Abstract
Objective
This study aims to clarify angiogenesis mechanisms in ulcerative colitis and identify potential therapeutic targets.
Methods
The Gene Expression Omnibus (GEO) database was used to obtain expression profiles and clinical data for UC and healthy colon tissues. Angiogenesis-related gene sets were acquired from GeneCards. Differential expression analysis and weighted gene co-expression network analysis (WGCNA) identified UC-associated hub genes. The CIBERSORT algorithm assessed immune cell infiltration. Analyses of Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) were performed to determine biological mechanisms. External datasets were utilized to validate and characterize the angiogenesis-related genes in relation to biological agents. Additionally, an ulcerative colitis mouse model was constructed to verify the key genes’ expression using real-time quantitative PCR. To predict potential therapeutic agents, we used the DGIdb database. Molecular docking modeled small molecule binding conformations to key gene targets.
Results
This study identified 1,247 DEGs enriched in inflammatory/immune pathways from UC and healthy colon samples. WGCNA indicated the black and light cyan modules were most relevant. Intersecting these with 89 angiogenesis genes revealed 5 UC-associated hub genes (pdgfrb, vegfc, angpt2, tnc, hgf). Validation via ROC analysis, differential expression, and a mouse model confirmed upregulation, supporting their potential as UC diagnostic biomarkers. Bioinformatics approaches like protein–protein interaction, enrichment analysis, and GSEA revealed involvement in PDGFR and PI3K-Akt signaling pathways. CIBERSORT analysis of immune cell infiltration showed positive correlations between the key genes and various immune cells, especially neutrophils, highlighting angiogenesis-inflammation interplay in UC. A ceRNA network was constructed. Drug prediction and molecular docking revealed potential UC therapies like sunitinib and imatinib targeting angiogenesis.
Conclusion
This study identified and validated five angiogenesis-related genes (pdgfrb, vegfc, angpt2, tnc, hgf) that may serve as diagnostic biomarkers and drug targets for UC.
Keywords: ulcerative colitis, bioinformatics analysis, WGCNA, GSEA, molecular docking
Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease with a rising global incidence. Recent epidemiological studies report incidence rates ranging from 0.6 to 23.1 per 100,000 person-years, with higher rates observed in industrialized countries.1,2 The disease severity in UC is typically classified as mild, moderate, or severe based on clinical symptoms, endoscopic findings, and biomarkers.3 The Mayo Score and the Ulcerative Colitis Disease Activity Index (UCDAI) are commonly used tools for assessing disease severity.4 Approximately 30% of patients experience severe disease at some point, which is associated with increased hospitalization rates, higher risk of colectomy, and reduced quality of life.5 Understanding disease severity is crucial for tailoring treatment strategies and predicting long-term outcomes in UC patients.3 The pathological features of UC include mucosal inflammation, ulceration, and tissue remodeling, with angiogenesis playing a crucial role in disease development and progression.6 Angiogenesis, the formation of new blood vessels from pre-existing ones, is abnormally active in UC, leading to reconstruction and expansion of the intestinal microvascular network.7
The vascular endothelial growth factor (VEGF) family, especially VEGF-A, plays a central role in UC-associated angiogenesis by promoting endothelial cell proliferation, migration, and tubule formation.8–11 Other pro-angiogenic factors are also crucial. The angiopoietin (Ang) family, particularly Ang-1 and Ang-2, regulates vascular stability and remodeling.12–14 Fibroblast growth factors (FGFs), notably FGF-2, promote endothelial cell proliferation and act synergistically with VEGF.15–17 Inflammatory mediators significantly contribute to UC-associated angiogenesis. TNF-α stimulates VEGF production and directly activates endothelial cells.18,19 IL-1β upregulates VEGF expression and promotes endothelial cell proliferation.20,21 Hypoxia in the inflammatory microenvironment triggers HIF-1α activation, orchestrating the cellular response to low oxygen conditions.22–24 Various cell types contribute to UC-associated angiogenesis. Macrophages serve as major sources of pro-angiogenic factors.25,26 Neutrophils release pro-angiogenic factors and matrix-degrading enzymes.27,28 Fibroblasts, particularly activated myofibroblasts, produce growth factors stimulating endothelial cell proliferation.29 The melanocortin system has also emerged as a significant modulator of inflammation in IBD, with potential therapeutic implications.30 Lifestyle factors, such as physical activity, can influence disease course in UC patients, with studies showing low activity levels among many IBD patients.31
Recognizing angiogenesis’s crucial role in UC pathogenesis, several therapeutic approaches targeting this process have been explored. Anti-VEGF antibodies have shown promise in preclinical studies but yielded mixed results in clinical trials.32 Other anti-angiogenic strategies, including small molecule inhibitors of VEGF receptors and agents targeting multiple angiogenic pathways, are under investigation.33 Despite these advances, current anti-angiogenic approaches in UC face several limitations. The multifaceted nature of angiogenesis in UC, involving numerous growth factors and signaling pathways, makes it challenging to achieve effective inhibition with single-target therapies.14 Moreover, the timing of anti-angiogenic intervention is critical, as VEGF and other angiogenic factors also play important roles in tissue repair and mucosal healing.34 There is also a need for better biomarkers to identify patients who are most likely to benefit from anti-angiogenic therapies and to monitor treatment response.35 Furthermore, our understanding of the complex interplay between angiogenesis, inflammation, and tissue remodeling in UC remains incomplete. The roles of newly identified angiogenic mediators, the contribution of different cell types to pathological angiogenesis, and the impact of the gut microbiome on vascular remodeling are areas that require further investigation.36
This study aims to elucidate the mechanisms of pathological angiogenesis in UC, potentially facilitating the development of more effective, personalized anti-angiogenic therapies.
Methods
Data Sources and Preprocessing
This study primarily utilized publicly available gene expression datasets from the GEO database (https://www.ncbi.nlm.nih.gov/geo/) for the identification of angiogenesis-related gene signatures in UC. The dataset selection process involved an initial search using keywords “ulcerative colitis” and “gene expression”, followed by application of inclusion criteria: confirmed UC diagnosis, matched healthy colon tissue controls from the same GEO platform, minimum of 20 samples, and GEO platforms with >10,000 probes. After quality control assessing data completeness and consistency, nine datasets (GSE87466, GSE92415, GSE65114, GSE107499, GSE53306, GSE36807, GSE37283, GSE73661 and GSE75214) were included for independent downstream analysis (Table 1). To remove potential batch effects, we applied the ComBat algorithm from the sva R package (version 3.42.0) to each dataset.37 Differential expression analysis between UC and control samples was conducted using the limma R package (version 3.50.3), with DEGs defined by adjusted p < 0.05 and |log2FC|>1. Visualization of DEG results was performed using ggplot2 (version 3.3.6) and pheatmap (version 1.0.12) R packages. Additionally, angiogenesis-related genes were retrieved from GeneCards (https://www.genecards.org).38 The rentrez R package (version 1.2.3) was used to facilitate the retrieval of gene information from NCBI databases.
Table 1.
A Summary of Microarray Information
Biological Function and Pathway Enrichment Analysis
Genes differentially expressed in UC were analyzed using GO and KEGG enrichment analyses in order to elaborate on the underlying pathological mechanisms.39 GO analysis categorizes genes into biological processes, cellular components, and molecular functions, enabling interpretation of overrepresented themes in the data. Analysis was conducted using the “clusterProfiler” R package by calculating enrichment p-values for each GO term. Significantly enriched terms were visualized using “ggplot2” R package. KEGG analysis identified enriched pathways among the differentially expressed genes, providing further biological context. The KEGG database contains information on molecular pathways and disease processes.40
Additional analysis explored the potential functions of the hub genes identified through enrichment approaches. Instead of comparing gene sets between experimental groups, these analyses used the expression signature of each individual hub gene to query associated pathways and processes from curated databases. This reveals which biological pathways and themes show significant enrichment connected to the validated gene. By relating individual hub genes to enriched gene sets, we can better determine the pathways and functional implications upregulated in connection with our UC biomarkers.41 The Molecular Signatures Database provided reference gene sets. For all enrichment analyses, a p-value threshold of 0.05 determined statistical significance. Together, the multi-level enrichment analyses provided a comprehensive overview of the biological themes, pathways, and gene sets perturbed in UC, enabling deeper interpretation compared to individual gene analysis alone.
Weighted Gene Co-Expression Network Analysis
The GSE65114 dataset was utilized in WGCNA to identify co-expression modules associated with UC. WGCNA was performed using the R package “WGCNA”. WGCNA computes gene co-expression networks based on transcriptomics data.42 Unlike traditional cluster analysis, WGCNA accounts for the inherent correlation patterns amongst genes to identify modules of highly synergistically expressed genes.
Briefly, a similarity matrix containing all pairwise gene correlations is generated based on expression profile similarity. This matrix is then transformed into an adjacency matrix by raising it to a power β, which amplifies strong correlations and penalizes weak correlations in an exponential manner. The adjacency matrix is further transformed into a topological overlap matrix (TOM), which measures gene interconnectedness. Hierarchical clustering based on TOM discerns discrete gene modules, characterized by high intra-modular connectivity and low inter-modular connectivity. By correlating module eigengenes with external sample traits, WGCNA identifies modules associated with disease phenotypes. This data-driven approach facilitates an unbiased analysis of gene correlations and module–trait relationships.
Identification of Key Differentially Expressed Angiogenesis-Related Genes (DE-AGGs)
To identify DE-AGGs implicated in UC, we intersected DEGs from two datasets with known angiogenesis genes using Venn diagrams. This highlighted reproducibly dysregulated angiogenesis genes in UC. WGCNA constructed modules of highly co-expressed genes.43 Based on gene significance and module membership thresholds, we identified a key module enriched for angiogenesis-related DEGs associated with UC. WGCNA enables unbiased, systems-level analysis of gene correlations.
Within this UC-associated module, we ranked genes by UC trait correlations to pinpoint hub genes with high connectivity and phenotypic correlations, indicating central roles.
Hub genes were evaluated using receiver operating characteristic (ROC) analysis of external datasets. DEGs with area under the curve (AUC) >0.9 were considered to have significant UC diagnostic power and were advanced for further validation.
By integrating differential expression, knowledge-based selection, co-expression mapping, and external testing, we identified key angiogenesis-related DEG hubs with putative UC diagnostic utility. We further validated these genes in additional datasets and models to assess their diagnostic and biological significance.
Immune Infiltration Analysis
To investigate immune infiltration in UC, we utilized CIBERSORT deconvolution analysis. CIBERSORT leverages gene expression data and immune cell signatures to quantify relative proportions of 22 leukocyte subsets from bulk tissue samples.44 Analysis was performed using the LM22 signature matrix containing cell-specific expression data for 500 genes that distinguish populations.45 Deconvolution with 100 permutations and quantile normalization was applied to UC and healthy colon samples to enable robust estimation of immune cell abundance. Student’s t-tests identified differences between UC and controls. Correlations between angiogenesis genes and immune cells were examined using corrplot. This analysis provided comprehensive immunoprofiling of the UC colon, identifying altered leukocyte subsets. Examining angiogenesis gene correlations with immune populations may elucidate immune–vascular interactions in UC. By integrating deconvolution, differential analysis, and correlation mapping, CIBERSORT enabled robust interrogation of the UC immune microenvironment and angiogenesis-immune associations from bulk gene expression.
Protein–Protein Interaction (PPI) Networks
String database (https://www.string-db.org/) and GeneMANIA software (https://genemania.org/) were used to construct PPI networks and pathway interaction networks. The GeneMANIA database is available for investigating functional gene networks, offering a range of bioinformatics research techniques. These include interactions with physical factors, gene enrichment, localization and coexpression analysis, as well as prediction of sites.46 The STRING database integrates multiple sources of information, including gene neighborhood, fusion, co-occurrence, co-expression, protein–protein interactions, and literature mining, to generate scores that capture functional relatedness between genes.47 Cytoscape (http://www.cytoscape.org/) was used for plotting the PPI network using the interaction score of 0.4.48 To investigate significant gene clusters and key genes, MCODE algorithm was used with these settings: K core = 2, degree cutoff = 2, maximum depth = 100, node score cutoff = 0.2. Additionally, we utilized the cytohubba-MCC plugin with default parameters.49
Construction of the Mouse Model
We induced acute colitis in male C57BL mice aged 6–8 weeks under pathogen-free conditions.50 A total of sixteen mice were randomly divided into control and dextran sulfate sodium (DSS) groups (n = 8 per group) after seven days of acclimatization with access to food and water ad libitum. The Animal Ethics Committee of Research and Selection Biotechnology (Hangzhou) Co., Ltd. approved all procedures (Ethics Approval No. YXSW2308141850). Colitis was induced by drinking water containing 3% DSS (Source Leaf Bio) for 7 days, while control subjects drank normal water. A daily assessment of body weight, fecal consistency, and rectal bleeding was conducted (Supplement Table 1). An RT-PCR test was performed on colon tissue on day 8 after the mice were euthanized.
Tissue RNA Extraction and RT-qPCR
The total RNA from colonic tissues was extracted and purified using Trizol reagent (Life Technologies, 15596018). Reverse transcription was performed using GeniuScriptTM RT SuperMix with gDNA Eraser 2.0 (Boyue, M5RT04) to produce cDNA. This study used primers obtained from PrimerBank (https://pga.mgh.harvard.edu/primerbank/). RT-qPCR was performed on a Bio-Rad T100 Thermal Cycler using β-actin as an internal reference (Supplement Table 2). GraphPad Prism was used for graphing.
Potential Therapeutic Drug Prediction and Molecular Docking
The Drug Signatures Database (DSigDB) was utilized to retrieve FDA-approved and experimental drug compounds, which currently contains 17,389 unique molecules targeting 19,531 genes (http://tanlab.ucdenver.edu/DSigDB).51 To analyze the binding interactions between drug candidates and target proteins, molecular docking was carried out using AutoDock Vina 1.2.2. A three-dimensional model of ENMD-2076 was obtained from PubChem Compounds (CID 74424439).52 Crystal structures of receptor proteins were retrieved from the RCSB Protein Data Bank (https://www.rcsb.org).53 Ligand and receptor files were formatted to PDBQT, with non-polar hydrogens merged and water molecules removed. A 30 x 30×30 Å grid box was centered on the active site to permit ligand flexibility. Molecular docking simulations were executed in AutoDock Vina 1.2.2 (http://autodock.scripps.edu/) using default parameters.
The ceRNA Network Construction
To identify putative miRNA regulators of the identified hub genes, we utilized three target prediction databases: miRDB (http://mirdb.org/), TargetScanHuman (http://www.targetscan.org), and miRWalk (http://mirwalk.umm.uni-heidelberg.de/). These resources apply complementary algorithms to predict miRNA binding sites based on seed match complementarity, thermodynamics, and conservation.54,55 For circRNA targeting, we used circAtlas, which contains over 800,000 sequenced-based predicted miRNA-circRNA interactions. The identified miRNAs and circRNAs were compiled and visualized as interaction networks using Cytoscape software.56 By overlaying multi-level miRNA-mRNA-circRNA relationships, this systems biology approach provided insight into the upstream and downstream regulation of key angiogenesis-associated genes in ulcerative colitis. Integrative in silico prediction from multiple databases enabled comprehensive identification of the hub genes’ putative miRNA and circRNA interaction partners within the regulatory network.
Statistical Analysis
Our statistical analyses were performed using the R software (version 4.2.2, https://www.r-project.org) and its associated packages. Differential gene expression between UC and control samples was assessed using bootstrap t-tests. Adjusted p-values were derived by applying the Benjamini–Hochberg false discovery rate (FDR) correction method at a significance threshold of 1% to correct for multiple hypothesis testing. An FDR threshold of 1% was chosen to align with more conservative recent recommendations for family-wise error control. T-tests were employed to compare normally distributed variables, with results expressed as mean ± standard error. Biomarkers for diagnostics were evaluated with ROC curve analysis. For downstream enrichment analyses involving multiple comparisons such as GO, KEGG, WGCNA, etc., the Benjamini–Hochberg method was again applied to control FDR at 1%. The relationship between infiltrating immune cells and genetic markers was evaluated with Spearman correlation analysis. Correlation analysis was performed using the R software packages “ggpubr” and “stats”. All statistical tests performed in this study used two-tailed p-values, with a significance threshold set at P < 0.05. This approach was consistently applied across all analyses, including differential expression analysis, enrichment analyses, and comparisons between groups.
Results
The Main Content and Framework of This Study
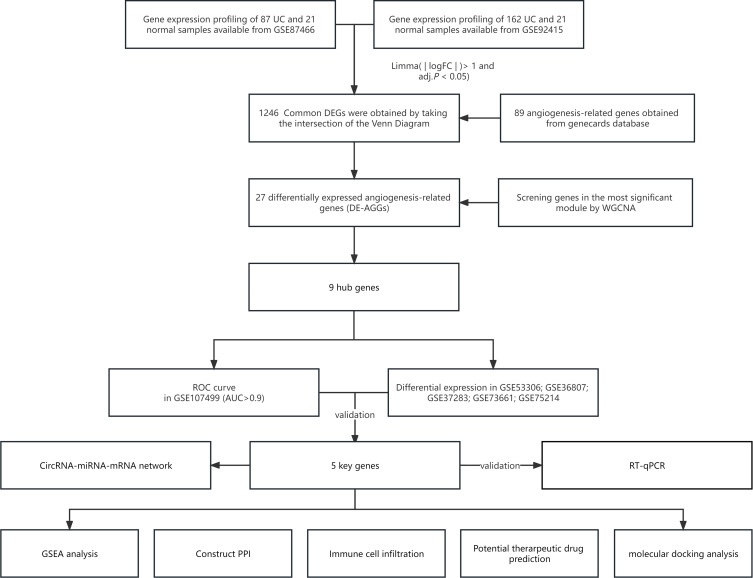
Figure 1 illustrated the flowchart and datasets used in this study. GSE87466 contained gene expression profiles from 87 UC samples and 21 healthy controls. Meanwhile, GSE92415 included profiles from 162 UC samples and 21 healthy samples. Differential gene analysis was performed on the UC samples and normal samples of these two datasets according to the criteria of |log2FC|>1 and adjusted p < 0.05. By taking the intersection, we obtained 1,246 common differentially expressed genes with concordant case–control differences across both datasets (Figure 2A–D). GO and KEGG were employed for further exploration of biological mechanisms of these DEGs. Angiogenesis-related hub genes were identified by intersecting DE-AGGs with genes identified by WGCNA. External datasets (GSE107499, GSE53306, GSE37283, GSE73661, and GSE75214) were used for the validation of ROC and differential expressions. GSEA analysis was performed and the DGIdb database was consulted to predict potential therapeutic agents, and molecular docking was performed to model small molecule compound binding to key targets. Detailed information about the datasets can be found in Table 1.
Figure 1.
The flowchart of the analysis process.
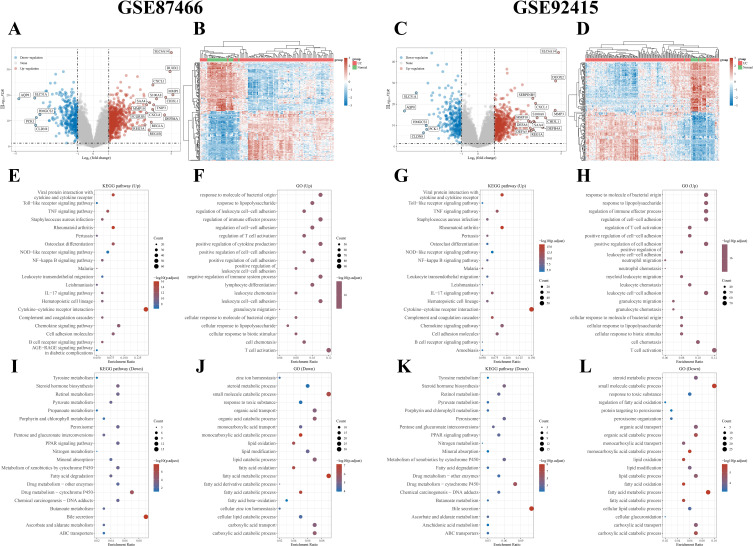
Figure 2.
Identification and functional annotation of DEGs. Volcano plots (A, GSE87466; C, GSE92415) and heatmaps (B, GSE87466; D, GSE92415) were used to display the DEGs between the ulcerative colitis (UC) and control groups. In the volcano plots, red points represent upregulated DEGs, gray points represent genes with no significant difference, and blue points represent downregulated DEGs. The heatmaps show each DEG as a row and each sample as a column, either UC or normal. KEGG enrichment analyses were conducted for the upregulated DEGs (E, GSE87466; G, GSE92415). GO enrichment analyses were also performed for the upregulated DEGs, including biological process (BP), cellular component (CC), and molecular function (MF) (F, GSE87466; H, GSE92415). Similarly, KEGG enrichment analyses were performed for the downregulated DEGs (I, GSE87466; K, GSE92415), along with GO enrichment analyses for biological process (BP), cellular component (CC), and molecular function (MF) (J, GSE87466; L, GSE92415).
DEG Pathway Enrichment Analysis
Pathway enrichment analysis was then conducted on the DEGs from GSE87466 and GSE92415 separately to elucidate the underlying mechanisms and functions associated with UC. The results of GO enrichment analysis indicate KEGG enrichment analysis indicated that up-regulated genes in UC patients were significantly enriched in inflammatory response-related pathways. In particular, the Cytokine–Cytokine Receptor interaction, the Chemokine signaling pathway, the Viral protein interaction with cytokines and cytokine receptors, and the Rheumatoid arthritis (Figure 2E and G). On the other hand, the down-regulated genes were significantly associated with signaling pathways related to small molecule catabolic processes and fatty acid metabolism (Figure 2J and L). The up-regulated genes were notably linked to immune-related processes and cell adhesion, while the down-regulated genes showed associations with small molecule catabolism and fatty acid metabolism. Additionally, GO enrichment analysis categorized genes into biological processes where the up-regulated genes were primarily related to signaling pathways related to immune effector process regulation, cytokine production stimulation, T cell activation, leukocyte cell–cell adhesion, and cell adhesion promotion (Figure 2F and H). Based on these findings, we speculate that these pathways may play a role in UC pathogenesis. In contrast, the down-regulated genes exhibited notable enrichment in signaling pathways associated with Bile secretion and Drug metabolism - cytochrome P450 (Figure 2I and K). This suggested the involvement of these pathways in altered bile metabolism and drug processing in UC patients.
Angiogenesis-Related Hub Genes Identified by WGCNA
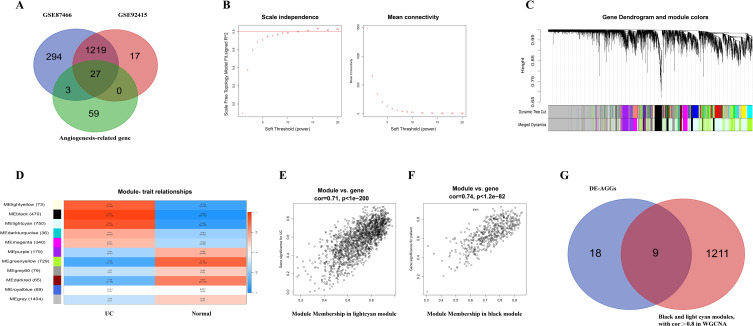
The Genecards database (https://www.genecards.org/) was used as our primary source for angiogenesis-related genes (AGGs). Within Genecards, we utilized the PathCards subcategory and searched for “angiogenesis”. The Cell Signaling Technology (CST) pathway emerged with the highest relevance score, providing a set of 89 angiogenesis-related genes. By employing Venn diagrams, we identified 27 differential genes that were both associated with angiogenesis and differentially expressed in datasets GSE87466 and GSE92415 (Figure 3A). To identify hub genes among DE-AGGs, we employed WGCNA analysis. WGCNA allowed us to identify modules of genes with similar co-expression patterns. We then focused on the intersections between the modules showing the highest relevance to UC and DE-AGGs, considering them as the hub genes of DE-AGGs. A soft threshold power of β = 16 (R2 = 0.85) was applied to capture informative connectivity patterns (Figure 3B). Utilizing hierarchical clustering, we identified 10 consensus co-expression modules by merging modules with minimal gaps (Figure 3C). The heatmap depicted the relationship between each module and UC, revealing that the black and light cyan modules exhibited a significant correlation with UC (Figure 3D). Correlation analysis showed a strong connection between the red MM and the selected module genes, as indicated by the gene significance (GS) with |cor|>0.8 (Figure 3E and F), indicating a high correlation between genes in the black and light cyan modules and active UC. By intersecting 1, 220 genes from these modules with DE-AGGs, we identified 9 hub genes (timp3, epha2, pdgfrb, vegfc, vwf, grem1, angpt2, tnc, hgf) for further study (Figure 3G).
Figure 3.
Identify hub genes of angiogenesis-related differentially expressed genes (DE-AGGs) by WGCNA. (A) Venn diagram shows the overlapping genes between differentially expressed genes and angiogenesis-related genes. (B) Soft threshold power screening and scale-free network construction. (C) Module clustering dendrogram based on a dissimilarity measure (1-TOM). (D) Module–trait relationships in UC. The relevant P value and correlation coefficient are listed in each cell. (E and F) A scatterplot of gene significance (GS) versus module membership (MM) in the light cyan and black module. (G) Venn diagram shows genes identified from the intersection of DE-AGGs and significant module genes in WGCNA.
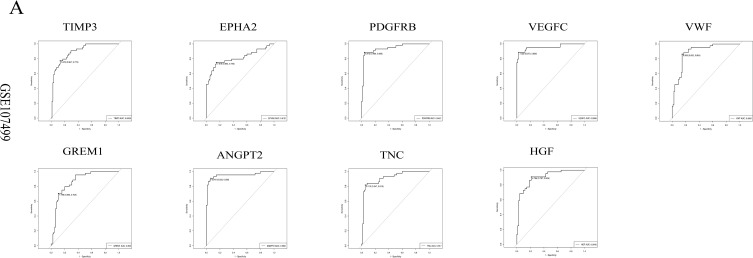
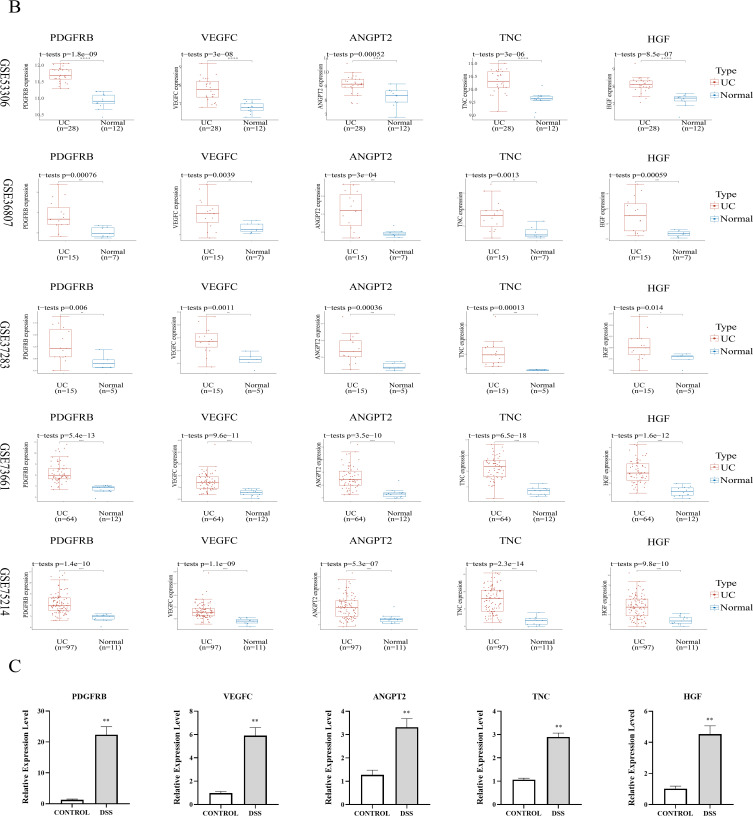
Validation of 9 Angiogenesis-Related Hub Genes
ROC analysis was conducted on the GSE107499 dataset to understand nine genes associated with angiogenesis. All 9 hub genes had AUC values greater than 0.8, indicating promising diagnostic potential (Figure 4A). Genes with AUC > 0.9 were considered key genes associated with angiogenesis, including pdgfrb, vegfc, angpt2, tnc, and hgf. The GSE53306, GSE36807, GSE37283, GSE73661 and GSE75214 were used to validate the differential expression (Figure 4B) and ROC (Supplementary Figure 1) for these 5 key genes. Statistically significant differences were observed in the 5 key genes between UC samples and control samples. To confirm the expression of these key genes, an animal model of DSS-induced colitis was used. In the DSS-exposed group, we observed increased gene expression in UC using reverse transcription-quantitative polymerase chain reaction (RT-qPCR) (Figure 4C).
Figure 4.
Continued.
Figure 4.
Identify key genes of angiogenesis-related differentially expressed genes (DE-AGGs). (A) The receiver operating characteristic curve analysis of hub genes in GSE107499, genes with AUC>0.9 were considered as key genes. (B) External validation of different expression levels of 5 key genes. (C) qRT-PCR validation of 5 key genes. ****P < 0.0001, ***P < 0.001, **P < 0.01, *P < 0.05.
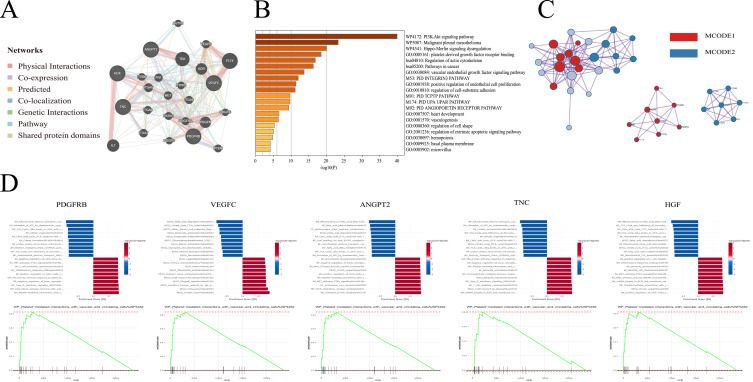
Protein–Protein Interaction Enrichment Analysis and GSEA
GeneMANIA was utilized to predict 20 potential transcription co-regulators recruited by transcription factors to the 5 key genes. Subsequently, PPI network was constructed using these 25 genes (Figure 5A). The STRING database was used for enrichment analysis of these key genes and potential co-regulators. Significant associations with GO enrichments associated with platelet-derived growth factor receptor binding, vascular endothelial growth factor response, and positive regulation of endothelial cell proliferation function were observed. Furthermore, KEGG enrichment analysis indicated the involvement of these genes in the PI3K-Akt signaling pathway (Figure 5B).
Figure 5.
Functional annotation and network of 5 key genes. (A) The protein–protein interaction network of 5 key genes. (B) Functional annotation and pathway enrichment of 5 key genes. (C) MCODE components identified in the Protein-protein interaction network. (D) Results of single gene enrichment analysis for each of the 5 key hub genes.
To explore the network components, we used the Molecular Complex Detection (MCODE) algorithm. Figure 5C shows the aggregated MCODE networks for the gene lists. MCODE 1 primarily encompassed GO terms such as platelet-derived growth factor receptor binding, Rap1 signaling pathway and transmembrane receptor protein tyrosine kinase signaling pathway. On the other hand, MCODE 2 mainly included biological processes such as ECM proteoglycans, ECM-receptor interaction and Integrin cell surface interactions.
Subsequently, single-gene gene set enrichment analysis (GSEA) of hub was performed using the “clusterProfiler” R package. We grouped the samples based on a single hub gene expression level in the datasets (Figure 5D). The analysis revealed enrichment of all five genes in the platelet-mediated interactions with vascular and circulating cells pathway (WP4462), which is associated with highly expressed genes in the genome signaling pathway. Furthermore, there were significant enrichments in other pathways such as PTK2 activates signaling (HSA-8874081), Inflammatory Response Pathway (WP453), and T cell-mediated cytotoxicity (BP:0001913). These foundings have shown that the identified gene clusters were associated with platelet-derived growth factor receptor binding, positive regulation of endothelial cell proliferation, vascular endothelial growth factor response, and the PI3K-Akt signaling pathway. The MCODE algorithm revealed interconnected network components related to platelet-related processes, extracellular matrix interactions, and other biological pathways such as Rap1 signaling pathway. Single GSEA analysis revealed significant enrichments in pathways related to platelet-mediated interactions with vascular and circulating cells, PTK2-activated signaling, inflammatory response, and T cell-mediated cytotoxicity. These pathways were highly connected with UC, indicating that angiogenesis may participate in UC development through a combination of immune, inflammatory, and cell adhesion mechanisms.
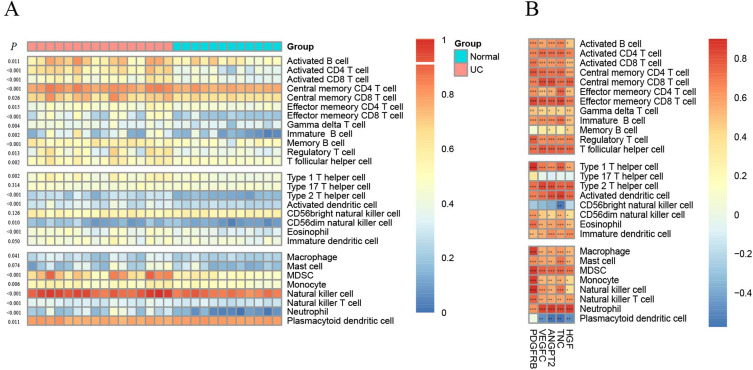
Infiltration of Immune Cells in UC
Figure 6A illustrates the immune cell infiltration patterns between two clusters using the CIBERSORT algorithm. There was a higher enrichment of genes associated with immunity in the UC group compared to the normal group. There were a variety of immune cells identified in the UC group, including activated CD4 T and CD8 cells, natural killer cells, immature B cells, myeloid-derived suppressor cells (MDSCs), activated B cells, and effective memory CD4 and CD8 T cells. The relationship between the 5 key genes and immune cell infiltration can be seen in Figure 6B. Positive correlations were observed with the 5 key genes for all immune cell types except plasmacytoid dendritic cells and CD56 bright natural killer cells. Notably, neutrophils exhibited the strongest positive correlation among all immune cell types. The findings indicated immune cell infiltration may participate in the pathogenesis of UC, and angiogenesis-related genes may contribute to its development.
Figure 6.
Immune cell infiltration analysis. (A) 28 distinct immune cell subtype compositions in both UC and normal tissue samples. (B) Spearman correlation between 5 key genes with immune infiltrating cells. ***P < 0.001, **P < 0.01, *P < 0.05.
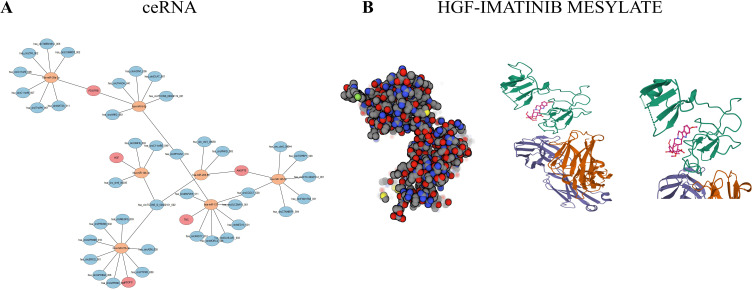
Construction of the ceRNA Network
MicroRNAs, as widely researched epigenetic regulators, hold significant promise as therapeutic targets for a wide range of human diseases. ceRNAs are a novel regulator of gene silencing in which CircRNAs compete with miRNAs via miRNA response elements, thereby sequestering miRNAs from mRNA targets and diminishing gene silencing. We constructed a ceRNA network that includes cirRNAs, miRNAs, and the 5 key genes as a way to understand the regulation mechanisms of these genes. We performed a comprehensive analysis using TargetScan, miRTarBase, and starbase databases, resulting in the identification of 7 miRNAs that bind to the key genes of interest. Additionally, we identified 39 circRNAs that have the potential to bind to these miRNAs (Figure 7A). The analysis revealed the involvement of numerous pathway genes in ceRNA regulations, indicating their potential significance in mediating cross-talks. Nevertheless, further verification is necessary to elucidate the specific mechanism underlying this ceRNA network.
Figure 7.
ceRNA and binding mode of screened drugs to their targets by molecular docking. (A) The integrated CircRNA-miRNA-hub genes network, Red circle: key genes. Orange circle: miRNA. Blue circle: CircRNARNA. (B) Binding mode of vegfc to SUNITINIB.
Targeting Drug Prediction and Molecular Docking
Angiogenesis plays an important role in the pathogenesis of UC, yet antiangiogenic medications are unclear in clinical trials. Using the DGIdb database, we screened the 5 key genes for potential small molecule compounds for UC management. The top 4 predicted therapeutic agents for each gene are shown in Table 2. For PDGFRB, BECAPLERMIN shows the highest scores. VEGFC results highlight VGX-100 with the highest Interaction Score. ANGPT2 data reveals NESVACUMAB with remarkably high scores, particularly its Interaction Score. TNC presents four compounds with identical scores, suggesting similar potential. For HGF, RILOTUMUMAB and FICLATUZUMAB show equally high scores. The role of molecular docking in structure-based drug design and screening is to identify the optimal conformation that allows small molecule compounds to interact with their targets. Autodock Vina v.1.2.2 was used to determine the binding poses and interactions of the two drug candidates with the respective proteins. As shown in Figure 7B, we calculated the binding energies for each interaction. IMATINIB MESYLATE exhibits visible hydrogen bonding and robust electrostatic interactions with HGF (binding energy −7.3 kcal/mol). Due to limitations in the molecular docking databases, we were unable to find suitable docking models for the other proteins. The conceptual findings suggest that the pathogenesis of UC involves distinct angiogenic regulation, which contributes to the maintenance of chronic inflammation in the bowel. Interventions aimed at enhancing antiangiogenic gene expression or inhibiting proangiogenic mediators present promising avenues for future IBD treatments.
Table 2.
Potential Top Drug Compounds for 5 Hubgenes
| pdgfrb | vegfc | angpt2 | tnc | hgf | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug | Query Score | Interaction Score | Drug | Query Score | Interaction Score | Drug | Query Score | Interaction Score | Drug | Query Score | Interaction Score | Drug | Query Score | Interaction Score |
| BECAPLERMIN | 10.76 | 2.18 | VGX-100 | 4.3 | 10.3 | NESVACUMAB | 12.91 | 46.37 | F16SIP 131I | 4.3 | 12.37 | RILOTUMUMAB | 10.76 | 12.88 |
| PETROSIOL A | 8.61 | 1.74 | AFLIBERCEPT | 1.72 | 4.12 | MEDI-3617 | 4.3 | 15.46 | 81C6 131I | 4.3 | 12.37 | FICLATUZUMAB | 10.76 | 12.88 |
| CDP-860 | 4.3 | 0.87 | CONBERCEPT | 1.08 | 2.58 | TREBANANIB | 2.15 | 7.73 | 8H9 131I | 4.3 | 12.37 | MP-0250 | 2.15 | 2.58 |
| SUNITINIB | 2.87 | 0.29 | SUNITINIB | 0.44 | 0.53 | RIBAVIRIN | 0.27 | 0.97 | TENATUMOMAB | 4.3 | 12.37 | IMATINIB MESYLATE | 1.72 | 1.03 |
Discussion
Our study focused on several key genes involved in angiogenesis in ulcerative colitis (UC), including PDGF, VEGFC, ANGPT2, TNC, and CD99. Previous research has examined these genes individually in UC, supporting our findings. Kumagai et al demonstrated the expression of PDGF in areas of active inflammation and fibrosis in inflammatory bowel disease.57 Tacconi et al and D’Alessio et al highlighted VEGFC’s role in ameliorating experimental colitis.11,58 Wang et al showed that silencing ANGPT2 alleviated UC symptoms.59 Ning et al found increased levels of TNC in UC patients,60 while Jodeleit et al identified CD99 as a potential biomarker in UC.61 Our research takes a novel approach by examining these angiogenesis-related genes as part of an integrated network in UC, leveraging advanced bioinformatics techniques. This holistic perspective allows us to better understand the complex interplay between these factors in UC pathogenesis, providing a more comprehensive picture of the role of angiogenesis in UC and paving the way for more targeted therapeutic strategies. By intersecting DE-AGGs with WGCNA modules curated genes, five key angiogenesis genes (pdgfrb, vegfc, angpt2, tnc, hgf) were identified as potential biomarkers for UC. pdgfrb, vegfc, and hgf have been previously reported in intestinal tissues of UC patients compared to controls.58,62,63 These pro-angiogenic factors are implicated in pathological neovascularization, immune cell recruitment, and perpetuation of inflammation based on prior UC research.64 Our findings of upregulated expression of these 5 genes in UC are consistent with previous observations.
It is well established that pathological angiogenesis driven by pro-angiogenic growth factors like VEGF contributes to chronic inflammation in UC.65 The PDGFR signaling pathway is integral to angiogenesis and tissue remodeling, processes that are dysregulated in UC.66 In the context of UC, PDGFR signaling contributes to increased vascular permeability and the recruitment of inflammatory cells.57 Moreover, PDGF has been shown to stimulate the proliferation and activation of fibroblasts, potentially contributing to the fibrosis observed in chronic UC.29 The PI3K-Akt signaling pathway, on the other hand, is a central regulator of cell survival, proliferation, and metabolism. In UC, aberrant activation of this pathway has been associated with enhanced inflammatory responses and resistance to apoptosis in immune cells.67 Specifically, PI3K-Akt signaling promotes the survival and activation of T cells, which are key players in the chronic inflammation characteristic of UC.68 Our findings of enriched PDGFR and PI3K-Akt pathways not only corroborate their known involvement in UC but also suggest their potential as therapeutic targets. Furthermore, angpt2 may disrupt intestinal barrier integrity and permit leukocyte infiltration to drive colitis.69 tnc can also exacerbate inflammation through effects on epithelial permeability and immune cell chemotaxis.70 Lastly, despite its protective roles, persistent hgf production has been linked to chronic inflammation in UC models.71 In our study, our screen validating elevated expression of these 5 angiogenesis-related genes aligns with prior demonstrations of their pro-inflammatory and pro-angiogenic roles in UC pathogenesis.14 It is interesting to note that these genes also play a significant role in promoting tumor development in many types of cancer.72,73 Further research will be important to fully elucidate the specific mechanisms by which these angiogenesis genes influence intestinal inflammation in UC.
The pathway enrichment analysis of differentially expressed genes (DEGs) in UC provided insights into the underlying mechanisms. Gene ontology analysis revealed up-regulated genes were enriched in pathways related to immune processes like T cell activation, cytokine signaling, and cell adhesion. This is consistent with the critical role of aberrant immune responses in UC pathogenesis.74 Meanwhile, down-regulated genes showed enrichment in pathways involved in metabolism like fatty acid oxidation and cytochrome P450 drug metabolism. This suggests UC is associated with disruptions in metabolic homeostasis. KEGG analysis further demonstrated up-regulated gene enrichment in inflammatory pathways including cytokine–cytokine receptor interactions, chemokine signaling, and rheumatoid arthritis pathways. The involvement of these inflammatory pathways aligns with the chronic inflammation in UC. In contrast, down-regulated genes were enriched in bile secretion and drug metabolism pathways. Dysregulation of bile acid metabolism is known to contribute to intestinal inflammation. Altered drug metabolism likely relates to pharmacotherapy challenges in UC patients. Overall, the pathway analysis pointed to upregulation of inflammatory and immune pathways along with downregulation of metabolic and bile/drug pathways. These results are consistent with current knowledge of the pathways implicated in UC pathogenesis and complications.75
MicroRNAs also play crucial roles in UC progression and associated neoangiogenesis. Notably, miR-331-3p promotes angiogenesis and tumor growth in colorectal cancer by targeting NRP2, a VEGF co-receptor (Wang et al, 2016). Conversely, hsa-let-7d-5p exhibits tumor-suppressive properties through K-RAS regulation (Wang et al, 2018). These microRNAs may interact with the angiogenesis-related genes identified in our study, such as VEGFA and its receptors, adding complexity to UC’s angiogenic processes. Future research exploring the interplay between these microRNAs and our identified genes could provide a more comprehensive understanding of angiogenic mechanisms in UC progression to cancer.
The CIBERSORT analysis revealed increased enrichment of various immune cell types in UC compared to normal controls, including myeloid cells, B cells, activated T cells, natural killer cells, and memory T cells. This immune infiltrate correlates with the chronic inflammation in UC.76 Specifically, the 5 identified hub genes showed positive correlations with most infiltrating immune cells, especially neutrophils. This suggests proangiogenic signaling mediated by these genes may help promote immune cell recruitment into inflamed UC tissue.77 Contrary to previous studies, there was no correlation between the hub genes and plasmacytoid dendritic cells or natural killer cells.78 The implications of this specific finding are unclear and warrant further investigation. Overall, the results indicated immune cell infiltration, particularly of neutrophils, plays a key role in UC pathogenesis. The identified angiogenesis-related genes likely contribute by enhancing localized inflammation and immune cell recruitment.79 This aligns with knowledge that neovascularization helps facilitate leukocyte extravasation into tissues.80,81
In our study, we constructed a ceRNA network to elucidate the regulatory mechanisms of key genes in UC progression. Recent research has highlighted the importance of specific microRNAs, particularly miR-331-3p and hsa-let-7d-5p, in the oncological progression of UC to colorectal cancer (CRC). Chacon-Millan et al identified these miRNAs as upregulated in UC progression to CRC, connecting them to known colitis-associated CRC mRNAs.82 Their findings align with our ceRNA network analysis, although specific gene targets differed. Additionally, Rao et al demonstrated miR-331-3p’s crucial role in UC progression through its interaction with lncRNA UCA1 and BRD4,83 supporting our approach of constructing a comprehensive ceRNA network.
While our research identified different specific interactions, the overall regulatory patterns and the importance of miRNA-mediated gene silencing in UC progression align with these recent findings.
The computational screening predicted imatinib and sunitinib as potential small molecule compounds targeting the identified proangiogenic hub genes in UC. Imatinib against pdgfrb and sunitinib against vegfc showed favorable binding profiles in the molecular docking models. The receptor tyrosine kinase PDGFR-beta was identified as the target of the top predicted agent imatinib. PDGF signaling has been implicated in pathological intestinal fibroblast proliferation underlying stricture formation and complications in UC patients.84 Therefore, attenuation of PDGFR activation may confer antifibrotic effects alongside anti-inflammatory benefits.85 The upregulated expression of PDGFR-beta reflects dysfunction of PDGF-mediated pathways in the UC microenvironment, providing grounds for corrective targeting. The predicted therapeutic sunitinib targets VEGF signaling, which plays key pro-angiogenic and pro-inflammatory roles in experimental colitis. Preclinical rodent studies of sunitinib demonstrated ameliorated macroscopic and histological damage in DSS-induced inflammation compared to vehicle treatment.86 These earlier animal model investigations lend proof-of-concept support for sunitinib efficacy in IBD scenarios.
Tailoring their use based on angiogenesis-related gene expression profiles, as our study enables, could improve outcomes compared to untargeted application. However, previous inconsistencies highlight the need for robust validation. Direct head-to-head comparisons to existing biologics will be important to determine if angiogenesis-targeted therapies provide meaningful advantages for UC management.
To our knowledge, this is the first comprehensive analysis exploring angiogenesis in UC. Limitations should be acknowledged. First, public databases provided incomplete clinical information on samples, such as unavailable clinicopathologic features for some datasets. Second, our analysis relied on RNA sequencing data. Although animal experiments supported the bioinformatics findings, reproducibility and generalizability need validation in future clinical samples, as acquiring sufficient UC samples was unfeasible presently. Third, the ceRNA network and drug predictions were based on in silico analyses without ex vivo confirmation, thus requiring further experimental validation.
While this study established an initial foundation around angiogenesis-related genes in UC, deeper elucidation of functional mechanisms was outside the current scope but warrants future work. Specifically, the use of single-cell RNA sequencing and tools like CIBERSORTx could enable the construction of cell type-specific gene expression signatures within the UC immune microenvironment. Deconvoluting subset-specific profiles could provide enhanced resolution on the mechanistic interplay between immune cells, signaling pathways, and vascular processes compared to bulk tissue analysis. Additionally, exploring genetic regulation by integrated miRNA and circRNA networks with experimental validation could better delineate upstream control of the identified biomarkers. By spotlighting these avenues as limitations in the current analysis, we hope to motivate multi-dimensional mechanistic exploration of angiogenesis and inflammation in UC pathogenesis.
While our study provides valuable insights into angiogenesis-related gene signatures in UC, it is important to acknowledge several limitations. Our analysis primarily relied on publicly available datasets, which may have inherent biases in patient selection or data processing. The bioinformatics approaches used, while powerful, can be influenced by the quality of gene annotations and analytical algorithms. The DSS-induced colitis model, although widely accepted, does not fully recapitulate the complexity of human UC, particularly its chronic nature. Our findings lack direct validation in human UC tissues, which will be crucial for confirming their clinical relevance. By focusing on angiogenesis, we may have overlooked other important pathways contributing to UC pathogenesis. Additionally, our study provides a snapshot of gene expression patterns but does not capture the dynamic changes over the course of the disease or variations across different colonic regions. Despite these limitations, we believe our study offers valuable insights into the role of angiogenesis in UC and identifies potential new biomarkers and therapeutic targets. Future research addressing these limitations will be essential to further validate and extend our findings.
In summary, these exploratory findings could provide clues into angiogenesis in UC that warrant confirmation through additional mechanistic studies and clinical validation. Our findings open several avenues for future research. Key priorities include in vivo validation of identified biomarkers in larger UC patient cohorts, functional studies to elucidate the mechanistic roles of these genes and pathways, and exploration of novel therapeutic targets. Integration with other “omics” data and longitudinal studies could provide a more comprehensive understanding of UC pathogenesis. Additionally, investigating the potential of our findings in personalized medicine approaches and conducting long-term clinical studies to evaluate their utility in clinical practice will be crucial. These directions aim to translate our results into improved diagnosis, treatment, and management strategies for UC patients.
Conclusion
Our study identified and validated five key angiogenesis-related genes - pdgfrb, vegfc, angpt2, tnc, and hgf, which involved in inflammatory processes and immunoregulatory mechanisms, suggesting their potential as diagnostic biomarkers for UC. Additionally, our analysis predicted imatinib as a potential therapeutic targeting these angiogenesis-related genes in UC treatment.
Acknowledgments
The authors gratefully acknowledge the National Cancer Institute for providing the Gene Expression Omnibus dataset used in this study. We also sincerely thank the editors and reviewers for their insightful critiques and suggestions, which significantly strengthened the quality of this paper.
Funding Statement
This work was supported by the Medical and Health Science and Technology Program of Zhejiang Province, grant number 2023KY1317 and the Taizhou Science and Technology Bureau Fund, grant number 23ywa23.
Data Sharing Statement
The data analyzed in this study were obtained from the public Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/geo/). The R code used for analysis in this work is available from the corresponding author upon reasonable request.
Ethics Approval
All animal procedures were conducted in accordance with the Guide for the Care and Use of Laboratory Animals and the ARRIVE guidelines. The study protocol, including animal experiments, was approved by the Institutional Animal Care and Use Committee (Approval No. YXSW2308141850). All efforts were made to minimize animal suffering and reduce the number of animals used.
For the human data component, this study utilized publicly available data from open databases. According to our institution’s ethical policy, studies using only publicly available data do not require additional ethical review or Institutional Review Board (IRB) approval. Therefore, this aspect of our study was exempt from additional ethical review.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ng SC, Shi HY, Hamidi N. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–2778. doi: 10.1016/S0140-6736(17)32448-0 [DOI] [PubMed] [Google Scholar]
- 2.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46–54.e42;quize30. doi: 10.1053/j.gastro.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 3.Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389(10080):1756–1770. doi: 10.1016/S0140-6736(16)32126-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D’Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007;132(2):763–786. doi: 10.1053/j.gastro.2006.12.038 [DOI] [PubMed] [Google Scholar]
- 5.Fumery M, Singh S, Dulai PS, Gower-Rousseau C, Peyrin-Biroulet L, Sandborn WJ. Natural history of adult ulcerative colitis in population-based cohorts: a systematic review. Clin Gastroenterol Hepatol. 2018;16(3):343–356.e3. doi: 10.1016/j.cgh.2017.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deban L, Correale C, Vetrano S, Malesci A, Danese S. Multiple pathogenic roles of microvasculature in inflammatory bowel disease: a Jack of all trades. Am J Pathol. 2008;172(6):1457–1466. doi: 10.2353/ajpath.2008.070593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danese S, Sans M, de la Motte C, et al. Angiogenesis as a novel component of inflammatory bowel disease pathogenesis. Gastroenterology. 2006;130(7):2060–2073. doi: 10.1053/j.gastro.2006.03.054 [DOI] [PubMed] [Google Scholar]
- 8.Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9(6):669–676. doi: 10.1038/nm0603-669 [DOI] [PubMed] [Google Scholar]
- 9.Scaldaferri F, Vetrano S, Sans M, et al. VEGF-A links angiogenesis and inflammation in inflammatory bowel disease pathogenesis. Gastroenterology. 2009;136(2):585–95.e5. doi: 10.1053/j.gastro.2008.09.064 [DOI] [PubMed] [Google Scholar]
- 10.Kapsoritakis A, Sfiridaki A, Maltezos E, et al. Vascular endothelial growth factor in inflammatory bowel disease. Int J Colorectal Dis. 2003;18(5):418–422. doi: 10.1007/s00384-003-0495-y [DOI] [PubMed] [Google Scholar]
- 11.D’Alessio S, Correale C, Tacconi C, et al. VEGF-C-dependent stimulation of lymphatic function ameliorates experimental inflammatory bowel disease. J Clin Invest. 2014;124(9):3863–3878. doi: 10.1172/JCI72189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fagiani E, Christofori G. Angiopoietins in angiogenesis. Cancer Lett. 2013;328(1):18–26. doi: 10.1016/j.canlet.2012.08.018 [DOI] [PubMed] [Google Scholar]
- 13.Saharinen P, Eklund L, Alitalo K. Therapeutic targeting of the angiopoietin-TIE pathway. Nat Rev Drug Discov. 2017;16(9):635–661. doi: 10.1038/nrd.2016.278 [DOI] [PubMed] [Google Scholar]
- 14.Koutroubakis IE, Tsiolakidou G, Karmiris K, Kouroumalis EA. Role of angiogenesis in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12(6):515–523. doi: 10.1097/00054725-200606000-00012 [DOI] [PubMed] [Google Scholar]
- 15.Presta M, Dell’Era P, Mitola S, Moroni E, Ronca R, Rusnati M. Fibroblast growth factor/fibroblast growth factor receptor system in angiogenesis. Cytokine Growth Factor Rev. 2005;16(2):159–178. doi: 10.1016/j.cytogfr.2005.01.004 [DOI] [PubMed] [Google Scholar]
- 16.Kanazawa S, Tsunoda T, Onuma E, Majima T, Kagiyama M, Kikuchi K. VEGF, basic-FGF, and TGF-beta in Crohn’s disease and ulcerative colitis: a novel mechanism of chronic intestinal inflammation. Am J Gastroenterol. 2001;96(3):822–828. doi: 10.1111/j.1572-0241.2001.03527.x [DOI] [PubMed] [Google Scholar]
- 17.Compagni A, Wilgenbus P, Impagnatiello MA, Cotten M, Christofori G. Fibroblast growth factors are required for efficient tumor angiogenesis. Cancer Res. 2000;60(24):7163–7169. [PubMed] [Google Scholar]
- 18.Rutella S, Fiorino G, Vetrano S, et al. Infliximab therapy inhibits inflammation-induced angiogenesis in the mucosa of patients with Crohn’s disease. Am J Gastroenterol. 2011;106(4):762–770. doi: 10.1038/ajg.2011.48 [DOI] [PubMed] [Google Scholar]
- 19.Yoshida S, Ono M, Shono T, et al. Involvement of interleukin-8, vascular endothelial growth factor, and basic fibroblast growth factor in tumor necrosis factor alpha-dependent angiogenesis. Mol Cell Biol. 1997;17(7):4015–4023. doi: 10.1128/MCB.17.7.4015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung YJ, Isaacs JS, Lee S, Trepel J, Neckers L. IL-1beta-mediated up-regulation of HIF-1alpha via an NFkappaB/COX-2 pathway identifies HIF-1 as a critical link between inflammation and oncogenesis. FASEB J. 2003;17(14):2115–2117. doi: 10.1096/fj.03-0329fje [DOI] [PubMed] [Google Scholar]
- 21.Ligumsky M, Simon PL, Karmeli F, Rachmilewitz D. Role of interleukin 1 in inflammatory bowel disease--enhanced production during active disease. Gut. 1990;31(6):686–689. doi: 10.1136/gut.31.6.686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taylor CT, Colgan SP. Hypoxia and gastrointestinal disease. J Mol Med. 2007;85(12):1295–1300. doi: 10.1007/s00109-007-0277-z [DOI] [PubMed] [Google Scholar]
- 23.Semenza GL. Hypoxia-inducible factors in physiology and medicine. Cell. 2012;148(3):399–408. doi: 10.1016/j.cell.2012.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giatromanolaki A, Sivridis E, Maltezos E, et al. Hypoxia inducible factor 1alpha and 2alpha overexpression in inflammatory bowel disease. J Clin Pathol. 2003;56(3):209–213. doi: 10.1136/jcp.56.3.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murdoch C, Muthana M, Lewis CE. Hypoxia regulates macrophage functions in inflammation. J Immunol. 2005;175(10):6257–6263. doi: 10.4049/jimmunol.175.10.6257 [DOI] [PubMed] [Google Scholar]
- 26.Schippers A, Muschaweck M, Clahsen T, et al. β7-Integrin exacerbates experimental DSS-induced colitis in mice by directing inflammatory monocytes into the colon. Mucosal Immunol. 2016;9(2):527–538. doi: 10.1038/mi.2015.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gong Y, Koh DR. Neutrophils promote inflammatory angiogenesis via release of preformed VEGF in an in vivo corneal model. Cell Tissue Res. 2010;339(2):437–448. doi: 10.1007/s00441-009-0908-5 [DOI] [PubMed] [Google Scholar]
- 28.Ardi VC, Kupriyanova TA, Deryugina EI, Quigley JP. Human neutrophils uniquely release TIMP-free MMP-9 to provide a potent catalytic stimulator of angiogenesis. Proc Natl Acad Sci U S A. 2007;104(51):20262–20267. doi: 10.1073/pnas.0706438104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rieder F, Fiocchi C. Intestinal fibrosis in inflammatory bowel disease - Current knowledge and future perspectives. J Crohns Colitis. 2008;2(4):279–290. doi: 10.1016/j.crohns.2008.05.009 [DOI] [PubMed] [Google Scholar]
- 30.Kannengiesser K, Maaser C, Heidemann J, et al. Melanocortin-derived tripeptide KPV has anti-inflammatory potential in murine models of inflammatory bowel disease. Inflamm Bowel Dis. 2008;14(3):324–331. doi: 10.1002/ibd.20334 [DOI] [PubMed] [Google Scholar]
- 31.Gravina AG, Pellegrino R, Durante T, et al. Inflammatory bowel diseases patients suffer from significant low levels and barriers to physical activity: the “BE-FIT-IBD” study. World J Gastroenterol. 2023;29(41):5668–5682. doi: 10.3748/wjg.v29.i41.5668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Danese S, Scaldaferri F, Vetrano S, et al. Critical role of the CD40 CD40-ligand pathway in regulating mucosal inflammation-driven angiogenesis in inflammatory bowel disease. Gut. 2007;56(9):1248–1256. doi: 10.1136/gut.2006.111989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cromer WE, Mathis JM, Granger DN, Chaitanya GV, Alexander JS. Role of the endothelium in inflammatory bowel diseases. World J Gastroenterol. 2011;17(5):578–593. doi: 10.3748/wjg.v17.i5.578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.D’Alessio S, Tacconi C, Fiocchi C, Danese S. Advances in therapeutic interventions targeting the vascular and lymphatic endothelium in inflammatory bowel disease. Curr Opin Gastroenterol. 2013;29(6):608–613. doi: 10.1097/MOG.0b013e328365d37c [DOI] [PubMed] [Google Scholar]
- 35.Alkim C, Alkim H, Koksal AR, Boga S, Sen I. Angiogenesis in inflammatory bowel disease. Int J Inflam. 2015;2015:970890. doi: 10.1155/2015/970890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chidlow Jr JH, Shukla D, Grisham MB, Kevil CG. Pathogenic angiogenesis in IBD and experimental colitis: new ideas and therapeutic avenues. Am J Physiol Gastrointest Liver Physiol. 2007;293(1):G5–G18. doi: 10.1152/ajpgi.00107.2007 [DOI] [PubMed] [Google Scholar]
- 37.Tong J, Meng L, Bei C, et al. Modern Beijing sublineage of Mycobacterium tuberculosis shift macrophage into a hyperinflammatory status. Emerg Microbes Infect. 2022;11(1):715–724. doi: 10.1080/22221751.2022.2037395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jiang X, Xu Y, Chen D, et al. A novel angiogenesis-related prognostic signature associated with the hepatocellular carcinoma immune microenvironment and survival outcome. Int J Gen Med. 2022;15:311–323. doi: 10.2147/IJGM.S349210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yu G, Wang LG, Han Y, He QY. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16(5):284–287. doi: 10.1089/omi.2011.0118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kanehisa M, Sato Y, Kawashima M, Furumichi M, Tanabe M. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. 2016;44(D1):D457–62. doi: 10.1093/nar/gkv1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci U S A. 2005;102(43):15545–15550. doi: 10.1073/pnas.0506580102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinf. 2008;9:559. doi: 10.1186/1471-2105-9-559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liang Q, Guan G, Li X, et al. Profiling pro-neural to mesenchymal transition identifies a lncRNA signature in glioma. J Transl Med. 2020;18(1):378. doi: 10.1186/s12967-020-02552-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen K, Shang S, Yu S, Cui L, Li S, He N. Identification and exploration of pharmacological pyroptosis-related biomarkers of ulcerative colitis. Front Immunol. 2022;13:998470. doi: 10.3389/fimmu.2022.998470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y, Liang Y, Wang Y, Ye F, Kong X, Yang Q. A novel ferroptosis‑related gene signature for overall survival prediction and immune infiltration in patients with breast cancer. Int J Oncol. 2022;61(6). doi: 10.3892/ijo.2022.5438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yuan Y, Li N, Fu M, Ye M. Identification of critical modules and biomarkers of ulcerative colitis by using WGCNA. J Inflamm Res. 2023;16:1611–1628. doi: 10.2147/JIR.S402715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Assaf R, Xia F, Stevens R. Detecting operons in bacterial genomes via visual representation learning. Sci Rep. 2021;11(1):2124. doi: 10.1038/s41598-021-81169-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Song J, Lu Y, Sun W, Han M, Zhang Y, Zhang J. Changing expression profiles of lncRNAs, circRNAs and mRNAs in esophageal squamous carcinoma. Oncol Lett. 2019;18(5):5363–5373. doi: 10.3892/ol.2019.10880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qian Y, Yin J, Ni J, Chen X, Shen Y. A network pharmacology method combined with molecular docking verification to explore the therapeutic mechanisms underlying simiao pill herbal medicine against hyperuricemia. Biomed Res Int. 2023;2023:2507683. doi: 10.1155/2023/2507683 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 50.Guo C, Guo D, Fang L, et al. Ganoderma lucidum polysaccharide modulates gut microbiota and immune cell function to inhibit inflammation and tumorigenesis in colon. Carbohydr Polym. 2021;267:118231. doi: 10.1016/j.carbpol.2021.118231 [DOI] [PubMed] [Google Scholar]
- 51.Zhang Y, Yu B, Tian Y, et al. A novel risk score model based on fourteen chromatin regulators-based genes for predicting overall survival of patients with lower-grade gliomas. Front Genet. 2022;13:957059. doi: 10.3389/fgene.2022.957059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morris GM, Huey R, Olson AJ. Using AutoDock for ligand-receptor docking. Curr Protoc Bioinf. 2008;8–14. doi: 10.1002/0471250953.bi0814s24 [DOI] [PubMed] [Google Scholar]
- 53.Wang Y, Bryant SH, Cheng T, et al. PubChem BioAssay: 2017 update. Nucleic Acids Res. 2017;45(D1):D955–D963. doi: 10.1093/nar/gkw1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhong X, Heinicke F, Rayner S. miRBaseMiner, a tool for investigating miRBase content. RNA Biol. 2019;16(11):1534–1546. doi: 10.1080/15476286.2019.1637680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sticht C, De La Torre C, Parveen A, Gretz N. miRWalk: an online resource for prediction of microRNA binding sites. PLoS One. 2018;13(10):e0206239. doi: 10.1371/journal.pone.0206239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ma Z, Zhong P, Yue P, Sun Z. Identification of immune-related molecular markers in intracranial aneurysm (IA) based on machine learning and cytoscape-cytohubba plug-in. BMC Genom Data. 2023;24(1):20. doi: 10.1186/s12863-023-01121-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kumagai S, Ohtani H, Nagai T, et al. Platelet-derived growth factor and its receptors are expressed in areas of both active inflammation and active fibrosis in inflammatory bowel disease. Tohoku J Exp Med. 2001;195(1):21–33. doi: 10.1620/tjem.195.21 [DOI] [PubMed] [Google Scholar]
- 58.Tacconi C, Schwager S, Cousin N, et al. Antibody-mediated delivery of VEGFC ameliorates experimental chronic colitis. ACS Pharmacol Transl Sci. 2019;2(5):342–352. doi: 10.1021/acsptsci.9b00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang X, Huang J, Liu J, et al. Silencing ANGPT2 alleviates ulcerative colitis by regulating autophagy-mediated NLRP3 inflammasome inactivation via the mTOR signaling pathway. Braz J Med Biol Res. 2024;57:e13379. doi: 10.1590/1414-431x2024e13379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ning L, Li S, Gao J, et al. Tenascin-C is increased in inflammatory Bowel disease and is associated with response to infliximab therapy. Biomed Res Int. 2019;2019:1475705. doi: 10.1155/2019/1475705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jodeleit H, Milchram L, Soldo R, et al. Autoantibodies as diagnostic markers and potential drivers of inflammation in ulcerative colitis. PLoS One. 2020;15(2):e0228615. doi: 10.1371/journal.pone.0228615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Matsumura K, Nakase H, Kosugi I, et al. Establishment of a novel mouse model of ulcerative colitis with concomitant cytomegalovirus infection: in vivo identification of cytomegalovirus persistent infected cells. Inflamm Bowel Dis. 2013;19(9):1951–1963. doi: 10.1097/MIB.0b013e318293c5bf [DOI] [PubMed] [Google Scholar]
- 63.Li N, Zhang Y, Nepal N, et al. Dental pulp stem cells overexpressing hepatocyte growth factor facilitate the repair of DSS-induced ulcerative colitis. Stem Cell Res Ther. 2021;12(1):30. doi: 10.1186/s13287-020-02098-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pousa ID, Maté J, Gisbert JP. Angiogenesis in inflammatory bowel disease. Eur J Clin Invest. 2008;38(2):73–81. doi: 10.1111/j.1365-2362.2007.01914.x [DOI] [PubMed] [Google Scholar]
- 65.Adini A, Ko VH, Puder M, et al. PR1P, a VEGF-stabilizing peptide, reduces injury and inflammation in acute lung injury and ulcerative colitis animal models. Front Immunol. 2023;14:1168676. doi: 10.3389/fimmu.2023.1168676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Valatas V, Bamias G, Kolios G. Experimental colitis models: insights into the pathogenesis of inflammatory bowel disease and translational issues. Eur J Pharmacol. 2015;759:253–264. doi: 10.1016/j.ejphar.2015.03.017 [DOI] [PubMed] [Google Scholar]
- 67.Huang XL, Xu J, Zhang XH, et al. PI3K/Akt signaling pathway is involved in the pathogenesis of ulcerative colitis. Inflamm Res. 2011;60(8):727–734. doi: 10.1007/s00011-011-0325-6 [DOI] [PubMed] [Google Scholar]
- 68.Weaver CT, Hatton RD. Interplay between the TH17 and TReg cell lineages: a (co-)evolutionary perspective. Nat Rev Immunol. 2009;9(12):883–889. doi: 10.1038/nri2660 [DOI] [PubMed] [Google Scholar]
- 69.Park HR, Shiva A, Cummings P, et al. Angiopoietin-2-dependent spatial vascular destabilization promotes T-cell exclusion and limits immunotherapy in melanoma. Cancer Res. 2023;83(12):1968–1983. doi: 10.1158/0008-5472.CAN-22-2838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dhaouadi S, Ben Abderrazek R, Loustau T, et al. Novel human Tenascin-C function-blocking camel single domain nanobodies. Front Immunol. 2021;12:635166. doi: 10.3389/fimmu.2021.635166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stakenborg M, Verstockt B, Meroni E, et al. Neutrophilic HGF-MET signalling exacerbates intestinal inflammation. J Crohns Colitis. 2020;14(12):1748–1758. doi: 10.1093/ecco-jcc/jjaa121 [DOI] [PubMed] [Google Scholar]
- 72.Goel HL, Mercurio AM. VEGF targets the tumour cell. Nat Rev Cancer. 2013;13(12):871–882. doi: 10.1038/nrc3627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin Oncol. 2002;29(6 Suppl 16):15–18. doi: 10.1053/sonc.2002.37263 [DOI] [PubMed] [Google Scholar]
- 74.Zhang YZ, Li YY. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. 2014;20(1):91–99. doi: 10.3748/wjg.v20.i1.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hua YL, Jia YQ, Zhang XS, et al. Baitouweng Tang ameliorates DSS-induced ulcerative colitis through the regulation of the gut microbiota and bile acids via pathways involving FXR and TGR5. Biomed Pharmacother. 2021;137:111320. doi: 10.1016/j.biopha.2021.111320 [DOI] [PubMed] [Google Scholar]
- 76.Huang J, Zhang J, Wang F, Zhang B, Tang X. Revealing immune infiltrate characteristics and potential diagnostic value of immune-related genes in ulcerative colitis: an integrative genomic analysis. Front Public Health. 2022;10:1003002. doi: 10.3389/fpubh.2022.1003002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang C, Zhang J, Zhang Y, et al. Identifying neutrophil-associated subtypes in ulcerative colitis and confirming neutrophils promote colitis-associated colorectal cancer. Front Immunol. 2023;14:1095098. doi: 10.3389/fimmu.2023.1095098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kanauchi Y, Yamamoto T, Yoshida M, et al. Cholinergic anti-inflammatory pathway ameliorates murine experimental Th2-type colitis by suppressing the migration of plasmacytoid dendritic cells. Sci Rep. 2022;12(1):54. doi: 10.1038/s41598-021-04154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Asare Y, Schmitt M, Bernhagen J. The vascular biology of macrophage migration inhibitory factor (MIF). Expression and effects in inflammation, atherogenesis and angiogenesis. Thromb Haemost. 2013;109(3):391–398. doi: 10.1160/TH12-11-0831 [DOI] [PubMed] [Google Scholar]
- 80.McGarry T, Biniecka M, Veale DJ, Fearon U. Hypoxia, oxidative stress and inflammation. Free Radic Biol Med. 2018;125:15–24. doi: 10.1016/j.freeradbiomed.2018.03.042 [DOI] [PubMed] [Google Scholar]
- 81.Galkina E, Ley K. Leukocyte recruitment and vascular injury in diabetic nephropathy. J Am Soc Nephrol. 2006;17(2):368–377. doi: 10.1681/ASN.2005080859 [DOI] [PubMed] [Google Scholar]
- 82.Chacon-Millan P, Lama S, Del Gaudio N, et al. A combination of microarray-based profiling and biocomputational analysis identified miR331-3p and hsa-let-7d-5p as potential biomarkers of ulcerative colitis progression to colorectal cancer. Int J Mol Sci. 2024;25(11):5699. doi: 10.3390/ijms25115699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rao J, Shao L, Lin M, Huang J, Fan L. LncRNA UCA1 accelerates the progression of ulcerative colitis via mediating the miR-331-3p/BRD4 axis. Int J Gen Med. 2021;14:2427–2435. doi: 10.2147/IJGM.S304837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Di Sabatino A, Jackson CL, Pickard KM, et al. Transforming growth factor beta signalling and matrix metalloproteinases in the mucosa overlying Crohn’s disease strictures. Gut. 2009;58(6):777–789. doi: 10.1136/gut.2008.149096 [DOI] [PubMed] [Google Scholar]
- 85.Nair DG, Miller KG, Lourenssen SR, Blennerhassett MG. Inflammatory cytokines promote growth of intestinal smooth muscle cells by induced expression of PDGF-Rβ. J Cell Mol Med. 2014;18(3):444–454. doi: 10.1111/jcmm.12193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Knod JL, Crawford K, Dusing M, Frischer JS. Murine colitis treated with multitargeted tyrosine kinase inhibitors. J Surg Res. 2016;200(2):501–507. doi: 10.1016/j.jss.2015.09.023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed in this study were obtained from the public Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/geo/). The R code used for analysis in this work is available from the corresponding author upon reasonable request.