Abstract
Early prediction of patient responses to neoadjuvant chemotherapy (NACT) is essential for the precision treatment of early breast cancer (EBC). Therefore, this study aims to noninvasively and early predict pathological complete response (pCR). We used dynamic ultrasound (US) imaging changes acquired during NACT, along with clinicopathological features, to create a nomogram and construct a machine learning model. This retrospective study included 304 EBC patients recruited from multiple centers. All enrollees had completed NACT regimens, and underwent US examinations at baseline and at each NACT cycle. We subsequently determined that percentage reduction of tumor maximum diameter from baseline to third cycle of NACT serves to independent predictor for pCR, enabling creation of a nomogram ( ). Our predictive accuracy further improved (
). Our predictive accuracy further improved ( ) by combining dynamic US data and clinicopathological features in a machine learning model. Such models may offer a means of accurately predicting NACT responses in this setting, helping to individualize patient therapy. Our study may provide additional insights into the US-based response prediction by focusing on the dynamic changes of the tumor in the early and full NACT cycle.
) by combining dynamic US data and clinicopathological features in a machine learning model. Such models may offer a means of accurately predicting NACT responses in this setting, helping to individualize patient therapy. Our study may provide additional insights into the US-based response prediction by focusing on the dynamic changes of the tumor in the early and full NACT cycle.
Keywords: Breast cancer, Neoadjuvant chemotherapy, Early response prediction, Ultrasound, Nomogram, Support vector machine
Subject terms: Breast cancer, Cancer imaging, Predictive markers
Introduction
Neoadjuvant chemotherapy (NACT) is systemic treatment administered prior to surgery. In patients with early breast cancer (EBC), NACT may mitigate surgical damage and broaden surgical possibilities, improving eligibility for such options as breast-conserving surgery and exempted axillary node dissection1. Individual NACT regimens may also be adjusted in accord with observed patients’ drug sensitivities2. In recent years, indications for NACT have increased substantially3–6, especially in terms of triple-negative breast cancer (TNBC) and HER2-enriched (HER2+) breast cancer7. Patient-level analysis has shown that achieving pathological complete response (pCR) after NACT is associated with increased event-free survival (EFS) and overall survival (OS) compared with patients with non-pCR2,8–10. However, only 5–38% of patients with EBC actually achieve pCR, with the majority having residual disease, meaning failure of NACT2,8,9. It is particularly important that therapeutic responses are accurately evaluated, because ineffective NACT will potentially increase resistant heterogeneous clones, inducing drug resistance and compounding toxic side effects. Treatment strategies should thus be revised timely to reduce unnecessary drug burdens and avoid suboptimal surgical timing. Hence, early and accurate identification of tumor response to NACT is critical for precision treatment decision-making and individualization of surgical procedures.
Mammography, ultrasound (US), and magnetic resonance imaging (MRI) are often regularly undertaken in patients receiving NACT for purpose of therapeutic response monitoring. MRI is currently deemed the most accurate approach to detect tumor response to NACT11–14, but procedural drawbacks (i.e., high cost and discomfort during testing) limit its use in this setting. Mammography is less accurate than US in predicting residual tumor size after NACT15,16. Liquid biopsy, such as circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) may readily reflect the efficacy of NACT in early-stage17,18. Unfortunately, liquid biopsy is clinically problematic, owing to its invasiveness, low content, the insufficient sensitivity of next-generation sequencing technology (NGS), and a lack of adequate medical evidence.
Various benefits of US afforded in non-invasiveness, economy, operability, accessibility, and freedom from radiation makes it the best method for frequent, dynamic monitoring of NACT efficacy. Studies have shown that US is a useful tool for early assessment of pCR after NACT, even though it is less reliable in predicting poor pathological outcomes19. Although some studies have utilized US and MRI parameters acquired before NACT to predict pCR20, tumor characteristics are apt to change during NACT21. It is thus doubtful that a single pre- or post-NACT static state is an accurate representation of patients’ response to NACT. While not entirely foolproof, dynamic changes in tumors during NACT may offer clues for predicting responses to NACT.
In recent years, artificial intelligence has been invoked for tumor epidemiologic analysis, auxiliary tumor imaging diagnostics, and prognostic predictive models. Existing research aimed at machine learning methods has relied on mammography, MRI, and US imaging to predict the efficacy of NACT in patients with breast cancer22–24. Herein, we have constructed a nomogram and a support vector machine (SVM) for early prediction of pCR, based on both clinicopathological characteristics of EBC patients and longitudinal dynamic changes in US images during NACT. Our intent was to help clinicians make critical treatment decisions and formulate appropriate surgical plans.
Methods
Patient population
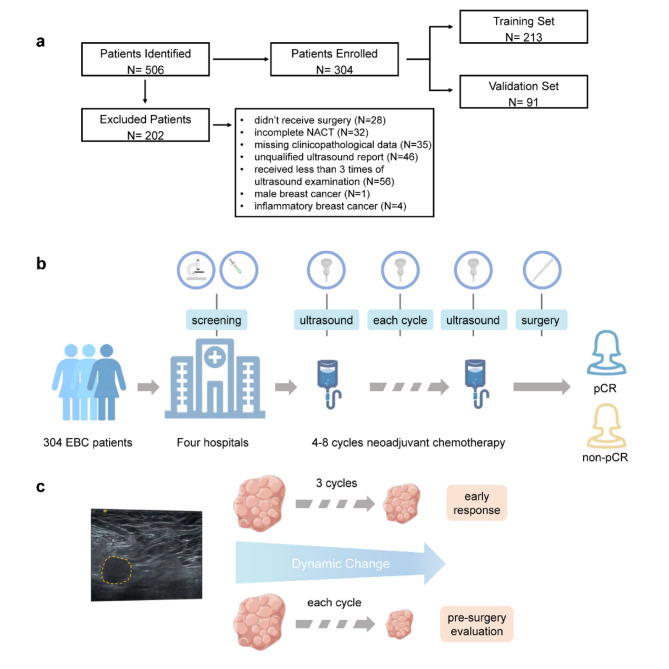
This multicenter retrospective study enrolled 506 patients with EBC from four medical centers between October 2013 and December 2021. All had been diagnosed with primary breast cancer and treated with NACT. We excluded 202 of these candidates on the following grounds: no surgery performed ( ), incomplete NACT (
), incomplete NACT ( ), missing clinicopathological data (
), missing clinicopathological data ( ), unqualified US report (
), unqualified US report ( ), less than three US examinations (
), less than three US examinations ( ), male breast cancer (
), male breast cancer ( ), and inflammatory breast cancer (
), and inflammatory breast cancer ( ). Ultimately, 304 patients remained for randomization to training and validation sets at a 7:3 ratio. The study design is shown in Fig. 1. Figure 1 was created by Figdraw (https://www.figdraw.com/static/index.html).
). Ultimately, 304 patients remained for randomization to training and validation sets at a 7:3 ratio. The study design is shown in Fig. 1. Figure 1 was created by Figdraw (https://www.figdraw.com/static/index.html).
Fig. 1.
Research process (Created by Figdraw). (a) Study enrollment process, randomly assigning 304 patients to a training or validation set at 7:3 ratio. (b) Each of the 304 patients selected received 4–8 cycles of neoadjuvant chemotherapy (NACT), once diagnosed with early breast cancer (EBC) by core needle biopsy. Ultrasound (US) examinations were done before NACT and at each cycle of NACT. Upon completing NACT, surgery was performed, and postoperative pathological test was used to determine the pathological response. (c) Our research objective was two-pronged. The first part was to predict early NACT response through dynamic change in tumor during first three treatment cycles, to gauge forthcoming treatment needs. The second was predicting pCR preoperatively, based on dynamic tumor changes at each cycle of NACT, to formulate operative strategies.
The study was approved by the ethics committee of Second Affiliated Hospital of Dalian Medical University. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent has been obtained from patients.
Clinical and pathological evaluations
We collected patient clinical characteristics at baseline (before NACT), including age and clinical tumor/nodal stage. Data on hormone receptors (estrogen receptor, ER; progesterone receptor, PR) and other markers (HER2 and Ki67) were obtained from pre-treatment core needle biopsies. Hormone receptor positivity (either ER+ or PR+) was defined as ≥ 1% of tumor cells staining positively in immunohistochemistry (IHC)25. Tumors with immunohistochemical HER2 3+ or HER2 2+ with HER2 gene amplification confirmed by fluorescent in situ hybridization (FISH) were considered HER2+26. The Ki67 index was denoted by percentage of stained cells27. In accord with the above criteria, we classified tumors as HR+/HER2+, HR−/HER2+, HR+/HER2−, or HR−/HER2−.
Neoadjuvant chemotherapy and pathological response
Each patient was treated with 4–8 cycles of NACT, based on anthracycline (A) and/or taxanes (T). Some patients received carboplatin (Cb) as well. The patients with HER2+ tumors were treated with trastuzumab or trastuzumab plus pertuzumab in conjunction with chemotherapy.
Biopsy specimens acquired before NACT and surgical specimens assessed after NACT were used to evaluate pathological response, applying the Miller-Payne system28. Pathological complete response (pCR) was indicated by the absence of invasive tumor cells in both breast and axillary lymph nodes, and ductal carcinoma in situ could be present (ypT0/is ypN0)29–31.
Ultrasound examinations
All US scans of breast were performed by three experienced radiologists independently. All radiologists were required to undergo a unified training in operating technology according to the guidelines of the American College of Radiology (BI-RADS lexicon) and the expert consensus of the National Ultrasound Quality Control Centre. The largest radial section of the lesion (longitudinal section) and the largest section vertical to it (transverse section) were required to be obtained. Two maximum diameters vertical to each other were measured in the longitudinal section of the lesion, and then the transverse diameter was measured in the transverse section. The maximum tumor diameter was selected from the two sections. Volumes were calculated from recorded three maximum diameters. Patients routinely underwent US examinations at baseline and at every cycle of NACT to determine maximum tumor diameters and volumes over time. To measure early dynamic changes of tumors, we defined  as
as  , where
, where  and
and  were maximum tumor diameters at baseline and at NACT cycle x, respectively.
were maximum tumor diameters at baseline and at NACT cycle x, respectively.
Nomogram development
Logistic regression was done to identify associations of clinical, pathological, and US parameters with pCR. We reserved variables of significance (p < 0.05) in univariate analysis for multivariate analysis, determining independent predictive factors of pCR. The identified factors provided a basis for nomogram construction. Predictive accuracy of  was assessed by the receiver operating characteristic (ROC) curve, deriving sensitivity and specificity from the area under the curve (AUC). Values of AUC (range, 0–1) indicate perfect concordance at 1, no better than chance at 0.5, and discordance at 032. Internal validation of the nomogram was performed by a calibration method and by the AUC in the training set. External validation was conferred by performing AUC in the validation set. The calibration curve, assessed by Hosmer–Lemeshow goodness-of-fit test (p > 0.05 indicating good fit), and the decision curve analysis (DCA) served to evaluate predictive model utility. The final nomogram was conducted using R software (v4.2.1; The R Foundation for Statistical Computing, Vienna, Austria).
was assessed by the receiver operating characteristic (ROC) curve, deriving sensitivity and specificity from the area under the curve (AUC). Values of AUC (range, 0–1) indicate perfect concordance at 1, no better than chance at 0.5, and discordance at 032. Internal validation of the nomogram was performed by a calibration method and by the AUC in the training set. External validation was conferred by performing AUC in the validation set. The calibration curve, assessed by Hosmer–Lemeshow goodness-of-fit test (p > 0.05 indicating good fit), and the decision curve analysis (DCA) served to evaluate predictive model utility. The final nomogram was conducted using R software (v4.2.1; The R Foundation for Statistical Computing, Vienna, Austria).
Machine learning model
The samples were randomly divided into a training set and a validation set in a 7:3 ratio. Various parameters, including ER, PR, HER2, and Ki67 status; NACT regimen; and maximum tumor diameters/volumes by cycle enabled the construction of our machine learning model. Data were preprocessed in three steps, the first being observed dynamic tumor changes. For this, we excluded any samplings examined less than three times. At the second step, data were standardized to eliminate differences between features. Considering the imbalance of data types, the pCR sampling was extended as part of the training set for step three, using the Synthetic Minority Over-sampling Technique (SMOTE) method. We then constructed the pCR prediction model using the support vector machine (SVM). SVM is a binary classification model, transforming classification issues into convex quadratic programming for problem solving. The radial basis function (RBF) was used as the kernel in SVM. To avoid overfitting, we conducted fivefold cross-validation when selecting parameters for RBFs. This model was evaluated by precision, recall, and F1-score, all obtained from the confusion matrix. To assess the predictive performance of the model, ROC curves and AUC were calculated. The process was conducted using Python (v3.8.12; Python Software Foundation).
Statistical analysis
We compared patient characteristics of the training and validation sets. Mann–Whitney U test was applied to compare  between pCR and non-pCR patients at different NACT cycles. The Hosmer–Lemeshow test was used to assess the fitness of the nomogram. All statistical tests were two-sided, driven by standard softwares (SPSS v25.0 [IBM Corp, Armonk, NY, USA] and R v4.2.1).
between pCR and non-pCR patients at different NACT cycles. The Hosmer–Lemeshow test was used to assess the fitness of the nomogram. All statistical tests were two-sided, driven by standard softwares (SPSS v25.0 [IBM Corp, Armonk, NY, USA] and R v4.2.1).
Results
Patient characteristics
We randomly assigned 304 EBC patients to a training ( ) or a validation (
) or a validation ( ) set. Among all enrollees, 85 (28.0%) achieved pCR. Clinical characteristics of the patient population are summarized in Table 1. More than half (53.0%) of those achieving pCR received anthracycline and taxane agents as chemotherapy, and HER2+ tumors were more often associated with pCR (HR+/HER2+, 28.2%; HR−/HER2+, 33.0%). The pCR rate in HR+/HER2− subtype was 28.2%. Patients with HR−/HER2− subtype were least likely (10.6%) to achieve pCR.
) set. Among all enrollees, 85 (28.0%) achieved pCR. Clinical characteristics of the patient population are summarized in Table 1. More than half (53.0%) of those achieving pCR received anthracycline and taxane agents as chemotherapy, and HER2+ tumors were more often associated with pCR (HR+/HER2+, 28.2%; HR−/HER2+, 33.0%). The pCR rate in HR+/HER2− subtype was 28.2%. Patients with HR−/HER2− subtype were least likely (10.6%) to achieve pCR.
Table 1.
Clinicopathological characteristics of enrolled patients with EBC.
| Characteristic | Overall (304) | Training set (213) | Validation set (91) | |||
|---|---|---|---|---|---|---|
| pCR (85) | Non-pCR (219) | pCR (52) | Non-pCR (161) | pCR (33) | Non-pCR (58) | |
| Age (year), (n, %) | ||||||
| ≤ 50 | 46 (54.1) | 102 (46.6) | 27 (51.9) | 71 (44.1) | 19 (57.6) | 31 (53.4) |
| > 50 | 39 (45.9) | 117 (53.4) | 25 (48.1) | 90 (55.9) | 14 (42.4) | 27 (46.6) |
| cT stage, (n, %) | ||||||
| T1 | 15 (17.7) | 9 (4.1) | 8 (15.4) | 7 (4.3) | 7 (21.2) | 2 (3.4) |
| T2 | 58 (68.2) | 156 (71.2) | 34 (65.4) | 112 (69.6) | 24 (72.7) | 44 (75.9) |
| T3 | 12 (14.1) | 53 (24.2) | 10 (19.2) | 41 (25.5) | 2 (6.1) | 12 (20.7) |
| T4 | 0 (0) | 1 (0.5) | 0 (0) | 1 (0.6) | 0 (0) | 0 (0) |
| cN stage, (n, %) | ||||||
| N0 | 6 (7.1) | 40 (18.2) | 3 (5.8) | 27 (16.8) | 3 (9.1) | 13 (22.4) |
| N1 | 70 (82.4) | 155 (70.8) | 42 (80.8) | 116 (72.1) | 28 (84.8) | 39 (67.3) |
| N2 | 2 (2.3) | 3 (1.4) | 2 (3.8) | 2 (1.2) | 0 (0) | 1 (1.7) |
| N3 | 7 (8.2) | 21 (9.6) | 5 (9.6) | 16 (9.9) | 2 (6.1) | 5 (8.6) |
| T0 (cm), M (P25, P75) | 3.5 (2.7, 4.84) | 3.5 (2.7, 4.82) | 3.735 (2.7, 5.0) | 3.785 (2.7, 5.0) | 3.2 (2.5, 4.4) | 3.2 (2.53, 4.4) |
| ΔT3 (%), M (P25, P75) | 0.26 (0.10, 0.45) | 0.26 (0.09, 0.45) | 0.26 (0.07, 0.46) | 0.26 (0.07, 0.46) | 0.27 (0.11, 0.44) | 0.26 (0.11, 0.43) |
| ER status, (n, %) | ||||||
| Positive | 37 (43.5) | 164 (74.9) | 26 (50.0) | 122 (75.8) | 11 (33.3) | 42 (72.4) |
| Negative | 48 (56.5) | 55 (25.1) | 26 (50.0) | 39 (24.2) | 22 (66.7) | 16 (27.6) |
| PR status, (n, %) | ||||||
| Positive | 42 (49.4) | 156 (71.2) | 28 (53.8) | 118 (73.3) | 14 (42.4) | 38 (65.5) |
| Negative | 43 (50.6) | 63 (28.8) | 24 (46.2) | 43 (26.7) | 19 (57.6) | 20 (34.5) |
| HER2 status, (n, %) | ||||||
| Positive | 52 (61.2) | 60 (27.4) | 29 (55.8) | 48 (29.8) | 23 (69.7) | 12 (20.7) |
| Negative | 33 (38.8) | 159 (72.6) | 23 (44.2) | 113 (70.2) | 10 (30.3) | 46 (79.3) |
| Ki67 expression (%), M (P25, P75) | 0.3 (0.2, 0.5) | 0.3 (0.2, 0.5) | 0.3 (0.2, 0.5) | 0.3 (0.2, 0.5) | 0.3 (0.2, 0.45) | 0.3 (0.2, 0.5) |
| NACT regimen, (n, %) | ||||||
| Anthracycline-based | 4 (4.7) | 20 (9.1) | 3 (5.8) | 15 (9.3) | 1 (3.0) | 5 (8.6) |
| Taxane-based | 20 (23.5) | 20 (9.1) | 8 (15.4) | 15 (9.3) | 12 (36.4) | 5 (8.6) |
| Anthracycline + Taxane | 45 (53.0) | 170 (77.7) | 29 (55.7) | 123 (76.4) | 16 (48.5) | 47 (81.1) |
| Carboplatin-based | 16 (18.8) | 9 (4.1) | 12 (23.1) | 8 (5.0) | 4 (12.1) | 1 (1.7) |
| Molecular subtype | ||||||
| HR+/HER2+ | 24 (28.2) | 42 (19.2) | 14 (26.9) | 37 (23.0) | 10 (30.3) | 5 (8.6) |
| HR−/HER2+ | 28 (33.0) | 18 (8.2) | 15 (28.9) | 11 (6.8) | 13 (39.4) | 7 (12.1) |
| HR+/HER2− | 24 (28.2) | 134 (61.2) | 18 (34.6) | 96 (59.6) | 6 (18.2) | 38 (65.5) |
| HR−/HER2− | 9 (10.6) | 25 (11.4) | 5 (9.6) | 17 (10.6) | 4 (12.1) | 8 (13.8) |
cT stage clinical tumor stage, cN stage clinical nodal stage,  the maximum tumor diameter at baseline,
the maximum tumor diameter at baseline,  percentage reduction of tumor maximum diameter from baseline to third cycle of NACT, ER estrogen receptor, PR progesterone receptor, HR hormone receptor, HER2 human epidermal growth factor receptor 2, Ki67 Ki67 proliferative index, NACT neoadjuvant chemotherapy, pCR pathological complete response.
percentage reduction of tumor maximum diameter from baseline to third cycle of NACT, ER estrogen receptor, PR progesterone receptor, HR hormone receptor, HER2 human epidermal growth factor receptor 2, Ki67 Ki67 proliferative index, NACT neoadjuvant chemotherapy, pCR pathological complete response.
Predictors of pathological complete response (pCR)
Logistic regression was performed to explore predictors of pCR, analyzing potential relations with patient age,  ,
,  , ER, PR, HER2, Ki67, and NACT regimen (Table 2). In univariate analysis, smaller
, ER, PR, HER2, Ki67, and NACT regimen (Table 2). In univariate analysis, smaller  values were associated with higher probability of pCR (odds ratio
values were associated with higher probability of pCR (odds ratio  ; 95% confidence interval [CI], 0.711–0.965;
; 95% confidence interval [CI], 0.711–0.965;  ). Likewise, HR (ER/PR) status, HER2 status, and NACT regimen (all p < 0.001), as well as Ki67 expression level (
). Likewise, HR (ER/PR) status, HER2 status, and NACT regimen (all p < 0.001), as well as Ki67 expression level ( ), emerged as significant predictors of pCR. To determine the feasibility of predicting therapeutic response through early tumor dynamic changes, we analyzed percentages of change in
), emerged as significant predictors of pCR. To determine the feasibility of predicting therapeutic response through early tumor dynamic changes, we analyzed percentages of change in  (as shown by US) relative to baseline values across initial four NACT cycles. In Fig. 2a,
(as shown by US) relative to baseline values across initial four NACT cycles. In Fig. 2a,  values at respective NACT cycles are shown to compare between pCR and non-pCR. Significant differences were apparent in cycles 2–4. Furthermore,
values at respective NACT cycles are shown to compare between pCR and non-pCR. Significant differences were apparent in cycles 2–4. Furthermore,  was confirmed as a significant predictor of pCR. Despite the importance of early response prediction, the earliest values were not the best. Figure 2b demonstrates that
was confirmed as a significant predictor of pCR. Despite the importance of early response prediction, the earliest values were not the best. Figure 2b demonstrates that  and
and  surpassed
surpassed  and
and  in terms of capacity to predict pCR, which was shown by AUC. Additionally, the ROC shows that
in terms of capacity to predict pCR, which was shown by AUC. Additionally, the ROC shows that  and
and  had similar AUC. Due to the aim of early response evaluation, we subsequently selected change in maximum tumor diameter at third cycle as the preferred metric, denoted as
had similar AUC. Due to the aim of early response evaluation, we subsequently selected change in maximum tumor diameter at third cycle as the preferred metric, denoted as  (
( ). ROC analysis yielded a cut-off value of 29.9% for
). ROC analysis yielded a cut-off value of 29.9% for  .
.
Table 2.
Univariate and multivariate analyses of pCR.
| Characteristic | Univariate analysis | Multivariable analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Age (year) | ||||||
| > 50 | 1 | |||||
| ≤ 50 | 1.353 | 0.819–2.236 | 0.238 | |||
| T0 | 0.828 | 0.711–0.965 | 0.016 | 0.706 | 0.582–0.857 | < 0.001 |
| ΔT3 | 9.518 | 3.327–27.232 | < 0.001 | 10.795 | 3.077–37.880 | < 0.001 |
| ER status | ||||||
| Negative | 1 | |||||
| Positive | 0.259 | 0.153–0.438 | < 0.001 | 0.417 | 0.192–0.907 | 0.027 |
| PR status | ||||||
| Negative | 1 | 1 | ||||
| Positive | 0.394 | 0.235–0.661 | < 0.001 | 0.946 | 0.440–2.035 | 0.887 |
| HER2 status | ||||||
| Negative | 1 | 1 | ||||
| Positive | 4.176 | 2.464–7.078 | < 0.001 | 1.641 | 0.797–3.375 | 0.179 |
| Ki67 expression | 5.573 | 1.828–16.988 | 0.003 | 4.843 | 1.202–19.519 | 0.027 |
| NACT regimen | < 0.001 | |||||
| Anthracycline-based | 1 | 1 | ||||
| Taxane-based | 5.000 | 1.448–17.271 | 0.011 | 3.083 | 0.712–13.342 | 0.132 |
| Anthracycline + Taxane | 1.324 | 0.431–4.067 | 0.625 | 1.376 | 0.391–4.847 | 0.619 |
| Carboplatin-based | 8.889 | 2.307–34.248 | 0.001 | 7.928 | 1.567–40.112 | 0.012 |
OR odds ratio, CI confidence interval,  the maximum tumor diameter at baseline,
the maximum tumor diameter at baseline,  percentage reduction of tumor maximum diameter from baseline to third cycle of NACT, ER estrogen receptor, PR progesterone receptor, HR hormone receptor, HER2 human epidermal growth factor receptor 2, Ki67 Ki67 proliferative index, NACT neoadjuvant chemotherapy, pCR pathological complete response.
percentage reduction of tumor maximum diameter from baseline to third cycle of NACT, ER estrogen receptor, PR progesterone receptor, HR hormone receptor, HER2 human epidermal growth factor receptor 2, Ki67 Ki67 proliferative index, NACT neoadjuvant chemotherapy, pCR pathological complete response.
p < 0.05 was considered statistically significant.
Fig. 2.
The comparison of  ,
,  ,
,  , and
, and  for predicting the probability of pCR. (a) The comparison of
for predicting the probability of pCR. (a) The comparison of  between pCR and non-pCR patients at first four cycles of NACT. Significant differences were apparent in cycles 2–4, except for cycle 1. (b) The receiver operating characteristic (ROC) curves of
between pCR and non-pCR patients at first four cycles of NACT. Significant differences were apparent in cycles 2–4, except for cycle 1. (b) The receiver operating characteristic (ROC) curves of  ,
,  ,
,  , and
, and  for predicting the probability of pCR.
for predicting the probability of pCR.  and
and  had better ability to predict pCR compared to
had better ability to predict pCR compared to  and
and  . To measure the early dynamic changes of the tumor, we defined
. To measure the early dynamic changes of the tumor, we defined  as
as  .
.  refers to the maximum diameter of the tumor at the baseline.
refers to the maximum diameter of the tumor at the baseline.  refers to the maximum diameter of the tumor at different cycles of NACT.
refers to the maximum diameter of the tumor at different cycles of NACT.  refers to the cycle of NACT. p < 0.05 was considered statistically significant.
refers to the cycle of NACT. p < 0.05 was considered statistically significant.
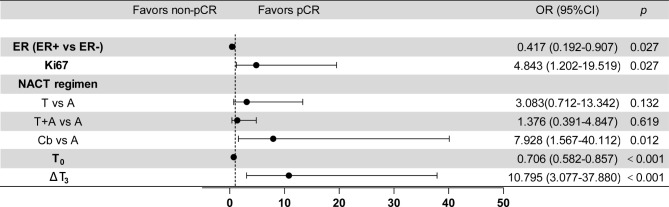
Multivariate logistic regression analysis was next carried out in search of independent predictors for pCR. The forest plot is shown as Fig. 3. Relative to ER+ patients, those with ER- status were more likely to achieve pCR ( ,
,  ;
;  ). In addition,
). In addition,  (
( ,
,  ;
;  ) and
) and  (
( ) displayed significant associations with pCR, as did Ki67 expression (
) displayed significant associations with pCR, as did Ki67 expression ( ,
,  ;
;  ). Once adjusted for ER status, Ki67 expression,
). Once adjusted for ER status, Ki67 expression,  , and
, and  , a significantly higher rate of pCR was also evident after carboplatin-based (vs anthracycline-based) treatment (
, a significantly higher rate of pCR was also evident after carboplatin-based (vs anthracycline-based) treatment ( ,
,  ;
;  ). Although significance was not reached, patients receiving taxane-based (
). Although significance was not reached, patients receiving taxane-based ( ) or anthracycline plus taxane-based (
) or anthracycline plus taxane-based ( ) regimen seemed to have a higher odds ratio than those administered anthracycline-based treatment (
) regimen seemed to have a higher odds ratio than those administered anthracycline-based treatment ( ).
).
Fig. 3.
Forest plot of variables for prediction of pCR. ER, estrogen receptor status; Ki67, Ki67 proliferative index;  , the maximum tumor diameter at baseline;
, the maximum tumor diameter at baseline;  , percentage reduction of tumor maximum diameter from baseline to third cycle of NACT; NACT regimen, T, Taxanes; A, Anthracycline; Cb, carboplatin; pCR, pathological complete response. p < 0.05 was considered statistically significant.
, percentage reduction of tumor maximum diameter from baseline to third cycle of NACT; NACT regimen, T, Taxanes; A, Anthracycline; Cb, carboplatin; pCR, pathological complete response. p < 0.05 was considered statistically significant.
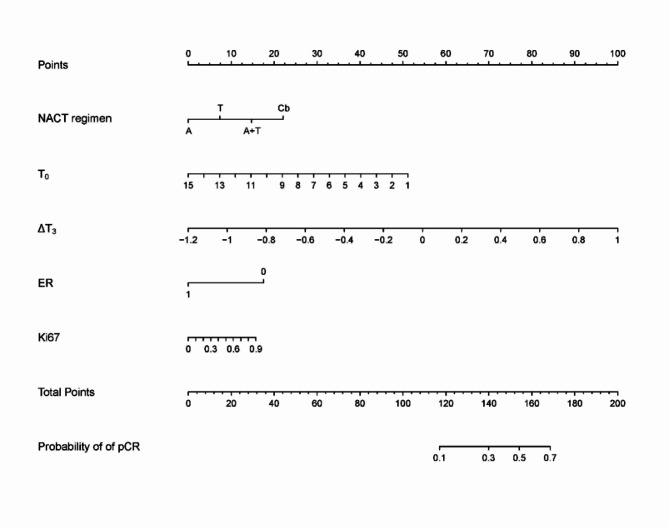
Nomogram construction and validation
Our nomogram incorporated significant predictors of pCR ( , ER status, Ki67 expression, NACT regimen) established by multivariate logistic regression analysis, with the addition of
, ER status, Ki67 expression, NACT regimen) established by multivariate logistic regression analysis, with the addition of  (Fig. 4). Each variable was assigned a point value (top scale), the sum of which reflected pCR probability (bottom scale). Nomogram validation by ROC analysis generated AUC values of 0.75 in both training and validation sets (training set, 95% CI: 0.67–0.83; validation set, 95% CI: 0.64–0.86), suggesting good predictive efficiency (Fig. 5a,b). The calibration curve for pCR probability also showed good agreement between predicted and observed results (Fig. 5c). The Hosmer–Lemeshow test indicated no significant deviation of obtained results from an ideal fitting (
(Fig. 4). Each variable was assigned a point value (top scale), the sum of which reflected pCR probability (bottom scale). Nomogram validation by ROC analysis generated AUC values of 0.75 in both training and validation sets (training set, 95% CI: 0.67–0.83; validation set, 95% CI: 0.64–0.86), suggesting good predictive efficiency (Fig. 5a,b). The calibration curve for pCR probability also showed good agreement between predicted and observed results (Fig. 5c). The Hosmer–Lemeshow test indicated no significant deviation of obtained results from an ideal fitting ( ).
).
Fig. 4.
Nomogram for predicting the probability of pCR. Nomogram for predicting the probability of pCR. Variables including NACT regimen,  ,
,  , ER status, and Ki67 proliferative index. pCR, pathological complete response; NACT regimen, T, Taxanes; A, Anthracycline; Cb, carboplatin;
, ER status, and Ki67 proliferative index. pCR, pathological complete response; NACT regimen, T, Taxanes; A, Anthracycline; Cb, carboplatin;  , the maximum tumor diameter at baseline;
, the maximum tumor diameter at baseline;  , percentage reduction of tumor maximum diameter from baseline to third cycle of NACT; ER, estrogen receptor status; Ki67, Ki67 proliferative index.
, percentage reduction of tumor maximum diameter from baseline to third cycle of NACT; ER, estrogen receptor status; Ki67, Ki67 proliferative index.
Fig. 5.
The receiver operating characteristic (ROC) curves and calibration curve of a nomogram. (a) The ROC curves for predicting the probability of pCR in the training set. (b) The ROC curves for predicting the probability of pCR in the validation set. (c) The calibration curve of the nomogram. The dashed line named Ideal presents perfect performance, the other dashed line named Apparent presents the actual performance of the nomogram, and the solid line named Bias-corrected presents the actual performance of the nomogram after bias-correction.
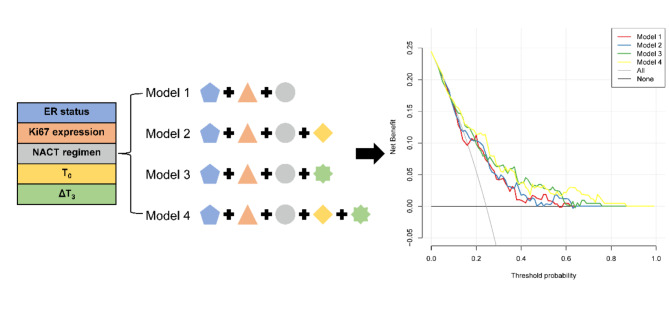
We additionally conducted a DCA to assess predictive performances of four separate models (Fig. 6). Model 1 was developed using ER status, Ki67 expression, and NACT regimen; Model 2 and Model 3 were created using predictors in Model 1 plus  or
or  ; and Model 4 encompassed all stated predictors. Ultimately, the greatest net benefit in predicting NACT response was conveyed by Model 4. Relative to Model 2 and Model 3, there were significant gains in predictive efficiency, supporting
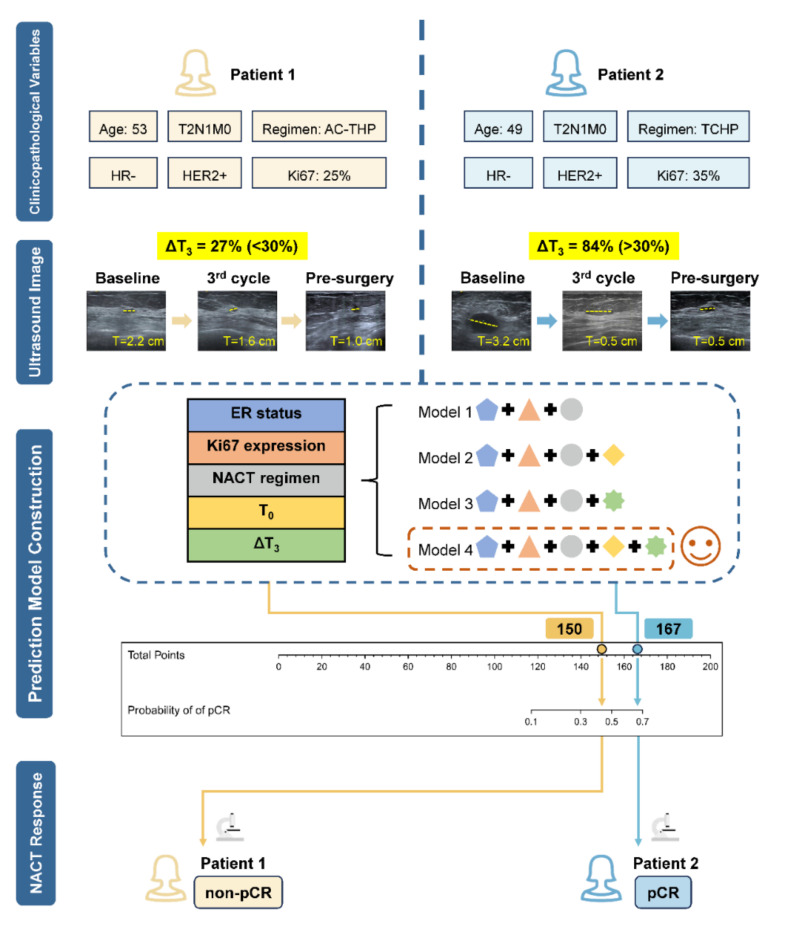
; and Model 4 encompassed all stated predictors. Ultimately, the greatest net benefit in predicting NACT response was conveyed by Model 4. Relative to Model 2 and Model 3, there were significant gains in predictive efficiency, supporting  as a driving factor for improved predictive performance. In Fig. 7, we have presented two patients presented with similar clinical characteristics but with differing tumor dynamic trends during NACT. After three treatment cycles, Patient 2 registered a higher
as a driving factor for improved predictive performance. In Fig. 7, we have presented two patients presented with similar clinical characteristics but with differing tumor dynamic trends during NACT. After three treatment cycles, Patient 2 registered a higher  than that of Patient 1 (84% vs 27%). The total points calculated by nomogram of Patient 1 and Patient 2 are respectively 150 and 167, and Patient 2 had a higher probability of pCR compared to Patient 1. Pathological results upon NACT completion were confirmatory of pCR in Patient 2 but not in Patient 1, underscoring the utility
than that of Patient 1 (84% vs 27%). The total points calculated by nomogram of Patient 1 and Patient 2 are respectively 150 and 167, and Patient 2 had a higher probability of pCR compared to Patient 1. Pathological results upon NACT completion were confirmatory of pCR in Patient 2 but not in Patient 1, underscoring the utility  as a relatively sensitive index of NACT response.
as a relatively sensitive index of NACT response.
Fig. 6.
The decision curve analysis (DCA) of four different models. DCA was performed to compare the predictive performance among four different models. Model 1, NACT regimen + ER + Ki67; Model 2, NACT regimen + ER + Ki67 +  ; Model 3, NACT regimen + ER + Ki67 +
; Model 3, NACT regimen + ER + Ki67 +  ; Model 4, NACT regimen + ER + Ki67 +
; Model 4, NACT regimen + ER + Ki67 +  +
+ . Model 4 had the highest net benefit to predict NACT response. Compared with Model 2, Model 3 showed a significant improvement in predictive efficiency, indicating that
. Model 4 had the highest net benefit to predict NACT response. Compared with Model 2, Model 3 showed a significant improvement in predictive efficiency, indicating that  is a driving factor for improving predictive performance.
is a driving factor for improving predictive performance.
Fig. 7.
Schematic of dynamic tumor changes during NACT in two patients with similar clinicopathological characteristics (Created by Figdraw). Molecular subtypes were identical, both HR−/HER2 + with high-level Ki67 expression; TNM classifications were the same; and ages were roughly similar (49 vs 53 years). In Patient 2, maximum tumor diameter shrank from 3.2 cm at baseline to 0.5 cm after a third cycle of NACT (Anthracycline, Cyclophosphamide, Trastuzumab, and Pertuzumab [TCHP]), with  at 84%. Although unchanged (still 0.5 cm) upon completion of NACT. By contrast, the
at 84%. Although unchanged (still 0.5 cm) upon completion of NACT. By contrast, the  of Patient 1 was just 27% after a third cycle of NACT (Anthracycline and Cyclophosphamide followed by Taxanes, Trastuzumab, and Pertuzumab [AC-THP]), with maximum tumor diameter remained at 1.0 cm after NACT. The total points calculated by nomogram of Patient 1 and Patient 2 were respectively 150 and 167. Based on the prediction model, Patient 2 had a higher probability of pCR compared to Patient 1. Pathological results upon NACT completion were confirmatory of pCR in Patient 2 but not in Patient 1.
of Patient 1 was just 27% after a third cycle of NACT (Anthracycline and Cyclophosphamide followed by Taxanes, Trastuzumab, and Pertuzumab [AC-THP]), with maximum tumor diameter remained at 1.0 cm after NACT. The total points calculated by nomogram of Patient 1 and Patient 2 were respectively 150 and 167. Based on the prediction model, Patient 2 had a higher probability of pCR compared to Patient 1. Pathological results upon NACT completion were confirmatory of pCR in Patient 2 but not in Patient 1.
Machine learning model
During NACT, dynamic changes of US images should not be underestimated. We performed several machine learning algorithms to construct the prediction models, including support vector machines (SVM), decision tree, random forest (RF), gradient boosting machine (GBM), and fully connected neural network (Table 3). The results showed that the SVM exhibited the best predictive performance ( ). Consequently, our final endeavor was constructing a SVM model driven by clinicopathological data and US parameters at each treatment cycle, including maximum tumor diameters and volumes. The model’s precision, recall and F1 scores were 77.0%, 71.0%, and 74.0%, respectively. The confusion matrix is provided as Fig. 8.
). Consequently, our final endeavor was constructing a SVM model driven by clinicopathological data and US parameters at each treatment cycle, including maximum tumor diameters and volumes. The model’s precision, recall and F1 scores were 77.0%, 71.0%, and 74.0%, respectively. The confusion matrix is provided as Fig. 8.
Table 3.
The AUC values of different machine learning algorithms for predicting pCR.
| Machine learning algorithms | AUC |
|---|---|
| SVM | 0.868 |
| Fully connected neural network | 0.827 |
| RF | 0.816 |
| GBM | 0.805 |
| Decision tree | 0.633 |
SVM support vectors machines, RF random forest, GBM gradient boosting machine.
Fig. 8.
The confusion matrix of the SVM model (a) and the ROC curve of the SVM model (b).
Discussion
Cure is the ultimate goal of treatment in patients with EBC. Breast cancer is a systemic disease requiring systemic intervention, including chemotherapy and targeted therapy33. However, the therapeutic effects will vary according to individual, some responding to systemic therapy and others left unaffected. Multicenter prospective clinical studies, such as CREATE-X and KATHERINE, have confirmed that intensified follow-up adjuvant therapy in proven non-responders may improve long-term survival34,35. Early response evaluations during treatment or even at baseline are therefore essential for optimal outcomes.
NACT is an individual drug sensitivity assessment platform. Patients insensitive to standard NACT regimens must be detected as soon as possible to avoid unnecessary toxicity exposures and extra costs. There is an unmet clinical need for a biomarker to distinguish patient subsets by pCR and non-pCR. Non-pCR patients calls for treatment revision or expeditious surgical management.
Imaging methods and liquid biopsy have been previously utilized during a number of studies to evaluate patient response early. In the PHERGain trial, 18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET) was performed to metabolically detect HER2+ breast cancer patients, enabling dual targeted therapies and avoiding chemotherapy after just two cycles of treatment36. Dynamic contrast-enhanced (DCE)-MRI performed after two cycles of NACT may also help predict pathological responses in the setting of breast cancer37. Liquid biopsies were undertaken in the WSG-ADAPT-TP trial to determine patient responses in early-stage, defined as 30% decline in Ki67 expression or low cellularity38. Also, ctDNA and circulating free DNA (cfDNA) have known merit as predictive and prognostic factors39–41. The current contention in China is that MRI and PET-computed tomography (CT), as well as secondary biopsies, may be costly and inordinately traumatic for patients.
US imaging is a noninvasive and cost-effective method for examining the breast. In the GeparTrio trial, US served to identify non-responders who initially received taxanes/anthracycline/cyclophosphamide (TAC) regimen. Switching to TAC plus vinorelbine/capecitabine (TAC-NX) improved their prognosis, without cross-drug resistance or NACT prolongation42. Similarly, US imaging has facilitated early NACT response prediction in the Neo-ALTTO trial43; and some small-scale studies have focused on its role in early response evaluation44,45, without a uniform consensus on timing or criteria of such efforts. In the present study, we primarily addressed early tumor shrinkage in the nomogram, validating tumor reduction after three cycles of NACT as a basis for early response determinations. This finding indicated that the concept of early prediction does not imply that the earlier the prediction, the more accurate it will be. The changes of the tumor after three cycles of NACT may prove to be a more accurate predictor of the response than the earlier assessments. Interestingly, the cut-off value of 29.9% is just comparable to the definition of partial response (PR) by RECIST standards (version 1.1)46. This outcome readily demonstrates that early US examinations during NACT are beneficial, ensuring timely modifications of therapeutic regimens.
Machine learning has been extensively applied to therapeutic response evaluations, revealing tumor characteristics that escape the naked eye47–49. One such model has already been reported for handling dynamic longitudinal US imaging data to predict pCR early during NACT in patients with HER2+ breast cancer50. Several other studies have concentrated on pre-, mid-, and post-NACT features of US-delineated NACT response, while failing to explore dynamic tumor changes51,52. Herein, we assessed US parameters at each cycle of NACT to fully capture tumor dynamics in our prediction model. To the best of our knowledge, it is the first time to investigate the predictive efficacy of dynamic changes in ultrasound-measured tumor maximum diameter throughout the entire NACT cycle. We also input static elements, including hormone receptor (ER/PR) status, HER2 status, Ki67 expression, and NACT regimen. By integrating both dynamic and static features, predictive performance was heightened ( ) to levels reached elsewhere, capable of reliably guiding therapeutic decisions. Furthermore, other researchers have reported that MRI has the potential to predict pCR to NACT, with AUC values ranging from 0.7 to 0.953,54. This suggests that our US-based prediction models are comparable to other MRI-based prediction models. Although MRI is considered to have the highest sensitivity for breast cancer detection and the high accuracy to predict the response to NACT13,55, it is a costly procedure, rendering it impractical for frequent scanning during NACT. In comparison, US is a more cost-effective and widely available modality, and therefore more suitable to be the routine NACT monitoring tool.
) to levels reached elsewhere, capable of reliably guiding therapeutic decisions. Furthermore, other researchers have reported that MRI has the potential to predict pCR to NACT, with AUC values ranging from 0.7 to 0.953,54. This suggests that our US-based prediction models are comparable to other MRI-based prediction models. Although MRI is considered to have the highest sensitivity for breast cancer detection and the high accuracy to predict the response to NACT13,55, it is a costly procedure, rendering it impractical for frequent scanning during NACT. In comparison, US is a more cost-effective and widely available modality, and therefore more suitable to be the routine NACT monitoring tool.
Clinicopathological parameters also figured prominently in response evaluation. We identified other independent predictors of pCR, including ER status, Ki67 expression,  , and NACT regimen. The nomogram reached an AUC of 0.75. Patients with ER− (vs ER+) tumors displayed a comparatively higher rate of pCR, aligning with past studies and perhaps translating to less NACT sensitivity of ER+ patients32. Ki67 is a biomarker of cellular proliferation with predictive ramifications56. In our study, the higher the expression level of Ki67, the more likely pCR would be achieved, albeit with no consensus on a related cut-off value.
, and NACT regimen. The nomogram reached an AUC of 0.75. Patients with ER− (vs ER+) tumors displayed a comparatively higher rate of pCR, aligning with past studies and perhaps translating to less NACT sensitivity of ER+ patients32. Ki67 is a biomarker of cellular proliferation with predictive ramifications56. In our study, the higher the expression level of Ki67, the more likely pCR would be achieved, albeit with no consensus on a related cut-off value.  emerged as an independent predictor as well, and larger tumors had worse responses. Carboplatin is a DNA alkylating agent often administered for TNBC, which bears higher rates of BRCA1/2 mutation57,58. Patients treated with carboplatin and paclitaxel, with or without anthracycline, were more inclined to pCR, as opposed to recipients of anthracycline-based regimens. However, 80% of those treated with carboplatin were HER2+ and additionally received targeted therapy. We did add
emerged as an independent predictor as well, and larger tumors had worse responses. Carboplatin is a DNA alkylating agent often administered for TNBC, which bears higher rates of BRCA1/2 mutation57,58. Patients treated with carboplatin and paclitaxel, with or without anthracycline, were more inclined to pCR, as opposed to recipients of anthracycline-based regimens. However, 80% of those treated with carboplatin were HER2+ and additionally received targeted therapy. We did add  to the nomogram, and
to the nomogram, and  distinctly contributed to improved predictive performance in the subsequent DCA.
distinctly contributed to improved predictive performance in the subsequent DCA.
There are certain study limitations to acknowledge. The prediction models were constructed based on retrospective data, which may have biases. To eliminate potential biases, patients were enrolled from multiple centers and objective variables were selected for multivariate analysis. This was done in order to minimize the effect of these biases on the results. The incorporation of prospective data from more clinical trials would improve the clinical evidence supporting the validity of our model. Another drawback is the small number of patients enrolled, knowing that various molecular subtypes commonly influence treatment and therapeutic effects. Moreover, because trastuzumab (Herceptin) has been widely used in China since 2017, some patients with HER2+ tumors did not receive targeted therapy. Furthermore, intra- and inter-observer variability is also typically high for US imaging, which may potentially impact the accuracy and reliability of US results. In light of the aforementioned considerations, all radiologists were required to follow standard guidelines and protocols in order to minimize the potential US variability. In the future, more work is planned to refine this prediction model, especially an expanded patient sampling with broader clinical implications. Prospective clinical trials are ultimately needed to optimize our prediction model.
In conclusion, we have proposed a method for timely prediction of NACT responses. This simple graphic representation is intuitive and may assist clinicians in rendering expeditious, individualized therapeutic decisions. We have also constructed an analogous machine learning model that combines dynamic US changes and static clinicopathological characteristics. It may well serve as a reference for preoperative clinical decision-making. Given their overall clinical potential, validation is warranted for both models through future clinical trials.
Author contributions
XW and YZ conceived this study, performed the data analyses and wrote the manuscript. MY and PQ performed the machine learning part. NW, SW, HC, TZ, and YZ assisted revising the manuscript. ZJ, AZ, FY, XW, and FJ provided a portion of the data. JW designed the study and was the director for the fund. All authors read and approved the final manuscript.
Funding
This study was supported by the “1 + X” program cross-disciplinary innovation project (2022JCXKYB07), and Wu Jieping Medical Foundation (320.6750.2022-19-81).
Data availability
The medical data used in this study are not publicly available due to patient privacy considerations. Interested users may request access to the data for research purposes, through contacting the corresponding author. Institutional approvals of data sharing will be required along with signed data use agreements and/or material transfer agreements.
Declarations
Competing interests
The authors declare that they have no competing interests.
Ethics declarations
This is a retrospective study approved by the ethics committee of Second Affiliated Hospital of Dalian Medical University. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent has been obtained from patients.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Xinyi Wang and Yuting Zhang.
References
- 1.Korde, L. A. et al. Neoadjuvant chemotherapy, endocrine therapy, and targeted therapy for breast cancer: ASCO guideline. J. Clin. Oncol.39, 1485–1505. 10.1200/jco.20.03399 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cortazar, P. et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet384, 164–172. 10.1016/s0140-6736(13)62422-8 (2014). [DOI] [PubMed] [Google Scholar]
- 3.Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol.19, 27–39. 10.1016/s1470-2045(17)30777-5 (2018). [DOI] [PMC free article] [PubMed]
- 4.Clough, K. B. et al. Rates of neoadjuvant chemotherapy and oncoplastic surgery for breast cancer surgery: A French national survey. Ann. Surg. Oncol.22, 3504–3511. 10.1245/s10434-015-4378-6 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Mougalian, S. S. et al. Use of neoadjuvant chemotherapy for patients with stage I to III breast cancer in the United States. Cancer121, 2544–2552. 10.1002/cncr.29348 (2015). [DOI] [PubMed] [Google Scholar]
- 6.Khokher, S., Mahmood, S., Qureshi, M. U., Khan, S. A. & Chaudhry, N. A. “Initial clinical response” to neoadjuvant chemotherapy: an in-vivo chemosensitivity test for efficacy in patients with advanced breast cancer. Asian Pac. J. Cancer Prev.12, 939–946 (2011). [PubMed] [Google Scholar]
- 7.Miglietta, F., Dieci, M. V., Griguolo, G. & Guarneri, V. Neoadjuvant approach as a platform for treatment personalization: focus on HER2-positive and triple-negative breast cancer. Cancer Treat. Rev.98, 102222. 10.1016/j.ctrv.2021.102222 (2021). [DOI] [PubMed] [Google Scholar]
- 8.Fisher, B. et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J. Clin. Oncol.41, 1795–1808. 10.1200/jco.22.02571 (2023). [DOI] [PubMed] [Google Scholar]
- 9.Esserman, L. J. et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J. Clin. Oncol.30, 3242–3249. 10.1200/jco.2011.39.2779 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pierga, J. Y. et al. Prognostic factors for survival after neoadjuvant chemotherapy in operable breast cancer. the role of clinical response. Eur. J. Cancer39, 1089–1096. 10.1016/s0959-8049(03)00069-8 (2003). [DOI] [PubMed]
- 11.Balu-Maestro, C. et al. Imaging in evaluation of response to neoadjuvant breast cancer treatment benefits of MRI. Breast Cancer Res. Treat.72, 145–152. 10.1023/a:1014856713942 (2002). [DOI] [PubMed] [Google Scholar]
- 12.Park, S. H. et al. Diffusion-weighted MR imaging: pretreatment prediction of response to neoadjuvant chemotherapy in patients with breast cancer. Radiology257, 56–63. 10.1148/radiol.10092021 (2010). [DOI] [PubMed] [Google Scholar]
- 13.Gu, Y. L., Pan, S. M., Ren, J., Yang, Z. X. & Jiang, G. Q. Role of magnetic resonance imaging in detection of pathologic complete remission in breast cancer patients treated with neoadjuvant chemotherapy: a meta-analysis. Clin. Breast Cancer17, 245–255. 10.1016/j.clbc.2016.12.010 (2017). [DOI] [PubMed] [Google Scholar]
- 14.Janssen, L. M. et al. MRI to assess response after neoadjuvant chemotherapy in breast cancer subtypes: a systematic review and meta-analysis. NPJ Breast Cancer8, 107. 10.1038/s41523-022-00475-1 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dialani, V., Chadashvili, T. & Slanetz, P. J. Role of imaging in neoadjuvant therapy for breast cancer. Ann. Surg. Oncol.22, 1416–1424. 10.1245/s10434-015-4403-9 (2015). [DOI] [PubMed] [Google Scholar]
- 16.Keune, J. D. et al. Accuracy of ultrasonography and mammography in predicting pathologic response after neoadjuvant chemotherapy for breast cancer. Am. J. Surg.199, 477–484. 10.1016/j.amjsurg.2009.03.012 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magbanua, M. J. M. et al. Circulating tumor DNA in neoadjuvant-treated breast cancer reflects response and survival. Ann. Oncol.32, 229–239. 10.1016/j.annonc.2020.11.007 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Magbanua, M. J. M. et al. Circulating tumor DNA and magnetic resonance imaging to predict neoadjuvant chemotherapy response and recurrence risk. NPJ Breast Cancer7, 32. 10.1038/s41523-021-00239-3 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang, X. et al. Early prediction of pathological outcomes to neoadjuvant chemotherapy in breast cancer patients using automated breast ultrasound. Chin. J. Cancer Res.28, 478–485. 10.21147/j.issn.1000-9604.2016.05.02 (2016). [DOI] [PMC free article] [PubMed]
- 20.Chen, P. et al. Multivariable models based on baseline imaging features and clinicopathological characteristics to predict breast pathologic response after neoadjuvant chemotherapy in patients with breast cancer. Breast Care (Basel, Switzerland)17, 306–315. 10.1159/000521638 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park, Y. H. et al. Chemotherapy induces dynamic immune responses in breast cancers that impact treatment outcome. Nat. Commun.11, 6175. 10.1038/s41467-020-19933-0 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skarping, I., Larsson, M. & Förnvik, D. Analysis of mammograms using artificial intelligence to predict response to neoadjuvant chemotherapy in breast cancer patients: proof of concept. Eur. Radiol.32, 3131–3141. 10.1007/s00330-021-08306-w (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cain, E. H. et al. Multivariate machine learning models for prediction of pathologic response to neoadjuvant therapy in breast cancer using MRI features: a study using an independent validation set. Breast Cancer Res. Treat.173, 455–463. 10.1007/s10549-018-4990-9 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang, M. et al. Ultrasound-based deep learning radiomics in the assessment of pathological complete response to neoadjuvant chemotherapy in locally advanced breast cancer. Eur. J. Cancer147, 95–105. 10.1016/j.ejca.2021.01.028 (2021). [DOI] [PubMed] [Google Scholar]
- 25.Hammond, M. E. et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J. Clin. Oncol.28, 2784–2795. 10.1200/jco.2009.25.6529 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolff, A. C. et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. J. Clin. Oncol.36, 2105–2122. 10.1200/jco.2018.77.8738 (2018). [DOI] [PubMed] [Google Scholar]
- 27.Gerdes, J. et al. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J. Immunol. (Baltimore, MD.: 1950)133, 1710–1715 (1984). [PubMed]
- 28.Ogston, K. N. et al. A new histological grading system to assess response of breast cancers to primary chemotherapy: prognostic significance and survival. Breast12, 320–327. 10.1016/s0960-9776(03)00106-1 (2003). [DOI] [PubMed] [Google Scholar]
- 29.Fumagalli, D. et al. A common language in neoadjuvant breast cancer clinical trials: proposals for standard definitions and endpoints. Lancet Oncol.13, e240-248. 10.1016/s1470-2045(11)70378-3 (2012). [DOI] [PubMed] [Google Scholar]
- 30.Provenzano, E. et al. Standardization of pathologic evaluation and reporting of postneoadjuvant specimens in clinical trials of breast cancer: recommendations from an international working group. Mod. Pathol.28, 1185–1201. 10.1038/modpathol.2015.74 (2015). [DOI] [PubMed]
- 31.Huang, M. et al. Association of pathologic complete response with long-term survival outcomes in triple-negative breast cancer: a meta-analysis. Cancer Res.80, 5427–5434. 10.1158/0008-5472.Can-20-1792 (2020). [DOI] [PubMed] [Google Scholar]
- 32.Jin, X. et al. A nomogram for predicting pathological complete response in patients with human epidermal growth factor receptor 2 negative breast cancer. BMC Cancer16, 606. 10.1186/s12885-016-2652-z (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harbeck, N. Breast cancer is a systemic disease optimally treated by a multidisciplinary team. Nat. Rev. Dis. Primers6, 30. 10.1038/s41572-020-0167-z (2020). [DOI] [PubMed] [Google Scholar]
- 34.Masuda, N. et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N. Engl. J. Med.376, 2147–2159. 10.1056/NEJMoa1612645 (2017). [DOI] [PubMed] [Google Scholar]
- 35.von Minckwitz, G. et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N. Engl. J. Med.380, 617–628. 10.1056/NEJMoa1814017 (2019). [DOI] [PubMed] [Google Scholar]
- 36.Pérez-García, J. M. et al. Chemotherapy de-escalation using an (18)F-FDG-PET-based pathological response-adapted strategy in patients with HER2-positive early breast cancer (PHERGain): a multicentre, randomised, open-label, non-comparative, phase 2 trial. Lancet Oncol.22, 858–871. 10.1016/s1470-2045(21)00122-4 (2021). [DOI] [PubMed] [Google Scholar]
- 37.Tateishi, U. et al. Neoadjuvant chemotherapy in breast cancer: prediction of pathologic response with PET/CT and dynamic contrast-enhanced MR imaging–prospective assessment. Radiology263, 53–63. 10.1148/radiol.12111177 (2012). [DOI] [PubMed] [Google Scholar]
- 38.Harbeck, N. et al. De-escalation strategies in human epidermal growth factor receptor 2 (HER2)-positive early breast cancer (BC): final analysis of the West German Study Group adjuvant dynamic marker-adjusted personalized therapy trial optimizing risk assessment and therapy response prediction in early BC HER2- and hormone receptor-positive phase II randomized trial-efficacy, safety, and predictive markers for 12 weeks of neoadjuvant trastuzumab emtansine with or without endocrine therapy (ET) versus trastuzumab plus ET. J. Clin. Oncol.35, 3046–3054. 10.1200/jco.2016.71.9815 (2017). [DOI] [PubMed] [Google Scholar]
- 39.Zhou, Q. et al. Persistence of ctDNA in patients with breast cancer during neoadjuvant treatment is a significant predictor of poor tumor response. Clin. Cancer Res.28, 697–707. 10.1158/1078-0432.Ccr-21-3231 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ma, G. et al. Identification of the plasma total cfDNA level before and after chemotherapy as an indicator of the neoadjuvant chemotherapy response in locally advanced breast cancer. Cancer Med.9, 2271–2282. 10.1002/cam4.2906 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magbanua, M. J. M. et al. Clinical significance and biology of circulating tumor DNA in high-risk early-stage HER2-negative breast cancer receiving neoadjuvant chemotherapy. Cancer Cell41, 1091-1102.e1094. 10.1016/j.ccell.2023.04.008 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.von Minckwitz, G. et al. Response-guided neoadjuvant chemotherapy for breast cancer. J. Clin. Oncol.31, 3623–3630. 10.1200/jco.2012.45.0940 (2013). [DOI] [PubMed] [Google Scholar]
- 43.Di Cosimo, S. et al. The use of breast imaging for predicting response to neoadjuvant lapatinib, trastuzumab and their combination in HER2-positive breast cancer: Results from Neo-ALTTO. Eur. J. Cancer89, 42–48. 10.1016/j.ejca.2017.10.036 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adrada, B. E. et al. Early ultrasound evaluation identifies excellent responders to neoadjuvant systemic therapy among patients with triple-negative breast cancer. Cancer127, 2880–2887. 10.1002/cncr.33604 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hong, J. et al. Early response and pathological complete remission in Breast Cancer with different molecular subtypes: a retrospective single center analysis. J. Cancer11, 6916–6924. 10.7150/jca.46805 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer45, 228–247. 10.1016/j.ejca.2008.10.026 (2009). [DOI] [PubMed]
- 47.Bitencourt, A. G. V. et al. MRI-based machine learning radiomics can predict HER2 expression level and pathologic response after neoadjuvant therapy in HER2 overexpressing breast cancer. EBioMedicine61, 103042. 10.1016/j.ebiom.2020.103042 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tahmassebi, A. et al. Impact of machine learning with multiparametric magnetic resonance imaging of the breast for early prediction of response to neoadjuvant chemotherapy and survival outcomes in breast cancer patients. Investig. Radiol.54, 110–117. 10.1097/rli.0000000000000518 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gillies, R. J., Kinahan, P. E. & Hricak, H. Radiomics: Images are more than pictures, they are data. Radiology278, 563–577. 10.1148/radiol.2015151169 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu, Y. et al. Early prediction of treatment response to neoadjuvant chemotherapy based on longitudinal ultrasound images of HER2-positive breast cancer patients by Siamese multi-task network: A multicentre, retrospective cohort study. EClinicalMedicine52, 101562. 10.1016/j.eclinm.2022.101562 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eun, N. L., Son, E. J., Gweon, H. M., Kim, J. A. & Youk, J. H. Prediction of axillary response by monitoring with ultrasound and MRI during and after neoadjuvant chemotherapy in breast cancer patients. Eur. Radiol.30, 1460–1469. 10.1007/s00330-019-06539-4 (2020). [DOI] [PubMed] [Google Scholar]
- 52.Zhu, Q. et al. Early assessment window for predicting breast cancer neoadjuvant therapy using biomarkers, ultrasound, and diffuse optical tomography. Breast Cancer Res. Treat.188, 615–630. 10.1007/s10549-021-06239-y (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu, Z. et al. Radiomics of multiparametric MRI for pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: a multicenter study. Clin. Cancer Res.25, 3538–3547. 10.1158/1078-0432.Ccr-18-3190 (2019). [DOI] [PubMed] [Google Scholar]
- 54.Huang, Y. et al. Longitudinal MRI-based fusion novel model predicts pathological complete response in breast cancer treated with neoadjuvant chemotherapy: a multicenter, retrospective study. EClinicalMedicine58, 101899. 10.1016/j.eclinm.2023.101899 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mann, R. M., Cho, N. & Moy, L. Breast MRI: state of the art. Radiology292, 520–536. 10.1148/radiol.2019182947 (2019). [DOI] [PubMed] [Google Scholar]
- 56.Zhang, J. et al. A Novel model incorporating tumor stiffness, blood flow characteristics, and Ki-67 expression to predict responses after neoadjuvant chemotherapy in breast cancer. Front. Oncol.10, 603574. 10.3389/fonc.2020.603574 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hurley, J. et al. The use of neoadjuvant platinum-based chemotherapy in locally advanced breast cancer that is triple negative: retrospective analysis of 144 patients. Breast Cancer Res. Treat.138, 783–794. 10.1007/s10549-013-2497-y (2013). [DOI] [PubMed] [Google Scholar]
- 58.Farmer, H. et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature434, 917–921. 10.1038/nature03445 (2005). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The medical data used in this study are not publicly available due to patient privacy considerations. Interested users may request access to the data for research purposes, through contacting the corresponding author. Institutional approvals of data sharing will be required along with signed data use agreements and/or material transfer agreements.