Abstract
This report presents two cases of colonic perforation that occurred following an upper gastrointestinal series (UGIS) with barium as part of a health screening. UGIS is a widely performed examination in Japan and is useful for the early detection of gastric cancer and peptic ulcers, but it carries a rare risk of causing serious gastrointestinal perforation. This study details the mechanisms of perforation, risk factors, difficulties in imaging diagnosis, and treatment options. Cases of perforation require early diagnosis and appropriate surgical intervention, with Hartmann's procedure or colostomy being the common choices. This case series emphasizes the need to recognize the potential risks associated with UGIS, even though it is considered relatively safe. With the advancement of endoscopic examination technology in recent years, endoscopy is increasingly being adopted as an alternative to UGIS in health screenings, and there is a need to reconsider future examination methods.
Keywords: barium, colonic perforation, gastric cancer screening, peritonitis, upper gastrointestinal series
Introduction
Upper gastrointestinal barium studies are widely performed in Japan as part of health screenings and are valued for their accessibility and ability to detect early-stage abnormalities, such as gastric cancer and peptic ulcers [1]. However, gastrointestinal perforation, though rare (approximately three cases per 1,010,000 examinations), can lead to severe complications, including peritonitis and sepsis, if not promptly treated [2,3]. Identified risk factors include advanced age, diverticulosis, and chronic constipation, which can increase the likelihood of perforation [4,5].
Here, we report two cases of colonic perforation following upper gastrointestinal barium examinations, aiming to highlight the mechanisms and clinical implications of this rare but serious complication.
Case presentation
Case 1
A 53-year-old female with a history of ventricular septal defect presented to our hospital. Three days prior, she had undergone an upper gastrointestinal barium examination as part of a comprehensive medical check-up. Since the examination, she had noted daily passage of white stool. Subsequently, she developed abdominal pain, which progressively worsened, prompting her to be transported to our hospital on an emergency basis.
The patient was 155.0 cm in height and weighed 55.0 kg. Her body temperature was 35.1°C. Blood pressure was 92/76 mmHg, with a pulse rate of 55 beats per minute. Tenderness was noted in the left abdominal region, but there was no evidence of rebound tenderness or board-like rigidity.
Initial blood biochemical investigations at the time of admission revealed abnormalities in white blood cell count, which was elevated, while C-reactive protein (CRP) levels were within normal limits. Detailed laboratory findings are summarized in Table 1.
Table 1. Serum laboratory results on admission and hospital day three.
WBC: white blood cells; RBC: red blood cells; BUN: blood urea nitrogen; AST: aspartate transferase; ALT: alanine transaminase; INR: international normalized ratio; PT: prothrombin time; APTT: partial thromboplastin time; CRP: C-reactive protein; NA: not assessed
| Parameters | On admission | Hospital day 3 | Reference Range |
| WBC | 12.1 | 8.8 | 3.3-8.6 x 103/uL |
| Neutrophils relative percent | 85.4 | 90.9 | 44.0-70.0% |
| Lymphocytes | 10.9 | 7.4 | 31.0-49.0% |
| Monocytes | 3.2 | 1.2 | 3.0-8.0% |
| Eosinophils | 0.2 | 0.4 | 1.0-5.0% |
| Basophils | 0.3 | 0.1 | 0.0-3.0% |
| RBC | 4.97 | 3.66 | 3.86-4.92 x 106/uL |
| Hemoglobin | 16.0 | 11.9 | 11.6-14.8 g/dL |
| Hematocrit | 47.9 | 34.1 | 35.1-44.4% |
| Platelet count | 212 | 118 | 158-348 x 103/uL |
| PT | 98.0 | NA | 75-125% |
| INR | 1.0 | NA | |
| APTT | 25.4 | NA | 25-39 seconds |
| Total Protein | 6.1 | 4.6 | 6.6-8.1 g/dL |
| Albumin | 3.6 | 2.2 | 4.1-5.1 g/dL |
| Total Bilirubin | 0.4 | 0.4 | 0.4-1.5 mg/dL |
| AST | 21 | 19 | 13-30 U/L |
| ALT | 20 | 14 | 7-23 U/L |
| Alkaline phosphatase | 249 | 168 | 106-322 IFCC |
| BUN | 14.4 | 19.7 | 8-20 mg/dL |
| Creatinine | 0.76 | 0.76 | 0.46-0.79 mg/dL |
| Sodium | 142 | 141 | 138-145 mmol/L |
| Potassium | 4 | 4 | 3.6-4.8 mmol/L |
| Chloride | 108 | 111 | 101-108 mmol/L |
| Calcium | 9.0 | 8.5 | 8.8-10.1 mg/dL |
| CRP | 0.02 | 36.95 | 0.00-0.14 mg/dl |
| Lactate | NA | 1.0 | <=2.0 mmol/L |
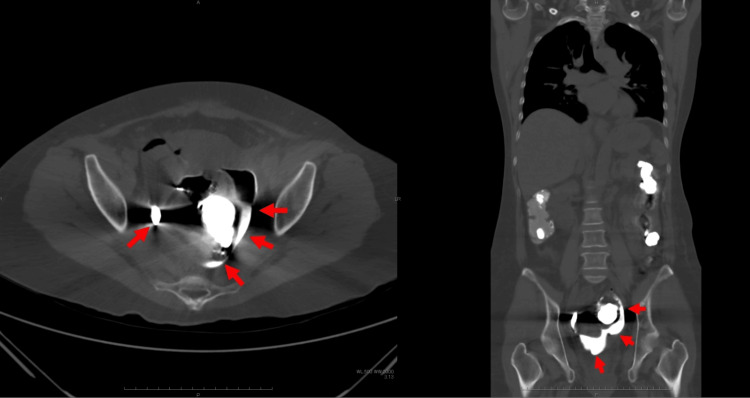
A computed tomography (CT) scan was performed due to suspected gastrointestinal perforation caused by barium. Residual barium was observed extending from the sigmoid colon to the rectum. Due to halation effects, precise evaluation was challenging; however, no definite evidence of intraperitoneal free air was noted. On the third day of hospitalization, the patient experienced worsening abdominal pain and a fever of 38.5°C. Blood biochemical tests performed on the same day revealed a significant increase in CRP levels and a decrease in platelet count. A follow-up CT scan revealed the presence of extraluminal leakage of barium (Figure 1).
Figure 1. Plain abdominal CT scan.
A follow-up plain abdominal CT scan (axial view, left; coronal view, right) demonstrated extraluminal barium extravasation (red arrow).
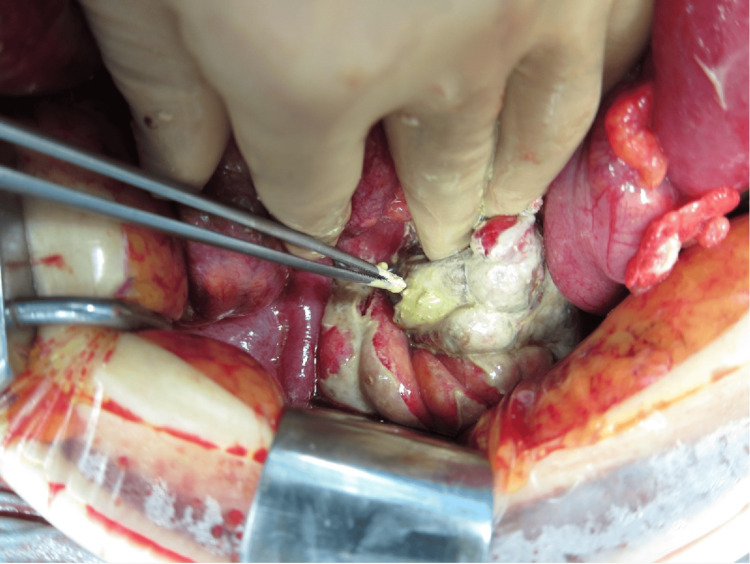
An emergency laparotomy was performed with a diagnosis of peritonitis caused by gastrointestinal perforation from barium. A perforation approximately 2 cm in size was found in the upper rectum, with barium leaking into the peritoneal cavity (Figure 2). The peritoneal cavity was irrigated, and the affected portion of the rectum, including the perforation site, was resected. A colostomy was created at the proximal end (Hartmann's procedure).
Figure 2. Emergency laparotomy.
A perforation approximately 2 cm in size was found in the upper rectum, with barium leaking into the peritoneal cavity.
Pathological examination of the resected specimen revealed necrosis and infiltration of acute inflammatory cells around the perforation site. No malignancy or diverticula were identified (Figure 3).
Figure 3. Resected specimen.
Necrosis and infiltration of acute inflammatory cells were observed in the intestinal tissue surrounding the perforation site. No evidence of malignancy or diverticula was found.
The postoperative course was uneventful, and the patient was discharged on the 31st day after surgery. A colostomy closure was successfully performed 10 months later.
Case 2
A 74-year-old female with a history of hypertension underwent an upper gastrointestinal barium examination at a health screening facility. The next day, she developed abdominal pain, which progressively worsened, leading her to consult a previous physician. A CT scan suggested sigmoid colon perforation, and she was referred to our hospital.
The patient was 156.0 cm in height and weighed 43.0 kg. Her body temperature was 38.3°C. Blood pressure was 155/68 mmHg, and her pulse rate was 105 beats per minute. Tenderness, rebound tenderness, and muscle guarding were noted throughout the abdomen.
Blood biochemical investigations showed a decreased white blood cell count, elevated CRP levels, and increased D-dimer, indicating an inflammatory and hypercoagulable state. Detailed laboratory findings are summarized in Table 2.
Table 2. Serum laboratory results on admission.
WBC: white blood cells; RBC: red blood cells; BUN: blood urea nitrogen; AST: aspartate transferase; ALT: alanine transaminase; INR: international normalized ratio; PT: prothrombin time; APTT: partial thromboplastin time; CRP: C-reactive protein
| Parameters | On admission | Reference Range |
| WBC | 2.1 | 3.3-8.6 x 103/uL |
| Neutrophils relative percent | 78.6 | 44.0-70.0% |
| Lymphocytes | 17.0 | 31.0-49.0% |
| Monocytes | 4.4 | 3.0-8.0% |
| Eosinophils | 0.0 | 1.0-5.0% |
| Basophils | 0.0 | 0.0-3.0% |
| RBC | 4.4 | 3.86-4.92 x 106/uL |
| Hemoglobin | 13.0 | 11.6-14.8 g/dL |
| Hematocrit | 38.5 | 35.1-44.4% |
| Platelet count | 306.0 | 158-348 x 103/uL |
| PT | 80.0 | 75-125% |
| INR | 1.1 | |
| APTT | 27.8 | 25-39 seconds |
| D-dimer | 5.5 | <1.0 ug/mL |
| Total Protein | 6.4 | 6.6-8.1 g/dL |
| Albumin | 3.0 | 4.1-5.1 g/dL |
| Total Bilirubin | 0.5 | 0.4-1.5 mg/dL |
| AST | 24.0 | 13-30 U/L |
| ALT | 14.0 | 7-23 U/L |
| Alkaline phosphatase | 236.0 | 106-322 IFCC |
| Glucose | 137.0 | 73-109 mg/dL |
| BUN | 15.3 | 8-20 mg/dL |
| Creatinine | 0.6 | 0.46-0.79 mg/dL |
| Sodium | 136.0 | 138-145 mmol/L |
| Potassium | 3.6 | 3.6-4.8 mmol/L |
| Chloride | 105.0 | 101-108 mmol/L |
| Calcium | 9.1 | 8.8-10.1 mg/dL |
| CRP | 1.2 | 0.00-0.14 mg/dL |
| Lactate | 2.2 | <=2.0 mmol/L |
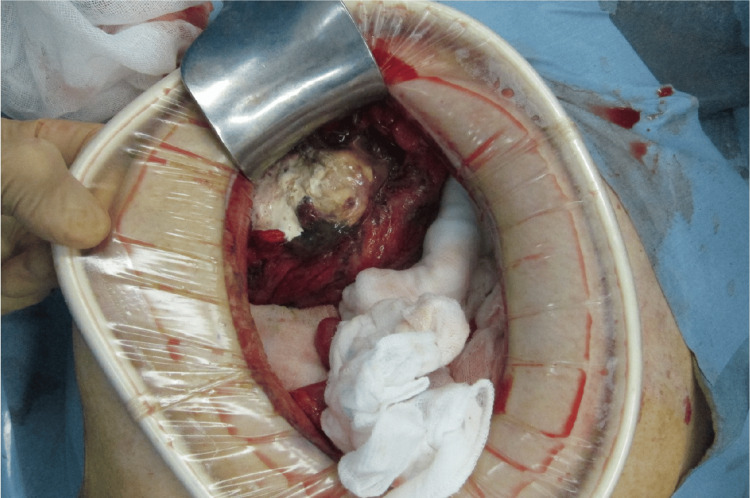
CT imaging performed by the referring physician confirmed sigmoid colon perforation due to barium. Extraluminal barium leakage, free intraperitoneal air, and a localized abscess were also identified (Figure 4).
Figure 4. Plain abdominal CT scan.
A plain abdominal CT scan (axial view, left; coronal view, right) demonstrates sigmoid colon perforation with extravasation of barium contrast medium, free intraperitoneal air (red arrow), and a localized intra-abdominal abscess.
Emergency laparotomy revealed peritonitis caused by barium-induced sigmoid colon perforation. The serosal surface of the sigmoid colon exhibited hematoma formation, necrotic changes, and a central perforation measuring 1 cm in diameter. Barium extravasation into the peritoneal cavity was confirmed (Figure 5). The peritoneal cavity was thoroughly irrigated, and the affected sigmoid colon, including the perforation site, was resected. A colostomy was performed at the proximal end using Hartmann's procedure.
Figure 5. Emergency laparotomy.
The serosal surface of the sigmoid colon showed hematoma formation and necrotic changes, with a central perforation measuring 1 cm in diameter.
Pathological examination revealed severe inflammatory cell infiltration, predominantly neutrophils, around the perforation site. A localized abscess was present in the subserosal tissue. No malignancy or diverticula were detected (Figure 6).
Figure 6. Resected specimen.
Severe inflammatory cell infiltration, predominantly neutrophils, was observed around the perforation site. A localized abscess was noted in part of the subserosal tissue. No evidence of malignancy or diverticula was found.
The patient’s postoperative course was uneventful, and she was discharged on the 36th day after surgery. A colostomy closure was successfully performed six months later.
Discussion
Upper gastrointestinal barium examinations, widely used in Japan's health screenings, play a critical role in detecting gastric cancer and peptic ulcers [1]. Despite their safety, rare complications such as colonic perforation, occurring in three out of 1,010,000 cases (0.0003%), have been reported [2]. Risk factors include advanced age and comorbidities, particularly in patients with diverticula or chronic constipation, where the accumulation of barium in the bowel and subsequent pressure may elevate the risk of perforation [2]. Additionally, the condition tends to be more common among elderly individuals and females, with decreased gastrointestinal flexibility and bowel stenosis due to aging acting as further risk factors [2].
There are several hypotheses regarding the mechanism of colonic perforation. Barium absorbs moisture within the intestine and hardens, making passage through the bowel difficult. It is believed that the hardened barium mass exerts strong pressure on the bowel wall, causing tears or perforation [3]. Furthermore, in cases of bowel stenosis or constipation, the intraluminal pressure tends to increase, and the retention of barium elevates the risk of perforation [5]. Most perforations occur in areas such as the sigmoid colon or rectum, which are structurally prone to increased pressure. In these areas, barium tends to accumulate, and the bowel is more susceptible to physical stretching, which can easily lead to ischemic conditions. Ischemia weakens the bowel wall, making it more prone to tears, ultimately resulting in perforation [6].
If perforation is suspected following a barium examination, patients often present with acute abdominal pain and symptoms of peritonitis. Prompt medical attention is necessary when these symptoms arise. CT is highly useful for diagnosing perforation as it allows for the identification of intraperitoneal free air and extraluminal leakage of barium, thus confirming the diagnosis. However, barium can create artifacts on CT images, potentially making it difficult to pinpoint the perforation site or detect free air in the peritoneal cavity [7]. In Case 1, the initial CT scan did not confirm gastrointestinal perforation due to the artifacts caused by barium, and the patient was placed under observation. The perforation was ultimately detected during a follow-up scan after the patient's symptoms worsened. This highlights the need for clinicians to always consider the possibility that artifacts from barium may obscure diagnosis.
When gastrointestinal perforation due to barium occurs, the inflammatory response progresses rapidly, with a high risk of infection and sepsis; therefore, emergency surgery is essential. The first-choice surgical procedures are Hartmann's procedure or a colostomy [6]. It is crucial to resect the perforated bowel segment and thoroughly irrigate the peritoneal cavity where barium has leaked. Postoperatively, strict management in an intensive care unit is required, including the administration of antibiotics and supportive therapy aimed at early recovery of bowel function. If severe inflammation progresses, postoperative recovery may take an extended period, necessitating an appropriate treatment plan based on the degree of infection.
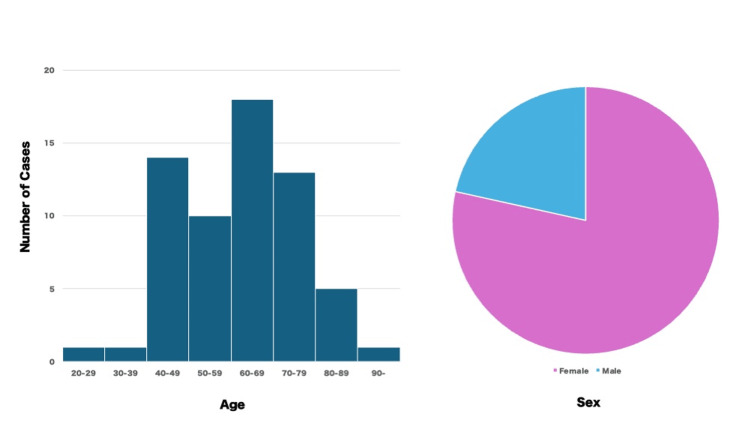
We reviewed 63 reported cases of colonic perforation following upper gastrointestinal barium examinations since 2000 [4,8-38]. The average age of patients was 61.6 years (ranging from 26 to 91 years), with the majority being middle-aged to elderly individuals in their 60s. Females accounted for 77.8% of the cases (Figure 7).
Figure 7. Age distribution histogram (left) and pie chart by gender (right).
Image Credits: Hideo Kidogawa
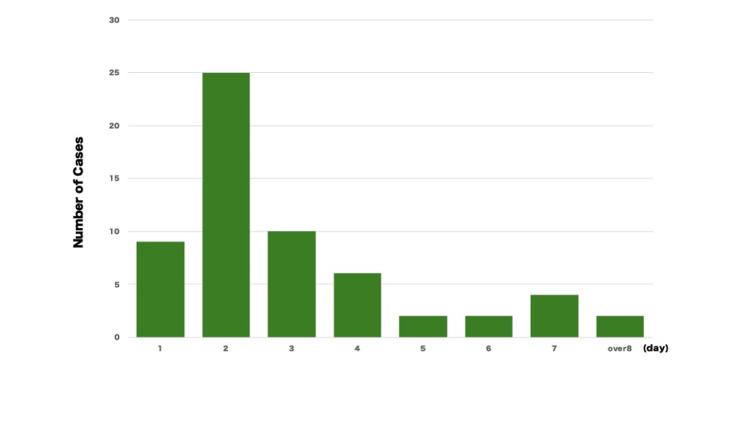
The most common time for symptom onset was within two days (Figure 8), although there was also a reported case where symptoms appeared 270 days later [9].
Figure 8. Days from examination to symptom onset.
Image Credits: Hideo Kidogawa
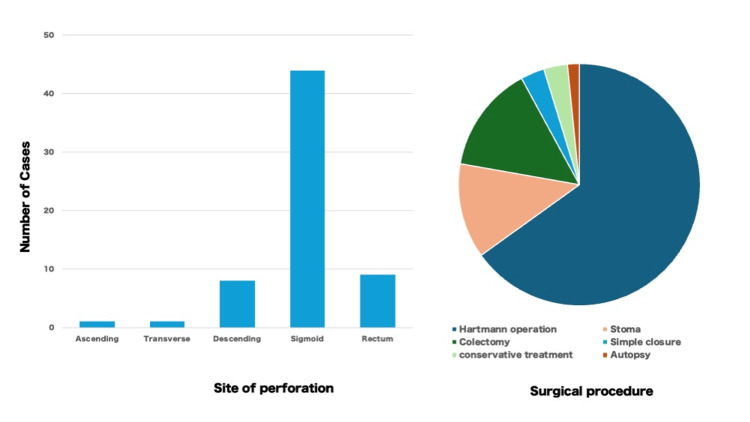
The most frequently affected site was the sigmoid colon (70.0%), followed by the rectum (14.3%) and the descending colon (12.7%). The most common surgical procedures were Hartmann's procedure or colostomy, comprising 77.8% of the cases, with some cases involving simple suture closure. The overall prognosis was generally favorable, though two fatalities were reported [35,38]. Many of the colostomy cases underwent stoma closure procedures several months later.
Figure 9. Site of perforation (left) and surgical procedure (right).
Image Credits: Hideo Kidogawa
All of these reported cases were from Japan, reflecting the country's unique gastric cancer screening system [1]. In Western countries, upper gastrointestinal barium examinations are performed only in symptomatic patients and are not used for routine health screenings. Barium examinations provide an indirect method of evaluating the gastric mucosa, and their diagnostic accuracy is inferior to that of endoscopy [39]. Although considered relatively safe, gastrointestinal perforation during barium examinations, though extremely rare, can lead to fatalities and require extensive surgical procedures, imposing a significant burden on patients. Minimizing the risk of severe complications is particularly important in asymptomatic individuals undergoing routine screenings.
In recent years, endoscopic examinations have increasingly been adopted for health screenings in Japan. This report highlights the rare but serious complication of colonic perforation following upper gastrointestinal barium examinations and underscores the importance of recognizing high-risk patients to improve screening safety.
Conclusions
We reported two cases of colonic perforation that occurred following an upper gastrointestinal series (UGIS) with barium as part of a health screening. This report provides important insights for considering the potential risks associated with UGIS in health screenings. Although the risk of gastrointestinal perforation due to barium is extremely rare, it can lead to significant complications, and early diagnosis and intervention are crucial to improving patient outcomes. It is time to consider transitioning to alternative screening methods, such as endoscopic examination.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Hideo Kidogawa, Ryo Nonomura, Toshihito Uehara, Shin Shinyama
Acquisition, analysis, or interpretation of data: Hideo Kidogawa, Kohji Okamoto
Drafting of the manuscript: Hideo Kidogawa, Ryo Nonomura, Toshihito Uehara, Shin Shinyama
Critical review of the manuscript for important intellectual content: Hideo Kidogawa, Shin Shinyama, Kohji Okamoto
Supervision: Kohji Okamoto
References
- 1.Nakajima S. Gastric Cancer. Gateway East, Singapore: Springer; 2019. Gastric cancer screening in Japan; pp. 99–117. [Google Scholar]
- 2.[Complications of gastric mass screening by indirect fluororadiography] Shibuya D, Konno Y, Aida S, Kato K, Shimada T. J Gastroenterol Cancer Screen. 2006;44:251–258. [Google Scholar]
- 3.Rectal perforations after barium enema: a review. de Feiter PW, Soeters PB, Dejong CH. Dis Colon Rectum. 2006;49:261–271. doi: 10.1007/s10350-005-0225-3. [DOI] [PubMed] [Google Scholar]
- 4.Eight cases of lower digestive tract perforation triggered by barium swallow in upper gastrointestinal series. Tsunokake J, Fujio A, Usuda M, Suzuki O, Teshima J, Miyata G. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Eight+cases+of+lower+digestive+tract+perforation+triggered+by+barium+swallow+in+upper+gastrointestinal+series&btnG= Journal of Japanese Society of Abdominal Emergency Medicine. 2021;82:120–126. [Google Scholar]
- 5.Rupture of the colon in the absence of any pathological abnormality. McPhedran NT. https://pubmed.ncbi.nlm.nih.gov/14176977/ Can J Surg. 1964;7:293–296. [PubMed] [Google Scholar]
- 6.Two cases with perforation of the large intestine after upper gastrointestinal series with barium. Tachioka M, Saito M, Abe I, et al. https://sciforschenonline.org/journals/surgery-open-access/JSOA-2-131.php J Surg Open Access. 2016;2:0. [Google Scholar]
- 7.[A case of colorectal perforation after a barium study] Bamba T, Umegae S, Noji M, Yamamoto T, Yuzawa H, Nakayama S. JJCS. 2015;76:813–816. [Google Scholar]
- 8.[A case of ischemic sigmoid perforation caused by giant barium stercoroma] Iso Y, Shimoda M, Nakano S, Rokkaku K, Yamamoto S, Kubota K. JJCS. 2002;63:1938–1942. [Google Scholar]
- 9.An unusual perforation of the colon: report of two cases. Matsuo S, Eguchi S, Azuma T, et al. Surg Today. 2002;32:836–839. doi: 10.1007/s005950200163. [DOI] [PubMed] [Google Scholar]
- 10.[Barium peritonitis caused by oral side perforation of cancer of the transverse colon following upper gastrointestinal radiography: report of a case] Tajima Y, Ishibashi K, Okada N, et al. Journal of Japanese Society of Abdominal Emergency Medicine. 2008;28:735–738. [Google Scholar]
- 11.[A case of barium peritonitis with prolonged postoperative inflammation] Tsutsumi N, Guntani A, Takahashi I, Nishizaki T, Ikejiri K. J Jpn Surg Assoc. 2009;70:1860–1863. [Google Scholar]
- 12.[Three cases of colorectal perforation due to barium retention after gastrography] Ukon K. J Jpn Surg Assoc. 2010;71:1560–1565. [Google Scholar]
- 13.[Descending colon perforation without organic disease following upper gastrointestinal radiography: a case report] Nakagawa H, Ono H, Miyauchi K. JJCS. 2010;65:1601–1604. [Google Scholar]
- 14.[A case of idiopathic perforation of the colon presenting with retroperitoneal emphysema] Dairaku K, Ueda K, Kamota T, Fujioka K. JJCS. 2010;71:137–140. [Google Scholar]
- 15.[A case of barium peritonitis causing postoperative empyema] Ogata S, Tagami T, Katakawa M, Bando Y. https://scholar.google.com/scholar?q=intitle:A%20case%20of%20barium%20peritonitis%20causing%20postoperative%20empyema Shikoku Medical Journal. 2011;67:65–70. [Google Scholar]
- 16.[A case of colorectal perforation after barium gastrography] Satani T, Watanabe Y, Shimazaki J, et al. Journal of the Japan Society of Coloproctology. 2012;65:65–69. [Google Scholar]
- 17.[A case of rectal perforation after gastrography] Matsuo R, Fukuzawa J, Ikeda O, Nakano J, Nakayama K. JJCS. 2012;73:87–90. [Google Scholar]
- 18.[A case of descending colon perforation caused by barium after gastric cancer screening] Okada A, Aotake T, Doi K, Tanaka F, Fujii H, Hirose Y. JJCS. 2012;73:3203–3206. [Google Scholar]
- 19.[A case of sigmoid colon perforation due to upper gastrointestinal radiography cured by conservative therapy] Kudo K, Suenaga Y, Kawamoto K, Iwagaki T, Sato H. JJCS. 2012;37:807–812. [Google Scholar]
- 20.[A case of sigmoid colorectal perforation due to barium retention after gastrography] Uchida E, Izumi M, Tsuchiya I, et al. Prog Dig Endosc. 2013;82:174–175. [Google Scholar]
- 21.[Three cases of colon perforation after upper gastrointestinal series using barium sulfate] Nogami M, Hirayama R, Otsuka R, Sawa M, Take H. https://onlinelibrary.wiley.com/doi/pdf/10.1002/jgf2.387 J Tokyo Women's Medical Univ. 2015;85:59–61. [Google Scholar]
- 22.[Steroid pulse therapy for barium peritonitis due to colonic perforation after fluoroscopy of the stomach] Tateno Y. JJCS. 2014;75:3094–3097. [Google Scholar]
- 23.[A case of colon perforation after an upper gastrointestinal barium series] Hamasaki K, Kawagoe K, Shibuya A, Fukuoka H, Sumida Y, Ishikawa H. JJCS. 2015;76:550–555. [Google Scholar]
- 24.[A case of survival after cardiopulmonary arrest caused by barium peritonitis due to colorectal perforation following upper gastrointestinal radiography] Sudo N, Kobayashi T, Hirose Y, Katada T, Takizawa K, Wakai T. Journal of Japanese Abdominal Emergency Medicine. 2015;35:119–124. [Google Scholar]
- 25.[A case of stercoral colonic perforation by barium in a young man with no underlying disease] Kinoshita M, Kataoka M, Tashiro M, Kato K, Kondo K. Journal of Japanese Abdominal Emergency Medicine. 2015;35:741–744. [Google Scholar]
- 26.[A case of colon perforation caused by fecaloma of barium after upper gastrointestinal radiography] Tsuchiya T, Yagi T, Tsukamoto M, et al. Journal of the Japan Society of Coloproctology. 2016;69:374–378. [Google Scholar]
- 27.[A case of rectal perforation without organic disease after upper gastrointestinal radiography] Kashiwabara T, Mizukami Y. Journal of Comprehensive Health Screening. 2016;31:486–491. [Google Scholar]
- 28.[A case of rectal perforation without organic disease by x-ray examination of the upper gastrointestinal tract] Kondo S, Kawai M. Journal of Gastrointestinal Cancer Screening. 2016;54:404–409. [Google Scholar]
- 29.[A case of necrosis of the abdominal wall caused by barium peritonitis due to colon perforation following upper gastrointestinal radiography] Tamura Y, Nakanishi N. J Jpn Soc Intensive Care Med. 2016;23:341–342. [Google Scholar]
- 30.[Four cases of colorectal injury after barium gastrography] Saida T, Shiigai M, Konishi T, Watanabe A, Ishiguro T, Atake S. Journal of Japanese Society of Abdominal Emergency Medicine. 2017;37:915–918. [Google Scholar]
- 31.[A case of sigmoid colon perforation after an upper gastrointestinal barium series] Kusano M, Komazawa D, Ito H, et al. Prog Dig Endosc. 2017;91:172–173. [Google Scholar]
- 32.[A case of colon perforation caused by barium retention after upper gastrointestinal radiography] Takayama H, Ikenaga M, Ohta K, et al. Jpn J Gastroenterol Surg. 2018;43:210–215. [Google Scholar]
- 33.[Two cases of colonic perforation after barium gastrography] Matsuno Y, Hagiwara K, Isagawa Y, et al. J Nihon Univ Med Ass. 2018;77:99–104. [Google Scholar]
- 34.[Five cases of colonic perforation following an upper gastrointestinal series] Tabe S, Shimizu H, Takanishi K, Otsuka M. Chiba Med J. 2019;95:147–151. [Google Scholar]
- 35.[Eight cases of colorectal perforation after an upper gastrointestinal series with barium] Shoji R, Aoyama K, Mikane Y, Okada T, Watanabe M, Shigemitsu K. Journal of Japanese Society of Abdominal Emergency Medicine. 2019;39:979–982. [Google Scholar]
- 36.[A case of sigmoid colon perforation following barium enema examination in health screening] Shin Y, Yamana I, Ichikawa J, et al. Journal of Japanese Society of Emergency Surgery. 2019;39:1095–1099. [Google Scholar]
- 37.[A case in which segmental absence of the intestinal musculature led to the development of colonic perforation after barium gastrography] Gochi M, Tani C, Otani M, et al. Journal of Japanese Society of Emergency Surgery. 2020;40:479–482. [Google Scholar]
- 38.Postmortem computed tomography of barium peritonitis due to descending colon perforation. Shinkawa N, Yanagita M, Yukawa N, Nagatomo T. Radiol Case Rep. 2024;19:2008–2012. doi: 10.1016/j.radcr.2024.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Comparing upper gastrointestinal X-ray and endoscopy for gastric cancer diagnosis in Korea. Lee HY, Park EC, Jun JK, Choi KS, Hahm MI. World J Gastroenterol. 2010;16:245–250. doi: 10.3748/wjg.v16.i2.245. [DOI] [PMC free article] [PubMed] [Google Scholar]