacrylamide electrophoresis gels, electroblotted onto nitrocellulose, and overlaid on agarose gels containing Glu-plasminogen (20 μg/ml) and plasmin-specific peptide substrate H-d-Val-Leu-Lys-ρ-nitroanilide S-2251 (100 μg/ml). Amidolytic activity resulting from release of ρ-nitroanilide was detected by the solid-phase method of Kulisek et al. (7) (Fig. 1B). Results indicated that the internal-deletion mutant is capable of forming active complexes with plasminogen. This result was further confirmed by testing whether SK fragments α1-123 (consisting of aa 1 to 123 of the α domain) and βγ238-414, which lack the polymorphic sequence, were capable of activating plasminogen. These fragments were constructed from H46A SK DNA by using original end primers (11) plus 5′-TCAAGGTTGGGTCGGCAAGGTTACCGA (reverse, bp 448 to 471) and 5′-CGTACGATTTTACCAATGGA (forward, bp 772 to 791), respectively. Individual or equimolar mixes of recombinant SK constructs (without glutathione S-transferase fusion) representing SK residues 1 through 123 and 238 through 414 in a volume of 200 μl were incubated with Glu-plasminogen (final concentration, 100 nM) for 5 min at 25°C on 50 mM Tris-Cl, 100 mM NaCl, pH 7.4, in microtiter plates (8). A volume of 20 μl of substrate S-2251 (500 μM) was added, and amidolytic activity was measured by the release of ρ-nitroanilide after 5 min of incubation at 405 nm. Data were measured in triplicate, and results were normalized to percent total activity by full-length SK (Fig. 1C). These results confirm that, while fragments from the α and γ domains (and the kringle-binding loop of the β domain) complement each other to form active complexes with plasminogen as previously described, such activation does not necessitate the 113-residue sequence that includes the polymorphic sequence of SK and the 170-loop of the β domain.
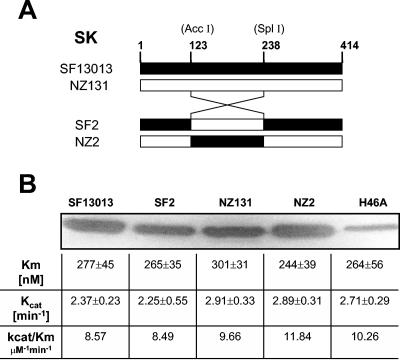
Finally, to test whether the structural composition of the polymorphic region influences the plasminogen activation kinetics of SK, chimeric SKs were constructed by exchange and cross-ligation of AccI/SplI DNA digests encoding the β124-237 fragment between cloned SF13013 and NZ131 ska genes. These genes were chosen because they share <50% sequence identity within this region (4, 10) and, while the NZ131 SK has been specifically linked to streptococcal disease (acute poststreptococcal glomerulonephritis) (12), SK of strain SF13013 has no pathogenic association and shares >90% sequence identity with the polymorphic region of the nonpathogenic SK from group C strain H46A (4). Equimolar SK-plasminogen complexes (final concentration, 40 nM) were formed by preincubation on 50 mM Tris, 100 mM NaCl, pH 7.4, in a 400-μl volume for 5 min on ice, followed by transfer to a 1-cm-path quartz cuvette containing 100 μl S-2251 (500 μM), and monitored at 405 nm for 5 min at 37°C. Initial reaction rates were obtained by plotting the change in A405/min2; the apparent Michaelis-Menten constant and the catalytic rate (kcat) were calculated from data fitted to a hyperbolic curve as previously described (20). Figure 2 shows that native and chimeric SKs convert substrate S-2251 on the solid-phase activation assay. Also, all amidolytic rates were comparable to those of the prototype SK from H46A, indicating that sequence polymorphism in the β domain does not affect the activity of the complex.
FIG. 2.
Effect of exchange of the polymorphic region of SK on plasminogen activation. (A) Exchange of residues 124 through 237 between SKs from GAS strains NZ131 and SF13013. The unique restriction sites used for sequence exchange are indicated in parentheses. (B) Plasminogen activation (solid phase [7] and steady-state kinetics [20]) by wild-type and chimeric (SF2 and NZ2) SKs; H46A is native, commercial SK (Kabi, Sweden). Electrotransfer differences across the blot may account for variations in band intensity.
Collectively, these results demonstrate that the main determinant of structural diversity among SKs that activate human plasminogen is nonessential for forming an active complex with this zymogen. However, its function remains to be determined. It is possible, in accordance with evidence that this polymorphic region is located on a superficial loop in the β domain (18), that this motif may interact with other host or streptococcal components. This would explain the reported associations between SK and APSGN (12) or the observed skin tissue tropism in certain GAS isolates (5). SK from nephritis-associated strain NZ131 exhibits an increased affinity to glomeruli compared to SK from nonpathogenic group C strain H46A (14), and replacement of the SK gene of NZ131 with that of H46A significantly reduces the nephritogenicity of the strain (13). As the β-domain polymorphic sequence is the primary source of sequence divergence between the two SK genes, such heterogeneity may account for the differential affinities to glomerular tissue and thus explain why APSGN develops in some cases. Ongoing studies are aimed at addressing the specific role of the β variable region in streptococcal pathogenesis.
Acknowledgments
We are grateful to Debra E. Bessen for critical review of the manuscript.
S.L. was supported by National Institutes of Health grant R01-AI-053826.
Editor: V. J. DiRita
REFERENCES
- 1.Dhar, J., A. H. Pande, V. Sundram, J. S. Nanda, S. C. Mande, and G. Sahni. 2002. Involvement of a nine-residue loop of streptokinase in the generation of macromolecular substrate specificity by the activator complex through interaction with substrate kringle domains. J. Biol. Chem. 277:13257-13267. [DOI] [PubMed] [Google Scholar]
- 2.Gladysheva, I. P., R. B. Turner, I. Y. Sazonova, L. Liu, and G. L. Reed. 2003. Coevolutionary patterns in plasminogen activation. Proc. Natl. Acad. Sci. USA 100:9168-9172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang, T. T., H. Malke, and J. J. Ferretti. 1989. The streptokinase gene of group A streptococci: cloning, expression in Escherichia coli, and sequence analysis. Mol. Microbiol. 3:197-205. [DOI] [PubMed] [Google Scholar]
- 4.Johnston, K. H., J. E. Chaiban, and R. C. Wheeler. 1991. Analysis of the variable domain of the SK gene from group A streptococci by the polymerase chain reaction, p. 190-194. In P. Cleary (ed.), Streptococcal genetics. American Society for Microbiology, Washington, D.C.
- 5.Kalia, A., and D. E. Bessen. 2004. Natural selection and evolution of streptococcal virulence genes involved in tissue-specific adaptations. J. Bacteriol. 186:110-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khil, J., M. Im, A. Heath, U. Ringdahl, L. Mundada, N. C. Engleberg, and W. P. Fay. 2003. Plasminogen enhances virulence of group A streptococci by streptokinase-dependent and streptokinase-independent mechanisms. J. Infect. Dis. 188:497-505. [DOI] [PubMed] [Google Scholar]
- 7.Kulisek, E. S., S. E. Holm, and K. H. Johnston. 1989. A chromogenic assay for the detection of plasmin generated by plasminogen activator immobilized on nitrocellulose using a para-nitroanilide synthetic peptide substrate. Anal. Biochem. 177:78-84. [DOI] [PubMed] [Google Scholar]
- 8.Lizano, S., and K. H. Johnston. 1995. Streptokinase-mediated plasminogen activation using a recombinant dual affinity fusion protein construct. A novel approach to study bacterial-host interactions. J. Microbiol. Methods 23:261-280. [Google Scholar]
- 9.Loy, J. A., X. Lin, M. Schenone, F. J. Castellino, X. C. Zhang, and J. Tang. 2001. Domain interactions between streptokinase and human plasminogen. Biochemistry 40:14686-14695. [DOI] [PubMed] [Google Scholar]
- 10.Malke, H. 1993. Polymorphism of the streptokinase gene: implications for the pathogenesis of post-streptococcal glomerulonephritis. Zentbl. Bakteriol. 278:246-257. [DOI] [PubMed] [Google Scholar]
- 11.Malke, H., B. Roe, and J. J. Ferretti. 1985. Nucleotide sequence of the streptokinase gene from Streptococcus equisimilis H46A. Gene 34:357-362. [DOI] [PubMed] [Google Scholar]
- 12.Nordstrand, A., M. Norgren, and S. E. Holm. 1999. Pathogenic mechanism of acute post-streptococcal glomerulonephritis. Scand. J. Infect. Dis. 31:523-537. [DOI] [PubMed] [Google Scholar]
- 13.Nordstrand, A., W. M. McShan, J. J. Ferretti, S. E. Holm, and M. Norgren. 2000. Allele substitution of the streptokinase gene reduces the nephritogenic capacity of group A streptococcal strain NZ131. Infect. Immun. 68:1019-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peake, P. W., P. A. Pussell, T. E. Karplus, E. H. Riley, and J. A. Charlesworth. 1991. Post-streptococcal glomerulonephritis: studies on the interaction between nephritis strain-associated protein (NSAP), complement, and the glomerulus. APMIS 99:460-466. [DOI] [PubMed] [Google Scholar]
- 15.Ringdahl, U., M. Svensson, A. C. Wistedt, T. Renne, R. Kellner, W. Muller-Esterl, and U. Sjobring. 1998. Molecular co-operation between protein PAM and streptokinase for plasmin acquisition by Streptococcus pyogenes. J. Biol. Chem. 273:6424-6430. [DOI] [PubMed] [Google Scholar]
- 16.Sun, H., U. Ringdahl, J. W. Homeister, W. P. Fay, N. C. Engleberg, A. Y. Yang, L. S. Rozek, X. Wang, U. Sjőbring, and D. Ginsburg. 2004. Plasminogen is a critical host pathogenicity factor for group A streptococcal infection. Science 305:1283-1286. [DOI] [PubMed] [Google Scholar]
- 17.Walter, F., M. Siegel, and H. Malke. 1989. Nucleotide sequence of the streptokinase gene from a Streptococcus pyogenes type 1 strain. Nucleic Acids Res. 17:1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang, X., J. Tang, B. Hunter, and X. C. Zhang. 1999. Crystal structure of streptokinase beta-domain. FEBS Lett. 459:85-89. [DOI] [PubMed] [Google Scholar]
- 19.Wang, X., X. Lin, J. A. Loy, J. Tang, and X. C. Zhang. 1998. Crystal structure of the catalytic domain of human plasmin complexed with streptokinase. Science 281:1662-1665. [DOI] [PubMed] [Google Scholar]
- 20.Wohl, R. C., L. Summaria, and K. C. Robbins. 1980. Kinetics of activation of human plasminogen by different activator species at pH 7.4 and 37 degrees. J. Biol. Chem. 255:2005-2013. [PubMed] [Google Scholar]