Abstract
Background
In China, investigations into the efficacy of neurological clinical teaching try to ascertain the impacts of various teaching methods on intervention outcomes. However, these studies often suffer from limited sample sizes, single-center studies and low quality, compounded by the lack of direct comparative analyses between teaching methods, thereby leaving the identification of the most effective method unresolved. This study aims to compare the effectiveness of various teaching methods in the standardized training of Chinese neurology clinicians to inform an optimal teaching model utilizing a Bayesian network meta-analysis (NMA) approach.
Methods
A comprehensive computer search was conducted to identify randomized controlled trials (RCTs) assessing the efficacy of 7 teaching methods: problem-based learning (PBL), case-based learning (CBL), flipped classroom model (FCM), evidence-based medicine (EBM), clinical practice (CP), team-based learning (TBL), and lecture-based learning (LBL). The search, which spanned databases including the China National Knowledge Infrastructure (CNKI), Chinese Citation Database (CDD), China Science Periodical Database (CSPD), Chinese BioMedical Literature Database (CBM), PubMed, Web of Science, and the Cochrane Library, covered the period from the inception of these databases to April 1, 2023. The quality of the included studies was evaluated, and the data were analyzed in R 4.3.2 and Stata 17.0 software.
Results
From the 31 studies included, comprising 2124 subjects, significant findings emerged. In theoretical examinations, a statistically significant difference was noted among the teaching methods, with CBL, PBL, TBL, FCM, and EBM showing superior performance over the LBL method. The effectiveness ranking of these methods was as follows: CBL > PBL > TBL > FCM > EBM > CP > LBL. In terms of practical skills examinations, a similar pattern of effectiveness was observed. Here, the order of effectiveness was CBL > EBM > PBL > TBL > FCM > CP > LBL.
Conclusions
This NMA indicated that the modern teaching pedagogies, particularly CBL, could be effective in neurology education, and might help improve the theoretical examinations and practical skills of neurology clinicians. Fully tapping into the strengths of modern teaching methods in neurology teaching will require additional work and advancing research.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06397-9.
Keywords: Neurology: teaching method, Teaching effectiveness, Bayesian network meta-analysis (NMA), Education
Background
In China, neurology, as a rigorously scientific and highly practical secondary clinical discipline, is characterized by its multitude of diseases, easy confusion, and complex physiological and pathological mechanisms, along with a strong requirement for specialized skills [1]. This makes the teaching requirements for neurology stringent. For example, neurology involves various diseases, such as stroke and Parkinson’s, whose complexity requires a deeper level of understanding. In this field, specialized skills are not only technical but also an understanding and accurate application of complex mechanisms [2]. Therefore, considering these characteristics, the teaching requirements for neurology are more urgent. However, clinical teaching methods in neurology still primarily adopt traditional approaches, mainly lecture-based learning (LBL), where teachers in classrooms impart knowledge to students within limited time. This traditional teaching method has some issues, such as limited opportunities for student interaction and practical experience, making it challenging to stimulate students’ active learning and critical thinking [3]. A learning model primarily based on lectures may not meet the requirements of modern neurology teaching. Modern education needs to emphasize student participation, interaction, and practical experience to cultivate students’ ability to independently think and apply knowledge in clinical practice.
Currently, researchers have conducted in-depth studies on the reform of teaching methods in neurology. This paper involves six innovative teaching methods: problem-based learning (PBL), case-based learning (CBL), flipped classroom model (FCM), evidence-based medicine (EBM), clinical practice (CP), team-based learning (TBL). The seven teaching methods included in this study were selected based on their proven efficacy in enhancing neurology education, as demonstrated in both general medical education literature and neurology-specific research. These methods were also chosen for their relevance to the current trends in active learning and competency-based education, which are increasingly emphasized in neurology training. While many teaching approaches are widely discussed in medical education, the methods included here were specifically selected due to their applicability to the unique challenges faced by neurology educators and trainees, such as the integration of complex clinical reasoning, diagnostic skills, and hands-on practice. Although the specific forms of these teaching methods vary, they all can better stimulate the initiative and enthusiasm of neurology students, promote the transition from the past “I have to learn” to “I want to learn” learning mode, and achieve better teaching results.
In response to the different modes of teaching described above, China has conducted several previous randomized controlled trials (RCTs) on the impact of neurological clinical teaching effectiveness to verify the effects of different teaching methods on intervention measures’ effectiveness. For example, in the study of Ma et al., a total of 240 neurology interns were randomly assigned to explore the effectiveness of CBL, and the results revealed that the CBL instruction significantly outperformed the LBL teaching in comprehensive abilities, clinical skills, and theoretical knowledge, which indicated that the application of CBL can effectively enhance students’ academic proficiency and practical skills [4]. Cai et al. analyzed the implementation of PBL in the teaching of 50 clinical neurology residents and found a significant improvement in both theoretical and practical scores for the PBL group compared to the control group [5]. Additionally, Long et al. found that the students in the PBL group exhibited higher satisfaction with the teaching approach, indicating its notable advantages in enhancing students’ analytical problem-solving abilities and motivation for learning [6].
These methods have not only sparked interns’ interest but also elevated students’ theoretical knowledge and practical skills. However, previous RCTs related to neurology teaching often suffer from issues such as small sample sizes, single-center studies, or low methodological quality. Furthermore, there is a lack of direct comparisons between the effectiveness of different teaching methods, and the optimal teaching method remains undetermined. Therefore, it is necessary and of practical significance to assess the impact of various teaching methods on neurology teaching effectiveness. Bayesian network meta-analysis (NMA) allows for simultaneous analysis and comparison of multiple different intervention factors within the same evidence framework based on traditional meta-analysis, ultimately leading to comprehensive rankings and assessments [7]. This study utilizes the Bayesian NMA method to analyze the effects of different teaching methods on the effectiveness of Chinese neurology teaching, aiming to provide references for selecting or constructing the optimal teaching model for this discipline. The results of this study will contribute to a better understanding of the effects of various teaching methods, provide empirical support for neurology teaching, and drive educational reforms in the field.
Methods
Study design
This review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines [8]. The researcher (LXY) has registered and published a Meta-analysis plan on the International System Evaluation/Meta-Analysis Registration Platform (https://inplasy.com), with the Registration Number: INPLASY202340025. The plan provides valuable insights into the intended scope and objectives of the meta-analysis. Meanwhile, the review included studies published by institutions within China, irrespective of the language of publication. Both English-language journals and Chinese-language journals were considered for inclusion, provided they met the predefined eligibility criteria.
Literature search
The China National Knowledge Infrastructure (CNKI), Chinese Citation Database (CDD), China Science Periodical Database (CSPD), Chinese BioMedical Literature Database (CBM), PubMed, Web of Science, and Cochrane Library were systematically searched from their inception to April 1, 2023. A search strategy was developed, as illustrated in Supplementary Table S1 using PubMed as an example. The search terms mainly comprised four aspects: 1) “problem-based learning” OR “PBL” OR “case-based learning” OR “CBL” OR “evidence-based medicine” OR “EBM” OR “flipped-class model” OR “FCM” OR “clinical pathway learning” OR “CP learning” OR “Team-based Learning” OR “TBL” AND 2) “neurology” AND 3) “regulation training” OR“graduate” OR “undergraduate” OR “apprentice” 4) “comparative study” OR “comparison” OR “randomized control” OR “randomization”. Furthermore, corresponding modifications were made to accommodate the requirements of different databases. In addition, the reference lists of relevant reviews or meta-analyses were manually screened to identify potentially eligible publications.
Inclusion and exclusion criteria
To ensure the precision and relevance of our study, we established inclusion criteria following the evidence-based PICOS principles. The criteria are structured as follows: (1) P (participant, subjects): neurology interns or residents undergoing standardized training in China; (2) I (intervention): PBL, CBL, EBM, FCM, TBL, CP teaching methods; (3) C (comparison): lecture-based learning (LBL); (4) O (outcome): theoretical exams or practical skill performance; (5) S (study design): randomized controlled trial (RCT) studies.
The exclusion criteria were as follows: (1) even through email inquiries, outcome measures that cannot be transformed into valid data expressed in a quantitative manner; (2) single-arm studies or cross-sectional studies; (3) literature with suspected duplicate publication or inaccessible full text; (4) using two or more teaching methods in the experimental group; (5) theoretical explorations, reviews, and meta-analyses.
Quality assessment
For the quality evaluation of the included studies, two researchers (LXY, ZJC) utilized the ROB bias risk assessment tool to evaluate potential biases within the included studies. Employing the bias risk assessment criteria from the Cochrane Handbook 5.1.0 [9], each criterion—such as random sequence generation, allocation concealment, blinding participants and personnel, blinding outcome assessment, incomplete outcome data, selective reporting, other bias—was meticulously assessed and categorized as “low risk,” “unclear,” or “high risk.” Recognizing the inherent challenges in blinding within teaching methods, where blinding of teachers and students is often unfeasible, a nuanced approach was adopted. In instances where lack of blinding was unlikely to significantly impact the outcome indicators, a “low risk” rating was assigned. This consideration was crucial to maintain a fair evaluation, accounting for the complexities of implementing blinding techniques within educational interventions.
However, the application of randomized experiments in educational research has been met with different opinions from scholars [10, 11]. Some argue that achieving complete blinding of both teachers and students in such settings may be infeasible [12]. This limitation calls into question the suitability of the Cochrane Handbook for accurately reflecting the quality of studies incorporated into meta-analyses in this context. To our knowledge, no evaluation tool has been developed specifically to assess the quality of these types of studies in the educational field.
Data extraction and literature screening
The literature selection process involved several systematic steps to ensure accuracy and reliability. The process began with the researcher (LXY) importing search results from various databases into EndNoteX9 reference management software, effectively eliminating duplicate literature. Following deduplication, two researchers (LXY, ZJC) independently assessed the titles and abstracts of the remaining literature. Using predetermined inclusion and exclusion criteria, irrelevant literature was excluded. Subsequently, the two researchers obtained and reviewed the full text of the selected articles, applying a rigorous screening process. In instances where disagreements arose between the two researchers, a resolution was sought through consultation with a third researcher (HX). The involvement of a third researcher aimed to provide an impartial perspective, contributing to a fair and balanced decision-making process. Ultimately, the inclusion of each study was determined through collaborative discussion and consensus among the research team. A standardized literature extraction form was used to extract information, including author, year, title, sample size, age, gender, intervention measures, control measures, and outcome indicators. This systematic and collaborative approach to the literature screening ensures the robustness and reliability of the selected studies, minimizing the potential for bias and enhancing the overall quality of the research process.
Statistical analysis
We utilized BUGSnet package [13] within R 4.3.2 software for Bayesian inference, employing Gibbs sampling to conduct a network meta-analysis of theoretical and practical skill performance. This program, developed by Béliveau and colleagues, stands out as a free, open-source R package that is visually powerful and fully functional and is specifically designed for Bayesian NMA analysis. It aligns with the PRISMA-NMA reporting guidelines established by Hutton [14] and other specifications for meta-analysis reports. For our analysis, we adopted the mean differences (MDs) as the outcome measure, accompanied by its corresponding 95% confidence intervals (95% CIs). The random-effects model was used to obtain more conservative conclusions regardless of heterogeneity [15]. An MD > zero indicates a higher score of the intervention teaching strategy, and 95% CI that did not include zero was considered statistically significant. The selection of the optimal fitting model was guided by the Deviance Information Criterion (DIC). Initial values were set with three Markov chains, the first iteration count at 1000, and subsequent iterations at 50,000. To mitigate initial value influences, an annealing process was implemented during the first 10,000 iterations, and sampling commenced from iteration 10,001 onward. In assessing the effectiveness of each teaching method in neurology, the surface under the cumulative ranking (SUCRA) was employed. The larger the area under the curve, the higher the ranking, the more effective the teaching method in the field [16]. Publication bias was evaluated visually by creating funnel plots via Stata 17.0 (Stata Corp, College Station, TX, USA), as well as by conducting Begg’s tests using meta package installed R software for outcomes with 5 or more studies [17]. p-value < 0.05 was considered as statistically significant publication bias.
Results
Study characteristics
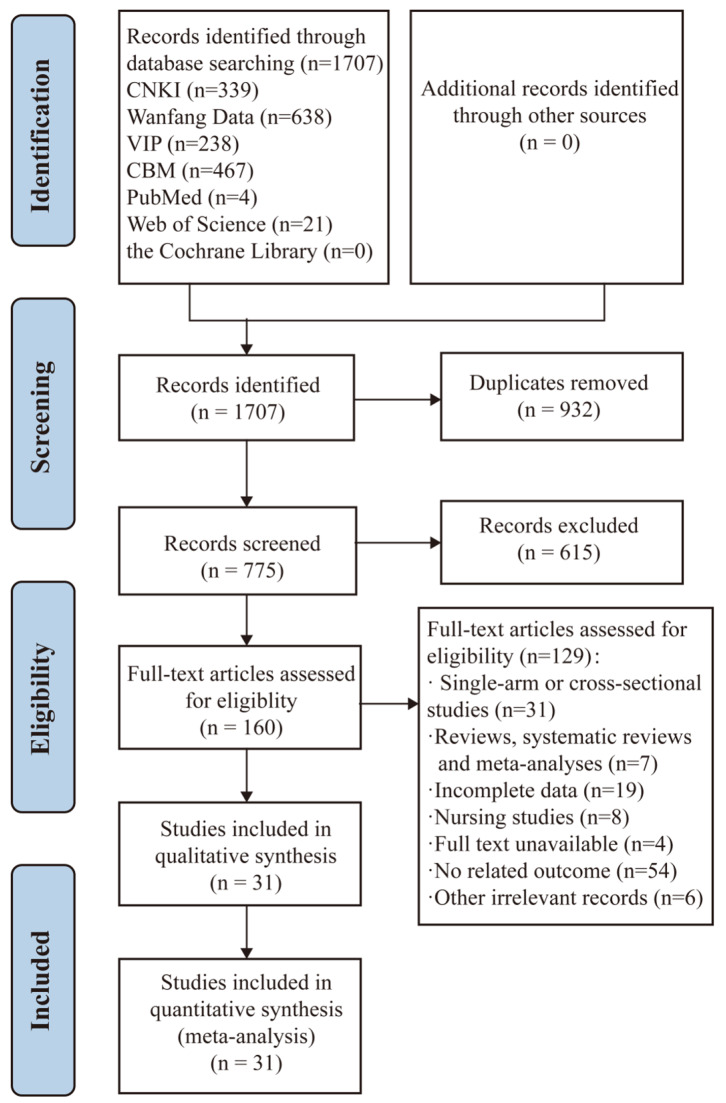
The literature retrieval process is shown in Fig. 1. Initially, 1707 relevant articles were obtained based on the search strategy, and after deduplication, 31 articles were selected. The basic characteristics of the literature are shown in Table 1, including a total of 2,124 research subjects, with 1,062 cases in both the experimental and control groups.
Fig. 1.
Flowchart of the literature search
Table 1.
Characteristics of the studies included in this network meta-analysis
| Reference | Region | Sample size | Age (year) | Sex (M/F) | Subjects | Duration (month) |
Interventions | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | T | C | |||||
| Xu et al. 2016 [18] | Zhejiang | 40 | 40 | 20.50 ± 2.30 | 20.70 ± 1.90 | 24/16 | 26/14 | interns | 13 | CBL | LBL | ①② |
| Zhang et al. 2018 [19] | Beijing | 50 | 50 | 27.77 ± 2.22 | 27.72 ± 2.12 | 30/20 | 29/21 | interns | 15 | CBL | LBL | ①② |
| Ma et al. 2018 [4] | Xinjiang | 120 | 120 | - | - | 73/47 | 72/48 | interns | - | CBL | LBL | ①② |
| Dong et al. 2018 [20] | Jiangsu | 25 | 25 | 26.07 ± 1.03 | 26.11 ± 0.97 | 5/20 | 6/19 | residents | 13 | CBL | LBL | ①② |
| Tang et al. 2019 [21] | Chongqing | 24 | 24 | 25.87 ± 1.22 | 25.69 ± 1.17 | 9/15 | 10/14 | residents | 12 | CBL | LBL | ①② |
| Peng et al. 2021 [22] | Hunan | 21 | 21 | 22.49 ± 1.59 | 22.40 ± 1.61 | 10/11 | 9/12 | interns | 13 | CBL | LBL | ①② |
| Li et al. 2021 [23] | Jiangsu | 23 | 23 | 21.31 ± 0.57 | 24.44 ± 0.63 | 10/13 | 8/15 | interns | 13 | CBL | LBL | ①② |
| Yang et al. 2022 [24] | Sichuan | 30 | 30 | 25.10 ± 1.09 | 25.13 ± 1.17 | 15/15 | 16/14 | interns | 12 | CBL | LBL | ① |
| Zhou et al. 2019 [25] | Shanghai | 20 | 20 | - | - | - | - | interns | 26 | CP | LBL | ①② |
| Hou et al. 2022 [26] | Guangdong | 20 | 20 | 24.18 ± 0.54 | 24.31 ± 0.53 | 9/11 | 10/10 | residents | 61 | CP | LBL | ①② |
| Li et al. 2012 [27] | Henan | 20 | 20 | - | - | - | - | interns | 6 | EBM | LBL | ①② |
| Jiang et al. 2017 [28] | Jiangsu | 31 | 31 | - | - | - | - | residents | 36 | EBM | LBL | ① |
| Jiang et al. 2020 [29] | Hubei | 40 | 40 | 21.84 ± 1.13 | 21.23 ± 1.11 | 21/19 | 22/18 | interns | 13 | EBM | LBL | ①② |
| Zhang et al. 2019 [30] | Henan | 42 | 43 | 21.90 ± 0.80 | 21.80 ± 0.70 | 20/22 | 22/21 | interns | 10 | FCM | LBL | ①② |
| Chen et al. 2020 [31] | Guizhou | 30 | 30 | - | - | - | - | interns | 12 | FCM | LBL | ①② |
| Wang et al. 2021 [32] | Neimenggu | 15 | 15 | 28.60 ± 1.30 | 28.50 ± 1.40 | 8/7 | 9/6 | residents | 18 | FCM | LBL | ①② |
| Zhu et al. 2022 [33] | Anhui | 21 | 21 | 24.76 ± 0.29 | 24.81 ± 0.31 | 11/17 | 13/18 | residents | 4 | FCM | LBL | ①② |
| Zhao Ting. 2014 [34] | Henan | 30 | 30 | 19.31 ± 1.02 | 19.05 ± 0.97 | 16/14 | 12/18 | interns | 6 | PBL | LBL | ① |
| Cai et al. 2017 [5] | Guizhou | 25 | 25 | 24.30 ± 2.70 | 24.20 ± 1.20 | 5/20 | 3/22 | residents | - | PBL | LBL | ①② |
| Liu et al. 2017 [35] | Anhui | 30 | 30 | 22.20 ± 1.51 | 22.90 ± 1.65 | 12/18 | 16/14 | interns | 10 | PBL | LBL | ①② |
| Li et al. 2017 [36] | Xinjiang | 40 | 40 | - | - | - | - | interns | 12 | PBL | LBL | ①② |
| Long et al. 2018 [6] | Ningxia | 26 | 26 | 22.63 ± 1.03 | 22.94 ± 1.05 | 11/15 | 10/16 | interns | 9 | PBL | LBL | ①② |
| Zhang et al. 2018 [37] | Liaoning | 21 | 21 | 21.90 ± 1.20 | 22.50 ± 1.60 | 7/14 | 6/15 | interns | 18 | PBL | LBL | ①② |
| Zhao et al. 2018 [38] | Neimenggu | 50 | 50 | - | - | - | - | interns | 33 | PBL | LBL | ①② |
| Ma et al. 2019 [39] | Fujian | 23 | 23 | 23.38 ± 1.06 | 23.25 ± 1.03 | 8/15 | 9/14 | interns | 33 | PBL | LBL | ①② |
| Hu et al. 2019 [40] | Anhui | 30 | 30 | 21.2 ± 0.41 | 21.27 ± 0.45 | 16/14 | 15/15 | interns | 10 | PBL | LBL | ①② |
| Rong et al. 2021 [41] | Anhui | 20 | 20 | 25.46 ± 1.04 | 25.42 ± 1.02 | 5/15 | 6/14 | interns | 12 | PBL | LBL | ①② |
| Lei et al. 2016 [42] | Xinjiang | 47 | 46 | 21.4 | 21.3 | 25/22 | 24/22 | interns | 6 | TBL | LBL | ① |
| Yin et al. 2019 [43] | Neimenggu | 15 | 15 | - | - | - | - | residents | 13 | TBL | LBL | ② |
| Fan et al. 2020 [44] | Shanxi | 33 | 33 | 22.27 ± 0.81 | 22.47 ± 0.76 | 14/19 | 15/18 | interns | 10 | TBL | LBL | ①② |
| Zhang et al. 2022 [45] | Liaoning | 100 | 100 | 23.76 ± 0.88 | 23.72 ± 0.89 | 56/44 | 57/43 | interns | 5 | TBL | LBL | ①② |
Age is described as the mean ± standard deviation. F, female; M, male; T, test group; C, control group. PBL, problem-based learning; CBL, case-based learning; EBM, evidence-based medicine; FCM, flipped classroom model; TBL, team-based learning; CP, clinical pathway; LBL, lecture-based learning. ① the theoretical exam scores; ② the practical skill scores
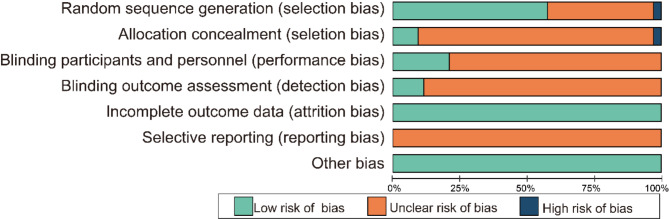
Risk assessment
The risk assessment of the included literature is shown in Fig. 2. A detailed ratings for each study is at Supplementary Table S2. Among the included articles, 17 studies employed the random number table method, 1 study utilized the random drawing method, and an additional study employed the odd-even month random method.
Fig. 2.
Risk of bias graph of the included RCTs. The vertical axis represents the risk of bias items, and the horizontal axis represents the percentage of the number of RCTs
Network meta-analysis result
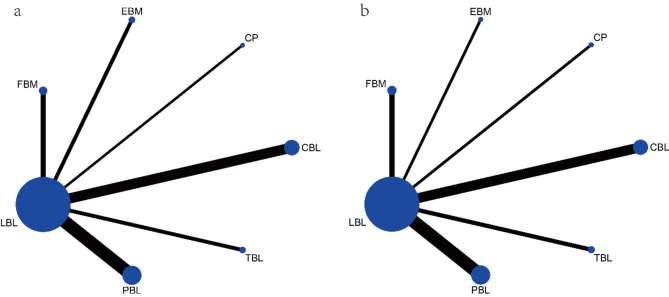
The evidence network of outcome indicators is presented in Fig. 3. The results indicate that theoretical exams and practical skill scores involve 30 and 27 direct comparisons, respectively, all of which are two-arm trials and have not formed a closed loop.
Fig. 3.
Network diagrams for different outcomes. (a) the theoretical exam scores; (b) the practical skill scores. The blue dots represent the different teaching methods, the larger the blue dot the larger the sample size. The line between the blue dots represents literature with direct comparisons, the thicker the line the larger the sample size containing direct comparisons
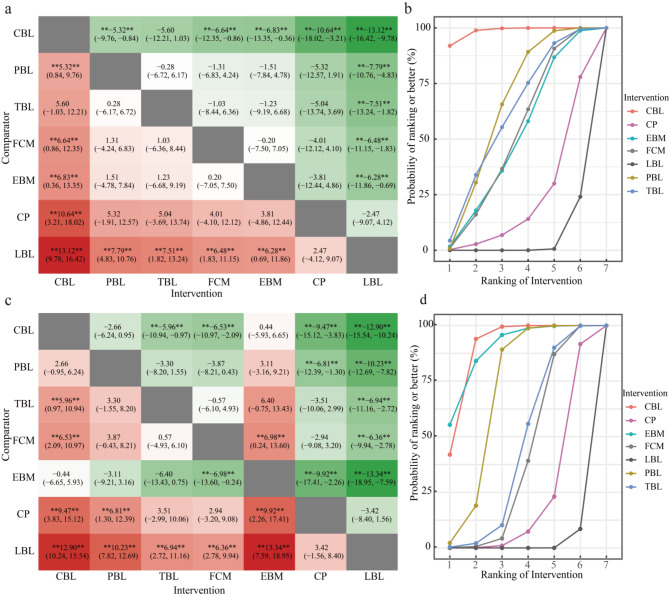
Compared to the LBL teaching method, various alternative teaching methods, including CBL, PBL, TBL, FCM, and EBM, exhibit a significant enhancement in theoretical exam scores. Notably, CBL demonstrated the most substantial impact [MD = 13.12, 95% CI (9.78,16.42), P < 0.001], followed by the PBL teaching method [MD = 7.79, 95% CI (4.83,10.76), P < 0.01], TBL teaching method [MD = 7.51, 95% CI (1.82,13.24), P < 0.001], FCM teaching method [MD = 6.48, 95% CI (1.83,11.15), P < 0.001], and EBM teaching method [MD = 6.28, 95% CI (0.69,11.86), P < 0.001]. In comparison to PBL, FCM, EBM, and CP teaching methods, the CBL teaching method emerges as significantly more effective in improving theoretical exam scores. Notably, the impact was most pronounced when compared to the CP teaching method [MD = 10.64, 95% CI (3.21,18.02), P < 0.001], followed by the EBM teaching method [MD = 6.83, 95% CI (0.36,13.35), P < 0.001], FCM teaching method [MD = 6.64, 95% CI (0.86,12.35), P < 0.001], and PBL teaching method [MD = 5.32, 95% CI (0.84,9.76), P < 0.001]. Figure 4 (a) illustrates the results of the network meta-analysis, showcasing the comparative effectiveness of different teaching methods. The ranking evaluation, detailed in Table 2; Fig. 4 (b), places the teaching methods in the following order: CBL > PBL > TBL > FCM > EBM > CP > LBL.
Fig. 4.
Mean difference (95% credible interval) and surface under the cumulative ranking curve (SUCRA) plots for different outcomes. a and b represent theoretical exam scores, while b and d represent practical skill scores. “**” in Fig. 4 (a, c) indicates statistical significance (P < 0.05). The vertical axis in Fig. 4 (b, d) represents cumulative probabilities, and the horizontal axis represents rank
Table 2.
Ranking evaluation for different outcomes based on different teaching methods
| Teaching methods | SUCRA of the theoretical exam score (%) | Probability of the best teaching methods of the theoretical exam score (%) | SUCRA of the practical skill score (%) | Probability of the best teaching methods of the practical skill score (%) |
|---|---|---|---|---|
| CBL | 98.4 | 91.9 | 89.2 | 42.0 |
| PBL | 64.1 | 0.7 | 68.2 | 2.2 |
| TBL | 60.3 | 4.4 | 43.1 | 0.4 |
| FCM | 51.2 | 1.0 | 38.5 | 0.1 |
| EBM | 49.8 | 1.7 | 89.0 | 55.4 |
| CP | 22.0 | 0.3 | 20.6 | 0.0 |
| LBL | 4.1 | 0.0 | 1.4 | 0.0 |
Compared to the LBL teaching method, various alternative teaching methods, including CBL, PBL, TBL, FCM, and EBM, also display a significant enhancement in theoretical exam scores. In particular, EBM demonstrated the most notable effect [MD = 13.34, 95% CI (7.59,18.95), P < 0.001], followed by the CBL teaching method [MD = 12.90, 95% CI (10.24,15.54), P < 0.01], PBL teaching method [MD = 10.23, 95% CI (7.82,12.69), P < 0.001], TBL teaching method [MD = 6.94, 95% CI (2.72,11.16), P < 0.001], and FCM teaching method [MD = 6.36, 95% CI (2.78,9.94), P < 0.001]. In comparison to the TBL teaching method, the CBL teaching method significantly enhances practical skill scores [MD = 5.96, 95% CI (0.97,10.94), P < 0.001]. When compared to the FCM teaching method, the EBM teaching method had the most noticeable effect on improving teaching performance skills [MD = 6.98, 95% CI (0.24,13.60), P < 0.001], followed by the CBL teaching method [MD = 6.53, 95% CI (2.09,10.97), P < 0.001]. Compared to the CP teaching method, the EBM teaching method had the most noticeable effect on enhancing teaching performance skills [MD = 9.92, 95% CI (2.26,17.41), P < 0.001], followed by the CBL teaching method [MD = 9.47, 95% CI (3.83,15.12), P < 0.001] and then the PBL teaching method [MD = 6.81, 95% CI (1.30,12.39), P < 0.001]. Figure 4 (c) presents the results of the network meta-analysis, offering a comparative perspective on the effectiveness of different teaching methods. The ranking evaluation, detailed in Table 2; Fig. 4 (d), positions the teaching methods as follows: CBL > EBM > PBL > TBL > FCM > CP > LBL.
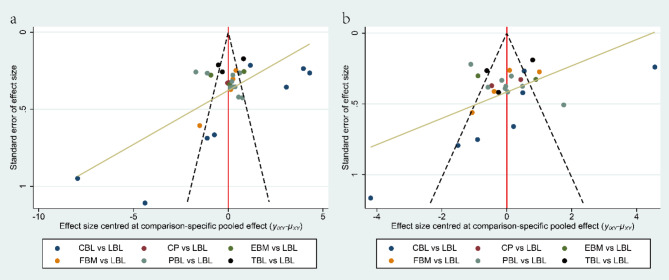
Publication bias
The results of Begg’ tests suggested no publication bias in the included studies. The comparison-adjusted funnel plots for each outcome were shown in Fig. 5. The points in the funnel chart were asymmetric based on the position of the centerline, and the scatter was found to be symmetrical along the null line to the left and right, indicating that there was no small sample effect and publication bias in theoretical exam scores (Fig. 5 (a), P = 0.060), and practical skill scores (Fig. 5 (b), P = 0.348).
Fig. 5.
Funnel plots for different outcomes. (a) the theoretical exam scores; (b) the practical skill scores
Discussion
Summary of main findings
This NMA collected all available evidence from 31 RCTs on the effectiveness of various teaching methods in the clinical teaching in Chinese neurology, involving 2,124 students and 7 teaching methods. Among them, 7 teaching methods include CBL, PBL, TBL, FCM, EBM, CP, and LBL. In terms of clinical teaching efficacy, CBL is the most effective neurology teaching methods in improving theoretical exam and practical skill performance. Our findings indicate that the ranking of theoretical assessment scores from best to worst is CBL > PBL > TBL > FCM > EBM > CP > LBL (Fig. 4 (b), Table 2), while the ranking of practical skill assessment scores is CBL > EBM > PBL > TBL > FCM > CP > LBL (Fig. 4 (d), Table 2). Although the ranking varies slightly among outcome measurements, the results based on currently available data show that the ranking results of various teaching methods for different outcomes are almost consistent. For example, the PBL teaching method ranks second in improving theoretical exam scores and third in practical skill exam scores when we focus on the experimental score. In this study, there is no evidence of publication bias. In addition, as shown in Fig. 2, there are no closed loops in the theoretical exam and practical skill scores. Hence, we did not employ a node-splitting analysis to evaluate the inconsistency of the model.
Scientific significance
CBL is the optimal strategy when we use theoretical or practical test scores to measure the effect of neurology education. Many studies [46, 47] show that an integrated CBL teaching method may increase the competencies of medical students. This might be explained by the fact that CBL focuses on specific cases with predetermined learning objectives, often providing more guidance from teachers and serving as a targeted complement to traditional teaching methods within a curriculum [48]. In addition, bringing a clinical element into neurology teaching could promote easy comprehension [4, 20]. Hence, CBL enhances the students’ ability to analyze and learn the application of neurology knowledge and can reflect on the educational experience gained through these cases. However, it has been found that students who learn CBL in conjunction with other teaching methods, such as CBL & PBL, have higher theoretical and practical scores than those learning with CBL alone [49]. This suggests that instructors and medical education institutions should exercise caution in designing courses and selecting a single teaching method, taking into account disciplinary characteristics, student demographics, and other factors to ensure optimal teaching effectiveness.
Interestingly, the result of SUCRA probability (Fig. 4 (b, d), Table 2) shows that the PBL method performed well in the reported outcome indicators. Students benefit from the implementation of PBL since PBL promotes active, real-world, and collaborative learning, emphasizing problem-solving skills among students and encouraging them to solve problems together [50]. As a result, students who may struggle with specific problems have better performance with the help of teachers and are more satisfied with PBL. In addition, Zgheib et al. reported that PBL involves open-ended, self-directed exploration of broader issues, indicating that PBL can foster students’ independent learning [51].
EBM teaching method is also a good education strategy in improving students’ practical test scores (Fig. 4 (c, d), Table 2). EBM serves as a bridge between theoretical learning and practical application, ensuring that students are well prepared to address complex challenges in the field of neurology [52]. In addition, this process cultivates proficiency in navigating the vast landscape of literature in neurology and thus nurtures the ability to make informed and evidence-based decisions [52]. Students learn the latest advancements and research outcomes in neurology by engaging in EBM so that they can apply them in practice. Finally, this procession empowers them to apply evidence-based principles to clinical scenarios effectively and enhances their practical skills. However, in terms of theoretical exam results, the SUCRA probabilities of EBM were less than 50%, indicating that the performance of EBM in improving students’ experimental test scores is worth further study.
Innovations and limitations
In recent years, an increasing number of clinical neurology teachers have recognized the limitations of traditional teaching methods and have experimented with advanced teaching approaches from both domestic and international arenas [46]. However, current RCTs on diverse teaching methods face limitations such as complex teaching models and a restricted sample size. In addition, the effectiveness of different teaching strategies has not been compared in neurology education. To address these gaps, this study innovatively adopts a Bayesian NMA method to evaluate various teaching methods in China [7]. To our knowledge, this NMA is the first comprehensive data analysis assessing the effects of different neurology education strategies.
Several limitations need to be taken into consideration. The study does not include research on hybrid and other personalized teaching methods in neurology, such as the integration of Case-Based Learning (CBL) and Problem-Based Learning (PBL). This exclusion may contribute to a somewhat limited perspective on the spectrum of clinical teaching models. In addition, the predominance of positive results in the literature (with only 2 studies [39, 40] presenting negative results), along with the tendency to favor such outcomes, raises questions about the evidence’s quality and the risk of exaggerated findings. Additionally, the different baseline conditions of students, diverse test-design frameworks [54] and the difference in teachers’ levels across all the included studies might contribute to the heterogeneity to some extent. Furthermore, the study does not report analyses of heterogeneity or inconsistency, which are crucial in NMA to assess the degree of variation and potential contradictions across studies. While heterogeneity analysis is well-established in traditional meta-analysis, its application in NMA is more complex, and there is currently no robust statistical framework to effectively evaluate heterogeneity in this context. The studies included in this review only present direct comparisons, with no indirect comparisons or loop formations, thus precluding consistency analysis. Future research should include heterogeneity or inconsistency analyses, such as I² statistics or node-splitting tests, to enhance the credibility of the findings and better assess the comparability of the included studies. Finally, different countries and regions have different educational backgrounds, teaching methods and assessments. We restrict our study to interns/residents within the Chinese educational context. The inclusion of studies published in both English and Chinese introduces potential language-related nuances that may have influenced the interpretation of findings. Differences in terminology, cultural context, and regional variations in clinical practice could have affected the way results were reported and interpreted in the included studies. While every effort was made to account for these variations, the language differences should be considered as a limitation when interpreting the findings. The main aim of our meta-analysis was to comprehensively review and synthesize teaching strategies implemented in the Chinese educational system. Therefore, the generalizability of our findings may be somewhat limited. Our results are constrained by the distinctive cultural, institutional, and pedagogical features inherent in China’s educational system.
Conclusions
Overall, this NMA provides a comprehensive and integrated evaluation and summary of the effects of different neurology teaching methods. The current evidence indicates that modern teaching methods, particularly CBL, are more effective in improving the theoretical examinations and practical skills of neurology clinicians. The superior performance of teaching methods should be integrated more prominently in their medical training programs, ensuring that clinicians are equipped with the necessary knowledge and skills to excel in their practice. Future research could focus on exploring the economic and satisfactory impacts of these teaching methods. It is meaningful for neurology pedagogues to consider and promote these teaching strategies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- PBL
Problem-based learning
- FCM
Flipped classroom model
- EBM
Evidence-based medicine
- CP
Clinical practice
- CBL
Case-based learning
- LBL
Lecture-based learning
- TBL
Team-based learning
Author contributions
X.H. and J.S. contributed to the conception of the study. X.L. and J.Z. collected and analyzed the data. X.L. and Y.L. drafted the manuscript. X.H., W.S. and M.L. contributed to the revision of the manuscript. All authors commented on previous versions. All authors read and approved the final manuscript.
Funding
This work is granted by Key Technologies Research and Development Program (2018YFC1705001), Central University Basic Research Fund of China (2022-JYB-XJSJJ-093), Wu Jieping Medical Foundation (320.6750.2022-25-13) and Beijing Tongzhou district Science and Technology Program (KJ2023CX064).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jiacheng Zhang, Email: 13426324787@163.com.
Xing Huang, Email: huangxing52071@163.com.
References
- 1.Sandrone S, Albert DVF, Dunham SR, et al. Training in neurology: how lessons learned on teaching, well-being, and telemedicine during the covid-19 pandemic can shape the future of neurology education. Neurology. 2021;96(24):E3007–10. 10.1212/wnl.0000000000012010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarron MO, Stevenson M, Loftus AM, et al. Neurophobia among general practice trainees: the evidence, perceived causes and solutions. Clin Neurol Neurosurg. 2014;122:124–8. 10.1016/j.clineuro.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Togher Z, Fullam S, Callanan I, et al. An evaluation of optimal tutorial methodologies for neurology teaching at undergraduate level optimal tutorial methods for neurology. Ir J Med Sci. 2021;190(3):965–9. 10.1007/s11845-020-02411-3. [DOI] [PubMed] [Google Scholar]
- 4.Ma JH. Analysis of the effectiveness of CBL teaching method in neurology traineeships. Psychol Doct. 2018;24(16):327–8. [Google Scholar]
- 5.Cai J, Shao Y, Zhang DL, et al. Analysis of the effect of PBL implementation in the teaching of 50 neurology clinical trainees. Electr J Clin Med Lit. 2017;4(55):10844–5. 10.16281/j.cnki.jocml.2017.55.123. [Google Scholar]
- 6.Long AY, Dong J. The use of PBL teaching methods in teaching neurology. Health Gu. 2018;41351. 10.3969/j.issn.1006-6845.2018.41.339.
- 7.Hinne M, Gronau QF, van den Bergh D, et al. A conceptual introduction to bayesian model averaging. Adv Methods Pract Psych Sci. 2020;3(2):200–15. 10.1177/2515245919898657. [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cumpston M, Li TJ, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Db Syst Rev. 2019;102Ed000142. 10.1002/14651858.Ed000142. [DOI] [PMC free article] [PubMed]
- 10.Thomas G. After the gold rush: questioning the gold standard and reappraising the status of experiment and randomized controlled trials in education. Harv Educ Rev. 2016;86(3):390–411. 10.17763/1943-5045-86.3.390. [Google Scholar]
- 11.Tolsgaard MG, Ku C, Woods NN, et al. Quality of randomised controlled trials in medical education reported between 2012 and 2013: a systematic review protocol. BMJ Open. 2014;4(7):4e005155. 10.1136/bmjopen-2014-005155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parks T. Randomized controlled trials in medical education. J R Soc Med. 2009;102(6):214–214. 10.1258/jrsm.2009.090099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Béliveau A, Boyne DJ, Slater J, et al. Bugsnet: an r package to facilitate the conduct and reporting of bayesian network meta-analyses. Bmc Med Res Methodol. 2019;19(1):196. 10.1186/s12874-019-0829-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutton B, Salanti G, Caldwell DM, et al. The prisma extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Intern Med. 2015;162(11):777–84. 10.7326/m14-2385. [DOI] [PubMed] [Google Scholar]
- 15.Hu D, O’Connor AM, Wang C, et al. How to conduct a bayesian network meta-analysis. Front Vet Sci. 2020;7:271. 10.3389/fvets.2020.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71. 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 18.Xu HQ, Chen SY, Xia NG. Application of a phased teaching method guided by the CBL accountability teaching pathway in neurology clinical teaching. China High Med Educ. 2016(04):104–.
- 19.Zhang N, Han F. Analysis of application of typical case teaching method in the clinical practice teaching in the department of Neurology. China Health Ind. 2018;15(17):158–9. 10.16659/j.cnki.1672-5654.2018.17.158. [Google Scholar]
- 20.Dong LG, Cui GY. The application of CBL teaching mode in the clinical teaching of neurology. Educ Teach Forum. 2018(44):66–7.
- 21.Tang J. Analysis of the effect of CBL teaching method in neurology internship teaching. Electr J Pract Clin Nurs Sci. 2019;4(23):181. [Google Scholar]
- 22.Peng Y. Analysis of the value of applying CBL teaching model in clinical teaching of Neurology. China Health Ind. 2021;18(30):129–32. 10.16659/j.cnki.1672-5654.2021.30.129. [Google Scholar]
- 23.Li XW. On the clinical application of case teaching mode in clinical teaching of neurology. Fash Bab. 2021;22(22):69–70. [Google Scholar]
- 24.Yang YL, Wang Y, Tang Q, et al. A study of teaching method in the standardised training of neurology residents. J Mod Med Health. 2022;38(09):1591–3. [Google Scholar]
- 25.Zhou KG, Zhao YC, Wang LL et al. Evaluation of the effect of clinical pathway teaching method in clinical teaching of Neurology. China High Med Educ. 2019(06):79–80.
- 26.Hou L, Mo ZL, Zhang H, et al. Experiences of teaching clinical pathways to neurologists in neurology training under a core competency orientation. Doct. 2022;7(3):132–4. [Google Scholar]
- 27.Li QF, Zhu Y, Wang SR, et al. Application of evidence-based medicine in the teaching of clinical practice of Neurology. Hainan Med J. 2012;23(04):136–8. [Google Scholar]
- 28.Jiang T, Zhou JS. The application of evidence-based medicine training mode in the standardized training for neurology residents and its effect evaluation. J Jiangsu Inst Commer. 2017;0255–7. 10.16335/j.cnki.issn1672-2604.2017.02.016.
- 29.Jiang RY. Evidence-based medicine in teaching neurology clerkships. Health Gu. 2020(18):62.
- 30.Zhang CC, Liu HY, Xu J. Application of flipped classroom based on we chat platform in teaching of neurological examination. China Contin Med Educ. 2019;11(30):10–2. [Google Scholar]
- 31.Chen Y, Xu ZC, Liao SS, et al. Application of flipping classroom based on micro-lecture in clinical practice teaching of Neurology. China Health Ind. 2020;17(13):158–60. 10.16659/j.cnki.1672-5654.2020.13.158. [Google Scholar]
- 32.Wang SB, Zeng QX. Observation on the effect of flipped classroom blended teaching mode applied to the standardized training of neurology residents. Encycloped Form. 2021;233787. 10.12253/j.issn.2096-3661.2021.23.2597.
- 33.Zhu FF, Shou GL, Xu YY, et al. Application of translational medicine combined with wechat flipped classroom teaching mode in neurology training teaching. China Contin Med Educ. 2022;14(13):140–4. [Google Scholar]
- 34.Zhao T. Analysis of the effect of PBL teaching method applied in neurology trainee teaching. Henan Med Res. 2014;23(10):150–2. [Google Scholar]
- 35.Liu XL, Chen YH, Xie J, et al. The application of PBL teaching mode in clinical practice teaching in department of Neurology. Chin J Gen Pract. 2017;15(10):1776–8. 10.16766/j.cnki.issn.1674-4152.2017.10.040. [Google Scholar]
- 36.Li GH, Xu JF, Zhang XN. Analyzing the effect of PBL teaching method in clinical teaching in neurology department. Diet Health. 2017;4(8):262. 10.3969/j.issn.2095-8439.2017.08.328. [Google Scholar]
- 37.Zhang XH. Analysis of the implementation method and effect of PBL in clinical teaching in neurology department. China Health Ind. 2018;15(21):119–20. 10.16659/j.cnki.1672-5654.2018.21.119. [Google Scholar]
- 38.Zhao XJ, Zheng XM, Bao H. Exploring the teaching effect of PBL in neurology internship teaching. World Lat Med Inf. 2018;18(90):294–5. 10.19613/j.cnki.1671-3141.2018.90.236. [Google Scholar]
- 39.Ma HZ, Wang JZ, Shi ZF, et al. A comparative study of PBL teaching model and traditional teaching model in neurology clinical internship teaching. Med Forum. 2019;23(23):3373–4. 10.19435/j.1672-1721.2019.023.079. [Google Scholar]
- 40.Hu J, Yang Q. Application and exploration of PBL teaching model in clinical teaching of standardized training for residents in Neurology. Contin Med Educ. 2019;33(05):36–8. [Google Scholar]
- 41.Rong YT. Analysis of the methods and effectiveness of implementing PBL in clinical teaching in neurology department. Fash Bab. 2021;22(6):77–8. 10.3969/j.issn.1671-5217.2021.06.074. [Google Scholar]
- 42.Lei J, Zhao XF, Ma JH. Control study on TBL teaching in undergraduate course in the probation neurology teaching. China Contin Med Educ. 2016;8(03):23–4. [Google Scholar]
- 43.Yin XH. A study on the application of team-based learning strategies in the teaching of intravenous thrombolysis in hyperacute cerebral infarction for physicians in standardised neurology residency training. Cardiovas Dis Electr J Int Trad Chin West Med. 2019;7(18):69. 10.16282/j.cnki.cn11-9336/r.2019.18.053. [Google Scholar]
- 44.Fan QY, Liu JJ, Wang HQ, et al. An investigation of the application of team-based learning joint error correction teaching method in the teaching of lumbar puncture surgery. Health Vocat Educ. 2020;38(20):143–5. [Google Scholar]
- 45.Zhang Y. Application of TBL teaching method in neurology teaching. J Shenyang Med Coll. 2022;24(05):557–60. 10.16753/j.cnki.1008-2344.2022.05.023. [Google Scholar]
- 46.Fu XT, Hu Y, Yan BC, et al. The use of blended teaching in higher medical education during the pandemic era. Int J Clin Pract. 2022;2022:3882975. 10.1155/2022/3882975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang W, Li H, Su A, et al. Application of problem based learning (pbl) and case based learning (cbl) in the teaching of international classification of diseases encoding. Sci Rep-Uk. 2023;13(1):15220. 10.1038/s41598-023-42175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao W, He L, Deng W, et al. The effectiveness of the combined problem-based learning (pbl) and case-based learning (cbl) teaching method in the clinical practical teaching of thyroid disease. BMC Med Educ. 2020;20(1):381. 10.1186/s12909-020-02306-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sangam MR, K P. Efficacy of case-based learning in anatomy. Cureus. 2021;13(12):e20472. 10.7759/cureus.20472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shen J, Yuan L, Ge R, et al. Improving medical student recruitment into neurosurgery through teaching reform. BMC Med Educ. 2022;22(1):656. 10.1186/s12909-022-03722-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim YJ. The pbl teaching method in neurology education in the traditional Chinese medicine undergraduate students: an observational study. Medicine. 2023;102(39):e35143. 10.1097/md.0000000000035143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brown G. Proposing problem-based learning for teaching future forensic speech scientists. Sci Justice: J Foren Sci Soc. 2022;62(6):669–75. 10.1016/j.scijus.2022.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Ilic D, Forbes K. Undergraduate medical student perceptions and use of evidence based medicine: a qualitative study. BMC Med Educ. 2010;10:58. 10.1186/1472-6920-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Horak H, Englander R, Barratt D, et al. Entrustable professional activities: a useful concept for neurology education. Neurology. 2018;90(7):326–32. 10.1212/wnl.0000000000004947. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.