Abstract
Background and Objectives
Congenital choanal atresia is a rare condition that occurs in approximately 1 in 7,000 to 8,000 live births and involves the obstruction of the posterior nasal airway. It may present as either unilateral or bilateral, with bilateral cases being more severe due to the risk of immediate neonatal respiratory distress. Bilateral congenital choanal atresia (BCCA) necessitates prompt medical intervention to prevent cyanosis and significant breathing difficulties. This study focuses on the timing of surgery, the duration of stent use, and postoperative care in patients with bilateral congenital choanal atresia who underwent endoscopic transnasal surgery. Unlike previous studies, this research emphasizes the efficacy of an extended stenting period and introduces novel stenting techniques aimed at reducing restenosis.
Methods
From 2018 to 2021, three patients with BCCA underwent transnasal surgery that included the placement of stents. We retrospectively analyzed their medical records, focusing on the surgical outcomes in relation to the duration of stent placement and postoperative care. A novel approach was adopted, involving the use of customized stent sizes tailored to the specific anatomical factors of each patient, which facilitated improved neochoana maintenance.
Results
The average interval from diagnosis to surgery was 3.6 weeks. Surgery was successful in all cases, and the stent was removed after 6 months. In all patients, stable neochoanae were maintained without significant restenosis. Additionally, we observed that maintaining a stent for a period longer than previously recommended significantly reduced the risk of restenosis compared to the shorter durations used in earlier studies.
Conclusion
Our study suggests that an extended stenting period of 6 months or more is crucial for maintaining long-term patency in patients with BCCA. This approach could lead to a more reliable stenting protocol and improved postoperative care, potentially establishing a new standard for managing BCCA.
Keywords: Choanal atresia, Nasopharynx, Transnasal, Endoscopy, Atresia
INTRODUCTION
Congenital choanal atresia (CCA) is a rare malformation that occurs in approximately 1 in 7,000 to 8,000 live births. It is characterized by the obstruction of the posterior nasal airway [1]. This condition can present either unilaterally or bilaterally. Bilateral cases are more severe, posing an immediate threat of airway obstruction in neonates. While unilateral atresia might remain undetected for months or even years, bilateral congenital choanal atresia (BCCA) can lead to respiratory distress and cyanosis, necessitating prompt intervention. Despite its relatively low incidence, the clinical significance of timely and effective management of BCCA cannot be overstated.
The anatomical obstruction in CCA is categorized into osseous, membranous, or mixed types, with the mixed type being the most prevalent, accounting for approximately 70% of cases [2,3]. From an embryological perspective, the persistence of the nasobuccal membrane is associated with the failure of choanal development, resulting in atresia [3-6]. Diagnosis is generally confirmed through nasal endoscopy and computed tomography (CT) scans, which help to determine the nature and extent of the obstruction.
Various surgical techniques have been developed over time, including transpalatal, transnasal, and transseptal approaches. However, the optimal timing for surgery and stent placement continues to be a subject of debate. Currently, the endoscopic transnasal approach is favored due to its minimally invasive nature, which is particularly advantageous in neonates whose developing palatal bones make more invasive approaches less suitable [7]. Although the transnasal endoscopic approach has gained popularity, preventing restenosis remains a significant challenge in postoperative management. Previous studies have shown varying rates of restenosis, especially when stents were either not used or removed prematurely. Despite this, there is a lack of consensus on the optimal duration for stenting, and research rarely concentrates on customizing stent sizing based on the specific anatomical features of the patient. Most notably, the potential of preoperative imaging to customize stent dimensions to the unique anatomical structures of neonates has not been thoroughly explored.
In this study, we introduce a novel approach to managing BCCA that involves extended stenting periods and customized stent sizing based on preoperative CT scans. This method targets two primary concerns: maintaining long-term choanal patency and decreasing restenosis rates. Additionally, we have refined the postoperative care protocol to address common complications, including stent occlusion and granulation formation. Our findings indicate that a combination of longer stent durations than previously recommended and a tailored approach to stent placement significantly improves surgical outcomes.
This study analyzes three cases of BCCA in newborns and infants, providing insights into a more effective protocol for surgical timing, stent placement, and postoperative management. Our findings suggest that extended stenting periods of 6 months or longer, along with individualized stent sizing, could establish new standards in BCCA management, potentially reducing complications and improving long-term outcomes.
METHODS
Patients
This retrospective study examined the clinical records of three newborns and infants diagnosed with BCCA at Severance Hospital from 2018 to 2021. We collected data on patient characteristics such as age, sex, type of atresia (osseous, membranous, or mixed), accompanying abnormalities (e.g., CHARGE and VACTERL syndromes), and initial symptoms. All patients underwent surgical repair using a transnasal endoscopic approach, followed by postoperative stent placement.
To ensure consistent and comparable outcomes, all patients underwent evaluation using a standardized diagnostic protocol, which included nasal endoscopy and CT scans. These assessments determined the extent of obstruction and provided anatomical considerations for stent placement. In situations where airway maintenance was necessary prior to surgery, either McGovern’s nipple or intubation was employed. This study received approval from the Institutional Review Board of Severance Hospital, Seoul, Korea (IRB No. 4-2024-0466). Informed consent was obtained from all participants, and the study adhered to the principles outlined in the Declaration of Helsinki.
Surgical technique
All three patients underwent endoscopic transnasal surgery, which was performed by the same surgical team using a 2.7-mm rigid endoscope, necessitated by the narrow nasal passages of the neonates. A significant innovation in our approach involved the use of nasal endoscopy and preoperative CT scans to tailor the stent size to each patient’s unique anatomy, a practice not widely adopted in previous studies. This patient-specific strategy facilitated more precise neochoana formation and decreased the risk of restenosis.
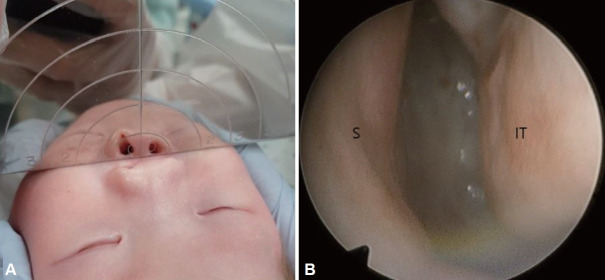
Once the patient was under general anesthesia, we visualized the surgical site using a 0° rigid endoscope. Initially, we perforated the central portion of the atretic plate with a pediatric curette. This was followed by gradual enlargement of the opening using curettes, cup forceps, and microdebriders (Fig. 1). In instances of mixed osseous and membranous atresia, a conservative approach was adopted to preserve mucosal integrity, thereby reducing the risk of postoperative granulation and scarring. To further decrease the likelihood of restenosis, a partial resection of the vomer was performed in all cases to ensure a wider nasal airway. Hemostasis was achieved using Bosmin-soaked cottonoids and bipolar cautery. Our technique differed from previous methods in that it involved more precise intraoperative measurements, which ensured an optimal fit for the stent.
Fig. 1.
Intraoperative endoscopic views of opening of choanal atresia. A: Central perforation of the left obliterated choana by suction tube. B: Make a hole in the lower, inner part of the atretic plate using a curette. C: Opened choanal atresia after laterally drilling the medial pterygoid plates. D: Insert intubation tube (*) as a stent.
Stent placement
A significant aspect of this study was the extended duration of stenting and the use of customized stents. The stents were bilaterally placed using a modified Nelaton catheter technique. Initially, a 2.5-mm endotracheal tube was used, followed by a 3.0-mm tube in one reoperation case. Unlike previous studies that employed stents for shorter durations, the stents in our study were maintained for a minimum of 6 months. The stent size and length were meticulously measured to ensure that the tube extended approximately 5 mm beyond the neochoana into the nasal passage, enhancing stability. Stent insertion was aided by attaching nylon 3-0 threads to a Nelaton catheter. This thread facilitated easier navigation through the narrow nasal passage and was tied off to secure the stents firmly (Fig. 2).
Fig. 2.
Intraoperative views of inserting the stent. A: Nelaton catheter was inserted through the nasal cavity to make the pathway. B: Nelaton tube connected with nylon 3-0 is inserted into the nostril, passed through the neochoana, and then withdrawn through the mouth. C: Removing the catheter and putting an intubation tube to act as a stent for the newly made passage.
Postoperative care and follow-up
Postoperative care was primarily aimed at preventing stent obstruction and the formation of granulation tissue, both of which are common complications noted in prior studies. Caregivers performed daily secretion clearance using narrow suction devices, and patients were advised to apply antibiotic ointment around their nostrils to prevent skin irritation. Antibiotics were prescribed based on body weight for the initial postoperative period, typically lasting 2–3 weeks, and subsequently during episodes of upper respiratory tract infections characterized by symptoms like sputum production. Follow-up endoscopic evaluations were conducted every 1–2 months to assess stent patency and detect any early indications of restenosis.
RESULTS
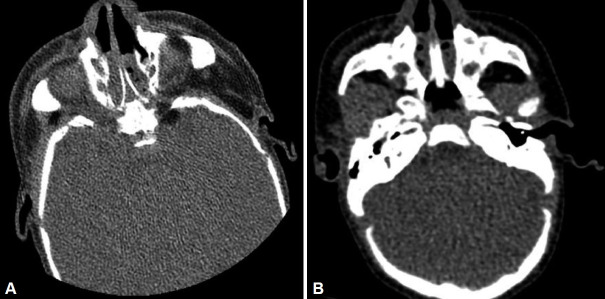
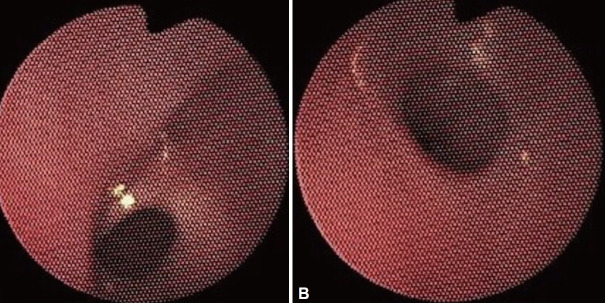
The average time from diagnosis to surgery was 3.6 weeks across the three cases. Case 1 involved a 23-day-old female with no associated syndromes, who underwent surgery 3 weeks after diagnosis. The other two cases—a 1-month-old female with CHARGE syndrome and a 4-month-old male with VACTERL syndrome—underwent surgery approximately 1 month after diagnosis. All cases presented with respiratory distress. Additionally, Case 3 experienced weaning difficulties due to tracheomalacia (Table 1). All patients were diagnosed with either mixed bony-membranous or osseous types of choanal atresia, as confirmed by nasal endoscopy (Fig. 3) and CT (Fig. 4).
Table 1.
Clinical information of patients
| Sex/age | Symptoms | Type | Accompanying disease | Interval* |
|---|---|---|---|---|
| F/23 day | Respiratory distress | Mixed | No | 3 weeks |
| F/1 month | Respiratory distress | Bony | CHARGE syndrome | 1 month |
| M/4 months | Weaning difficulty | Mixed | VACTERL syndrome | 1 month |
interval between final diagnosis (CT) and surgery
Fig. 3.
Preoperative evaluations using mirror (A) and endoscopic view of nasal cavity (B). Endoscopy shows a membranous atretic plate at choana. IT, inferior turbinate; S, septum.
Fig. 4.
Preoperative CT. Axial views of bilateral atretic plate of mixed bony/membranous component (A) and bony component (B) are shown.
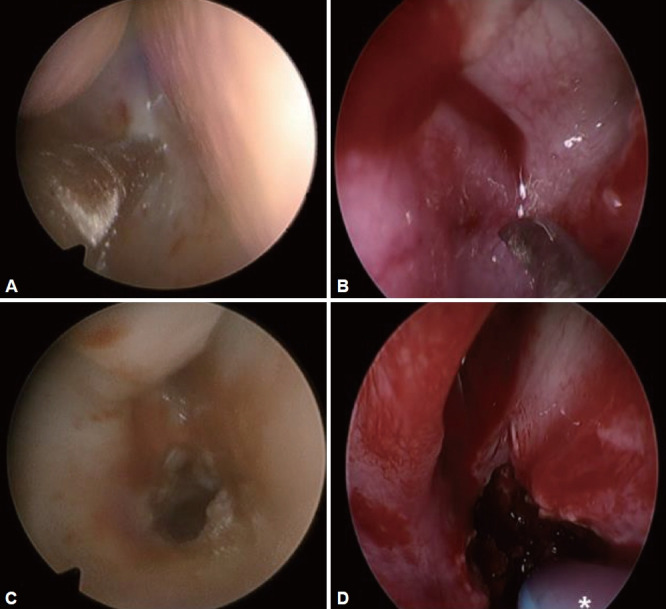
The endoscopic transnasal approach was utilized for all patients, with no intraoperative complications reported. In Case 1, the premature removal of the stent after 2 weeks led to restenosis, requiring a reoperation 2 weeks later. At this time, a larger (3.0 mm) stent was inserted, and it remained in place for 6 months (Table 2). Subsequently, no further restenosis occurred, and the 1-year follow-up indicated stable neochoana (Fig. 5).
Table 2.
Operative outcomes
| Method | Reoperation | Stent | Stenting time |
|---|---|---|---|
| Transnasal | Yes | ET 2.5/3.0 mm | 2 weeks/6 months |
| Transnasal | No | ET 2.5 mm | 6 months |
| Transnasal | No | ET 2.5 mm | 6 months |
ET, endotracheal tube
Fig. 5.
Postoperative endoscopic view at 1 year follow-up in Case 1. A: Left neochoana. B: Right neochoana.
In Cases 2 and 3, the stents remained in place for 6 months without early removal. After more than 3 years of follow-up, both patients maintained stable choanal patency with no signs of restenosis or granulation. Regular postoperative care, which included daily suctioning of secretions and frequent hospital endoscopic evaluations, played a crucial role in achieving these positive outcomes.
Overall, our study found that longer stenting periods (6 months or more) significantly reduced the risk of restenosis compared to cases reported previously, where stents were removed after 4–10 weeks. Additionally, patient-specific stent sizing, based on preoperative nasal endoscopy and CT measurements, contributed to improved outcomes. The precise anatomical fit minimized trauma and ensured stable neochoana formation.
DISCUSSION
Congenital choanal atresia is a relatively rare condition, affecting 1 in 7,000–8,000 newborns. It is more prevalent in females and typically presents as unilateral rather than bilateral [4,5,7-10]. Particularly in bilateral cases, this condition significantly challenges neonatal respiration and feeding [11]. Over the past decades, various surgical techniques have been explored; however, the primary treatment goal remains achieving long-term patency without restenosis. Our study provides new insights into the duration of postoperative stenting and the customization of stent sizing, addressing the ongoing issue of restenosis in neonates and infants.
Our key finding is that stenting for an extended period of at least 6 months significantly reduced restenosis rates, as demonstrated by the stable outcomes in all three cases. This contrasts with previous studies [12,13], which reported restenosis rates as high as 33.6% when stents were removed within 4–10 weeks. The extended duration of stenting allows for more complete healing of the neochoana and minimizes the formation of granulation tissue. Additionally, we adopted a patient-specific approach to stent sizing, utilizing preoperative nasal endoscopy and CT scans to determine the optimal stent dimensions based on individual anatomical features. This method proved to be superior to standard stent placement, as it reduced unnecessary trauma to the nasal passages and contributed to more stable choanal patency. This technique, along with our extended stenting protocol, may establish a new standard for choanal atresia repair, especially in high-risk cases associated with syndromes such as CHARGE and VACTERL [14,15].
The importance of individualized care for neonates is gaining recognition, and our study reinforces this by showing the effectiveness of customized surgical and postoperative strategies. In Case 1, the premature removal of a stent resulted in restenosis, emphasizing the need for a longer stenting protocol despite initial clinical improvements. Following the reoperation and an extended period of stenting, there were no additional complications, which underscores the benefits of this method.
Moreover, our experience indicates that regular postoperative monitoring is crucial for preventing complications such as stent occlusion. This monitoring should include frequent endoscopic evaluations and daily suctioning of secretions. Unlike previous reports where postoperative care was less rigorously managed, our protocol successfully ensured that the stents remained patent throughout the indwelling period, thereby further reducing the risk of complications.
Despite the small sample size of three cases, the consistency of outcomes across all patients supports the robustness of our approach. Future studies involving larger cohorts are necessary to confirm these findings and to further explore potential improvements in stenting materials and techniques.
In conclusion, this study introduces a novel approach to managing bilateral congenital choanal atresia, showing that tailored stent sizing and prolonged stent placement (6 months or longer) significantly lower the risk of restenosis. By customizing the stent size using nasal endoscopy and preoperative CT measurements, and by providing meticulous postoperative care, we achieved stable choanal patency in all patients. Our findings indicate that this method could become the new standard for treating choanal atresia, especially in high-risk neonates with associated syndromes. Future research should aim to validate these findings in larger populations and to further refine stenting techniques.
Acknowledgments
None
Footnotes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Seojin Moon. Data curation: Seojin Moon. Formal analysis: Seojin Moon, Yeonsu Jeong. Funding acquisition: Hyung-Ju Cho. Investigation: Min Seok Rha, Chang-Hoon Kim. Methodology: Seojin Moon. Project administration: Hyung-Ju Cho. Resources: Seojin Moon, Hyung-Ju Cho. Software: Seojin Moon. Supervision: Min Seok Rha, Chang-Hoon Kim, Hyung-Ju Cho. Validation: Seojin Moon. Visualization: Seojin Moon. Writing—original draft: Seojin Moon. Writing—review & editing: Hyung-Ju Cho.
Funding Statement
This study was supported by the “Team Science Award” of Yonsei University College of Medicine (6-2021-0005).
References
- 1.Feuerstein SS, Krespi YP, Sachdev RK. Transnasal correction of choanal atresia. Head Neck Surg. 1980;3(2):97–104. doi: 10.1002/hed.2890030204. [DOI] [PubMed] [Google Scholar]
- 2.Schoem SR. Transnasal endoscopic repair of choanal atresia: why stent? Otolaryngol Head Neck Surg. 2004;131(4):362–6. doi: 10.1016/j.otohns.2004.03.036. [DOI] [PubMed] [Google Scholar]
- 3.Kwong KM. Current updates on choanal atresia. Front Pediatr. 2015;3:52. doi: 10.3389/fped.2015.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hengerer AS, Brickman TM, Jeyakumar A. Choanal atresia: embryologic analysis and evolution of treatment, a 30-year experience. Laryngoscope. 2008;118(5):862–6. doi: 10.1097/MLG.0b013e3181639b91. [DOI] [PubMed] [Google Scholar]
- 5.Ramsden JD, Campisi P, Forte V. Choanal atresia and choanal stenosis. Otolaryngol Clin North Am. 2009;42(2):339–52. doi: 10.1016/j.otc.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Brown OE, Pownell P, Manning SC. Choanal atresia: a new anatomic classification and clinical management applications. Laryngoscope. 1996;106(1 Pt 1):97–101. doi: 10.1097/00005537-199601000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Corrales CE, Koltai PJ. Choanal atresia: current concepts and controversies. Curr Opin Otolaryngol Head Neck Surg. 2009;17(6):466–70. doi: 10.1097/MOO.0b013e328332a4ce. [DOI] [PubMed] [Google Scholar]
- 8.Alvo A, Villarroel G, Sedano C. Neonatal nasal obstruction. Eur Arch Otorhinolaryngol. 2021;278(10):3605–11. doi: 10.1007/s00405-020-06546-y. [DOI] [PubMed] [Google Scholar]
- 9.Rajan R, Tunkel DE. Choanal atresia and other neonatal nasal anomalies. Clin Perinatol. 2018;45(4):751–67. doi: 10.1016/j.clp.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Bedwell J, Shah RK, Bauman N, Zalzal GH, Preciado DA. Balloon dilation for management of choanal atresia and stenosis. Int J Pediatr Otorhinolaryngol. 2011;75(12):1515–8. doi: 10.1016/j.ijporl.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Diop M, Balakrishnan K. Neonatal nasal obstruction. Curr Otorhinolaryngol Rep. 2021;9:389–98. [Google Scholar]
- 12.Gulşen S, Baysal E, Celenk F, Aytaç I, Durucu C, Kanlikama M, et al. Treatment of congenital choanal atresia via transnasal endoscopic method. J Craniofac Surg. 2017;28(2):338–42. doi: 10.1097/SCS.0000000000003247. [DOI] [PubMed] [Google Scholar]
- 13.Albdah A, Alanbari M, Alwadi F. Choanal atresia repair in pediatric patients: is the use of stents recommended? Cureus. 2019;11(3):e4206. doi: 10.7759/cureus.4206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goudy SL. Diagnosis and management of pediatric ENT conditions. Clin Perinatol. 2018;45(4):i. [Google Scholar]
- 15. Mercado P, Eklund JE, Anderson JL. Charge syndrome. In: Lalwani K, Cohen IT, Choi EY, Raman VT, editors. Pediatric anesthesia: a problem- based learning approach. New York: Oxford University Press; 2018. p.19-28. [Google Scholar]