Abstract
Retrospective molecular epidemiology was performed on samples from four sooty mangabey (SM) colonies in the United States to characterize simian immunodeficiency virus SIVsm diversity in SMs and to trace virus circulation among different primate centers (PCs) over the past 30 years. The following SIVsm sequences were collected from different monkeys: 55 SIVsm isolates from the Tulane PC sampled between 1984 and 2004, 10 SIVsm isolates from the Yerkes PC sampled in 2002, 7 SIVsm isolates from the New Iberia PC sampled between 1979 and 1986, and 8 SIVsm isolates from the California PC sampled between 1975 and 1977. PCR and sequencing were done to characterize the gag, pol, and env gp36 genes. Phylogenetic analyses were correlated with the epidemiological data. Our analysis identified nine different divergent phylogenetic lineages that cocirculated in these four SM colonies in the Unites States in the past 30 years. Lineages 1 to 5 have been identified previously. Two of the newly identified SIVsm lineages found in SMs are ancestral to SIVmac251/SIVmac239/SIVmne and SIVstm. We further identified the origin of these two macaque viruses in SMs from the California National Primate Research Center. The diversity of SIVsm isolates in PCs in the United States mirrors that of human immunodeficiency virus type 1 (HIV-1) group M subtypes and offers a model for the molecular epidemiology of HIV and a new approach to vaccine testing. The cocirculation of divergent SIVsm strains in PCs resulted in founder effects, superinfections, and recombinations. This large array of SIVsm strains showing the same magnitude of diversity as HIV-1 group M subtypes should be extremely useful for modeling the efficacy of vaccination strategies under the real-world conditions of HIV-1 diversity. The genetic variability of SIVsm strains among PCs may influence the diagnosis and monitoring of SIVsm infection and, consequently, may bias the results of pathogenesis studies.
Simian immunodeficiency viruses (SIVs) are a divergent group of highly adapted viruses which may be grouped into eight phylogenetic lineages (5, 9, 16, 18). Malleability is one of the hallmarks of lentiviruses, and their diversity is the result of long-term coevolution with their respective hosts, cross-species transmission, preferential host switching, and recombination (5, 6, 10, 13, 30, 34, 69). The high prevalence of divergent SIVs in their natural hosts (3, 41, 60, 69) and the rapid spread of human immunodeficiency viruses (HIVs) in humans have generated a huge pool of genomic sequences with a high propensity for further diversification (62). Within their hosts, lentiviruses evolve due to robust and continuous replication (12, 31, 37, 40, 56, 57, 67, 71, 75) during long disease-free periods (35, 58). Mutations also occur frequently during lentiviral replication due to the error-prone reverse transcriptase (49, 64, 65).
SIVsm naturally infects sooty mangabeys (SMs) (Cercocebus atys) and is genetically close to HIV type 2 (HIV-2) and SIVmac (15, 25, 39, 50). Phylogenetic analyses and geographic concordance support the idea that multiple cross-species transmission events from SMs to humans gave rise to all eight known HIV-2 groups (14, 22, 28, 77). An accidental or experimental cross-species transmission of SIVsm to macaques was the origin of SIV infection in these Asian nonhuman primate species (29). SIVsm shows a relatively high pathogenic potential in rhesus macaques and humans following cross-species transmission. However, cross-species transmission events have extremely unbalanced epidemiologic consequences: of the eight cross-species transmissions of SIVsm to humans, only two were epidemiologically successful, generating the epidemic groups HIV-2 A and B (21, 28). Groups C to H (14, 22, 28, 77) are epidemiological failures that are weakly pathogenic, replicate poorly in infected humans, and are found only within the range of SMs or in persons who emigrated from West Africa (14, 28). Since groups C to H were each defined based on only one sequence/isolate, they do not meet the nomenclature requirements for a group. Two complete genomes, in conjunction with partial sequences of a third strain, are needed to designate a bona fide HIV-2 group (22). Therefore, it was proposed that groups C to H be considered putative HIV-2 groups (22).
In the wild, SIVsm strains show a high level of genetic divergence (5). Our previous studies reported that the genetic distance between strains originating from the same SM troop may be up to 15 to 25% for the env nucleotide sequences (3, 15). Therefore, since the prevalence in the wild is high and hundreds of SMs have been imported to the United States to establish the current colonies, it is not surprising that transmission in captivity of the founder viruses from SMs naturally infected at the time of their importation generated a high level of SIVsm diversity at U.S. primate centers (46). Furthermore, the cocirculation of highly divergent SIVsm strains in the United States was suggested by the previous isolation of three divergent viruses, i.e., SIVmac/mne, SIVstm, and SIVsmB670/PBj, from different species of macaques (23, 47, 53). Full-length SIVmac/mne sequences form a tight cluster in the HIV-2/SIVsm/SIVmac phylogenetic trees. It was suggested that these viruses may have originated from infected captive SMs at the California National Primate Research Center (CNPRC) (8, 48). SIVstm could also be traced to stump-tailed macaques (STMs) at CNPRC and was postulated to have originated from SIVsm-infected SMs (43, 47). Both of these viruses generated outbreaks of lymphomas and opportunistic infections in the two macaque species (29). However, the SM ancestors of these viruses have not been found. Their identification could allow analyses of the circumstances of selection of highly pathogenic SIVsm-like strains in macaques. A third SIVsm lineage known to circulate in the United States is represented by the SIVsmB670, SIVsmH9, and SIVsm543-3 strains. SIVsmB670 and SIVsmPBj were isolated independently at Tulane National Primate Research Center (TNPRC) and Yerkes National Primate Research Center (YNPRC) in 1986 (25, 53). These viruses were highly virulent in rhesus macaques (7, 24). The sources of these macaque viruses were shown to be SIVsm strains naturally infecting SMs at the two primate centers. Another pathogenic strain included in lineage 1 is SIVsmPBj, which resulted from experimental infections of pig-tailed macaques (Macaca nemestrina) (PTMs) with SIVsm (26, 51).
Here we report a phylogenetic analysis of SIVsm diversity in four primate centers in the United States over the past 30 years. We identified the SMs that harbored the ancestors of SIVmac and SIVstm and have shown that the cocirculation of nine different phylogenetic lineages displaying the same degree of divergence as the HIV-1 group M subtypes resulted in founder effects, recombinations, and superinfections. Therefore, SIVsm circulation in colonies in the United States mirrors the molecular epidemiology of HIV. This array of SIVsm strains naturally infecting SMs may be extremely useful for modeling the efficacy of vaccination in real-world situations. We also evaluated the impact of SIVsm diversity on the diagnosis and monitoring of SIVsm infections. These analyses are necessary for pathogenesis and vaccine studies of SIVsm in its natural host or in an animal model of AIDS, namely, rhesus monkeys infected with SIVsm.
MATERIALS AND METHODS
Animals and specimens.
Over the last 30 years, SMs have been housed in the United States in four colonies at the following primate centers: TNPRC, YNPRC, CNPRC, and the New Iberia Research Center (NIRC). All of these facilities are accredited by the Association for Assessment and Accreditation of Laboratory Animal Care. Housing and handling of the animals were done in accordance with the Guide for the Care and Use of Laboratory Animals (U.S. Public Health Service) and the Animal Welfare Act. All protocols and procedures were reviewed and approved by the institutional animal care and use committees.
Our analysis was done on samples collected over a 30-year period from 84 SMs originating from the four colonies of SMs housed by primate centers in the United States.
The TNPRC SM colony was mostly derived from 64 animals obtained from the YNPRC colony. Ten additional SMs originated from two different sources: four were from NIRC and six came directly from Africa.
EDTA-blood was obtained from the 33 SMs currently living in the TNPRC colony during a biannual health control evaluation. Plasma and peripheral blood mononuclear cells (PBMCs) were separated, placed in individual sterile tubes, and frozen at −80°C until used. Serum samples from 55 dead SMs stored at −70°C were also included.
PBMCs collected in 2002 from 10 SIVsm-infected SMs from YNPRC were also included.
Nine SMs were housed at NIRC during 1977-1986. These SMs had been transferred to NIRC from CNPRC in 1977 (n = 5) or were directly imported from Africa (n = 4). Serum samples from all nine of these SMs collected between 1979 and 1986 were included in this study. The samples were stored at −70°C prior to use.
Eight serum samples from SIVsm-infected SMs at the CNPRC had been collected in 1975 and 1977. The colony of SMs at the CNPRC was established by the direct importation of monkeys from Africa in 1964 (29). Samples from two of the SMs sent to NIRC in 1977 were included in this group (CFU212 and CFU226). These serum samples had been stored at −20°C.
Serology.
All samples originating from TNPRC were screened by a peptide-specific enzyme-linked immunosorbent assay, as described previously (68). This test uses a peptide matching a sequence in the immunodominant epitope of the transmembrane protein gp36 of SIVsm (TAIEKYLKDQAKLNSWGCAFRQVC). This peptide corresponds to a highly conserved epitope and yields broad reactivity. The gp36 peptide was synthesized to a purity of at least 90% (Fisher Scientific). Wells of polyvinyl microtiter plates (Falcon) were coated with 100 μl/well of antigen solution (2 μg/ml) diluted in 0.05 M bicarbonate buffer, pH 9.6, by incubation for 20 h at 37°C. All washes were done with phosphate-buffered saline (PBS) containing 0.5% Tween 20 (PBS-TW). The wells were saturated with PBS containing 2% newborn calf serum (NBCS) by incubation for 45 min at 37°C, followed by washing. Each serum sample was tested at a 1:100 dilution in 0.01 M sodium phosphate buffer, pH 7.4, containing 0.75 M NaCl, 10% NBCS, and 0.5% Tween 20 (PBS-TW-NBCS), with 100 μl being added to the wells and incubated for 30 min at room temperature. The wells were washed four times, and 100 μl of a 1:2,000 dilution of peroxidase-conjugated goat F(ab′)2 anti-human immunoglobulin (Sigma) in PBS-TW-NBCS was added. The plates were incubated for 30 min at room temperature. The wells were washed four times, and the reaction was revealed by incubation with hydrogen peroxide-o-phenylenediamine for 15 min at room temperature. Color development was stopped with 2 N H2SO4, and the absorbance value (optical density) was read at 492 nm. The cutoff was 0.20.
Samples that reacted in the enzyme-linked immunosorbent assay were confirmed by Western blotting (Zeptometrix, Buffalo, N.Y.) according to the manufacturer's instructions. Briefly, SIV strips were hydrated in PBS-TW for 10 min and then incubated with blocking buffer for 1 h at room temperature. Serum or plasma samples (100 μl) were incubated with the strips overnight at 4°C on an orbital shaker. The strips were washed three times with PBS-TW for 5 min each time and then incubated for 1 h at room temperature with 1:1,000 goat anti-rhesus immunoglobulin G conjugated to horseradish peroxidase (Southern Biotechnology, Birmingham, Ala.). Blots exhibiting Env bands alone or in combination with other virus-specific bands were scored as positive, blots with no reactivity were scored as negative, and blots showing Gag reactivities alone were scored as indeterminate.
Nucleic acid extraction.
DNAs were extracted from the PBMCs of SIVsm-infected SMs from TNPRC and YNPRC by the use of QIAamp kits (QIAGEN, Valencia, Calif.). RNAs were extracted from archived samples from dead animals originating from TNPRC, NIRC, and CNPRC. Viral RNAs were extracted from 280 to 560 μl of archived serum samples from TNPRC and NIRC by the use of QIAamp viral RNA extraction kits (QIAGEN, Valencia, Calif.). RNA extraction of the CNPRC samples, which were stored for 30 years at −20°C, was done on the available amount of 200 μl of serum for each sample.
PCR and sequencing.
Nested PCRs were performed to obtain amplified fragments from the gag, env, and pol regions. A 793-bp gag fragment was obtained by a nested PCR protocol using the GagA/GagB and GagC/GagF primers, as described previously (28). Alternatively, primers GF1/GR1 and GF2A/GR3 (15) were used in a nested PCR to generate a 909-bp fragment from the gag region. These two fragments completely overlapped. Nested primers were used for sequencing. A 438-bp fragment of the gp36 env region was obtained by use of a nested PCR protocol with the primers EF4/ER1 and EF5A/ER2A (14). A 602-bp pol integrase fragment was obtained by a slight variation of previously described primers used to amplify divergent SIVs (16, 17, 19, 20). Polis4B (5′-CCA GCH CAY AAA GGW ATA GGW GGA AA-3′) and PolORB (5′-ACT GCH CCT TCH CCT TTC CA-3′) were used for the first round of amplification, and Polis4B was used again in a seminested reaction with Unipol2B (5′-CCC CTA TTC CTC CCY TTC TTT TAA-3′). Since none of the old CNPRC samples were positive in the gag-specific nested PCRs listed above, a shorter LTR-gag fragment was amplified by seminested reverse transcription-PCR (RT-PCR) using the following primers: PBS (5′-TGG GCG CCC GAA CAG GGA C-3′)/gagrev2SM (5′-GCA CCA RAY KAC GCA GAC AGT-3′) as outer primers and PBS/gagrevSM (5′-CTG AAC CTG TYG GMA YTA ATG G-3′). An initial denaturation step for 5 min at 94°C was followed by 35 cycles of 94°C for 30 s, 55°C for 30 s, and 72°C for 30 s, with a final extension for 7 min at 72°C. The nested step conditions were the same, except for the annealing temperature, which was 59°C.
PCR products were purified by use of a QIAquick gel extraction kit or PCR purification kit (QIAGEN, Valencia, Calif.) and sequenced by direct sequencing and dye terminator methodologies (ABI PRISM Big Dye Terminator cycle sequencing ready reaction kit with AmpliTaq FS DNA polymerase [Applied Biosystems, Foster City, Calif.]) in an automated sequencer (ABI 373, stretch model; Applied Biosystems). Sequencing was done by using the inner primers of each reaction.
Phylogenetic analysis.
gag, pol, and env nucleotide sequence alignments were obtained from the Los Alamos National Laboratory HIV Sequence Database (http://hiv-web.lanl.gov). Newly derived SIVsm sequences were aligned by using the CLUSTAL W (72) profile alignment option. The resulting alignments were adjusted manually when necessary. Regions of ambiguous alignment and all gap-containing sites were excluded.
Phylogenetic trees were inferred from the nucleotide sequence alignments by the neighbor-joining method (66), using the HKY85 model of nucleotide substitution (33) implemented in PAUP* (70). The reliability of the branching order was assessed by performing 1,000 bootstrap replicates, again using neighbor joining and the HKY85 model. Phylogenetic trees were also inferred by the maximum likelihood method, using PAUP* with models inferred from the alignment by the use of Modeltest (63). The neighbor-joining tree topology was used as the starting tree for a heuristic search using tree bisection/reconnection branch swapping. Translations of sequences were done for analyses of the immunodominant antibody (Ab) epitope in the small loop of gp36 and of cytotoxic T lymphocyte (CTL) epitopes.
Nucleotide sequence accession numbers.
The nucleotide sequences of the LTR-gag, gag, pol, and env sequences from SIVsm-infected SMs were deposited in GenBank under accession numbers AY965348 to AY965519.
RESULTS
Nine divergent SIVsm lineages cocirculate in different primate centers.
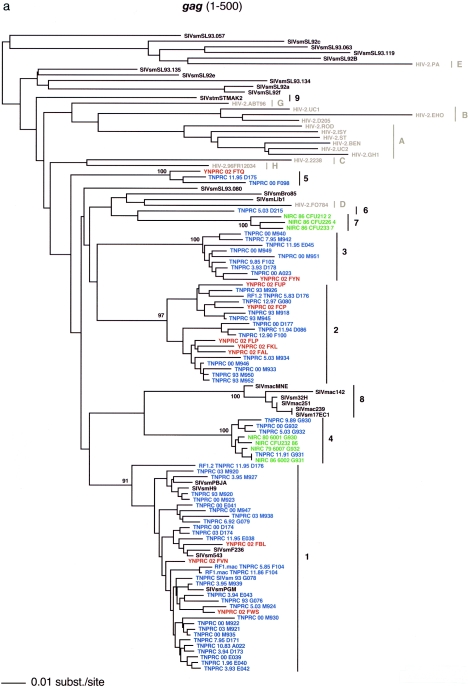
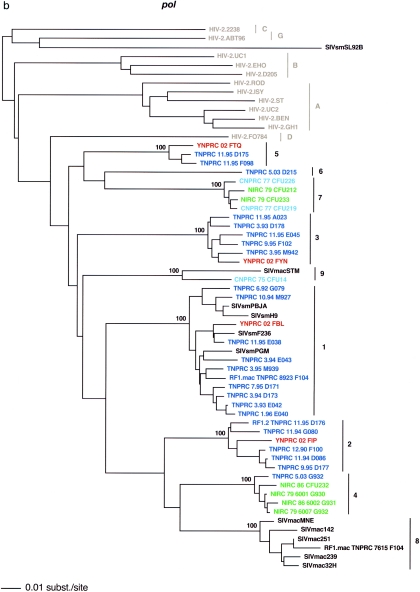
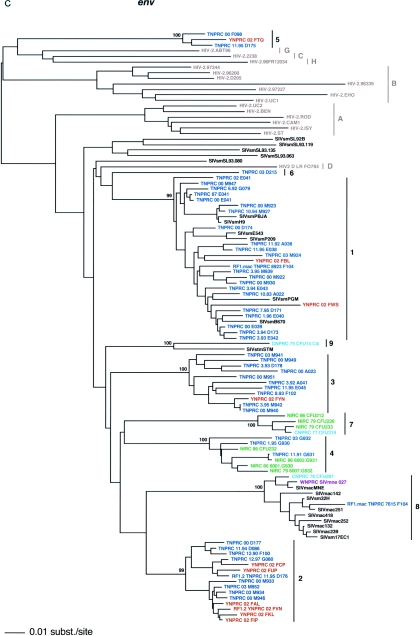
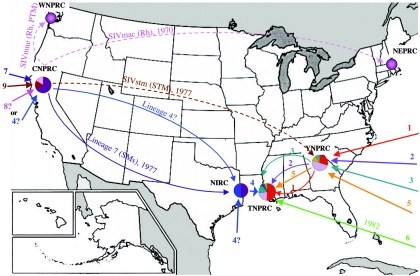
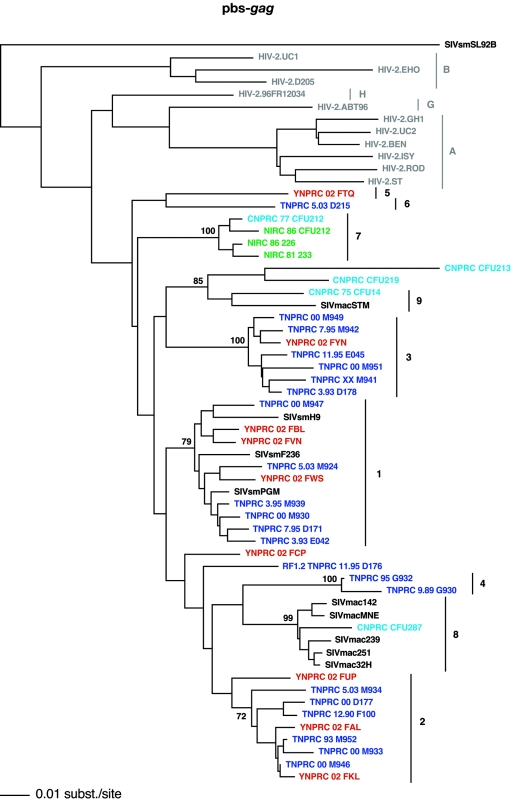
The study of SIVsm diversity in primate centers in the United States was prompted by our recent finding that SIVsm diversity in the TNPRC is much higher than was initially believed (46). In our initial study, by analyzing SIVsm strains infecting 16 of the 27 SIVsm-infected SMs alive in the Tulane colony, we found that five different lineages were cocirculating and that four of them had gone undetected prior to our report (46). Following this earlier study, we systematically investigated SIVsm diversity in the TNPRC colony. In order to place SIVsm diversity at the TNPRC in an epidemiological context, we expanded the study of SIVsm diversity to current and past SM colonies around the United States, covering a 30-year period. Our study revealed that at least nine phylogenetic lineages cocirculated in the SM colonies from the four primate centers during the last 30 years (Table 1; Fig. 1). These distinct phylogenetic clusters were named in the order of their discovery in SMs (lineages 1 through 9). Based on this phylogenetic clustering and existing epidemiological records, the circulation of SIVsm strains between primate centers over the past 30 years was traced, thus establishing molecular epidemiologic correlations between the different colonies of SMs in the United States (Fig. 2).
TABLE 1.
Distribution of different SIVsm lineages in SM colonies from four primate centers in the United States
| Primate center | No. of SIVsm strains characterized for each lineagea
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lineage 1 | Lineage 2 | Lineage 3 | Lineage 4 | Lineage 5 | Lineage 6 | Lineage 7 | Lineage 8 (SIVmac-like) | Lineage 9 (SIVstm-like) | |
| TNPRC | 28 | 12 | 9 | 3 | 2 | 1 | |||
| YNPRC | 3 | 5 | 1 | 1 | |||||
| NIRC | 4 | 3 | |||||||
| CNPRC | 4 | 1 | 1 | ||||||
Lineages 2 to 9 are newly discovered by our group. Lineages were established based on gag clustering patterns. For some strains, the clustering patterns are different between gag and env trees, pointing to a recombinant nature.
FIG. 1.
SIVsm diversity in SM colonies from four primate centers in the United States. Lineages are clusters of SIVs that are highly related and branch together. Newly characterized strains are color coded (blue, TNPRC; red, YNPRC; green, NIRC; pink, CNPRC). Lineage 1 contains the previously reported strains SIVsmB670, SIVsmPBj, SIVsm236/660/543-3, and SIVsmPGM (http://hiv-web.lanl.gov). Reference SIVsm strains and strains from wild-caught SMs are shown in black, whereas HIV-2 strains are shown in light gray. Lineages 8 and 9 include strains isolated from different species of macaques that were experimentally or accidentally infected. The trees are based on gag (500 bp) (a), pol (592 bp) (b), and env (405 bp) (c) fragments after gap-containing sites were removed. The phylogenetic trees were estimated by the neighbor-joining method using amino acid sequences. The reliability was estimated from 1,000 bootstrap replicates; only bootstrap values relevant for lineage definition are shown. Bars, number of amino acid replacements (0.01) per site. The strain nomenclature includes the assigned lineage, the primate center of origin, the year of strain collection, and the monkey identification number.
FIG. 2.
Molecular epidemiology of SIVsm lineages in different primate centers in the United States. The lineage prevalence in each SM colony was estimated based on the present results. Not all of the animals at YNPRC and CNPRC were tested. Therefore, additional SIVsm lineages may be present and the relative prevalence of SIVsm lineages may be different from that established based on limited sampling. Due to the close relationship in gag between lineage 4 strains and SIVmac (lineage 8), it is possible that lineage 4 or its ancestors circulated at CNPRC. However, based on the current data, there is no proof of its presence at CNPRC. Therefore, the alternative hypothesis that lineage 4 was imported directly from Africa to the NIRC cannot be ruled out. Transfers of SIV-infected animals from CNPRC to other primate centers are shown.
All strains from living and dead SMs in the TNPRC colony have been characterized. Serological screening confirmed SIVsm infection in 27 of 33 live SMs and 38 of 63 dead SMs. PCRs were performed in all of these cases, using PBMCs and serum samples collected between 1983 and 2003. Sequence analysis was performed on SIV strains from 58 of the 65 SIVsm-infected SMs at the TNPRC colony between 1980 and 2004. For the remaining SMs, serum samples were either insufficient for analysis or stored under poor conditions, and the PCRs were negative. The SMs in the Tulane colony were infected with six different lineages (lineages 1 to 6) (Table 1; Fig. 1a to c). Tulane SMs originating from the Yerkes colony were infected with lineages 1 to 3 and 5, whereas SMs originating from the New Iberia colony were infected with lineage 4. An SM in the Tulane colony originating from Africa (D215) was infected with a SIVsm strain that formed a distinct lineage 6.
Since most of the TNPRC SM colony originated from YNPRC and NIRC, SIVsm diversity in SMs was first investigated for these two centers. Samples from 10 SMs from YNPRC and 7 SIV-infected SMs from NIRC were sequenced in gag, pol, and env.
Sequencing of the SIVsm samples from the Yerkes colony confirmed the presence of lineages 1, 2, 3, and 5 (Table 1; Fig. 1a to c) in the group of 10 samples analyzed. Although the presence of lineage 1 strains was previously reported for YNPRC (27), the present investigation documents for the first time a high degree of SIVsm diversity in the Yerkes SM colony. Also, the study of SIVsm diversity in the YNPRC SM colony confirmed that lineages 1 to 3 and 5 from TNPRC originated from YNPRC (Fig. 2).
The testing of samples from New Iberia SMs identified the cocirculation of two different lineages (4 and 7) at NIRC (Table 1; Fig. 1a to c): lineage 4 viruses were detected in four monkeys, three of which were transferred to TNPRC (thus confirming the NIRC origin of this lineage, which was first identified from TNPRC) and one of which originated from CNPRC (CFU232). With the exception of the SM originating from CNPRC, all of the remaining SMs infected with lineage 4 at NIRC (6001/G930, 6002/G931, and 6007/G932) were imported directly from Africa. Samples from three monkeys from NIRC harbored SIVsm strains belonging to lineage 7 (CFU233, CFU212, and CFU226) (Table 1; Fig. 1a to c). All of these monkeys originated from CNPRC.
The testing of samples from California SMs was less successful. These samples had been stored at −20°C for almost 30 years. Some of these samples yielded discordant results for PCR amplification of different SIVsm genes. These negative PCR results can be explained by the poor storage conditions for long time periods, which may account for RNA degradation. In this context, primers amplifying short conserved fragments in the LTR-gag region were designed and used.
Of the eight CNPRC samples, three had positive RT-PCR results for env, four had positive results for pol, and five had positive results for LTR-gag. Remarkably, the env sequences clustered into three lineages: CFU219 clustered with lineage 7 strains, CFU287 clustered with SIVmne/mac (lineage 8), and CFU14 clustered with SIVstm (lineage 9) (Fig. 1c). The SIVsm pol sequences from CNPRC clustered within lineage 7 (SM#CFU219, SM#CFU213, and SM#CFU226) and with SIVstm (SM#CFU14) (Fig. 1b). None of the CNPRC samples were positive with the gag primers, probably due to the poor condition of the samples. However, with the LTR-gag primers, five of the CNPRC strains were amplified. These strains clustered with lineage 7 (SM#CFU212), SIVmac (SM#CFU287), and SIVstm (SM#CFU14) or independently (SM#CFU213 and SM#CFU219) (Fig. 3). Altogether, for six of the eight sera included in this study, at least one SIVsm sequence was amplified and characterized. Also, phylogenetic analyses showed that the lineage 7 viruses in NIRC originated from CNPRC because they provided evidence of circulation of this lineage at CNPRC before monkeys were ever sent to NIRC (strains 7_CNPRC_77_CFU212 and 7_CNPRC_77_CFU226 in Fig. 1b and 3). Sequencing of the CNPRC strains identified a Californian SM (SM#CFU287) that was infected with the ancestral lineage SIVmac251/239 (Fig. 1c and 3). Another SM (SM#CFU14) was infected with the ancestral lineage SIVstm (Fig. 1b and c and 3), thus confirming the previous hypothesis that the origin of these two viruses in macaques following accidental transmission was the CNPRC (29, 48).
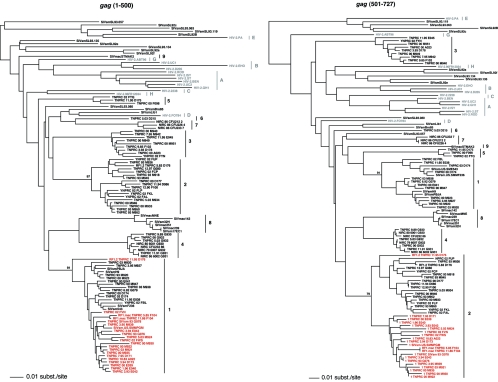
FIG. 3.
Phylogenetic tree of the LTR-gag fragment (450 bp after gap-containing sites were removed). This tree was constructed to include the CNPRC strains. SIVsm strains representative for each lineage were included. See the legend to Fig. 1 for details concerning color codes and the details of tree construction.
Diversity of SIVsm strains in primate centers as a model for HIV-1 group M subtypes.
The nine identified SIVsm lineages are distinct from all previously identified SIVsm strains of African origin. Many of the SIVsm strains characterized so far (45%) cluster together in lineage 1 (reference strains, SIVsmB670 and SIVsmPBj). Lineage 2 to 9 viruses are highly divergent from these prototype viruses. For the env fragment, intralineage nucleotide sequence genetic distances are <6%, whereas interlineage distances are >12.5%, with the largest degree of divergence seen for the viruses of the fifth lineage, which differ from all other strains by 22 to 26% (Table 2). A similar pattern was observed for the gag gene analyses, with a 3 to 5% intralineage genetic distance and a 13 to 18% interlineage nucleotide genetic distance. Table 2 also shows a close phylogenetic relationship in the gag gene between lineage 4 viruses and the SIVmac cluster. The genetic distance between these two lineages is only 8%, which is significantly lower than the gag interlineage distances.
TABLE 2.
gag and env nucleotide genetic distances of SIVsm lineages from SMs in four primate centers in the United States and from wild SMs
| Gene or SIV type | Genetic distance (mean ± SD)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lineage 1 | Lineage 2 | Lineage 3 | Lineage 4 | Lineage 5 | Lineage 6 | Lineage 7 | SIVmac-like | SIVstm | Wild strains | |
| gag | ||||||||||
| Lineage 1 | 4.98 ± 2.01 | |||||||||
| Lineage 2 | 11.44 ± 1.42 | 4.43 ± 1.81 | ||||||||
| Lineage 3 | 14.05 ± 0.83 | 13.89 ± 0.97 | 3.29 ± 1 | |||||||
| Lineage 4 | 11.71 ± 1.04 | 12 ± 0.66 | 14.55 ± 0.64 | 2.08 ± 1 | ||||||
| Lineage 5 | 12.71 ± 0.97 | 13.97 ± 0.98 | 15.75 ± 0.98 | 15.04 ± 0.5 | 2.88 ± 0.29 | |||||
| Lineage 6 | 13.75 ± 0.55 | 14.18 ± 0.89 | 14.33 ± 0.51 | 16.46 ± 0.26 | 16.25 ± 0.66 | NAa | ||||
| Lineage 7 | 14.67 ± 0.73 | 14.22 ± 0.76 | 16.43 ± 0.81 | 14.59 ± 0.39 | 14.81 ± 0.77 | 12.31 ± 0.46 | 2.15 ± 0.49 | |||
| SIVmac-like | 13.97 ± 0.93 | 13.23 ± 0.79 | 16.79 ± 0.96 | 9.03 ± 0.79b | 16.21 ± 0.58 | 16.04 ± 0.59 | 15.51 ± 0.6 | 1.71 ± 0.86 | ||
| SIVstm-like | 15.4 ± 0.48 | 14.31 ± 0.39 | 17.94 ± 0.6 | 17.55 ± 0.43 | 13.67 ± 0.89 | 17.63 | 16.94 ± 0.16 | 18.63 ± 0.41 | NAa | |
| Wild SMs | 19.88 ± 5.09 | 19.41 ± 4.7 | 20.3 ± 5 | 21.11 ± 4.58 | 21.11 ± 4.58 | 19.9 ± 4.92 | 20.75 ± 5.28 | 21.36 ± 4.56 | 20.65 ± 5.05 | 21.15 ± 5.83 |
| env | ||||||||||
| Lineage 1 | 5.5 ± 3.59 | |||||||||
| Lineage 2 | 13.73 ± 1.31 | 3.23 ± 1.4 | ||||||||
| Lineage 3 | 15.11 ± 1.41 | 13.49 ± 1 | 5.21 ± 1.23 | |||||||
| Lineage 4 | 15.2 ± 1.26 | 13.33 ± 1.16 | 13.96 ± 1.27 | 3.82 ± 1.51 | ||||||
| Lineage 5 | 23.22 ± 1.17 | 22.94 ± 0.73 | 23.96 ± 0.96 | 22.54 ± 1.19 | 2.82 ± 0.15 | |||||
| Lineage 6 | 12.58 ± 2.14 | 14.63 ± 0.63 | 15.35 ± 1.23 | 16.71 ± 1.22 | 24.16 ± 0.81 | NAa | ||||
| Lineage 7 | 17.7 ± 1.1 | 13.91 ± 1.01 | 16.09 ± 0.99 | 14.94 ± 1.02 | 23.85 ± 1.33 | 16.77 ± 0.31 | 2.46 ± 1.11 | |||
| SIVmac-like | 17.41 ± 3.01 | 11.94 ± 0.78 | 17.31 ± 1.1 | 16.05 ± 1.46 | 26.44 ± 1.3 | 21.14 ± 0.41 | 17.81 ± 1.33 | 2.84 ± 1.21 | ||
| SIVstm-like | 15.37 ± 1.41 | 13.38 ± 0.8 | 14.74 ± 1.11 | 15.01 ± 1.13 | 24.33 ± 1.47 | 16.78 ± 2.02 | 17.31 ± 1.01 | 18.65 ± 0.75 | 8.28 | |
| Wild SMs | 14.95 ± 3.83 | 14.36 ± 1.61 | 15.64 ± 1.18 | 14 ± 2.38 | 22.41 ± 1.81 | 15.7 ± 2.19 | 16.33 ± 1.84 | 18.12 ± 1.7 | 16.6 ± 1.69 | 14.71 ± 3.34 |
NA, not available (a single strain was available for each lineage).
Genetic distances in gag between lineage 4 and SIVmac lineage were significantly lower than all the remaining interlineage genetic distances and the distances between lineage 4 and SIVmac in the env gene, suggesting a common phylogenetic history for the two lineages and the recombinant nature of one of them.
Both SIVsm strains which have been reported to be pathogenic in SMs (SIVsmmPBj and SIVsmE041) (27, 45) and the strains reported to be pathogenic in rhesus monkeys or PTMs (SIVsmPBj, SIVsm236/660/543-3, SIVsmPTM, and SIVsmB670) (26, 38, 51, 53, 55) belong to lineage 1. One of the viruses belonging to lineage 4 (SIVsmG930) was recently shown to be pathogenic in a heterologous African species, the black mangabey (1). Lineages 2 to 7 have not been tested for virulence in rhesus monkeys.
The cocirculation of different SIVsm lineages in SMs from the TNPRC colony resulted in founder effects, recombinant forms (RFs), and superinfections.
Our results point to the introduction of at least nine different SIVsm strains with the importation of SMs to establish the four SM colonies in the United States (Fig. 2). The differentiation in lineages occurred following natural or accidental SIVsm spread over a 40-year period. Many of the TNPRC samples were obtained during leprosy experiments performed on SMs at TNPRC in the 1980s (32, 76). Most of the SMs involved in these studies were already positive when inoculated intravenously and intradermally with lepromatous tissues from monkey SM#A022, who was infected with a lineage 1 virus. In most cases, the testing of sera before and after leprosy exposure did not show any evidence of a superinfection. However, superinfection and recombination occurred in monkey SM#D176, who was infected with a lineage 2 virus prior to the leprosy experiments and harbored a recombinant form (lineage 1 gag/lineage 2 env) from 1 month post-leprosy exposure on (Fig. 1a to c). Another monkey (SM#F104) was shown to carry a recombinant lineage 1 gag/lineage 8 env virus prior to leprosy exposure (Fig. 1a to c and 4, left panel). After experimental exposures of animals to tissues from monkey SM#A022, an env fragment clustering with lineage 1 was transiently present and then only RF1/8 could be amplified (Fig. 1a to c). To exclude the possibility of PCR contamination, we extracted RNAs from two different time points prior to the leprosy exposure. Both of these fragments clustered with lineage 8 (SIVmac) in env trees and with lineage 1 in gag trees. Moreover, the SIVsmF104 recombinant did not result from an experimental/accidental exposure to prototype SIVmac strains because these samples were obtained prior to the discovery of SIVmac in 1985 (23). Finally, the SIVmac-like strain was already infecting monkey SM#F104 at the time of its transfer from YNPRC. Therefore, one may expect that SIVmac-like strains are circulating in the SM colony at YNPRC.
FIG. 4.
Phylogenetic evidence of intragenic recombination in gag. Neighbor-joining phylogenetic trees of the 5′ (bp 1 to 500) and 3′ (bp 501 to 727) gag fragments show distinct clustering patterns for 21 “lineage 1” strains. These strains (red) cluster with lineage 1 strains in the 5′ tree and with lineage 2 strains in the 3′ tree. The clustering patterns suggest that together these 21 strains share the same recombinant ancestry and therefore define a recombinant form.
One of the 10 samples from YNPRC (SM#FVN) also showed an RF1/2 structure (Fig. 1a to c). Finally, strain CFU219 from CNPRC clusters with lineage 7 in the pol tree and independently in the LTR-gag tree. Altogether, this analysis shows that, similar to the case with HIV-1 group M subtypes, for which the emergence of circulating recombinant forms (CRFs) has been documented for those regions in which several subtypes cocirculate (2), the cocirculation and accidental or experimental spread of different SIVsm lineages in colonies may result in SIV RFs and superinfections.
In the gag phylogenetic tree, one of the strains, D176, clusters basal to the lineage 1 strains. Diversity plotting was carried out to compare the relative pairwise diversity of this strain to that of other strains in the alignment (data not shown). D176 clustered more closely to the lineage 1 strains at the 5′ end of the alignment and more closely to lineage 2 strains at the 3′ end of the alignment. Phylogenetic trees were constructed for the 5′ and 3′ ends of the alignments (Fig. 4). D176 has a discordant phylogenetic position in these two phylogenies, clustering with lineages 1 and 2 in the 5′ and 3′ ends of the alignment, respectively, indicating that intragenic recombination has occurred. Interestingly, another 20 strains shared the same discordant phylogenetic relationships, suggesting that, together, these 21 strains share the same recombinant ancestry (Fig. 4). This putative recombinant history of these strains is the most parsimonious explanation for the observed relationships. An alternative history, supported by the consistent clustering of the strains in red in Fig. 4 with lineages 4 and 8, is that two recombination events occurred at about the same point. Note that the clustering with lineages 4 and 8 is not supported by the bootstrap replicates.
Our results point to the emergence of a circulating recombinant form (CRF) in SMs from primate centers in the United States. This form originated from YNPRC. A similar situation was described by us and others for humans, in which CRFs are rapidly spread (2, 59, 62). This SIVsm CRF1/2 was further spread at TNPRC through the leprosy experiments.
Impact of viral diversity on serological diagnostics.
The effects of SIVsm variability on the immunodominant Ab region of gp41 were investigated. The small loop of the immunodominant region of SIVsm/SIVmac/HIV-2 strains is highly conserved among lineages. Thus, 23 of 31 lineage 1 strains, 12 of 13 lineage 2 strains, 9 of 10 lineage 4 strains, and all lineage 3, 6, 7, and 9 viruses show no substitution compared to the consensus sequence. Lineage 5 viruses show two substitutions in this region. Also, SIVmac strains harbor a specific signature. All but one SIVsm strain originating from wild SMs show no substitution in this region. Our previous studies also revealed a limited variability in this region in HIV-2 (21). These sequence analyses suggest that the viral diversity of SIVsm/SIVmac strains will have little or no impact on serological diagnosis, which rules out the possibility that SIVsm strains will go undetected by standard diagnostic tests. To confirm this conclusion, we used a TM peptide assay to test 46 samples belonging to eight lineages and observed no significant difference in serological reactivities (data not shown). These results rule out the possibility that SIVsm infections went undetected by the HIV-2 serological tests that are widely used for SIVsm screening.
Impact of viral diversity on viral replication, as monitored by VL testing.
Some recent studies on the pathogenesis of SIVsm used RT-PCR to quantify SIVsm VL (42, 67). These studies did not consider viral diversity in their primer design, and therefore the results might be influenced by mismatches between primer sequences and virus genes. Since the gag fragment investigated in this study overlapped the region used for RT-PCR quantification, the suitability of the currently used primers for the quantification of divergent SIVsm lineages was evaluated. Table 3 shows the mismatches between the gag primers (based on the sequence of SIVmac239) and 86 isolates belonging to different lineages. This analysis shows that sequence variability may influence SIVsm quantification when SIVmac-based primers are used for RT-PCR. VL quantification in the plasma for lineages 2 and 3 and lineages 5 and 7, which harbor mismatches for the beginning sequence of the forward and the reverse primer, respectively, may be below the true values when this assay is used. A comparative quantification between different lineages is necessary prior to performing pathogenesis studies.
TABLE 3.
Potential impact of SIVsm diversity on VL quantification by RT-PCR
| SIV type (n) | Mismatches with primera
|
|
|---|---|---|
| AGAAAGCCTGTTGGAIAACAAAGAAGG (forward primer) | CACGCAGAAGAGAAAGTGAAACACACT (reverse primer) | |
| Lineage 1 (31) | 24G18C | 1T31T |
| 2A1G | ||
| 5T | ||
| Lineage 2 (19) | 1G1T12G9C9T1G | 1T1T1A2G19T |
| 7A3G | ||
| Lineage 3 (9) | 1G9G1T | 1G3C1G9T |
| Lineage 4 (11) | 11A 10C | 11T |
| Lineage 5 (3) | 1G3G | 3T3A |
| Lineage 6 (1) | 1A1T | 1T |
| Lineage 7 (6) | 2G8A | 5T3C |
| SIVmac (5) | ||
| SIVstm | 1G1T1C1A1G | 1T |
Numbers preceding mismatches represent the numbers of occurences.
DISCUSSION
We investigated the SIVsm diversity and molecular epidemiology in four primate centers in the United States over a 30-year period and determined the consequences for diagnosis and monitoring of SIVsm infections. Our results showed that nine putative SIVsm subtypes (called lineages in this report) have cocirculated in primate centers and that two of these subtypes were the ancestral lineages of the macaque reference strains SIVmac/SIVmne and SIVstm. Therefore, our results show that the epizootics of lymphomas and opportunistic infections in macaques at the California National Primate Research Center were due to SIVsm strains acquired by macaques (47, 48).
SIVsm diversity in primate centers mirrors the diversity of HIV-1 group M subtypes.
A significant challenge for HIV vaccine development is dealing with viral diversity, which is not adequately incorporated into existing nonhuman primate models of AIDS. The cocirculation of highly divergent viruses in SMs offers ample opportunities for the development of reagents that are useful for comparative pathogenesis and vaccine studies since these SIVsm lineages show the same degree of divergence as HIV-1 subtypes (2). This extensive SIVsm diversity went undetected before, and prior to our previous study (46), only one of the nine SIVsm lineages, SIVsmB670/PBJ/236, was known to infect SMs (36, 44, 47, 53). Two other hypothetical lineages have been postulated based on viruses isolated from rhesus monkeys and STMs (SIVmac251/SIVmac239/SIVmne and SIVstm), but they were not detected in SMs prior to this report.
For HIV-1 infections, the study of subtype distributions allowed worldwide viral spread to be monitored: numerous studies have shown that the subtype prevalence can vary significantly from country to country and within population groups and can change with time (2, 62). Our molecular epidemiologic study of SIVsm diversity in different primate centers in the United States allowed us to trace the virus spread between different colonies during the last 30 years (Fig. 2). The divergent SIVsm strains were most probably introduced to the United States via mangabey importation and were initially acquired by contact with infected SMs in their native habitat in West Africa, as is the case for the lineage 6 virus (strain SIVsmD215 from the TNPRC) isolated from a monkey imported directly from Africa. The idea of multiple SIVsm strain importation from Africa is supported by the fact that the genetic distances between SIVsm lineages are similar to those observed among SIVsm strains in the wild (Fig. 1; Table 2). The diversification of imported strains into lineages probably resulted as a consequence of independent founder effects occurring naturally or experimentally in SM colonies. The same founder effect mechanism was proposed by us and others for the emergence of HIV subtypes (2, 59, 73, 74). None of the SIVsm lineages were very closely related to any of the known HIV-2 groups or to previously reported SIVsm strains originating from the natural range of the naturally SIVsm-infected SMs (3, 15, 50, 61).
An analysis of samples collected over a 20-year period showed that the natural history of SIVsm transmission in a setting where different lineages cocirculated resulted in founder effects, recombination, and superinfections. These phenomena model the spread and diversification of HIV-1 group M strains in regions where different subtypes cocirculate (2, 62). This is particularly important because for this relatively small SM colony, we have documented mechanisms of lentiviral diversification similar to those described for HIV-1 subtypes worldwide. In the case of HIV-1, strain emergence and diversification rely on founder effects in particular epidemiologic contexts (54). Thus, HIV-1 emergence in the Western hemisphere involved subtype B, which established itself in homosexuals and intravenous drug users (54). In Eastern Europe, the HIV-1 epidemic first emerged involving relatively minor subtypes which were fueled by nosocomial transmission (4, 11). As a second step of HIV-1 diversification in a given geographical area, the cocirculation of different subtypes results in superinfections and recombinations, generating circulating recombinant forms (52). It is noteworthy that most of the CRFs described to date originated in intravenous drug users (2, 52, 62). In our study, superinfections and recombinations were documented following the experimental intravenous exposure of SMs to tissues in an attempt to transmit leprosy (32).
Our analysis of CNPRC samples shows that naturally infected SMs from the CNPRC were the source of all SIVmac/SIVmne and SIVstm strains. Also, SIVmac and lineage 4 strains clustered together in gag trees and independently in env trees, suggesting a recombinant nature for one of these lineages (Fig. 1a). The potential recombinant nature of SIVmac strains may explain their high pathogenic potential and fitness in a heterologous macaque host.
Consequences of SIVsm diversity for diagnosis and monitoring.
The observed sequence variation among the SIV lineages had no impact on the detection of anti-SIVsm antibodies in monkeys infected with SIVsm strains belonging to different phylogenetic lineages. However, sequence variation may affect the reliability of real-time PCR assays across different lineages, and therefore the specific sequence of the lineage targeted for quantification should be considered during primer design.
In conclusion, our study showed significant diversity among SIVsm strains in the past and present colonies of SMs in primate centers in the United States. This genetic diversity mirrors that of HIV-1 group M subtypes. A molecular epidemiologic investigation over a 30-year period revealed that the diversification of these SIVsm lineages was produced by the same mechanisms described for HIV-1 group M subtypes, involving founder effects, superinfections, and recombinations. Therefore, this study points to a model for the molecular epidemiology of HIV. This approach should be extremely useful for modeling the efficacy of vaccination strategies in real-world situations of HIV-1 diversity.
Most past experiments involving SIVsm transmission to rhesus monkeys used viruses belonging to lineage 1. The pathogenic potential of primary isolates from the other SIVsm lineages should be investigated in order to determine if these viruses are intrinsically pathogenic to rhesus monkeys. Finally, our study showed that SIVsm infection monitoring should take into account the high degree of SIV diversity in laboratory and animal colonies.
Acknowledgments
This work was supported by funds from grants RO1 AI-19301, RO1 AI-44596, RO1 AI149809, P20 RR020159, and P51 RR000164 from the National Institutes of Health.
We thank Megan Mefford, Meredith Hunter, Nora Dillon, and Robin Rodriguez for their technical assistance. We also thank the veterinary and animal care staff of TNPRC for their service and expertise.
REFERENCES
- 1.Apetrei, C., B. Gormus, I. Pandrea, M. Metzger, P. ten Haaft, L. N. Martin, R. Bohm, X. Alvarez, G. Koopman, M. Murphey-Corb, R. S. Veazey, A. A. Lackner, G. Baskin, J. Heeney, and P. A. Marx. 2004. Direct inoculation of simian immunodeficiency virus from sooty mangabeys in black mangabeys (Lophocebus aterrimus): first evidence of AIDS in a heterologous African species and different pathologic outcomes of experimental infection. J. Virol. 78:11506-11518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Apetrei, C., P. A. Marx, and S. M. Smith. 2004. The evolution of HIV and its consequences. Infect. Dis. Clin. N. Am. 18:369-394. [DOI] [PubMed] [Google Scholar]
- 3.Apetrei, C., M. J. Metzger, D. Robinson, B. Ling, P. T. Telfer, P. Reed, D. L. Robertson, and P. A. Marx. 2005. Detection and partial characterization of new simian immunodeficiency virus (SIVsm) strains from bush meat samples from rural Sierra Leone. J. Virol. 79:2631-2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apetrei, C., A. Necula, C. Holm-Hansen, I. Loussert-Ajaka, I. Pandrea, C. Cozmei, A. Streinu-Cercel, F. R. Pascu, E. Negut, G. Molnar, M. Duca, M. Pecec, F. Brun-Vezinet, and F. Simon. 1998. HIV-1 diversity in Romania. AIDS 12:1079-1085. [PubMed] [Google Scholar]
- 5.Apetrei, C., D. L. Robertson, and P. A. Marx. 2004. The history of SIVs and AIDS: epidemiology, phylogeny and biology of isolates from naturally SIV infected non-human primates (NHP) in Africa. Front. Biosci. 9:225-254. [DOI] [PubMed] [Google Scholar]
- 6.Bailes, E., F. Gao, F. Bibollet-Ruche, V. Courgnaud, M. Peeters, P. A. Marx, B. H. Hahn, and P. M. Sharp. 2003. Hybrid origin of SIV in chimpanzees. Science 300:1713. [DOI] [PubMed] [Google Scholar]
- 7.Baskin, G. B., L. N. Martin, S. R. Rangan, B. J. Gormus, M. Murphey-Corb, R. H. Wolf, and K. F. Soike. 1986. Transmissible lymphoma and simian acquired immunodeficiency syndrome in rhesus monkeys. J. Natl. Cancer Inst. 77:127-139. [PubMed] [Google Scholar]
- 8.Benveniste, R. E., L. O. Arthur, C. C. Tsai, R. Sowder, T. D. Copeland, L. E. Henderson, and S. Oroszlan. 1986. Isolation of a lentivirus from a macaque with lymphoma: comparison with HTLV-III/LAV and other lentiviruses. J. Virol. 60:483-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bibollet-Ruche, F., E. Bailes, F. Gao, X. Pourrut, K. L. Barlow, J. Clewley, J. M. Mwenda, D. K. Langat, G. K. Chege, H. M. McClure, E. Mpoudi-Ngole, E. Delaporte, M. Peeters, G. M. Shaw, P. M. Sharp, and B. H. Hahn. 2004. A new simian immunodeficiency virus lineage (SIVdeb) infecting de Brazza's monkeys (Cercopithecus neglectus): evidence for a Cercopithecus monkey virus clade. J. Virol. 78:7748-7762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bibollet-Ruche, F., A. Galat-Luong, G. Cuny, P. Sarni-Manchado, G. Galat, J. P. Durand, X. Pourrut, and F. Veas. 1996. Simian immunodeficiency virus infection in a patas monkey (Erythrocebus patas): evidence for cross-species transmission from African green monkeys (Cercopithecus aethiops sabaeus) in the wild. J. Gen. Virol. 77:773-781. [DOI] [PubMed] [Google Scholar]
- 11.Bobkov, A., M. M. Garaev, A. Rzhaninova, P. Kaleebu, R. Pitman, J. N. Weber, and R. Cheingsong-Popov. 1994. Molecular epidemiology of HIV-1 in the former Soviet Union: analysis of env V3 sequences and their correlation with epidemiologic data. AIDS 8:619-624. [PubMed] [Google Scholar]
- 12.Chakrabarti, L. A., S. R. Lewin, L. Zhang, A. Gettie, A. Luckay, L. N. Martin, E. Skulsky, D. D. Ho, C. Cheng-Mayer, and P. A. Marx. 2000. Normal T-cell turnover in sooty mangabeys harboring active simian immunodeficiency virus infection. J. Virol. 74:1209-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charleston, M. A., and D. L. Robertson. 2002. Preferential host switching by primate lentiviruses can account for phylogenetic similarity with the primate phylogeny. Syst. Biol. 51:528-535. [DOI] [PubMed] [Google Scholar]
- 14.Chen, Z., A. Luckay, D. L. Sodora, P. Telfer, P. Reed, A. Gettie, J. M. Kanu, R. F. Sadek, J. Yee, D. D. Ho, L. Zhang, and P. A. Marx. 1997. Human immunodeficiency virus type 2 (HIV-2) seroprevalence and characterization of a distinct HIV-2 genetic subtype from the natural range of simian immunodeficiency virus-infected sooty mangabeys. J. Virol. 71:3953-3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen, Z., P. Telfier, A. Gettie, P. Reed, L. Zhang, D. D. Ho, and P. A. Marx. 1996. Genetic characterization of new West African simian immunodeficiency virus SIVsm: geographic clustering of household-derived SIV strains with human immunodeficiency virus type 2 subtypes and genetically diverse viruses from a single feral sooty mangabey troop. J. Virol. 70:3617-3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Courgnaud, V., B. Abela, X. Pourrut, E. Mpoudi-Ngole, S. Loul, E. Delaporte, and M. Peeters. 2003. Identification of a new simian immunodeficiency virus lineage with a vpu gene present among different Cercopithecus monkeys (C. mona, C. cephus, and C. nictitans) from Cameroon. J. Virol. 77:12523-12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Courgnaud, V., P. Formenty, C. Akoua-Koffi, R. Noe, C. Boesch, E. Delaporte, and M. Peeters. 2003. Partial molecular characterization of two simian immunodeficiency viruses (SIV) from African colobids: SIVwrc from Western red colobus (Piliocolobus badius) and SIVolc from olive colobus (Procolobus verus). J. Virol. 77:744-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Courgnaud, V., F. Liegeois, W. M. Switzer, S. Loul, E. Mpoudi-Ngole, E. Delaporte, and M. Peeters. 2004. Full molecular characterization of simian immunodeficiency virus infecting talapoins monkeys: evidence for a new SIV lineage in Miopithecus species, abstr. 379. Abstr. 11th Conf. Retrovir. Opportunistic Infect., San Francisco, Calif.
- 19.Courgnaud, V., X. Pourrut, F. Bibollet-Ruche, E. Mpoudi-Ngole, A. Bourgeois, E. Delaporte, and M. Peeters. 2001. Characterization of a novel simian immunodeficiency virus from guereza colobus monkeys (Colobus guereza) in Cameroon: a new lineage in the nonhuman primate lentivirus family. J. Virol. 75:857-866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Courgnaud, V., M. Salemi, X. Pourrut, E. Mpoudi-Ngole, B. Abela, P. Auzel, F. Bibollet-Ruche, B. Hahn, A. M. Vandamme, E. Delaporte, and M. Peeters. 2002. Characterization of a novel simian immunodeficiency virus with a vpu gene from greater spot-nosed monkeys (Cercopithecus nictitans) provides new insights into simian/human immunodeficiency virus phylogeny. J. Virol. 76:8298-8309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Damond, F., C. Apetrei, D. L. Robertson, S. Souquiere, A. Lepretre, S. Matheron, J. C. Plantier, F. Brun-Vezinet, and F. Simon. 2001. Variability of human immunodeficiency virus type 2 (HIV-2) infecting patients living in France. Virology 280:19-30. [DOI] [PubMed] [Google Scholar]
- 22.Damond, F., M. Worobey, P. Campa, I. Farfara, G. Colin, S. Matheron, F. Brun-Vézinet, D. L. Robertson, and F. Simon. 2004. Identification of a highly divergent HIV-2 and proposal for a change in HIV-2 classification. AIDS Res. Hum. Retrovir. 20:666-672. [DOI] [PubMed] [Google Scholar]
- 23.Daniel, M. D., N. L. Letvin, N. W. King, M. Kannagi, P. K. Sehgal, R. D. Hunt, P. J. Kanki, M. Essex, and R. C. Desrosiers. 1985. Isolation of T-cell tropic HTLV-III-like retrovirus from macaques. Science 228:1201-1204. [DOI] [PubMed] [Google Scholar]
- 24.Fultz, P. N. 1994. SIVsmmPBj14: an atypical lentivirus. Curr. Top. Microbiol. Immunol. 188:65-76. [DOI] [PubMed] [Google Scholar]
- 25.Fultz, P. N., H. M. McClure, D. C. Anderson, R. B. Swenson, R. Anand, and A. Srinivasan. 1986. Isolation of a T-lymphotropic retrovirus from naturally infected sooty mangabey monkeys (Cercocebus atys). Proc. Natl. Acad. Sci. USA 83:5286-5290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fultz, P. N., H. M. McClure, D. C. Anderson, and W. M. Switzer. 1989. Identification and biologic characterization of an acutely lethal variant of simian immunodeficiency virus from sooty mangabeys (SIV/SMM). AIDS Res. Hum. Retrovir. 5:397-409. [DOI] [PubMed] [Google Scholar]
- 27.Fultz, P. N., and P. M. Zack. 1994. Unique lentivirus-host interactions: SIVsmmPBj14 infection of macaques. Virus Res. 32:205-225. [DOI] [PubMed] [Google Scholar]
- 28.Gao, F., L. Yue, D. L. Robertson, S. C. Hill, H. Hui, R. J. Biggar, A. E. Neequaye, T. M. Whelan, D. D. Ho, G. M. Shaw, et al. 1994. Genetic diversity of human immunodeficiency virus type 2: evidence for distinct sequence subtypes with differences in virus biology. J. Virol. 68:7433-7447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gardner, M. B. 1996. The history of simian AIDS. J. Med. Primatol. 25:148-157. [DOI] [PubMed] [Google Scholar]
- 30.Georges-Courbot, M. C., C. Y. Lu, M. Makuwa, P. Telfer, R. Onanga, G. Dubreuil, Z. Chen, S. M. Smith, A. Georges, F. Gao, B. H. Hahn, and P. A. Marx. 1998. Natural infection of a household pet red-capped mangabey (Cercocebus torquatus torquatus) with a new simian immunodeficiency virus. J. Virol. 72:600-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goldstein, S., I. Ourmanov, C. R. Brown, B. E. Beer, W. R. Elkins, R. Plishka, A. Buckler-White, and V. M. Hirsch. 2000. Wide range of viral load in healthy African green monkeys naturally infected with simian immunodeficiency virus. J. Virol. 74:11744-11753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gormus, B. J., K. Xu, G. B. Baskin, L. N. Martin, R. P. Bohm, J. L. Blanchard, P. A. Mack, M. S. Ratterree, H. M. McClure, W. M. Meyers, et al. 1995. Experimental leprosy in monkeys. I. Sooty mangabey monkeys: transmission, susceptibility, clinical and pathological findings. Lepr. Rev. 66:96-104. [DOI] [PubMed] [Google Scholar]
- 33.Hasegawa, M., H. Kishino, and T. Yano. 1985. Dating of the human-ape splitting by a molecular clock of mitochondrial DNA. J. Mol. Evol. 22:160-174. [DOI] [PubMed] [Google Scholar]
- 34.Hirsch, V. M., B. J. Campbell, E. Bailes, R. Goeken, C. Brown, W. R. Elkins, M. Axthelm, M. Murphey-Corb, and P. M. Sharp. 1999. Characterization of a novel simian immunodeficiency virus (SIV) from L'Hoest monkeys (Cercopithecus l'hoesti): implications for the origins of SIVmnd and other primate lentiviruses. J. Virol. 73:1036-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hirsch, V. M., G. Dapolito, R. Goeken, and B. J. Campbell. 1995. Phylogeny and natural history of the primate lentiviruses, SIV and HIV. Curr. Opin. Genet. Dev. 5:798-806. [DOI] [PubMed] [Google Scholar]
- 36.Hirsch, V. M., G. Dapolito, C. McGann, R. A. Olmsted, R. H. Purcell, and P. R. Johnson. 1989. Molecular cloning of SIV from sooty mangabey monkeys. J. Med. Primatol. 18:279-285. [PubMed] [Google Scholar]
- 37.Hirsch, V. M., T. R. Fuerst, G. Sutter, M. W. Carroll, L. C. Yang, S. Goldstein, M. Piatak, Jr., W. R. Elkins, W. G. Alvord, D. C. Montefiori, B. Moss, and J. D. Lifson. 1996. Patterns of viral replication correlate with outcome in simian immunodeficiency virus (SIV)-infected macaques: effect of prior immunization with a trivalent SIV vaccine in modified vaccinia virus Ankara. J. Virol. 70:3741-3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hirsch, V. M., and P. R. Johnson. 1994. Pathogenic diversity of simian immunodeficiency viruses. Virus Res. 32:183-203. [DOI] [PubMed] [Google Scholar]
- 39.Hirsch, V. M., R. A. Olmsted, M. Murphey-Corb, R. H. Purcell, and P. R. Johnson. 1989. An African primate lentivirus (SIVsm) closely related to HIV-2. Nature 339:389-392. [DOI] [PubMed] [Google Scholar]
- 40.Ho, D. D., A. U. Neumann, A. S. Perelson, W. Chen, J. M. Leonard, and M. Markowitz. 1995. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature 373:123-126. [DOI] [PubMed] [Google Scholar]
- 41.Jolly, C., J. E. Phillips-Conroy, T. R. Turner, S. Broussard, and J. S. Allan. 1996. SIVagm incidence over two decades in a natural population of Ethiopian grivet monkeys (Cercopithecus aethiops aethiops). J. Med. Primatol. 25:78-83. [DOI] [PubMed] [Google Scholar]
- 42.Kaur, A., R. M. Grant, R. E. Means, H. McClure, M. Feinberg, and R. P. Johnson. 1998. Diverse host responses and outcomes following simian immunodeficiency virus SIVmac239 infection in sooty mangabeys and rhesus macaques. J. Virol. 72:9597-9611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khan, A. S., T. A. Galvin, L. J. Lowenstine, M. B. Jennings, M. B. Gardner, and C. E. Buckler. 1991. A highly divergent simian immunodeficiency virus (SIVstm) recovered from stored stump-tailed macaque tissues. J. Virol. 65:7061-7065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Letvin, N. L., M. D. Daniel, P. K. Sehgal, R. C. Desrosiers, R. D. Hunt, L. M. Waldron, J. J. MacKey, D. K. Schmidt, L. V. Chalifoux, and N. W. King. 1985. Induction of AIDS-like disease in macaque monkeys with T-cell tropic retrovirus STLV-III. Science 230:71-73. [DOI] [PubMed] [Google Scholar]
- 45.Ling, B., C. Apetrei, I. Pandrea, R. S. Veazey, A. A. Lackner, B. Gormus, and P. A. Marx. 2004. Classic AIDS in a sooty mangabey after an 18-year natural infection. J. Virol. 78:8902-8908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ling, B., M. L. Santiago, S. Meleth, B. Gormus, H. M. McClure, C. Apetrei, B. H. Hahn, and P. A. Marx. 2003. Noninvasive detection of new simian immunodeficiency virus lineages in captive sooty mangabeys: ability to amplify virion RNA from fecal samples correlates with viral load in plasma. J. Virol. 77:2214-2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lowenstine, L. J., N. W. Lerche, J. L. Yee, A. Uyeda, M. B. Jennings, R. J. Munn, H. M. McClure, D. C. Anderson, P. N. Fultz, and M. B. Gardner. 1992. Evidence for a lentiviral etiology in an epizootic of immune deficiency and lymphoma in stump-tailed macaques (Macaca arctoides). J. Med. Primatol. 21:1-14. [PubMed] [Google Scholar]
- 48.Mansfield, K. G., N. W. Lerche, M. B. Gardner, and A. A. Lackner. 1995. Origins of simian immunodeficiency virus infection in macaques at the New England Regional Primate Research Center. J. Med. Primatol. 24:116-122. [DOI] [PubMed] [Google Scholar]
- 49.Mansky, L. M., and H. M. Temin. 1995. Lower in vivo mutation rate of human immunodeficiency virus type 1 than that predicted from the fidelity of purified reverse transcriptase. J. Virol. 69:5087-5094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marx, P. A., Y. Li, N. W. Lerche, S. Sutjipto, A. Gettie, J. A. Yee, B. H. Brotman, A. M. Prince, A. Hanson, R. G. Webster, et al. 1991. Isolation of a simian immunodeficiency virus related to human immunodeficiency virus type 2 from a west African pet sooty mangabey. J. Virol. 65:4480-4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McClure, H. M., D. C. Anderson, P. N. Fultz, A. A. Ansari, E. Lockwood, and A. Brodie. 1989. Spectrum of disease in macaque monkeys chronically infected with SIV/SMM. Vet. Immunol. Immunopathol. 21:13-24. [DOI] [PubMed] [Google Scholar]
- 52.McCutchan, F. E. 2000. Understanding the genetic diversity of HIV-1. AIDS 14(Suppl. 3):S31-S44. [PubMed] [Google Scholar]
- 53.Murphey-Corb, M., L. N. Martin, S. R. Rangan, G. B. Baskin, B. J. Gormus, R. H. Wolf, W. A. Andes, M. West, and R. C. Montelaro. 1986. Isolation of an HTLV-III-related retrovirus from macaques with simian AIDS and its possible origin in asymptomatic mangabeys. Nature 321:435-437. [DOI] [PubMed] [Google Scholar]
- 54.Myers, G. 1994. Tenth anniversary perspectives on AIDS. HIV: between past and future. AIDS Res. Hum. Retrovir. 10:1317-1324. [DOI] [PubMed] [Google Scholar]
- 55.Novembre, F. J., J. De Rosayro, S. P. O'Neil, D. C. Anderson, S. A. Klumpp, and H. M. McClure. 1998. Isolation and characterization of a neuropathogenic simian immunodeficiency virus derived from a sooty mangabey. J. Virol. 72:8841-8851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Onanga, R., C. Kornfeld, I. Pandrea, J. Estaquier, S. Souquiere, P. Rouquet, V. P. Mavoungou, O. Bourry, S. M'Boup, F. Barre-Sinoussi, F. Simon, C. Apetrei, P. Roques, and M. C. Muller-Trutwin. 2002. High levels of viral replication contrast with only transient changes in CD4+ and CD8+ cell numbers during the early phase of experimental infection with simian immunodeficiency virus SIVmnd-1 in Mandrillus sphinx. J. Virol. 76:10256-10263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pandrea, I., R. Onanga, C. Kornfeld, P. Rouquet, O. Bourry, S. Clifford, P. T. Telfer, K. Abernethy, L. T. White, P. Ngari, M. Muller-Trutwin, P. Roques, P. A. Marx, F. Simon, and C. Apetrei. 2003. High levels of SIVmnd-1 replication in chronically infected Mandrillus sphinx. Virology 317:119-127. [DOI] [PubMed] [Google Scholar]
- 58.Pandrea, I., R. Onanga, P. Rouquet, O. Bourry, P. Ngari, E. J. Wickings, P. Roques, and C. Apetrei. 2001. Chronic SIV infection ultimately causes immunodeficiency in African non-human primates. AIDS 15:2461-2462. [DOI] [PubMed] [Google Scholar]
- 59.Pandrea, I., D. L. Robertson, R. Onanga, F. Gao, M. Makuwa, P. Ngari, I. Bedjabaga, P. Roques, F. Simon, and C. Apetrei. 2002. Analysis of partial pol and env sequences indicates a high prevalence of HIV type 1 recombinant strains circulating in Gabon. AIDS Res. Hum. Retrovir. 18:1103-1116. [DOI] [PubMed] [Google Scholar]
- 60.Peeters, M., V. Courgnaud, B. Abela, P. Auzel, X. Pourrut, F. Bibollet-Ruche, S. Loul, F. Liegeois, C. Butel, D. Koulagna, E. Mpoudi-Ngole, G. M. Shaw, B. H. Hahn, and E. Delaporte. 2002. Risk to human health from a plethora of simian immunodeficiency viruses in primate bushmeat. Emerg. Infect. Dis. 8:451-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peeters, M., W. Janssens, K. Fransen, J. Brandful, L. Heyndrickx, K. Koffi, E. Delaporte, P. Piot, G. M. Gershy-Damet, and G. van der Groen. 1994. Isolation of simian immunodeficiency viruses from two sooty mangabeys in Cote d'Ivoire: virological and genetic characterization and relationship to other HIV type 2 and SIVsm/mac strains. AIDS Res. Hum. Retrovir. 10:1289-1294. [DOI] [PubMed] [Google Scholar]
- 62.Peeters, M., and P. M. Sharp. 2000. Genetic diversity of HIV-1: the moving target. AIDS 14(Suppl. 3):S129-S140. [PubMed] [Google Scholar]
- 63.Posada, D., and K. A. Crandall. 2001. Selecting the best-fit model of nucleotide substitution. Syst. Biol. 50:580-601. [PubMed] [Google Scholar]
- 64.Preston, B. D. 1997. Reverse transcriptase fidelity and HIV-1 variation. Science 275:228-229. (Letter; author reply, 275:230-231.) [DOI] [PubMed] [Google Scholar]
- 65.Roberts, J. D., K. Bebenek, and T. A. Kunkel. 1988. The accuracy of reverse transcriptase from HIV-1. Science 242:1171-1173. [DOI] [PubMed] [Google Scholar]
- 66.Saitou, N., and M. Nei. 1987. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol. Biol. Evol. 4:406-425. [DOI] [PubMed] [Google Scholar]
- 67.Silvestri, G., D. L. Sodora, R. A. Koup, M. Paiardini, S. P. O'Neil, H. M. McClure, S. I. Staprans, and M. B. Feinberg. 2003. Nonpathogenic SIV infection of sooty mangabeys is characterized by limited bystander immunopathology despite chronic high-level viremia. Immunity 18:441-452. [DOI] [PubMed] [Google Scholar]
- 68.Simon, F., S. Souquiere, F. Damond, A. Kfutwah, M. Makuwa, E. Leroy, P. Rouquet, J. L. Berthier, J. Rigoulet, A. Lecu, P. T. Telfer, I. Pandrea, J. C. Plantier, F. Barre-Sinoussi, P. Roques, M. C. Muller-Trutwin, and C. Apetrei. 2001. Synthetic peptide strategy for the detection of and discrimination among highly divergent primate lentiviruses. AIDS Res. Hum. Retrovir. 17:937-952. [DOI] [PubMed] [Google Scholar]
- 69.Souquiere, S., F. Bibollet-Ruche, D. L. Robertson, M. Makuwa, C. Apetrei, R. Onanga, C. Kornfeld, J. C. Plantier, F. Gao, K. Abernethy, L. J. White, W. Karesh, P. Telfer, E. J. Wickings, P. Mauclere, P. A. Marx, F. Barre-Sinoussi, B. H. Hahn, M. C. Muller-Trutwin, and F. Simon. 2001. Wild Mandrillus sphinx are carriers of two types of lentivirus. J. Virol. 75:7086-7096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Swofford, D. 1999. PAUP*. Phylogenetic analysis using parsimony (*and other methods), version 4. Sinauer Associates, Sunderland, Mass.
- 71.ten Haaft, P., K. Murthy, M. Salas, H. McClure, R. Dubbes, W. Koornstra, H. Niphuis, D. Davis, G. van der Groen, and J. Heeney. 2001. Differences in early virus loads with different phenotypic variants of HIV-1 and SIV(cpz) in chimpanzees. AIDS 15:2085-2092. [DOI] [PubMed] [Google Scholar]
- 72.Thompson, J. D., D. G. Higgins, and T. J. Gibson. 1994. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 22:4673-4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Triques, K., A. Bourgeois, S. Saragosti, N. Vidal, E. Mpoudi-Ngole, N. Nzilambi, C. Apetrei, M. Ekwalanga, E. Delaporte, and M. Peeters. 1999. High diversity of HIV-1 subtype F strains in Central Africa. Virology 259:99-109. [DOI] [PubMed] [Google Scholar]
- 74.Vidal, N., M. Peeters, C. Mulanga-Kabeya, N. Nzilambi, D. Robertson, W. Ilunga, H. Sema, K. Tshimanga, B. Bongo, and E. Delaporte. 2000. Unprecedented degree of human immunodeficiency virus type 1 (HIV-1) group M genetic diversity in the Democratic Republic of Congo suggests that the HIV-1 pandemic originated in Central Africa. J. Virol. 74:10498-10507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wei, X., S. K. Ghosh, M. E. Taylor, V. A. Johnson, E. A. Emini, P. Deutsch, J. D. Lifson, S. Bonhoeffer, M. A. Nowak, B. H. Hahn, et al. 1995. Viral dynamics in human immunodeficiency virus type 1 infection. Nature 373:117-122. [DOI] [PubMed] [Google Scholar]
- 76.Wolf, R. H., B. J. Gormus, L. N. Martin, G. B. Baskin, G. P. Walsh, W. M. Meyers, and C. H. Binford. 1985. Experimental leprosy in three species of monkeys. Science 227:529-531. [DOI] [PubMed] [Google Scholar]
- 77.Yamaguchi, J., S. G. Devare, and C. A. Brennan. 2000. Identification of a new HIV-2 subtype based on phylogenetic analysis of full-length genomic sequence. AIDS Res. Hum. Retrovir. 16:925-930. [DOI] [PubMed] [Google Scholar]