Abstract
Mutations in rRNA genes (rrn) that confer resistance to ribosomal inhibitors are typically recessive or weakly codominant and have been mostly reported for clinical strains of pathogens possessing only one or two rrn operons, such as Helicobacter pylori and Mycobacterium spp. An analysis of the genome sequences of several members of the Chlamydiaceae revealed that these obligate intracellular bacteria harbor only one or two sets of rRNA genes. To study the contribution of rRNA mutations to the emergence of drug resistance in the Chlamydiaceae, we used the sensitivities of Chlamydia trachomatis L2 (two rrn operons) and Chlamydophila psittaci 6BC (one rrn operon) to the aminoglycoside spectinomycin as a model. Confluent cell monolayers were infected in a plaque assay with about 108 wild-type infectious particles and then treated with the antibiotic. After a 2-week incubation time, plaques formed by spontaneous spectinomycin-resistant (Spcr) mutants appeared with a frequency of 5 × 10−5 for C. psittaci 6BC. No Spcr mutants were isolated for C. trachomatis L2, although the frequencies of rifampin resistance were in the same range for both strains (i.e., 10−7). The risk of emergence of Chlamydia strains resistant to tetracyclines and macrolides, the ribosomal drugs currently used to treat chlamydial infections, is discussed.
The Chlamydiaceae, formerly called Chlamydia, are obligate intracellular gram-negative bacteria which were recently divided in phylogenetic studies based on 16S rRNA and 23S rRNA gene sequence analyses into the two genera Chlamydia and Chlamydophila (10). In this new taxonomy, Chlamydia comprises the species Chlamydia trachomatis, its relative Chlamydia suis, and Chlamydia muridarum, and Chlamydophila currently includes Chlamydophila pneumoniae and Chlamydophila pecorum, in addition to Chlamydophila psittaci and the related Chlamydophila felis, Chlamydophila caviae, and Chlamydophila abortus. C. trachomatis and C. pneumoniae are mainly pathogens of humans, and the other chlamydial species mainly infect animals (13). However, severe zoonotic diseases have also been reported for C. psittaci, C. abortus, and C. felis. Infections associated with chlamydiae can evolve from a primarily acute phase with relatively mild symptoms to a chronic stage with significant damage to the host from the inflammatory response and tissue fibrosis or scarring. For example, C. pneumoniae is a prevalent cause of community-acquired respiratory tract infections and may contribute to chronic pulmonary disease, in addition to Alzheimer's disease and cardiovascular diseases such as atherosclerosis and stroke. C. trachomatis is responsible for ocular infections and trachoma that can lead to blindness. C. trachomatis is also the major agent of sexually transmitted diseases and can result in pelvic inflammatory disease, infertility, and reactive arthritis (13).
In acute disease, chlamydia development alternates from infectious elementary bodies (EBs) that can survive extracellularly to strictly intracellular reticulate bodies (RBs) that multiply in the cytoplasm of a susceptible host cell within a nonfusogenic vacuole termed an inclusion (81). At 18 to 48 h postinfection, depending on the species, increasing numbers of RBs convert back to infectious EBs as the remaining RBs continue to multiply until the cell lyses, enabling the EB progeny to pursue the infection by invading neighboring cells. Morphologically aberrant forms of chlamydiae (recently reviewed in reference 31) have been identified during chronic infections (53, 70), as well as in the laboratory in response to adverse environmental conditions such as nutrient depletion (12, 60), inflammatory cytokines (5, 57), and even antibiotic treatment. Indeed, abnormal chlamydial forms have been observed in infected cultures exposed to penicillin (40), ampicillin (79), d-cycloserine (51), sulfonamides (27), fluoroquinolones (16, 24), doxycycline (24), erythromycin (24), and azithromycin (7, 18). The specific inhibition of RB-to-EB differentiation leads to the formation of enlarged, nondividing, but viable chlamydial forms that can potentially revert back to typical RBs with maturation to infectious EBs after removal of the inducer. These so-called persistent bodies are characterized by an abnormal metabolic activity and consequently appear more resistant to conventional antibiotics that target the transcription, translation, or cell division of metabolically active organisms (16, 18, 41, 42).
In recent years, the use and overuse of antimicrobial agents have resulted in an increase in the appearance of antibiotic-resistant bacteria, which poses a growing public health problem. Although chlamydial infections are characterized by a 5 to 20% recurrence rate despite appropriate drug therapy (6, 29, 38, 78), relapses or persistent infections result mainly from patient failure to comply with medication, from repeated infections, or from phenotypic “resistance” associated with the persistent state of the bacteria rather than from real genotypic resistance due to chromosomal mutations (72). Since the chlamydial life cycle occurs in relative isolation, the opportunity for the acquisition of antibiotic resistance genes from other organisms is limited, and indeed, the acquisition of drug resistance in chlamydiae by horizontal gene transfer has been suggested for only one tetracycline-resistant isolate of C. suis, a pig pathogen (20). However, studies in the laboratory have shown that Chlamydia spp. share the same mutational mechanisms as other bacteria. Experiments involving serial exposures to subinhibitory concentrations of antimicrobials in cell culture have revealed that drug resistance can arise in Chlamydia spp. through point mutations that result in the overexpression or alteration of the inhibitor target. For example, increased expression of the ribonucleotide reductase confers resistance to hydroxyurea (67), whereas amino acid substitutions in the CTP synthetase (80), the β subunit of RNA polymerase (RpoB) (17), and DNA gyrase (GyrA) (15) confer stable and high-level resistance in C. trachomatis to cyclopentenyl cytosine, rifampin, and the fluoroquinolones ofloxacin and sparfloxacin, respectively.
Nevertheless, we still lack knowledge on the frequency of the appearance of resistance in Chlamydia spp. For this study, we determined the frequencies of spontaneous resistance of the sensitive Chlamydiaceae to spectinomycin and rifampin by using a plaque assay. Rifampin was chosen due to the highly specific nature of resistance, since single mutations in only one gene, rpoB, have been shown to confer high-level resistance on numerous bacteria, including C. trachomatis (17). Spectinomycin was used as a model drug for the ribosome-targeted antibiotics currently used to treat chlamydial infections (tetracyclines and macrolides). We show that spontaneous mutations arise in vitro in C. trachomatis L2 and C. psittaci 6BC at frequencies similar to those in other eubacteria. In particular, the number of ribosomal operons in the organism affected the recovery of spectinomycin-resistant variants but not of rifampin-resistant variants. The implications of these results on the antibiotic treatment of chlamydial infections are discussed.
MATERIALS AND METHODS
Bacterial strains and antibiotics.
The bacterial strains used for this study are listed in Table 1. Escherichia coli strain DH5α was used for cloning purposes. E. coli was grown in Luria-Bertani broth with aeration or on Luria-Bertani agar. Antibiotics (all purchased from Sigma) were added at the following concentrations, when required: 100 μg ml−1 ampicillin, 25 μg ml−1 chloramphenicol, 50 μg ml−1 kanamycin, 7.5 μg ml−1 tetracycline, and 20 μg ml−1 gentamicin (Gen). Various concentrations of spectinomycin (Spc) and rifampin (Rif) were used.
TABLE 1.
Bacterial strains used for this study
| Strain | Description | Source or reference |
|---|---|---|
| C. trachomatis | ||
| L2 | Biovar lymphogranuloma venereum L2/434/Bu | H. Caldwell |
| L2R1 | Serovar L2 rpoB1, Rifr | This work |
| C. psittaci | ||
| 6BC | Serovar 6BC | T. Hatch |
| BCR1 | Serovar 6BC rpoB2, Rifr | This work |
| BC0E1 | Serovar 6BC 16S1, Spcr | This work |
| BC0A2 | Serovar 6BC 16S2, Spcr | This work |
| BCS18 | Serovar 6BC 16S3, Spcr | This work |
| BCS34 | Serovar 6BC 16S4, Spcr | This work |
| E. coli | ||
| DH5α | F−φ80Δ(lacZY-argF)U169 deoR recA1 endA1 phoA hsdR17 supE44 λ−thi-1 gyrA96 relA1 Δ(lacZ)M15 | 28 |
Propagation of C. trachomatis, C. psittaci, and L2 cells.
C. trachomatis serovar L2/LGV/434/Bu and C. psittaci serovar 6BC were grown in mouse fibroblast L2 cells. L2 cells were maintained in Dulbecco's modified Eagle medium (DMEM; GIBCO) supplemented with 10% fetal bovine serum (FBS) at 37°C in an atmosphere of 5% CO2. Mouse fibroblast L2 cell monolayers were infected with Chlamydia spp. diluted in SPG (250 mM sucrose, 10 mM sodium phosphate, 5 mM l-glutamic acid) at a multiplicity of infection (MOI) of 1. Infected L2 cells were incubated for 44 h in DMEM supplemented with 10% FBS, 20 μg of Gen per ml, and 1 μg of cycloheximide per ml. EBs were harvested after sonication of the infected cells, divided into aliquots, and stored at −80°C in SPG.
Titration, antimicrobial susceptibility, and isolation of chlamydial mutants by plaque assay.
Confluent monolayers of mouse fibroblast L2 cells in 60-mm2 dishes were infected at 37°C in 5% CO2 with serial dilutions of crude chlamydial stocks. After a 2-h infection time, the inoculum was replaced with an agarose overlay (0.25% Seakem GTG agarose [FMC Bioproducts]) containing DMEM, FBS (10%), cycloheximide (0.2 μg ml−1), 1× NEM nonessential amino acids (Sigma-Aldrich), and Gen (20 μg ml−1) or various concentrations of Rif or Spc, when appropriate. On day 7, a second agarose overlay containing the same components as the first was added. The cells were stained with 0.5% neutral red for 3 h at 37°C in 5% CO2 to visualize the chlamydial plaques at the end of the incubation period (between 10 and 14 days postinoculation [p.i.]). Individual plaques were scraped with a pipette tip using 4 μl of sterile H2O, suspended in 1.5-ml microcentrifuge tubes that contained 200 μl of SPG, and frozen at −80°C. Samples were expanded in a plaque assay in the presence of the same concentration of antibiotic used beforehand, and a second round of purification of individual plaques was performed before further characterization.
To monitor the stability of resistance, we expanded each variant for a minimum of 4 days in the absence of antibiotic selection and then collected the variants. The numbers of PFU obtained in a plaque assay in the absence and presence of the antibiotic were compared.
The MIC was defined as the drug concentration that inhibited the development of 105 chlamydial PFU in a confluent L2 monolayer in a 60-mm2 dish. This inoculum size resulted in the infection of approximately 1 in 100 cells in the monolayer. For the isolation of spontaneous drug-resistant variants, 60-mm2 dishes were infected with 107 to 108 PFU (MOI, 1 to 10), and the drug was added at 2 h p.i. at a concentration high enough to inhibit the cytotoxicity associated with the inoculum size. The frequency of spontaneous mutation to drug resistance was determined by dividing the number of PFU on selective medium by the number of PFU added to the monolayer (as measured by the titration of PFU in the absence of antibiotics).
Cloning and sequencing of chlamydial rpoB and 16S rRNA genes.
Total genomic DNAs were prepared from infected cells with DNeasy tissue kits (QIAGEN). To detect changes in the rpoB sequence that were associated with rifampin resistance, we amplified the gene with its promoter region by using Ultra Pfu High-Fidelity DNA polymerase (Stratagene) and degenerate primers based on the available genome sequences of C. trachomatis serovar D, C. muridarum, and C. caviae GPIC (GenBank accession numbers NC000117, NC002620, and NC003361, respectively). The 4,294-bp and 4,036-bp fragments amplified from C. trachomatis L2 and C. psittaci 6BC, respectively, by use of the primers RpoB-F [5′-GGATTAGCTTT(A/G)AAAGAAGCTAAAGAAATGAC-3′] and RpoB-R [5′-CAT(T/C)GTCTCGAGAACCTTCTC(T/C)GAACAT-3′], were cloned into pPCR-Script Cam SK(+) (Stratagene) and sequenced. This experiment was repeated twice to confirm the rpoB sequence.
To detect changes in the 16S rRNA gene sequences associated with spectinomycin resistance, we amplified a 1,584-bp DNA fragment encoding the 16S rRNA of C. psittaci 6BC by using the primers 16SF1 (5′-AGAATTTGATCTTGGTTCAGATTG-3′) and 16SR1 (5′-CCTAGTCAAACCGTCCTAAGACAG-3′), designed from the sequence of the C. psittaci 6BC 16S rRNA (GenBank accession number AB001778). The amplified products were cloned into pGEMT (Promega) and sequenced. Alternatively, a 537-bp DNA fragment containing the helix 34 region of the 16S rRNA was amplified by using 16S1 (5′-GCATCTAATACTATCTTTCTAGAGGG-3′) and 16S2 (5′-AACCCAGGCAGTCTCGTTAG-3′) and then sequenced.
DNA sequences were aligned with Clone Manager 5 software (Scientific & Educational Software, Durham, N.C.) to identify the mutations present in the antibiotic-resistant chlamydial variants.
Southern blot analysis.
C. psittaci 6BC genomic DNA was prepared by use of a QIAGEN genomic kit from highly purified preparations of EBs obtained by centrifugation through Renocal-76 (Bracco Diagnostics, Princeton, N.J.) density gradients. Aliquots of chromosomal DNA were digested with various restriction endonucleases and analyzed by Southern gel transfer and hybridization with a nonradioactive labeled probe. A 537-bp DNA fragment internal to the C. psittaci 6BC 16S gene was labeled with digoxigenin-11-dUTP (Boehringer Mannheim) by PCR amplification using the 16S1 (5′-GCATCTAATACTATCTTTCTAGAGGG-3′) and 16S2 (5′-AACCCAGGCAGTCTCGTTAG-3′) primers based on the nucleotide sequence of the C. psittaci 6BC 16S rRNA gene (GenBank accession number AB001778). Hybridization and immunological detection of the probe were performed as described by Panaud et al. (56), using the enhanced chemiluminescence detection system (Amersham Pharmacia) according to the manufacturer's directions. An analysis of the restriction fragments that hybridized with the probe indicated that C. psittaci 6BC contained only one copy of the 16S rRNA gene (data not shown).
Nucleotide sequence accession numbers.
The rpoB sequences determined in the present study have been deposited in GenBank under accession numbers AY826975 for C. trachomatis L2 and AY826976 for C. psittaci 6BC.
RESULTS
Use of a plaque assay to measure drug inhibitory concentrations for Chlamydia spp.
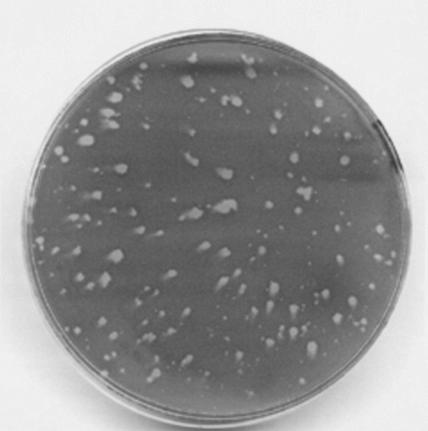
We measured the sensitivities of C. trachomatis L2 and C. psittaci 6BC to rifampin or spectinomycin by using a plaque assay. This assay is based on the ability of these obligate intracellular bacteria to invade and lyse mouse fibroblast L2 cells in a confluent monolayer (3). An agarose overlay containing all of the nutrients necessary to sustain cell viability is applied to the cell monolayer at the end of the invasion time, i.e., at 2 h p.i., so that infectious particles released from the infected cells can only reinfect neighboring cells. Consequently, the initial infection of a single eucaryotic cell by a single EB will lead to the formation of an individual plaque that can be visualized after staining of the monolayer. Plaques formed by C. trachomatis were observed at 14 days p.i., as reported previously (48). Plaques formed by C. psittaci 6BC were usually observed at 10 days p.i. (Fig. 1).
FIG. 1.
C. psittaci 6BC plaques at 10 days postinoculation. Each plaque, visualized here after neutral red staining of the cells, represents a clonal population of a single infectious particle from the initial infection that can be further purified and expanded.
We observed a dose-dependent effect of rifampin (Rif) and spectinomycin (Spc) on the inhibition of plaque formation for both C. trachomatis L2 and C. psittaci 6BC (Table 2). We defined the MIC as the lowest concentration of drug that inhibited the visible development of 105 PFU. This inoculum size reflects the standard established for numerous extracellular bacterial strains and corresponds to a multiplicity of infection (MOI) of about 0.01 in a plaque assay using 60-mm2 dishes. We observed a slight difference between the Rif MICs for the two chlamydial species, with C. psittaci 6BC being more resistant than C. trachomatis L2 (MICs of 25 ng/ml and 5 ng/ml, respectively). When the cell monolayer was inoculated with 107 to 108 PFU of either strain in the presence of a minimum of 50 ng/ml of Rif, a few plaques were visualized after staining of the cell monolayer.
TABLE 2.
Effect of rifampin and spectinomycin on chlamydial plaque formation
| Antibiotic | Drug concn (ng/ml [Rif] or μg/ml [Spc]) |
C. psittaci 6BC
|
C. trachomatis L2
|
||
|---|---|---|---|---|---|
| Input PFUa | No. of plaquesb | Input PFUa | No. of plaquesb | ||
| Rif | 2 | NT | NA | 2.4 × 103 | Too many to count |
| 5 | NT | NA | 2.4 × 105 | 0 | |
| 10 | 4.8 × 104 | 0 | 2.2 × 105 | 0 | |
| 25 | 4.8 × 105 | 0 | 2.2 × 106 | 0 | |
| 50 | 2.1 × 107 | 42 | 2.8 × 107 | 2 | |
| 100 | 108 | 50 | 2.2 × 107 | 1 | |
| 200 | 108 | 23 | 6.4 × 107 | 2* | |
| Spc | 20 | 1.1 × 105 | 0 | 2.4 × 103 | Too many to count |
| 40 | 2.9 × 105 | 0 | 2.4 × 105 | 0 | |
| 100 | 2.0 × 106 | 0 | 1.9 × 106 | 0 | |
| 200 | 2.1 × 107 | 13 | 2.3 × 107 | 0 | |
| 300 | 108 | 81 | 4.6 × 107 | 0* | |
The largest inoculum size tested that was not cytotoxic.
The average number of plaques (minimum of three independent experiments). NT, not tested; NA, not applicable; *, cell monolayer was unhealthy due to the large concentration of infectious particles.
The same assay was performed in the presence of spectinomycin (Spc), an aminoglycoside that targets the 30S subunit of bacterial ribosomes. Although C. trachomatis L2 and C. psittaci 6BC were both sensitive to Spc, with MICs of 40 μg/ml and 20 μg/ml, respectively, only large inocula of C. trachomatis, containing up to 5 × 107 PFU, were completely inhibited by the antibiotic at a concentration of 200 or 300 μg/ml. Under the same conditions, a few C. psittaci 6BC plaques survived drug selection (Table 2).
Molecular characterization of rifampin and spectinomycin resistance in Chlamydia spp.
We hypothesized that the plaques surviving a high concentration of antibiotic resulted from infection with spontaneous chlamydial variants that were resistant to the drug. Two Rif-resistant (Rifr) plaques, BCR1 and L2R1, selected from C. psittaci 6BC and C. trachomatis L2, respectively, in the presence of 200 ng/ml of Rif, and six independent C. psittaci plaques selected in the presence of 300 μg/ml of Spc were plaque purified twice and expanded in the presence of the antibiotic. The stability of the resistance acquired was then tested by growth in the absence of selective pressure (i.e., no antibiotic). For the Rifr variants, a single plaque from L2R1 or BCR1 was first expanded by growth in a 60-mm2 L2 cell confluent monolayer for 46 h, harvested, expanded in a 175-cm2 flask for another developmental cycle, and then harvested again. For the Spc-resistant (Spcr) variants, single plaques were purified two successive times in a plaque assay in the absence of the drug. The titers of the final harvests were similar in the plaque assay in the presence or absence of the antibiotic, indicating that the resistance phenotypes of these eight chlamydial mutants were stable (data not shown).
In many bacteria, rifampin resistance is due to mutations in the rpoB gene, which encodes the β-subunit of the RNA polymerase (77). We used degenerate primers to amplify the rpoB region from L2R1, BCR1, and the two wild-type chlamydial parents and sequenced the genes. The C. trachomatis L2 and C. psittaci 6BC rpoB open reading frames share 79% identity at the nucleotide level and 91% identity at the amino acid level. Single base-pair substitutions were identified in the rpoB sequences of the two Rifr variants, creating two different alleles (designed rpoB1 and rpoB2 for L2R1 and BCR1, respectively) (Table 3). Both alleles conferred a high level of Rif resistance on Chlamydia spp., with an MIC of 800 ng/ml for rpoB1 and 300 ng/ml for rpoB2. Amino acid substitutions at homologous sites in RpoB have been previously characterized for other Rifr mutants of bacterial strains (52, 76).
TABLE 3.
Nucleotide differences identified in rifampin- and spectinomycin-resistant isolates of C. psittaci 6BC and C. trachomatis L2
| Mutant strain | No. of independent mutations analyzed
|
Characteristic of mutant allelea
|
MIC | ||||
|---|---|---|---|---|---|---|---|
| Total | Distribution | Designation | Nucleotide change | Representative chlamydial mutant | Allele distribution in drug-resistant organisms | ||
| C. trachomatis L2 Rifr | 1 | 1 | rpoB1 | GAU→GGU (Asp516→Gly) | L2R1 | Mycobacterium tuberculosis, Helicobacter pylori | 800 ng/ml |
| C. psittaci 6BC Rifr | 1 | 1 | rpoB2 | AUG→AUC (Met515→Ile) | BCR1 | M. tuberculosis | 300 ng/ml |
| C. psittaci 6BC Spcr | 59 | 52 | 16S1 | C1192U | BC0E1 | E. coli, Neisseria sp., Nicotiana tabacum chloroplasts | >10 mg/mlb |
| 5 | 16S2 | A1191G | BC0A2 | Chlamydomonas reinhardtii chloroplasts | >10 mg/mlb | ||
| 1 | 16S3 | C1192G | BCS18 | E. coli | >10 mg/mlb | ||
| 1 | 16S4 | G1193C | BCS34 | Not previously reported | 5 mg/ml | ||
Each distinct mutation identified was given an allele name (designation), which represents a specific change (E. coli numbering) at the indicated nucleotide in the rpoB or 16S rRNA sequence.
Spc concentrations above 10 mg/ml were cytotoxic to mouse fibroblast cells in the monolayer.
Resistance to Spc due to modifications in the 16S rRNA drug target is well characterized in E. coli, Neisseria spp., and Mycobacterium smegmatis (21; http://server1.fandm.edu/departments/Biology/Databases/16SMDBexp.html). Sequencing of the 16S rRNA genes of six independent C. psittaci Spcr isolates indicated that all but one had a C-to-U substitution in the 16S rRNA at position 1192 (E. coli numbering) (Table 3). This mutation, designated the C. psittaci 6BC mutant 16S1 allele present in the chlamydial isolate BC0E1, confers a high level of Spc resistance on E. coli and Neisseria spp. and on Nicotiana tabacum chloroplasts. In contrast, 16S2, the allele identified in the BC0A2 Spcr variant, contains an A-to-G substitution in the 16S rRNA at position 1191 in the E. coli numbering system. This mutant allele has been identified only in Spcr chloroplasts. Both alleles increased the Spc MIC of C. psittaci 6BC >500-fold (Table 3).
Frequency of spontaneous mutations conferring rifampin or spectinomycin resistance on Chlamydia spp.
Each independent antibiotic-resistant variant of C. trachomatis L2 and C. psittaci 6BC, obtained from individual plaques surviving a high concentration of drug, contained a point mutation in the gene encoding the target of the antibiotic. Consequently, the frequency of spontaneous antibiotic resistance can be determined by dividing the number of mutant plaques that form on selective medium by the number of PFU added to the monolayer. The frequencies of spontaneous Rif resistance were of the same order of magnitude for C. trachomatis L2 and C. psittaci 6BC, i.e., 2 × 10−7 and 7 × 10−7, respectively. The rate of spontaneous resistance to Spc for C. psittaci 6BC was about 10 times higher, i.e., 10−6 (Table 4).
TABLE 4.
Frequencies of spontaneous mutation to rifampin or spectinomycin resistance in Chlamydia spp.a
| Strain | Mutation frequency in presence of drug
|
|
|---|---|---|
| Rif (200 ng/ml) | Spc (300 μg/ml) | |
| C. trachomatis L2 | ||
| Wild type | 1.55 × 10−7 ± 1.44 × 10−7 | <3.60 × 10−8 |
| L2R1 | NAc | <2.40 × 10−8 |
| C. psittaci 6BC | ||
| Wild type | 7.34 × 10−7 ± 6.23 × 10−7 | 1.12 × 10−6 ± 1.70 × 10−6 |
| Wild type after three passagesb | 1.90 × 10−8 ± 0.7 × 10−8 | 4.48 × 10−5 ± 0.89 × 10−5 |
| BCR1 | NA | 2.23 × 10−7 ± 1.59 × 10−7 |
| BC0E1 | 7.54 × 10−8 ± 3.38 × 10−8 | NA |
The frequency of spontaneously resistant mutants was calculated as described in Materials and Methods. Data are means ± SD.
Infectious particles from a single plaque were expanded during three developmental cycles to obtain a recent clonal population of C. psittaci 6BC.
NA, not applicable.
The frequency of mutation measures all mutants present in a given population, irrespective of whether the mutations occurred early or late during the growth of the population. Consequently, the Rif and Spc mutation frequencies obtained for our C. psittaci 6BC wild-type stock were compared with the values obtained for an early clonal population of the same strain, obtained from a single plaque which was expanded three times. The mutation frequencies were of the same order of magnitude, but with a smaller standard deviation for the recent bacterial population (Table 4). On the other hand, the frequencies of spontaneous resistance obtained with BCR1 and BC0E1 were lower than those seen with the wild-type strain, suggesting some incompatibility between the rpoB2 or 16S1 allele and additional mutations in the 16S rRNA or the rpoB gene, respectively (37). No Spcr plaques were ever detected with wild-type C. trachomatis L2 or L2R1. Therefore, the frequency of spontaneous Spcr mutation for this species was below the limit of detection, i.e., < 2.4 × 10−8.
Mutations in rRNA genes are generally recessive or codominant, and the expression of the resistant phenotype requires that a majority of the cellular rRNA be of the mutant form (63). Consequently, the number of rRNA operon copies present in the genome affects the frequency of spontaneous resistance to ribosomal antibiotics. Indeed, the genome sequence of C. trachomatis revealed the presence of two identical ribosomal operons (73). Our inability to isolate spontaneous Spcr variants of C. trachomatis L2 is consistent with the presence of multiple rRNA operons in this strain. On the other hand, Southern hybridization of a 16S rRNA probe indicated the presence of a single ribosomal operon in the C. psittaci 6BC genome (data not shown).
Spectrum of spontaneous Spcr mutations in C. psittaci 6BC.
We isolated 53 additional C. psittaci Spcr variants obtained from individual Spcr plaques purified once and expanded in the presence of the antibiotic. Sequencing of the 16S rRNA helix 34 region revealed that 46 mutants had the same C1192U mutation as that found in BC0E1 and 5 mutants had the same A1191G mutation as that found in BC0A2. Two new alleles conferring high levels of Spc resistance to C. psittaci 6BC were identified (Table 3). The 16S3 allele present in BCS18 carried a C1192G mutation that was previously identified in Spcr E. coli(http://server1.fandm.edu/departments/Biology/Databases/16SMDBexp.html). Interestingly, the 16S4 allele present in BCS34 harbored a G1193C transition that has never been reported. However, an A substitution at the same position has been identified in Spcr chloroplasts of Chlamydomonas reinhardtii.
DISCUSSION
Because chlamydiae are obligate intracellular bacterial pathogens, drug susceptibilities have traditionally been studied by adding various concentrations of test antibiotics to infected cultured animal cells and detecting the bacteria by direct immunofluorescence. The MIC, the standard measure of antibiotic activity in vitro, has been defined as the lowest antibiotic concentration that completely inhibits the inclusion formation of generally 103 to 104 infectious particles after 48 to 72 h of incubation in cells grown in 48- or 96-well microtiter plates (25, 75). For our study, susceptibility tests were performed with a plaque assay using a 60-mm2 confluent L2 monolayer. This assay uses the ability of the bacteria to lyse the host cells and form plaques resulting from infection and spreading of a single EB over several successive infection and development cycles. In some aspects, a chlamydial plaque can be seen as similar to a bacterial colony on an agar plate, as each plaque/colony represents a clonal bacterial population that can be purified and expanded. In an early study, Banks et al. showed plaque formation by >100 chlamydial isolates of mammalian, avian, and human origins, including C. trachomatis biovar LGV (3). Later, Matsumoto et al. reported plaque formation by C. trachomatis serovars C, D, F, H, I, and L2 and by C. psittaci Cal10 (47). Recently, the assay was modified to isolate and purify clonal variants of C. pneumoniae, including strains AR-39, TW-183, and CWL-029 and the clinical isolate MUL-250 (23). In our study, we extended the plaque assay to C. psittaci 6BC and found that it formed plaques with diameters ranging from 0.5 to 1.5 mm at 10 days p.i. When the antibiotic was added at 2 h p.i., we observed that the inhibitory concentration of the antibiotic was dependent on the size of the chlamydial inoculum. This result was expected, as the presence of bacteria growing at a high density can confer a low level of antibiotic resistance (46). Therefore, we defined the MIC as the lowest antibiotic concentration that completely inhibited the plaque formation of 105 infectious particles, as this inoculum size reflects the current standard established for determining MICs for extracellular bacteria (2). Interestingly, the rifampin MIC for C. trachomatis in the plaque assay, i.e., 5 ng/ml, was similar to the MIC determined by the traditional methodology, i.e., 7.5 ng/ml, when the same multiplicity of infection (i.e., 0.01) was tested (17). This indicates that the MOI rather than the inoculum size per se is the critical parameter for reproducible MICs for chlamydiae.
Although the Chlamydiaceae have been shown to be highly sensitive to rifamycins, the rapid emergence of resistance to these drugs was observed in vitro as early as 1973, and their use in the treatment of chlamydial infections has been avoided (39). Rifampin is a hydrophobic antibiotic and consequently employs passive diffusion to cross the four biological membranes—host cell, inclusion, and RB inner and outer membranes—exerting its inhibitory action by binding to the β subunit of the bacterial RNA polymerase (RpoB). Sequencing of the rpoB genes from C. trachomatis L2 and C. psittaci 6BC revealed that their open reading frames are 91% identical at the amino acid level. Yet C. psittaci 6BC appeared five times less sensitive to rifampin than C. trachomatis L2. The dissimilarity in sensitivity to rifampin between the two strains may be due to differences in the drug's affinity for the two proteins. It has been shown that serial passaging of C. trachomatis in subinhibitory concentrations of rifampin, penicillins, sulfonamides, or fluoroquinolones allows the selection of bacterial populations resistant to the respective antibiotic (72), but the multiple steps involved in this process make it impossible to determine the frequency of drug resistance. Dreses-Werringloer et al. isolated Rifr C. trachomatis variants by using an in vitro model of continuous infection of HEp-2 cells for up to 20 days, with the drug being added at 2 days p.i. (17). A molecular characterization of five Rifr variants identified two different mutations leading to two amino acid substitutions in RpoB that were previously identified in other Rifr bacteria. Whereas the chlamydial variants harboring an Ala-to-Val change at codon 522 (E. coli numbering) showed a MIC of 4 μg ml−1, the replacement of His526 with Tyr conferred a MIC of either 64 or 256 μg ml−1, suggesting that the extended incubation time with the antibiotic selected for multiple mutations conferring a higher resistance level. In addition, the authors demonstrated the presence of extensive genetic variations in each C. trachomatis mutant. Consequently, the phenotype observed for these bacterial populations reflected the sum of many individual genotypes.
With the plaque assay, when we infected cells with C. trachomatis L2 or C. psittaci 6BC at an MOI of >1, i.e., 107 infectious particles, plaques surviving the presence of rifampin at a concentration at least 10 times the MIC appeared for both strains at a frequency of 10−7 to 10−8. This is the first time that a frequency of spontaneous mutation has been determined for any phenotype of chlamydiae, and strikingly, this frequency falls within the spontaneous Rifr frequencies determined for E. coli (33), Helicobacter pylori (76), Listeria monocytogenes (50), and Mycobacterium tuberculosis (45). Even though we limited our study to C. trachomatis and C. psittaci, it is reasonable to suppose that similar types of mutation can arise in other members of the Chlamydiaceae because of their close genetic relationship. The RpoB amino acid sequences from two chlamydial Rifr variants revealed the presence of single substitutions at positions 515 and 516 (E. coli numbering) which were previously identified in other Rifr bacterial species. Whereas Asp516 has been recognized as an important Rif binding site, mutations affecting Met515 have not been described as frequently for Rifr bacteria. This amino acid has been identified in close proximity to σ70 in the E. coli RNA polymerase holoenzyme complex (55). Consequently, mutations at this position may affect the efficacy of transcriptional initiation and could have a serious impact on the physiology of the resistant bacteria.
Tetracycline or its derivative doxycycline and macrolides such as azithromycin and erythromycin are currently the antibiotics of choice for Chlamydia spp. These antibiotics target the ribosome by binding to the 16S or 23S rRNA and consequently affect bacterial translation (19). Resistance to ribosome-targeting antibiotics due to mutations in rRNA genes has been observed mainly in pathogens possessing low copy numbers of rRNA operons because the selective advantage of a mutation in one rRNA gene copy is usually masked by the abundance of wild-type drug-sensitive rRNAs transcribed from unmutated gene copies. Interestingly, chlamydiae harbor one or two rRNA operons, depending on the species. Genome sequence analysis or hybridization with an rRNA probe revealed that C. trachomatis and C. muridarum harbor two homologous rRNA sets, whereas C. psittaci 6BC carries a unique rRNA operon, similar to C. pneumoniae and C. caviae (also called C. psittaci GPIC) (36, 61, 62). Therefore, rRNA mutation is a feasible and likely mechanism of resistance to drugs used in clinical settings.
For this study, we used the aminoglycoside spectinomycin (Spc) as a model antibiotic to monitor the potential development of chlamydial resistance by mutations in rRNA genes. Due to their low level of intracellular penetration, aminoglycosides are considered poorly active or inactive against obligate intracellular bacteria, and indeed, their ability to inhibit chlamydial growth is essentially nil at any clinically relevant concentration. However, earlier reports indicated that high concentrations of Spc could inhibit the development of C. trachomatis and C. psittaci in vitro (34, 43). We confirmed these observations with our plaque assay and showed that the Spc MICs for C. trachomatis L2 and C. psittaci 6BC were 40 and 20 μg/ml, respectively. In addition, we clearly demonstrated that distinct mutations within the 16S rRNA gene result in Spc resistance in C. psittaci 6BC. The 59 independent mutants analyzed carried a total of four different single point mutations located in the upper stem of the phylogenetically conserved helix 34. Data obtained from crystal structure, chemical footprinting, and mutagenesis experiments revealed that Spc interacts directly with the G1064-C1192 base pair (E. coli numbering system), where it inhibits peptidyl-tRNA translocation by preventing the binding of elongation factor G to the ribosome (8, 11). As expected, the majority of C. psittaci 6BC Spcr isolates had a mutation at position 1192, therefore perturbing the drug-binding pocket. The rest of the mutations affected the neighboring nucleotides at positions 1191 and 1193, which were previously characterized only for Spcr chloroplasts. Interestingly, phylogenetic and genomic analyses have linked the Chlamydiaceae with the cyanobacterial/chloroplast lineage (9). However, expression of the A1191G mutation in recombinant E. coli strains gave rise to Spcr, suggesting that the low content of rRNA operons shared by C. psittaci and tobacco or Chlamydomonas chloroplasts, rather than their proposed phylogenetic relationship, was involved in the recovery of such mutants (R. Binet and A. T. Maurelli, unpublished results). Whereas additional mutations at positions 1066 and 1064 have been associated with Spcr in E. coli, chloroplasts, and Neisseria meningitidis, we have not found any evidence of Spcr-associated mutations at equivalent locations within the 16S rRNA gene of any resistant C. psittaci strain. In the absence of a genetic system for chlamydiae, we cannot determine at this time if any of these mutations would be deleterious to the organism.
C. psittaci 6BC Spcr variants arose at a frequency of 5 × 10−5. On the other hand, the development of Spc resistance in C. trachomatis L2 was below the level of detection of the plaque assay, i.e., <2.4 × 10−8, in agreement with the larger ribosomal operon copy number in this strain. In support of our results, the frequency of appearance of spontaneous resistance to the aminoglycoside amikacin is as high as 10−5 for Mycobacterium chelonae and Mycobacterium abscessus, which contain a unique ribosomal operon (59). On the other hand, M. smegmatis fails to develop spontaneous mutants resistant to the aminoglycoside hygromycin B unless one of the two chromosomal rRNA copies is previously inactivated (58). Thus, it appears that the expression of aminoglycoside resistance requires that >50% of the ribosomal population be of the resistant phenotype (63). On the other hand, tetracycline or macrolide resistance occurs when at least 50% of the ribosomal population is mutated (4, 14, 22, 32, 69). Interestingly, these differences reflect the respective growth inhibitory activities of these different families of antibiotics, as aminoglycosides are generally bactericidal, whereas macrolides and tetracyclines are mostly bacteriostatic (74). In clinical strains, however, rRNA genes are generally homozygous, likely following gene conversion, a form of recombination resulting in the conversion of one allele to another (30). The homogenization of the genotype seems to be linked to more stability or homogeneity of the resistance phenotype. For example, the heterogeneous expression of erythromycin resistance in clinical isolates of Bordetella pertussis, of which both sensitive and resistant organisms were cultured in vitro, results from heterogeneity in the number of mutated 23S rRNA gene copies relative to the number of wild-type copies present in the organisms (4). Consequently, the “heterotypic” phenotypes described for C. trachomatis clinical isolates that are resistant to tetracycline (35, 44, 71) or azithromycin (49) could also result from a heterozygous genotype. Interestingly, Misyurina et al. detected both wild-type and mutated copies of 23S rRNA in azithromycin-resistant clinical isolates of C. trachomatis, although it was not clear what percentage of the population was heterozygous or homozygous (49). Additional passages in the presence of azithromycin allowed homogenization of the genotype but resulted in a loss of bacterial viability, suggesting that these resistant clinical isolates would not survive in nature. This apparent decrease in C. trachomatis fitness associated with the 23S rRNA macrolide resistance mutation could explain why, although treatment failures have also been reported for the use of macrolides for C. pneumoniae (26, 29, 65, 66) and C. felis, which are closely related to C. psittaci (54), no genetic evidence of macrolide resistance was detected in the few isolates retrieved (64). In addition, attempts to isolate macrolide-resistant variants of C. pneumoniae in vitro by repeated passaging in the presence of clarithromycin or azithromycin have failed (64, 68), even though a C. pneumoniae quinolone-resistant variant resulting from a point mutation in the gyrase gene was isolated recently in vitro by the same procedure (68).
In an era in which antibiotic resistance is a growing public health concern, knowledge regarding the frequency as well as the biological consequences of resistance may be our best strategy to counter it. We showed here that spontaneous mutations arise in vitro in C. trachomatis L2 and C. psittaci 6BC at frequencies similar to those for other eubacteria. In particular, the frequencies of spectinomycin resistance in C. psittaci 6BC and C. trachomatis L2 were comparable to those established for mycobacteria with regard to the number of rRNA copies present in the bacterial strains. In addition, because resistance to macrolides or tetracyclines is dominant in a merodiploid strain, resistance to the drugs currently used to treat chlamydial infections could emerge from single mutations whether the strain harbors one rRNA copy, such as C. psittaci and C. pneumoniae strains, or two rRNA copies, such as C. trachomatis strains, provided that the mutation does not confer a physiological burden. Indeed, whether drug-resistant organisms persist in nature depends on their likely occurrence as well as their fitness relative to their drug-sensitive counterparts (1). We are currently investigating the fitness costs due to mutations in the 16S rRNA associated with spectinomycin resistance in C. psittaci 6BC. This will provide additional information on the use of the plaque assay as an effective method to predict, monitor, and perhaps prevent the emergence of antibiotic resistance in chlamydiae.
Acknowledgments
This work was supported by grant AI44033 from the National Institute of Allergy and Infectious Diseases.
We thank H. Caldwell for the gift of C. trachomatis serovar L2, T. Hatch for the gift of C. psittaci serovar 6BC, and M. N. Flora and the USUHS Biomedical Instrumentation Center for DNA sequencing and oligonucleotide synthesis services. R.B. also gratefully acknowledges S. Létoffé and A. J. McCoy for their stimulating comments.
The opinions or assertions contained herein are those of the authors and are not to be construed as official or reflecting the views of the Department of Defense or the Uniformed Services University of the Health Sciences.
REFERENCES
- 1.Andersson, D. I., and B. R. Levin. 1999. The biological cost of antibiotic resistance. Curr. Opin. Microbiol. 2:489-493. [DOI] [PubMed] [Google Scholar]
- 2.Andrews, J. M. 2001. Determination of minimum inhibitory concentrations. J. Antimicrob. Chemother. 48(Suppl. 1):5-16. [DOI] [PubMed] [Google Scholar]
- 3.Banks, J., B. Eddie, J. Schachter, and K. F. Meyer. 1970. Plaque formation by Chlamydia in L cells. Infect. Immun. 1:259-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartkus, J. M., B. A. Juni, K. Ehresmann, C. A. Miller, G. N. Sanden, P. K. Cassiday, M. Saubolle, B. Lee, J. Long, A. R. Harrison, Jr., and J. M. Besser. 2003. Identification of a mutation associated with erythromycin resistance in Bordetella pertussis: implications for surveillance of antimicrobial resistance. J. Clin. Microbiol. 41:1167-1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beatty, W. L., G. I. Byrne, and R. P. Morrison. 1993. Morphologic and antigenic characterization of interferon γ-mediated persistent Chlamydia trachomatis infection in vitro. Proc. Natl. Acad. Sci. USA 90:3998-4002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blythe, M. J., B. P. Katz, B. E. Batteiger, J. A. Ganser, and R. B. Jones. 1992. Recurrent genitourinary chlamydial infections in sexually active female adolescents. J. Pediatr. 121:487-493. [DOI] [PubMed] [Google Scholar]
- 7.Bragina, E. Y., M. A. Gomberg, and G. A. Dmitriev. 2001. Electron microscopic evidence of persistent chlamydial infection following treatment. J. Eur. Acad. Dermatol. Venereol. 15:405-409. [DOI] [PubMed] [Google Scholar]
- 8.Brink, M. F., G. Brink, M. P. Verbeet, and H. A. de Boer. 1994. Spectinomycin interacts specifically with the residues G1064 and C1192 in 16S rRNA, thereby potentially freezing this molecule into an inactive conformation. Nucleic Acids Res. 22:325-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brinkman, F. S., J. L. Blanchard, A. Cherkasov, Y. Av-Gay, R. C. Brunham, R. C. Fernandez, B. B. Finlay, S. P. Otto, B. F. Ouellette, P. J. Keeling, A. M. Rose, R. E. Hancock, S. J. Jones, and H. Greberg. 2002. Evidence that plant-like genes in Chlamydia species reflect an ancestral relationship between Chlamydiaceae, cyanobacteria, and the chloroplast. Genome Res. 12:1159-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bush, R. M., and K. D. Everett. 2001. Molecular evolution of the Chlamydiaceae. Int. J. Syst. Evol. Microbiol. 51:203-220. [DOI] [PubMed] [Google Scholar]
- 11.Carter, A. P., W. M. Clemons, D. E. Brodersen, R. J. Morgan-Warren, B. T. Wimberly, and V. Ramakrishnan. 2000. Functional insights from the structure of the 30S ribosomal subunit and its interactions with antibiotics. Nature 407:340-348. [DOI] [PubMed] [Google Scholar]
- 12.Coles, A. M., D. J. Reynolds, A. Harper, A. Devitt, and J. H. Pearce. 1993. Low-nutrient induction of abnormal chlamydial development: a novel component of chlamydial pathogenesis? FEMS Microbiol. Lett. 106:193-200. [DOI] [PubMed] [Google Scholar]
- 13.Corsaro, D., and D. Venditti. 2004. Emerging chlamydial infections. Crit. Rev. Microbiol. 30:75-106. [DOI] [PubMed] [Google Scholar]
- 14.Dailidiene, D., M. T. Bertoli, J. Miciuleviciene, A. K. Mukhopadhyay, G. Dailide, M. A. Pascasio, L. Kupcinskas, and D. E. Berg. 2002. Emergence of tetracycline resistance in Helicobacter pylori: multiple mutational changes in 16S ribosomal DNA and other genetic loci. Antimicrob. Agents Chemother. 46:3940-3946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dessus-Babus, S., C. M. Bebear, A. Charron, C. Bebear, and B. de Barbeyrac. 1998. Sequencing of gyrase and topoisomerase IV quinolone-resistance-determining regions of Chlamydia trachomatis and characterization of quinolone-resistant mutants obtained in vitro. Antimicrob. Agents Chemother. 42:2474-2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dreses-Werringloer, U., I. Padubrin, B. Jürgens-Saathoff, A. P. Hudon, H. Zeidler, and L. Köhler. 2000. Persistence of Chlamydia trachomatis is induced by ciprofloxacin and ofloxacin in vitro. Antimicrob. Agents Chemother. 44:3288-3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dreses-Werringloer, U., I. Padubrin, L. Kohler, and A. P. Hudson. 2003. Detection of nucleotide variability in rpoB in both rifampin-sensitive and rifampin-resistant strains of Chlamydia trachomatis. Antimicrob. Agents Chemother. 47:2316-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dreses-Werringloer, U., I. Padubrin, H. Zeidler, and L. Kohler. 2001. Effects of azithromycin and rifampin on Chlamydia trachomatis infection in vitro. Antimicrob. Agents Chemother. 45:3001-3008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drysdale, M. J., G. Lentzen, N. Matassova, A. I. H. Murchie, F. Aboul-Ela, and M. Afshar. 2002. RNA as a drug target. Prog. Med. Chem. 39:73-119. [DOI] [PubMed] [Google Scholar]
- 20.Dugan, J., D. D. Rockey, L. Jones, and A. A. Andersen. 2004. Tetracycline resistance in Chlamydia suis mediated by genomic islands inserted into the chlamydial inv-like gene. Antimicrob. Agents Chemother. 48:3989-3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galimand, M., G. Gerbaud, and P. Courvalin. 2000. Spectinomycin resistance in Neisseria spp. due to mutations in 16S rRNA. Antimicrob. Agents Chemother. 44:1365-1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerrits, M. M., M. Berning, A. H. van Vliet, E. J. Kuipers, and J. G. Kusters. 2003. Effects of 16S rRNA gene mutations on tetracycline resistance in Helicobacter pylori. Antimicrob. Agents Chemother. 47:2984-2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gieffers, J., R. J. Belland, W. Whitmire, S. Ouellette, D. Crane, M. Maass, G. I. Byrne, and H. D. Caldwell. 2002. Isolation of Chlamydia pneumoniae clonal variants by a focus-forming assay. Infect. Immun. 70:5827-5834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gieffers, J., J. Rupp, A. Gebert, W. Solbach, and M. Klinger. 2004. First-choice antibiotics at subinhibitory concentrations induce persistence of Chlamydia pneumoniae. Antimicrob. Agents Chemother. 48:1402-1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hammerschlag, M. R. 1994. Antimicrobial susceptibility and therapy of infections caused by Chlamydia pneumoniae. Antimicrob. Agents Chemother. 38:1873-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hammerschlag, M. R., K. Chirgwin, P. M. Roblin, M. Gelling, W. Dumornay, L. Mandel, P. Smith, and J. Schachter. 1992. Persistent infection with Chlamydia pneumoniae following acute respiratory illness. Clin. Infect. Dis. 14:178-182. [DOI] [PubMed] [Google Scholar]
- 27.Hammerschlag, M. R., and J. C. Vuletin. 1985. Ultrastructural analysis of the effect of trimethoprim and sulphamethoxazole on the development of Chlamydia trachomatis in cell culture. J. Antimicrob. Chemother. 15:209-217. [DOI] [PubMed] [Google Scholar]
- 28.Hanahan, D. 1983. Studies on transformation of Escherichia coli with plasmids. J. Mol. Biol. 166:557-580. [DOI] [PubMed] [Google Scholar]
- 29.Harris, J. A., A. Kolokathis, M. Campbell, G. H. Cassell, and M. R. Hammerschlag. 1998. Safety and efficacy of azithromycin in the treatment of community acquired pneumonia in children. Pediatr. Infect. Dis. J. 17:865-871. [DOI] [PubMed] [Google Scholar]
- 30.Hashimoto, J. G., B. S. Stevenson, and T. M. Schmidt. 2003. Rates and consequences of recombination between rRNA operons. J. Bacteriol. 185:966-972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hogan, R. J., S. A. Mathews, S. Mukhopadhyay, J. T. Summersgill, and P. Timms. 2004. Chlamydial persistence: beyond the biphasic paradigm. Infect. Immun. 72:1843-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hulten, K., A. Gibreel, O. Skold, and L. Engstrand. 1997. Macrolide resistance in Helicobacter pylori: mechanism and stability in strains from clarithromycin-treated patients. Antimicrob. Agents Chemother. 41:2550-2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jin, D. J., and C. A. Gross. 1988. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that leads to rifampicin resistance. J. Mol. Biol. 202:45-58. [DOI] [PubMed] [Google Scholar]
- 34.Johnson, F. W., M. J. Clarkson, and W. N. Spencer. 1983. Susceptibility of Chlamydia psittaci (ovis) to antimicrobial agents. J. Antimicrob. Chemother. 11:413-418. [DOI] [PubMed] [Google Scholar]
- 35.Jones, R. B., B. Van der Pol, D. H. Martin, and M. K. Shepard. 1990. Partial characterization of Chlamydia trachomatis isolates resistant to multiple antibiotics. J. Infect. Dis. 162:1309-1315. [DOI] [PubMed] [Google Scholar]
- 36.Kalman, S., W. Mitchell, R. Marathe, C. Lammel, J. Fan, R. W. Hyman, L. Olinger, J. Grimwood, R. W. Davis, and R. S. Stephens. 1999. Comparative genomes of Chlamydia pneumoniae and C. trachomatis. Nat. Genet. 21:385-389. [DOI] [PubMed] [Google Scholar]
- 37.Karunakaran, P., and J. Davies. 2000. Genetic antagonism and hypermutability in Mycobacterium smegmatis. J. Bacteriol. 182:3331-3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Katz, B. P., D. Fortenberry, and D. Orr. 1998. Factors affecting chlamydial persistence or recurrence one and three months after treatment, p. 35-38. In R. S. Stephens, G. I. Byrne, G. Christiansen, I. N. Clark, J. T. Grayson, R. G. Rank, G. L. Ridgeway, P. Saikku, J. Schachter, and W. E. Stamm (ed.), Chlamydial infections. Proceedings of the Ninth International Symposium on Human Chlamydial Infection. UCSF, San Francisco, Calif.
- 39.Keshishyan, H., L. Hanna, and E. Jawetz. 1973. Emergence of rifampin-resistance in Chlamydia trachomatis. Nature 244:173-174. [DOI] [PubMed] [Google Scholar]
- 40.Kramer, M. J., and F. B. Gordon. 1971. Ultrastructural analysis of the effects of penicillin and chlortetracycline on the development of a genital tract Chlamydia. Infect. Immun. 3:333-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kutlin, A., P. M. Roblin, and M. R. Hammerschlag. 1999. In vitro activities of azithromycin and ofloxacin against Chlamydia pneumoniae in a continuous-infection model. Antimicrob. Agents Chemother. 43:2268-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kutlin, A., P. M. Roblin, and M. R. Hammerschlag. 2002. Effect of prolonged treatment with azithromycin, clarithromycin, or levofloxacin on Chlamydia pneumoniae in a continuous-infection model. Antimicrob. Agents Chemother. 46:409-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee, C. K., W. R. Bowie, and E. R. Alexander. 1978. In vitro assays of the efficacy of antimicrobial agents in controlling Chlamydia trachomatis propagation. Antimicrob. Agents Chemother. 13:441-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lefevre, J. C., J. P. Lepargneur, D. Guion, and S. Bei. 1997. Tetracycline-resistant Chlamydia trachomatis in Toulouse, France. Pathol. Biol. (Paris) 45:376-378. [PubMed] [Google Scholar]
- 45.Mariam, D. H., Y. Mengistu, S. E. Hoffner, and D. I. Andersson. 2004. Effect of rpoB mutations conferring rifampin resistance on fitness of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 48:1289-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martinez, J. L., and F. Baquero. 2000. Mutation frequencies and antibiotic resistance. Antimicrob. Agents Chemother. 44:1771-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Matsumoto, A., H. Izutsu, N. Miyashita, and M. Ohuchi. 1998. Plaque formation by and plaque cloning of Chlamydia trachomatis biovar trachoma. J. Clin. Microbiol. 36:3013-3019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCoy, A. J., R. C. Sandlin, and A. T. Maurelli. 2003. In vitro and in vivo functional activity of Chlamydia MurA, a UDP-N-acetylglucosamine enolpyruvyl transferase involved in peptidoglycan synthesis and fosfomycin resistance. J. Bacteriol. 185:1218-1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Misyurina, O. Y., E. V. Chipitsyna, Y. P. Finashutina, V. N. Lazarev, T. A. Akopian, A. M. Savicheva, and V. M. Govorun. 2004. Mutations in a 23S rRNA gene of Chlamydia trachomatis associated with resistance to macrolides. Antimicrob. Agents Chemother. 48:1347-1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morse, R., K. O'Hanlon, M. Virji, and M. D. Collins. 1999. Isolation of rifampin-resistant mutants of Listeria monocytogenes and their characterization by rpoB gene sequencing, temperature sensitivity for growth, and interaction with an epithelial cell line. J. Clin. Microbiol. 37:2913-2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moulder, J. W., D. L. Novosel, and J. E. Officier. 1963. Inhibition of the growth of agents of the psittacosis group by d-cycloserine and its specific reversal by d-alanine. J. Bacteriol. 85:707-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Musser, J. M. 1995. Antimicrobial agent resistance in mycobacteria: molecular genetic insights. Clin. Microbiol. Rev. 8:496-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nanagara, T., F. Li, A. Beutler, A. Hudson, and H. R. Schumacher. 1995. Alteration of Chlamydia trachomatis biologic behavior in synovial membranes: suppression of surface antigen production in reactive arthritis and Reiter's syndrome. Arthritis Rheum. 38:1410-1417. [DOI] [PubMed] [Google Scholar]
- 54.Owen, W. M., C. P. Sturgess, D. A. Harbour, K. Egan, and T. J. Gruffydd-Jones. 2003. Efficacy of azithromycin for the treatment of feline chlamydophilosis. J. Feline Med. Surg. 5:305-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Owens, J. T., R. Miyake, K. Murakami, A. J. Chmura, N. Fujita, A. Ishihama, and C. F. Meares. 1998. Mapping the sigma70 subunit contact sites on Escherichia coli RNA polymerase with a sigma70-conjugated chemical protease. Proc. Natl. Acad. Sci. USA 95:6021-6026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Panaud, O., G. Magpantay, and S. McCouch. 1993. A protocol for non-radioactive DNA labelling and detection in the RFLP analysis of rice and tomato using single-copy probes. Plant Mol. Biol. Rep. 11:54-59. [Google Scholar]
- 57.Pantoja, L. G., R. D. Miller, J. A. Ramirez, R. E. Molestina, and J. T. Summersgill. 2000. Characterization of Chlamydia pneumoniae persistence in HEp-2 cells treated with gamma interferon. Infect. Immun. 69:7927-7932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pfister, P., M. Risch, D. E. Brodersen, and E. C. Bottger. 2003. Role of 16S rRNA helix 44 in ribosomal resistance to hygromycin B. Antimicrob. Agents Chemother. 47:1496-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prammananan, T., P. Sander, B. A. Brown, K. Frischkorn, G. O. Onyi, Y. Zhang, E. C. Bottger, and R. J. Wallace, Jr. 1998. A single 16S ribosomal RNA substitution is responsible for resistance to amikacin and other 2-deoxystreptamine aminoglycosides in Mycobacterium abscessus and Mycobacterium chelonae. J. Infect. Dis. 177:1573-1581. [DOI] [PubMed] [Google Scholar]
- 60.Raulston, J. E. 1997. Response of Chlamydia trachomatis serovar E to iron restriction in vitro and evidence for iron-regulated chlamydial proteins. Infect. Immun. 65:4539-4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Read, T. D., R. C. Brunham, C. Shen, S. R. Gill, J. F. Heidelberg, O. White, E. K. Hickey, J. Peterson, T. Utterback, K. Berry, S. Bass, K. Linher, J. Weidman, H. Khouri, B. Craven, C. Bowman, R. Dodson, M. Gwinn, W. Nelson, R. DeBoy, J. Kolonay, G. McClarty, S. L. Salzberg, J. Eisen, and C. M. Fraser. 2000. Genome sequences of Chlamydia trachomatis MoPn and Chlamydia pneumoniae AR39. Nucleic Acids Res. 28:1397-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Read, T. D., G. S. Myers, R. C. Brunham, W. C. Nelson, I. T. Paulsen, J. Heidelberg, E. Holtzapple, H. Khouri, N. B. Federova, H. A. Carty, L. A. Umayam, D. H. Haft, J. Peterson, M. J. Beanan, O. White, S. L. Salzberg, R. C. Hsia, G. McClarty, R. G. Rank, P. M. Bavoil, and C. M. Fraser. 2003. Genome sequence of Chlamydophila caviae (Chlamydia psittaci GPIC): examining the role of niche-specific genes in the evolution of the Chlamydiaceae. Nucleic Acids Res. 31:2134-2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Recht, M. I., and J. D. Puglisi. 2001. Aminoglycoside resistance with homogeneous and heterogeneous populations of antibiotic-resistant ribosomes. Antimicrob. Agents Chemother. 45:2414-2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Riska, P. F., A. Kutlin, P. Ajiboye, A. Cua, P. M. Roblin, and M. R. Hammerschlag. 2004. Genetic and culture-based approaches for detecting macrolide resistance in Chlamydia pneumoniae. Antimicrob. Agents Chemother. 48:3586-3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Roblin, P. M., and M. R. Hammerschlag. 1998. Microbiologic efficacy of azithromycin and susceptibilities to azithromycin of isolates of Chlamydia pneumoniae from adults and children with community-acquired pneumonia. Antimicrob. Agents Chemother. 42:194-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roblin, P. M., G. Montalban, and M. R. Hammerschlag. 1994. Susceptibilities to clarithromycin and erythromycin of isolates of Chlamydia pneumoniae from children with pneumonia. Antimicrob. Agents Chemother. 38:1588-1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roshick, C., E. R. Iliffe-Lee, and G. McClarty. 2000. Cloning and characterization of ribonucleotide reductase from Chlamydia trachomatis. J. Biol. Chem. 275:38111-38119. [DOI] [PubMed] [Google Scholar]
- 68.Rupp, J., A. Gebert, W. Solbach, and M. Maass. 2005. Serine-to-asparagine substitution in the GyrA gene leads to quinolone resistance in moxifloxacin-exposed Chlamydia pneumoniae. Antimicrob. Agents Chemother. 49:406-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sander, P., T. Prammananan, A. Meier, K. Frischkorn, and E. C. Bottger. 1997. The role of ribosomal RNAs in macrolide resistance. Mol. Microbiol. 26:469-480. [DOI] [PubMed] [Google Scholar]
- 70.Skowasch, D., K. Yeghiazaryan, O. Schrempf, U. Golubnitschaja, C. Welsch, C. J. Preusse, J. A. Likungu, A. Welz, B. Lüderitz, and G. Bauriedel. 2003. Persistence of Chlamydia pneumoniae in degenerative aortic valve stenosis indicated by heat shock protein 60 homologues. J. Heart Valve Dis. 12:68-75. [PubMed] [Google Scholar]
- 71.Somani, J., V. B. Bhullar, K. A. Workowski, C. E. Farshy, and C. M. Black. 2000. Multiple drug-resistant Chlamydia trachomatis associated with clinical treatment failure. J. Infect. Dis. 181:1421-1427. [DOI] [PubMed] [Google Scholar]
- 72.Stamm, W. E. 2000. Potential for antimicrobial resistance in Chlamydia pneumoniae. J. Infect. Dis. 181(Suppl. 3):S456-S459. [DOI] [PubMed] [Google Scholar]
- 73.Stephens, R. S., S. Kalman, C. Lammel, J. Fan, R. Marathe, L. Aravind, W. Mitchell, L. Olinger, R. L. Tatusov, Q. Zhao, E. V. Koonin, and R. W. Davis. 1998. Genome sequence of an obligate intracellular pathogen of humans: Chlamydia trachomatis. Science 282:754-759. [DOI] [PubMed] [Google Scholar]
- 74.Stratton, C. W. 2003. Dead bugs don't mutate: susceptibility issues in the emergence of bacterial resistance. Emerg. Infect. Dis. 9:10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Suchland, R. J., W. M. Geisler, and W. E. Stamm. 2003. Methodologies and cell lines used for antimicrobial susceptibility testing of Chlamydia spp. Antimicrob. Agents Chemother. 47:636-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang, G., T. J. Wilson, Q. Jiang, and D. E. Taylor. 2001. Spontaneous mutations that confer antibiotic resistance in Helicobacter pylori. Antimicrob. Agents Chemother. 45:727-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wehrli, W. 1983. Rifampin: mechanisms of action and resistance. Rev. Infect. Dis. 5:S407-S450. [DOI] [PubMed] [Google Scholar]
- 78.Whittington, W. L., C. Kent, P. Kissinger, M. K. Oh, J. D. Fortenberry, S. E. Hillis, B. Litchfield, G. A. Bolan, M. E. St. Louis, T. A. Farley, and H. H. Handsfield. 2001. Determinants of persistent and recurrent Chlamydia trachomatis infection in young women: results of a multicenter cohort study. Sex. Transm. Dis. 28:117-123. [DOI] [PubMed] [Google Scholar]
- 79.Wolf, K., E. Fischer, and T. Hackstadt. 2000. Ultrastructural analysis of developmental events in Chlamydia pneumoniae-infected cells. Infect. Immun. 68:2379-2385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wylie, J. L., L. L. Wang, G. Tipples, and G. McClarty. 1996. A single point mutation in CTP synthetase of Chlamydia trachomatis confers resistance to cyclopentenyl cytosine. J. Biol. Chem. 271:15393-15400. [DOI] [PubMed] [Google Scholar]
- 81.Wyrick, P. B. 2000. Intracellular survival by Chlamydia. Cell Microbiol. 2:275-282. [DOI] [PubMed] [Google Scholar]