Abstract
Background
The objective of this study is to evaluate the risk of being diagnosed with an eating disorder among transgender and gender-diverse (TGD) individuals, specifically examining how this risk differs following gender-affirming medical therapy (GAMT).
Methods
The study utilizes electronic medical record (EMR) data from the TriNetX database. A total of 90,955 TGD individuals were identified in the TriNetX database. TGD individuals were divided into cohorts according to gender-affirming interventions they received. To assess the risk of eating disorder diagnoses across groups, we applied a Cox proportional hazards model with gender-affirming care as a time-varying covariate.
Results
Here we show that transfeminine individuals receiving hormone therapy (HT) have a significantly higher likelihood of being diagnosed with an eating disorder compared to those without intervention (HR:1.67, 95% CI:1.41, 1.98). Conversely, transmasculine individuals on HT exhibit a reduced risk of being diagnosed with an eating disorder relative to those without intervention (HR: 0.83, 95% CI: 0.76, 0.90).
Conclusions
After undergoing gender-affirming medical therapy, the risk of eating disorder diagnosis increases for transfeminine individuals and decreases for transmasculine individuals. The observed differences in risk between transfeminine and transmasculine individuals on GAMT may be attributed to factors such as gendered societal norms, variations in screening practices, and the physiological effects of hormone therapy on eating disorder symptomatology. Further research is needed to clarify these influences and support tailored interventions.
Subject terms: Diagnosis, Epidemiology
Loria, Tabernacki et al. investigate the risk of eating disorder diagnoses among transgender and gender-diverse individuals. Transfeminine individuals on hormone therapy are more likely to be diagnosed with eating disorders, while transmasculine individuals on hormone or surgical therapy are less likely to receive such diagnoses.
Plain Language Summary
Transgender and gender-diverse (TGD) individuals are at a higher risk of developing eating disorders, but the effects of gender-affirming interventions on this risk is not well known. Our study used data from nearly 91,000 TGD individuals to explore how hormone therapy and surgical transitioning might influence eating disorder diagnosis risk. We found that transfeminine individuals (those assigned male at birth who identify as female) on hormone therapy were more likely to be diagnosed with an eating disorder, while transmasculine individuals (those assigned female at birth who identify as male) on hormone therapy were less likely to receive such a diagnosis compared to TGD individuals not on hormone therapy. This difference in risk between transfeminine and transmasculine individuals may be explained by gendered societal norms, variations in screening practices, and the physiological effects of hormone therapy on eating disorder symptoms. Our findings highlight the need for supportive care and careful screening for eating disorders in TGD individuals receiving gender-affirming interventions.
Introduction
Eating disorders (ED) are psychiatric conditions which significantly impact physical health and psychosocial functioning, and can be characterized by an intense preoccupation with weight and body shape. Examples of the most common eating disorders include: anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED). In the United States, roughly 1 in 7 males and 1 in 5 females will experience an eating disorder by age 401. Eating disorders can occur across all age groups and genders. A significant upward trend in the prevalence of eating disorders has been observed recently, increasing from 3.5% during 2000-2006 to 7.8% during 2013-20182.
The causes of eating disorders are multifaceted and complex. They include biological, psychological, developmental, racial and socio-cultural factors3. Biological risk factors include genetic predisposition and neurotype factors4. Psychological traits such as perfectionism, impulsivity, and harm avoidance can also predispose individuals to these disorders4. Developmental factors such as early childhood trauma, internalized socio-cultural factors, and western standards of beauty factors that emphasize thinness can also increase the risk of eating disorders4,5. The majority of research in the field of eating disorders focuses on individuals who were assigned female at birth, and primarily with cisgender girls and women (i.e. those whose gender aligns with their sex assigned at birth).
Transgender and gender diverse (TGD) individuals are those whose gender identity does not align with their sex assigned at birth. Many studies have indicated that transgender individuals may be at increased risk of developing eating disorders6–9. In fact Heiden-Rootes et al. reported that 15 of the articles included in the systematic review all reported higher prevalence of ED among TGD individuals compared to cisgender counterparts9. One study in particular among TGD college students, found a 4.6x fold increase in risk of being diagnosed with an ED compared to other cisgender college students10.
Moreover, TGD individuals have been found to have a higher prevalence of eating disorder symptoms compared to their cisgender counterparts11,12. Specifically, transfeminine individuals had a higher likelihood of past-month use of diet pills (OR, 2.05; 95% CI, 1.48–2.83) and vomiting or laxative use (OR, 2.46; 95% CI, 1.83–3.30) in comparison to cisgender heterosexual women10. Other subgroups, such as young adult transgender men, have reported high rates of problematic eating behaviors, including binge eating (35%), fasting (34%), and vomiting (7%)13. When examining the reasons for ED symptoms among TGD, Algars et al found that TGD individuals reported ED symptoms as a means of suppressing characteristics of their sex assigned at birth and/or augmenting their gender identity14. This is supported by several case studies in which the main reason for ED symptomatology was to control physical shape to align with their gender identity15–17. Furthermore, a recent systematic review compiled a list of other high risks for the development of eating disorder symptomatology including: body dysmorphia, body shape concerns, dissatisfaction with body compared to cultural gender-body ideals, lack of support in school, and familial rejection9,11.
When considering those undergoing gender-affirming interventions, studies have shown improvement in mental health symptoms, including disordered eating behaviors after such interventions.6,18–20. Specifically, studies like Nowaskie et al. have found that gender-affirming medical therapy (GAMT; both medical and surgical) lead to decreased eating disorder symptomatology20. The effect of GAMT on ED symptomatology was found to be primarily driven through a reduction in body dysmorphia21. However, the type of GAMT received may affect this reduction. Nowaskie et al. reported that a reduction in ED symptomatology was only present among TGD who had hormone therapy and surgical intervention; they found no reduction in ED symptomology in those with just hormone therapy20. While GAMT may be one protective factor against eating disorder development, Heiden- Rootes et al. also found that family and social support, and a safe school environment9 also serve as protective factors. This together builds the complex biopsychosocial complexities involved in ED development that necessitate further research to clarify these factors
When specifically examining the effects of GAMT on eating disorder (ED) development, many studies, such as those by Rasmussen et al. and Heiden-Rootes et al., analyze ED symptomatology among TGD individuals before and after GAMT8,9. However, there is minimal research characterizing how GAMT may modulate the risk of being diagnosed with a new ED and how this risk may differ between transmasculine and transfeminine individuals. Understanding these changes in diagnosis risk throughout an individual’s gender transition is essential.
The primary objective of this study was to evaluate the risk of being diagnosed with a new eating disorder among the TGD population and how that risk differs between transfeminine spectrum individuals (TF; those assigned male at birth and identify as a woman or on the feminine spectrum) and transmasculine spectrum individuals (TM; those assigned female at birth and identify as a man or on the masculine spectrum). Among all new eating disorder diagnoses, we particularly examined the risk of being diagnosed with AN, BN, or BED. Additionally, a second objective of this study was to elucidate how this risk of ED diagnosis may be modulated by the medical and surgical gender-affirmation journey. We find that among TF individuals, the risk of being diagnosed with an eating disorder increases after medical, but not surgical gender-affirming interventions. Conversely, we find that among TM individuals, the risk of being diagnosed with an eating disorder decreases after both medical and surgical gender-affirming interventions. Of all eating disorders diagnoses among both TF and TM individuals, Anorexia Nervosa is the most significant contributor.
Methods
Data source
We used global-based data from the network TriNetX (TriNetX, Inc., Cambridge, MA, United States), a multinational collaborative clinical research platform that collects real-time medical records on patients of all insurance types. This network included 81 healthcare organizations at the time of analysis, including data from around 107 million patients. Sources of patient records were relatively evenly distributed across the United States (25% Northeast, 24% Midwest, 21% South and 30% West). The TriNetX platform uses aggregated counts and statistical summaries of de-identified information so that no protected health information or personal data are made available to users of the platform. All participating HCOs attest that they have the necessary rights, consents, approvals and authorities to provide this data with TriNetX through Business Associate Agreements as long as patients’ names remain anonymous and this data is used for research purposes. At our institution, University Hospital’s, the institutional review board determined that data from TriNetX is not human subject research and is therefore exempt from approval.
TriNetX completes an intensive data preprocessing stage to minimize missing values. Data are mapped to a standard and controlled set of clinical terminologies and converted to a proprietary data schema. This transformation process includes an extensive data quality assessment to reject records that do not meet quality standards. Quality assurance of the data is performed using a standardized format before integration into the database.
All covariates are either binary, categorical (which expands to a set of binary columns), or continuous but essentially guaranteed to exist. Age is guaranteed to exist. Missing sex values are represented using “Unknown Sex”. The missing data for race and ethnicity are presented as “Unknown race” or “Unknown Ethnicity”. For other variables including medical conditions, procedures, lab tests, and socio-economic determinant health, the value is either present or absent so “missing” is not pertinent.
We gained access to TriNetX through agreeing to a data user agreement arranged between University Hospitals and TriNetX. Data was extracted and analyzed from the Research Network on the TriNetX platform on July 10, 2023. Patients with a F64 Gender Identity Disorder ICD-10 code were divided into cohorts based on treatment received per ICD-10 codes. The cohort creation criteria for the transfeminine and transmasculine cohorts can be found in the Supplementary Data.
Study population
In this retrospective cohort study, we queried the database to select patients who identified as transgender and gender diverse (TGD) based on the presence of ICD-10 codes indicating gender identity disorders (GID) (ICD-10 codes F64.0-F64.9), which has been shown to be a highly specific method of identifying transgender patients in the EHR/EMR record22–24. Recent studies have shown an 88-100% accuracy in identifying transgender status based on ICD codes22. We acknowledge that the term GID has been updated in the DSM-5 to Gender Dysphoria and therefore we will only use the term GID to reference the specific ICD-10 code used to query our population. We also agree that the current use of ICD-10 codes for GID diagnosis can pathologize one’s transgender identity into a medical diagnosis. We therefore only use this ICD-10 code to identify transgender individuals and we do not support this code’s pathologization of a non-cisgender identity. Furthermore, this group was then divided into several cohorts based on whether the type of gender-affirming care an individual received. We created four cohorts: those receiving hormone replacement therapy (HT), those who received gender-affirming surgical intervention (SX), those who received any form of gender-affirming care (HT and/or SX)(Any GAMT), and those who have had no gender-affirming interventions (Referred to as no intervention; NI). For all patients, we collected available clinical data including patient demographics (age, race, sex, ethnicity), BMI, comorbid conditions (Table 1), and the outcomes of developing an eating disorder (ICD-10: F50), including Anorexia Nervosa, Bulimia, and Binge eating (both as individual and composite outcomes), occurring any time after the diagnosis of GID (index event). The primary outcome was a new diagnosis of F50 after the index event. While Anorexia Nervosa, Bulimia, and Binge Eating disorder were the three most prevalent eating disorders, other eating disorders such as Other Specified Feeding or Eating Disorders (OSFED) and Eating Disorder Not Otherwise Specified (EDNOS) would be captured in the cohort titled “Eating Disorder (composite)”. This cohort includes individuals with any subtype of a F50 diagnosis (EDNOS and OSFED included).
Table 1.
Baseline demographics and characteristics between patients with gender dysphoria (GD) and no documented gender-affirming medical therapy (no GAMT) versus patients with GD and with any documented GAMT
| Characteristic | Overall (GD diagnosis) N = 90,955 | NI N = 34,556 |
Any GAMT (HT or SX) N = 56,399 | HT N = 52,699 |
SX N = 10,537 |
p-value |
|---|---|---|---|---|---|---|
| Age at diagnosis | 25.8 ± 13.3 | 24.6 ± 14.6 | 26.6 ± 12.4 | 26.4 ± 12.5 | 28.5 ± 11.8 | <0.001 |
| Unknown | 63 | 52 | 11 | 10 | 2 | |
| Median length since GID Diagnosis (days) | 675 | 370 | 908 | 952 | 510 | |
| Sex at birth | <0.001 | |||||
| Female | 51,896 (57.1%) | 20,420 (59.1%) | 31,476 (55.8%) | 28,890 (54.8%) | 6954 (66.0%) | |
| Male | 38,082 (41.9%) | 13,816 (40.0%) | 24,266 (43.0%) | 23,224 (44.1%) | 3421 (32.5%) | |
| Unknown | 977 (1.1%) | 320 (0.9%) | 657 (1.2%) | 585 (1.1%) | 162 (1.5%) | |
| Race | <0.001 | |||||
| American Indian or Alaska Native | 773 (0.8%) | 307 (0.9%) | 466 (0.8%) | 440 (0.8%) | 78 (0.7%) | |
| Asian | 2110 (2.3%) | 828 (2.4%) | 1282 (2.3%) | 1208 (2.3%) | 252 (2.4%) | |
| Black or African American | 7256 (8.0%) | 3119 (9.0%) | 4137 (7.3%) | 3882 (7.4%) | 787 (7.5%) | |
| Native Hawaiian or Other Pacific Islander | 309 (0.3%) | 166 (0.5%) | 143 (0.3%) | 138 (0.3%) | 20 (0.2%) | |
| White | 63,204 (69.5%) | 23,139 (67.0%) | 40,065 (71.0%) | 37,569 (71.3%) | 1994 (18.9%) | |
| Unknown | 17,303 (19.0%) | 6997 (20.2%) | 10,306 (18.3%) | 9462 (18.0%) | 7406 (70.3%) | |
| Ethnicity | <0.001 | |||||
| Hispanic or Latino | 7298 (8.0%) | 2937 (8.5%) | 4361 (7.7%) | 4123 (7.8%) | 815 (7.7%) | |
| Not Hispanic or Latino | 63,113 (69.4%) | 22,787 (65.9%) | 40,326 (71.5%) | 37,966 (72.0%) | 7396 (70.2%) | |
| Unknown | 20,544 (22.6%) | 8832 (25.6%) | 11,712 (20.8%) | 10,610 (20.1%) | 2326 (22.1%) | |
| BMI | 26.2 ± 7.3 | 25.4 ± 7.4 | 26.6 ± 7.2 | 26.5 ± 7.2 | 27.8 ± 6.9 | <0.001 |
| Unknown | 59,812 | 23,054 | 36,758 | 34,482 | 6554 | |
| Pre-existing conditions | ||||||
| Eating disorder | 1943 (2.1%) | 1112 (3.2%) | 831 (1.5%) | 804 (1.5%) | 108 (1.0%) | <0.001 |
| Anxiety | 24,510 (26.9%) | 11,518 (33.3%) | 12,992 (23.0%) | 12,482 (23.7%) | 1945 (18.5%) | <0.001 |
| Obsessive Compulsive Disorder | 1586 (1.7%) | 820 (2.4%) | 766 (1.4%) | 731 (1.4%) | 115 (1.1%) | <0.001 |
| Type II Diabetes Mellitus | 3163 (3.5%) | 1580 (4.6%) | 1583 (2.8%) | 1511 (2.9%) | 224 (2.1%) | <0.001 |
| Body dysmorphic disorder | 167 (0.2%) | 92 (0.3%) | 75 (0.1%) | 71 (0.1%) | 9 (0.1%) | <0.001 |
| Depression | 10,216 (11.2%) | 4538 (13.1%) | 5678 (10.1%) | 5404 (10.3%) | 947 (9.0%) | <0.001 |
(± refers to 1 SD from the mean).
Nearly all patient data for transgender individuals ranged from 2016 to 2023, but data from TriNetX ranges from 2000 to 2023. In the case of individuals with unknown data, including sex assigned at birth, these individuals were excluded from the analysis. The missing data was only reported in the baseline characteristics (Table 1).
Of note, categorizing transgender and gender-diverse individuals into specific cohorts does not fully encompass the broad lived experiences of these individuals. For the purposes of this study, and to include as much of the gender spectrum as possible, we categorized those with a GID diagnosis with a male sex assigned at birth as transfeminine spectrum (TF) and those with a GID diagnosis with a female sex assigned at birth as transmasculine spectrum (TM). Nonbinary folks are still represented within our dataset; however, the terminology used in this paper may categorize them into either the transfeminine or transmasculine spectrum based on the type of GAMT received and in the case of no GAMT, based on their sex assigned at birth. We acknowledge that this does not fully encompass the non-binary and gender fluid experience and is thus a limitation of our study and the database used to conduct this research.
Statistical analysis
We examined baseline differences between groups using independent t-tests for continuous data and chi-square or Fisher’s exact test (as appropriate) for categorical data (presented as frequencies and percentages). To evaluate the risk of eating disorder outcomes between groups, we used Cox proportional hazards model with gender-affirming care as a time-varying covariate. The primary outcome was a new eating disorder diagnosis of any type. But, a particular analysis of AN, BN, and BED were also included. We tested the proportional hazards assumption using Schoenfeld individual test (cox.zph function in R), which resulted in non-significant p-value. To balance for possible confounding variables of the relationship between receiving gender-affirming care and being diagnosed with an eating disorder, we used inverse probability of treatment weighting (IPTW). Propensity scores for the probability of receiving gender-affirming care in each cohort were estimated by logistic regression with sex assigned at birth, age at gender dysphoria diagnosis, race, ethnicity, and prior diagnosis of eating disorders, diabetes, body dysmorphic disorder, and/or depression as predictors. The factors for the propensity score matching were decided upon by using Hambleton et al.’s article detailing the psychiatric and medical comorbidities of eating disorders25. Using these scores, we calculated stabilized inverse probability weights (balanced to absolute standardized mean differences <0.1. All analyses were performed using R statistical software version 4.2.1 (WeightIt and survival package) All tests were two-tailed with an alpha level of 0.05
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Baseline characteristics
We identified 90,955 TGD individuals. 56,399 (62%) of whom had some form of gender-affirming medical intervention (Any GAMT) and 34,556 (38%) who had no form of GAMT (Referred to as no intervention; NI) (Table 1). Among those who had any GAMT, we identified 52,699 (93%) that had gender-affirming hormone therapy (HT) and 10,537 (19%) who had gender-affirming surgical interventions (SX). Of note, patients in the HT or SX group may also have other forms of GAMT.
The baseline characteristics of the cohorts are described in Table 1. There were significant differences in prior eating disorder diagnoses, anxiety, obsessive-compulsive disorder, Type II diabetes mellitus, body dysmorphic disorder, and anxiety between GAMT, HT, and SX groups compared to NI.
Outcomes
Among transfeminine individuals (TF), those on HT had an increase in risk of being diagnosed with any new eating disorder compared to TF not receiving any gender-affirming medical intervention (NI) (HR:1.67, 95% CI:1.41, 1.98). We also found a specific increase in the risk of being diagnosed with Anorexia nervosa (HR:1.94, 95% CI:1.37, 2.74) compared to TFNI (Table 2). For the SX cohort, no significant difference in eating disorder diagnosis was observed compared to TFNI (Table 3).
Table 2.
HT vs NI Time-dependent Cox proportional hazards model on the outcome of a diagnosis of an eating disorder including Anorexia nervosa, Bulimia, Binge eating (analyzed as individual outcomes and as composite), among patients without any gender-affirming medical therapy (NI, reference group), to patients receiving hormone therapy (HT)
| Unweighted | Weighted | |||||
|---|---|---|---|---|---|---|
| Model | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| Outcome: Eating disorder (composite) | ||||||
| Transfeminine | 1.17 | 0.99, 1.38 | 0.06 | 1.67** | 1.41, 1.98 | <0.001 |
| Transmasculine | 0.57 | 0.53, 0.62 | <0.001 | 0.83** | 0.76, 0.90 | <0.001 |
| Outcome: Anorexia nervosa | ||||||
| Transfeminine | 1.41 | 1.00, 1.97 | 0.047 | 1.94** | 1.37, 2.74 | <0.001 |
| Transmasculine | 0.51 | 0.43, 0.60 | <0.001 | 0.73** | 0.62, 0.86 | <0.001 |
| Outcome: Bulimia | ||||||
| Transfeminine | 0.86 | 0.54, 1.37 | 0.525 | 1.18 | 0.73, 1.89 | 0.504 |
| Transmasculine | 0.66 | 0.51, 0.85 | 0.002 | 0.89 | 0.68, 1.17 | 0.423 |
| Outcome: Binge eating | ||||||
| Transfeminine | 1.45 | 0.84, 2.50 | 0.180 | 1.74 | 1.00, 3.02 | 0.051 |
| Transmasculine | 0.89 | 0.64, 1.23 | 0.471 | 1.13 | 0.81, 1.57 | 0.487 |
Result shown both before and after inverse probability treatment weighting.
Table 3.
SX vs NI
| Unweighted | Weighted | |||||
|---|---|---|---|---|---|---|
| Model | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| Outcome: Eating disorder (composite) | ||||||
| Transfeminine | 0.74 | 0.55, 1.00 | 0.047 | 1.31 | 0.91, 1.89 | 0.141 |
| Transmasculine | 0.37 | 0.31, 0.43 | <0.001 | 0.62** | 0.51, 0.75 | <0.001 |
| Outcome: Anorexia nervosa | ||||||
| Transfeminine | 0.41 | 0.18, 0.95 | 0.037 | 1.23 | 0.46, 3.31 | 0.684 |
| Transmasculine | 0.3 | 0.21, 0.41 | <0.001 | 0.44** | 0.31, 0.63 | <0.001 |
| Outcome: Bulimia | ||||||
| Transfeminine | 0.62 | 0.25, 1.57 | 0.315 | 1.14 | 0.43, 3.01 | 0.791 |
| Transmasculine | 0.55 | 0.35, 0.85 | 0.007 | 0.84 | 0.51, 1.38 | 0.496 |
| Outcome: Binge eating | ||||||
| Transfeminine | 1.01 | 0.41, 2.52 | 0.98 | 1.5 | 0.58, 3.90 | 0.402 |
| Transmasculine | 0.77 | 0.48, 1.25 | 0.296 | 1.01 | 0.59, 1.75 | 0.962 |
Time-dependent Cox proportional hazards model on the outcome of a diagnosis of an eating disorder including Anorexia nervosa, Bulimia, Binge eating (analyzed as individual outcomes and as composite), among patients without any gender-affirming medical therapy (NI; reference group), to patients receiving surgical intervention (SX). Result shown both before and after inverse probability treatment weighting.
** Significant.
Among transmasculine individuals (TM), those on HT had a decrease in risk of being diagnosed with an eating disorder (HR: 0.83, 95% CI: 0.76, 0.90) and a decrease in risk of being diagnosed with Anorexia nervosa (HR:0.73, 95% CI:0.62, 0.86) compared to TMNI (Table 2). Unlike TFSX, for the TMSX cohort, we did observe a decrease in risk of being diagnosed with an eating disorder (HR: 0.62, 95% CI: 0.51, 0.75) and a decrease in risk of being diagnosed with Anorexia nervosa (HR: 0.44, 95% CI: 0.31, 0.63) compared to TMNI (Table 3).
Data from Tables 2 and 3 are depicted in Fig. 1.
Fig. 1. Forest plot depictions of eating disorder diagnosis risk in gender-affirming therapy groups.
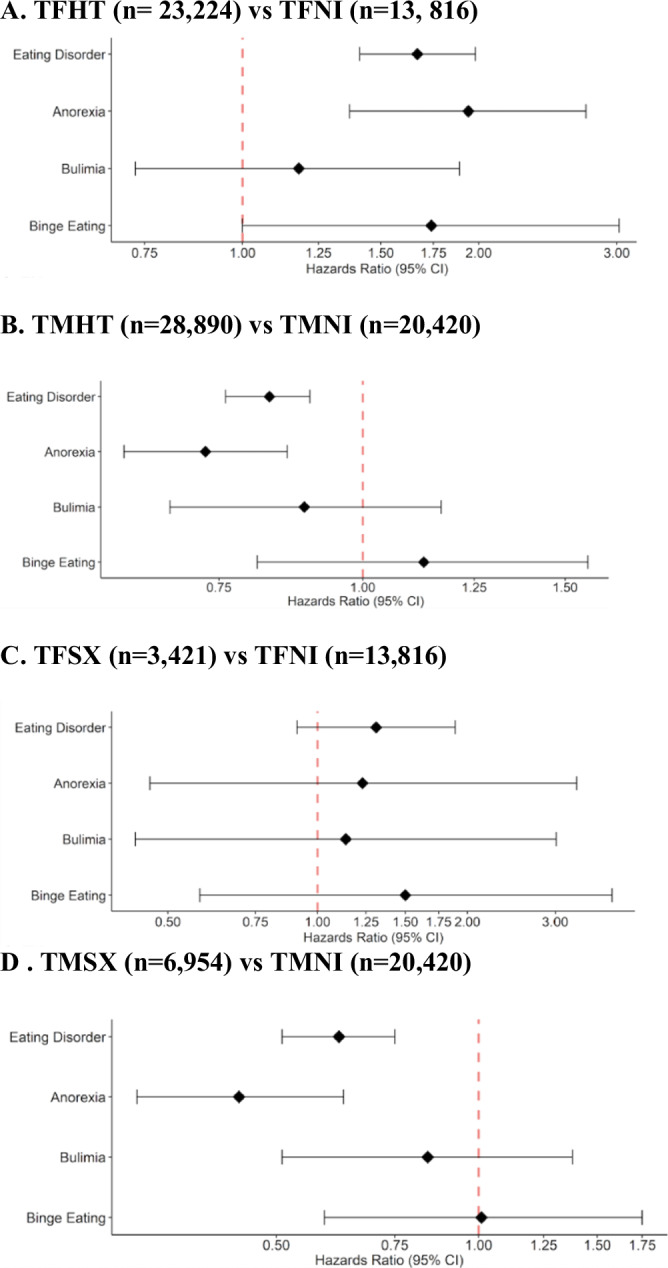
Hazard ratios and 95% confidence intervals are shown for the risk of eating disorder diagnoses (composite outcome [Eating Disorder], anorexia nervosa, bulimia, and binge eating). Results are based on time-dependent Cox proportional hazards models comparing after inverse probability treatment weighting: A transfeminine patients receiving hormone therapy (TFHT) vs. those not receiving therapy (TFNI); B transmasculine patients receiving hormone therapy (TMHT) vs. those not receiving therapy (TMNI); C transfeminine patients undergoing surgery (TFSX) vs. those not receiving therapy (TFNI); and D transmasculine patients undergoing surgery (TMSX) vs. those not receiving therapy (TMNI). Sample size for each comparison is noted in panel titles.
Discussion
Evidence supports that eating disorder risk is greater among TGD populations relative to cisgender counterparts11,12. Many of these articles have suggested that minority stress factors due to anti-trans discrimination in school, employment, or housing may contribute strongly to the development of eating disorders26. Additionally, other social factors such as food insecurity have been implicated in eating disorder development. TGD individuals have high rates of food insecurity which can often lead to periods of disordered eating based on food scarcity or availability27. Linsenmeyer et al. found that on average TGD individuals had twice the rate of food insecurity compared to the national average and that TGD individuals with prior EDs further increased the rates of current food insecurity28. While the risk of eating disorders may be elevated in the TGD community, several studies have also shown an improvement in symptoms of an eating disorder upon undergoing gender-affirming interventions6,18–20. However, little work has been done to explore how gender-affirming medical therapy (GAMT) may modulate the risk of being diagnosed with an eating disorder. In this study, we examined how the risk of new eating disorder diagnoses among TGD individuals changed with gender-affirming hormone and surgical interventions.
We found that transfeminine (TF) individuals on hormone therapy (HT) had a higher risk and transmasculine (TM) individuals on HT had a decreased risk of being diagnosed with an eating disorder compared to TFNI and TMNI, respectively, with Anorexia Nervosa being the most significant contributor in both groups. When considering the SX group, no statistically significant difference was seen between TFSX and TFNI, but a significant decrease was seen between TMSX and TMNI, again with Anorexia Nervosa being the main contributor.
Eating disorders represent a critical public health concern especially among women; it is well established that being a cisgender woman, compared to a cisgender man, increases your risk for being diagnosed with an eating disorder29. Interestingly, we found that transfeminine individuals experienced an increase in the risk of being diagnosed with eating disorders after undergoing HT. Furthermore, transmasculine individuals experienced a decrease in risk of a new eating disorder diagnosis after HT or SX.
We propose five possible explanations for the observed data: gendered body standards, BMI cutoffs for gender-affirming surgery, provider biases, effects of hormone therapy, and ascertainment bias. It is important to consider that none of these explanations are mutually exclusive, as multiple factors may influence the risk of being diagnosed with an eating disorder.
Explanation #1: Gendered body standards
One possible explanation for our observed results is that TGD individuals who medically and surgically transition may feel pressured to conform to gendered body standards. It is well established that body image plays a crucial role in the development of eating disorders, and it is influenced in part by sociocultural ideals of beauty. In general, western-centric body ideals are binary and emphasize muscularity for cisgender men and thinness for cisgender women30–33. Studies have shown that striving to conform to these gendered ideals of body ideals and beauty may be associated with the onset and perpetuation of eating disorder symptoms34–36. However, TGD individuals may be extremely susceptible to these gendered norms for several reasons. First, some TGD individuals, may feel pressure to live up to cis-centric western binary concepts of masculine or feminine ideals of beauty or desirability5. Second, many TGD individuals may feel highly pressured to conform to gendered body standards so they can “pass” and navigate the world safely —“Passing” for TGD individuals is defined as being perceived by others in the world as your identified gender. Passing has been highly correlated with increased safety for TGD individuals. Peixoto et al. found that among TGD individuals who deemed themselves as passing well in society had an 81% lower chance of suffering physical violence in open public spaces compared to TGD counterparts who deemed themselves as not passing37.
With this strong concern for physical safety, TGD individuals may be extremely compelled to conform to western gendered body ideals so they may “pass” and achieve this feeling of safety. Therefore, with thinness being a western centric ideal of female beauty, this might encourage calorie restriction in some transfeminine individuals. Conversely, transmasculine individuals may display less restrictive eating symptomatology due to western masculine ideals of larger, more muscular bodies. Nevertheless, these conclusions are not always applicable to the experience of all individuals. Several qualitative studies suggest that some transfeminine individuals will increase their caloric intake to create the appearance of curves while transmasculine individuals may focus on decreasing fat in chest and hip area to attain a more defined physical appearance13,38.
Explanation #2: BMI cutoffs for gender-affirming surgery
Another possible explanation for these findings may be the influence of BMI cutoffs, which are often set as prerequisites for gender-affirming surgery. The World Professional Association for Transgender Health does not detail a BMI requirement for gender-affirming surgery39. Nevertheless, many gender-affirming surgical centers still use BMI cutoffs for surgery which may preclude some trans patients from accessing gender-affirming surgery40–43. Thus, surgical transition may be a particularly vulnerable period of risk for ED symptomatology development among all TGD patients regardless of their sex assigned at birth because some patients may feel pressured to lower their BMI to meet surgical criteria or to lower their risk of complications35,40. However, it has been reported that rates of obesity are nearly double among transmasculine individuals compared to transfeminine individuals44. Thus, the pressures to lose weight, and consequently the increase in ED symptomatology development, may be more prominent among transmasculine individuals. Our data contradicts this notion, as the risk of being diagnosed with an ED decreased among transmasculine individuals, making this explanation less plausible.
Explanation #3: Provider biases
Furthermore, providers who may be screening for eating disorders may be affected by their gendered stereotypical expectations of what populations are at risk of developing an eating disorder. In focus group interviews from35, TGD individuals reported that unless they were cis and white women presenting, they felt like their concern for having an eating disorder was not taken seriously by providers. Therefore in our results, TFHT, who may be more feminine presenting, may be more likely to be screened for ED than TMHT. These findings for TF individuals may be further supported by the baseline statistics for the medical therapy groups, which had a higher proportion of Caucasian individuals, more closely resembling stereotypical perceptions of demographic groups most at risk for eating disorders.
Explanation #4: Effect of hormone therapy
The observed results may also be due to the physical effects of gender-affirming hormone therapy on body composition. Estrogen use is well correlated with gaining weight, while testosterone is associated with an increase in muscularity, and decreased body fat percentage44. These rapid changes in body composition may then lead to differences in the rates of restrictive eating disorders, such as anorexia nervosa. Conversely, transfeminine individuals may increase dietary restriction preemptively when beginning estrogen due to fear of weight gain as a side effect. However, these correlations remain unclear as much prior research has suggested that those on HT have alleviated ED symptoms20.
Explanation #5: Ascertainment bias
It may also be possible that rates of eating disorders among TGD without any intervention may be lower in the TriNetX dataset than in the actual population. TGD individuals might not seek medical care for their eating disorder directly due to fear of not being taken seriously or being discriminated against. However, it is more likely that they may go to a physician for gender-affirming care. Thus, if a person cannot or does not want to undergo GAMT, they might not seek medical care for their eating disorder thereby lowering the rates of eating disorder diagnosis among the TGD NI cohort.
Moving forward
These findings highlight the need for gender-affirming care teams who, in collaboration with the transgender community, investigate and research the development of an ED within this population. This care team should consist of gender-affirming health care providers, including physicians, psychologists, social workers, registered dietitians, and clinical researchers with expertise in ED.. These teams should view the relationship between having a gender-diverse identity and an eating disorder from a multifactorial perspective. First, these care teams should ensure that these individuals are able to access food and attain a balanced nutrition. Second, they should assess their barriers to accessing gender-affirming care, since the absence of this care can lead to disordered eating in an attempt to control body shape and weight as a gender-affirming practice and/or safety practice45,46. Third, these teams should continue implementing anti-discriminatory and inclusive policies within their healthcare institutions, so that transgender people can approach their health care providers with their health concerns without fear. Finally, these teams should help influence a wider public health policy that advocates for the right of transgender people to self-determination in light of the recent bans on gender-affirming care in several states across the United States47.
Strengths and limitations
Several limitations of our study must be acknowledged. Healthcare access disparities among TGD populations may contribute to an underrepresentation of certain covariates and outcomes. Though TriNetX offers a field denoting sex assigned at birth, an individual’s identified gender may have been reported instead. Since sex assigned at birth carries a higher weight biologically when it comes to medical decisions, we believe most EMR systems still register patients with their sex assigned at birth. Furthermore, while our identification codes for TGD patients display high specificity, their sensitivity is somewhat lower22–24. This indicates that it is likely we may not have captured the entirety of the TGD population. Transgender individuals with an F64 diagnosis code may under-represent the entire trans population because some individuals may choose not to pursue medical documentation. Our study also relies on a sequentiality of medical record coding, requiring a GID diagnosis prior to an ED diagnosis. In the real world, for example, individuals may present for care and obtain a new ED diagnosis and then later receive a diagnosis of GID in their medical records despite having transitioned at the time of ED diagnosis. Lastly, our analysis focused on the three most prevalent eating disorders in TriNetX (Anorexia Nervosa, Bulimia, and Binge Eating Disorder), we did not explore how other eating disorders, such as EDNOS and OSFED, may be connected to gender identities and the gender-affirmation journey.
Despite these limitations, our study has several key strengths. Firstly, the size of our cohort, larger than any prior investigation, lends weight to our findings. Our dataset offers a wide geographical and racial diversity, which contributes to a more representative understanding that may be difficult to capture in other studies. Additionally, our methodology provides the capacity to control for an array of potential confounders, enhancing our analysis of gender-affirming therapy and eating disorder diagnosis risk among TGD individuals.
Future research
Future studies may stratify findings by race and ethnicity to further understand the intersections with gender identity, how this may influence access to care, and the importance of financial/economic resources. As well, future research can focus on TGD individual’s experience of gendered social norms and explore how their experiences may affect their eating habits and relationship with their body while they transition. Moving to a broader scale view, we implore future researchers to examine the multitude of systematic factors that may influence eating disorder presentations among TGD individuals. Of particular note, these researchers are interested in examining the driving factors of societal gender norms, such as digital media, that may affect the TGD population’s experience of gender affirmation.
Conclusion
This study used a large database to assess the risk of being diagnosed with an eating disorder among TGD individuals on GAMT. Overall, we report that during the gender-affirmation journey, transfeminine individuals experience an increased risk of being diagnosed with an eating disorder, while transmasculine individuals experience a decreased risk. For both groups, the risk of being diagnosed with AN was the most significant. Our results may be explained by a variety of factors including: GAMT may alter individuals’ pressure to conform to gendered societal norms, provider archetypes of who develop eating disorders may affect screening rates, physiological side effects of HT may affect ED symptomatology, and TGD interactions with the healthcare system may lead to an ascertainment bias.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
Funding/Support: This publication was made possible through the support of the Clinical Research Center of University Hospitals Cleveland Medical Center (UHCMC) and the Case Western Reserve University Clinical and Translational Science Collaborative (CTSC) 4UL1TR000439. We acknowledge the partial support provided to the senior author, Dr. Swagata Banik, through funding from the U.S. Department of Education (Grant #P116Z220103).
Glossary
- GID
Gender Identity Disorder
- Transgender and gender diverse or TGD
Those whose gender identity does not align with their sex assigned at birth.
- Transfeminine spectrum or TF
Those whose sex assigned at birth is male but identify as a woman or on the feminine spectrum
- Transmasculiune spectrum or TM
Those whose sex assigned at birth is female but identify as a man or on the masculine spectrum
- GAMT
Gender Affirming Medical Therapy
- NI
No Gender Affirming Medical Treatment Intervention
- HT
Gender Affirming Hormone Therapy
- SX
Gender Affirming Surgical Intervention
- ED
Eating Disorder
Author contributions
ML and TT led the project, were the primary authors for the manuscript, and were involved in all aspect of manuscript development. EF aided in conceptualization of the project and methodical design. J. Perez was the primary data analyst. EF, CC, JA, J.Palozzi aided in interpretation of the data and manuscript writing. MM, SG, KM provided supervision and manuscript editing. SB was the primary supervisor. All authors read and approved the final manuscript.
Peer review
Peer review information
Communications Medicine thanks Whitney Linsenmeyer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Data availability
All data from this manuscript comes from de-identified data from the TriNetX platform. The data used in Fig. 1 is included within Tables 2 and 3. The data that support the findings of this study are available from TriNetX but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Due to data privacy restrictions in the User Data Agreement between University Hospitals and TriNetX, individual patient-level data will not be shared publicly, but aggregated and de-identified data may be available upon request for qualified researchers, with proper citation of the TriNetX network in all publications. Those interested in accessing the data should contact the corresponding author of this manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Matthew Loria, Tomasz Tabernacki.
Supplementary information
The online version contains supplementary material available at 10.1038/s43856-024-00704-7.
References
- 1.Ward, Z. J., Rodriguez, P., Wright, D. R., Austin, S. B. & Long, M. W. Estimation of eating disorders prevalence by age and associations with mortality in a simulated nationally representative US Cohort. JAMA Netw. Open2, e1912925 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galmiche, Marie et al. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am. J. Clin. Nutr.109, 1402–1413 (2019). [DOI] [PubMed] [Google Scholar]
- 3.Gordon, A. R., Austin, S. B., Krieger, N., Hughto, J. M. W. & Reisner, S. L. “I have to constantly prove to myself, to people, that I fit the bill”: Perspectives on weight and shape control behaviors among low-income, ethnically diverse young transgender women. Soc. Sci. Med.165, 141–149 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barakat, Sarah et al. Risk factors for eating disorders: findings from a rapid review. J. Eat. Disord.11, 17 (2023). Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parker, L. L. & Harriger, J. A. Eating disorders and disordered eating behaviors in the LGBT population: a review of the literature. J. Eat. Disord.8, 1–20 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riddle, M. C. & Safer, J. D. Medical considerations in the care of transgender and gender diverse patients with eating disorders. J. Eat. Disord.10, 178 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell, L., Viswanadhan, K., Lois, B. & Dundas, M. Emerging evidence: a systematic literature review of disordered eating among transgender and nonbinary youth. J. Adolesc. Health.74, 18–27 (2024). [DOI] [PubMed] [Google Scholar]
- 8.Rasmussen, S. M. et al. Eating disorder symptomatology among transgender individuals: a systematic review and meta-analysis. J. Eat. Disord.11, 84 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heiden-Rootes, K., Linsenmeyer, W., Levine, S., Oliveras, M. & Joseph, M. A scoping review of the research literature on eating and body image for transgender and nonbinary adults. J. Eat. Disord.11, 111 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diemer, E. W., Grant, J. D., Munn-Chernoff, M. A., Patterson, D. A. & Duncan, A. E. Gender identity, sexual orientation, and eating-related pathology in a national sample of college students. J. Adolesc. Health57, 144–149 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grammer, A. C. et al. Characterizing eating disorder diagnosis and related outcomes by sexual orientation and gender identity in a national sample of college students. Eat. Behav.42, 101528 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coelho, JenniferS. et al. Eating disorder diagnoses and symptom presentation in transgender youth: a scoping review. Curr. Psychiatry Rep.21, 107 (2019). [DOI] [PubMed] [Google Scholar]
- 13.Nagata, J. M., Ganson, K. T. & Austin, S. B. Emerging trends in eating disorders among sexual and gender minorities. Curr. Opin. Psychiatry33, 562–567 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ålgars, M., Alanko, K., Santtila, P. & Sandnabba, N. K. Disordered eating and gender identity disorder: a qualitative study. Eat. Disord.20, 300–311 (2012). [DOI] [PubMed] [Google Scholar]
- 15.Couturier, J., Pindiprolu, B., Findlay, S. & Johnson, N. Anorexia nervosa and gender dysphoria in two adolescents. Int J. Eat. Disord.48, 151–155 (2015). [DOI] [PubMed] [Google Scholar]
- 16.Ewan, L. A., Middleman, A. B. & Feldmann, J. Treatment of anorexia nervosa in the context of transsexuality: a case report. Int J. Eat. Disord.47, 112–115 (2014). [DOI] [PubMed] [Google Scholar]
- 17.Ristori, J. et al. Gender dysphoria and anorexia nervosa symptoms in two adolescents. Arch. Sex. Behav.48, 1625–1631 (2019). [DOI] [PubMed] [Google Scholar]
- 18.Tordoff, D. M. et al. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Netw. Open5, e220978 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Testa, RylanJ. et al. Gender confirming medical interventions and eating disorder symptoms among transgender individuals. Health Psychol.36, 927–936 (2017). [DOI] [PubMed] [Google Scholar]
- 20.Nowaskie, D. Z., Filipowicz, A. T., Choi, Y. & Fogel, J. M. Eating disorder symptomatology in transgender patients: differences across gender identity and gender affirmation. Int. J. Eat. Disord.54, 1493–1499 (2021). [DOI] [PubMed] [Google Scholar]
- 21.Jones, B. A., Haycraft, E., Murjan, S. & Arcelus, J. Body dissatisfaction and disordered eating in trans people: A systematic review of the literature. Int. Rev. psychiatry (Abingdon, Engl.)28, 81–94 (2016). [DOI] [PubMed] [Google Scholar]
- 22.Nik-Ahd, F. et al. Seeing the unseen: how can we best identify transgender women within the Veterans Affairs healthcare system’s electronic medical record? J. Sex. Med.20, 559–567 (2023). [DOI] [PubMed] [Google Scholar]
- 23.Rich, A. J. et al. Development of a computable phenotype to identify a transgender sample for health research purposes: a feasibility study in a large linked provincial healthcare administrative cohort in British Columbia, Canada. BMJ Open11, e040928 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Proctor, K., Haffer, S. C., Ewald, E., Hodge, C. & James, C. V. Identifying the transgender population in the medicare program. Transgend Health1, 250–265 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hambleton, A. et al. Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature. J. Eat. Disord.10, 132 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muratore, LauraA., Flentje, Annesa, Schuster, David & Capriotti, MatthewR. Disordered eating and body dissatisfaction in transgender and gender-expansive adults: an evaluation and integration of the gender minority stress and resilience and tripartite influence models. Behav. Ther.53, 869–886 (2022). [DOI] [PubMed] [Google Scholar]
- 27.Russomanno, J., Patterson, J. G. & Jabson, J. M. Food insecurity among transgender and gender nonconforming individuals in the Southeast United States: a qualitative study. Transgender health4, 89–99 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linsenmeyer, W. R. et al. Disordered eating, food insecurity, and weight status among transgender and gender nonbinary youth and young adults: a cross-sectional study using a nutrition screening protocol. LGBT health8, 359–366 (2021). [DOI] [PubMed] [Google Scholar]
- 29.Striegel-Moore, R. H. et al. Gender difference in the prevalence of eating disorder symptoms. Int. J. Eat. Disord.42, 471–474 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murray, S. B. et al. The enigma of male eating disorders: a critical review and synthesis. Clin. Psychol. Rev.57, 1–11 (2017). [DOI] [PubMed] [Google Scholar]
- 31.Lavender, J. M., Brown, T. A. & Murray, S. B. Men, muscles, and eating disorders: An overview of traditional and muscularity-oriented disordered eating. Curr. Psychiatry Rep.19, 32 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Franceschini, A. & Fattore, L. Gender-specific approach in psychiatric diseases: Because sex matters. Eur. J. Pharmacol.896, 173895 (2021). [DOI] [PubMed] [Google Scholar]
- 33.Aparicio-Martinez, P. et al. Social media, thin-ideal, body dissatisfaction and disordered eating attitudes: An exploratory analysis. Int. J. Environ. Res. Public Health16, 4177 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiotsa, B., Naccache, B., Duval, M., Rocher, B. & Grall-Bronnec, M. Social media use and body image disorders: Association between frequency of comparing one’s own physical appearance to that of people being followed on social media and body dissatisfaction and drive for thinness. Int. J. Environ. Res. Public Health18, 2880 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hartman-Munick, S. M. et al. Eating disorder screening and treatment experiences in transgender and gender diverse young adults. Eat. Behav.41, 101517 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Romito, M. et al. Exploring transgender adolescents’ body image concerns and disordered eating: semi-structured interviews with nine gender minority youth. Body Image37, 50–62 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peixoto, E. M. et al. Interpersonal violence and passing: results from a Brazilian trans-specific cross-sectional study. J. Interpers. Violence37, NP14397–NP14410 (2022). [DOI] [PubMed] [Google Scholar]
- 38.Nagata, J. M. et al. Community norms for the eating disorder examination questionnaire (EDE-Q) among transgender men and women. Eat. Behav.37, 101381 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Coleman, E. et al. The standards of care of the world professional association for transgender health. 7th version Int. J. Transgenderism13, 165–232 (2011). [Google Scholar]
- 40.Brownstone, L. M., DeRieux, J., Kelly, D. A., Sumlin, L. J. & Gaudiani, J. L. Body mass index requirements for gender-affirming surgeries are not empirically based. Transgender Health6, 121–124 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uniacke, B., Glasofer, D., Devlin, M., Bockting, W. & Attia, E. Predictors of eating-related psychopathology in transgender and gender nonbinary individuals. Eat. Behav.42, 101527 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shin, S. J., Kumar, A. & Safer, J. D. Gender-affirming surgery: perioperative medical care. Endocr. Pract.28, 420–424 (2022). [DOI] [PubMed] [Google Scholar]
- 43.Ives, G. C. et al. Evaluation of BMI as a risk factor for complications following gender-affirming penile inversion vaginoplasty. Plast. Reconstructive Surg.7, e2097 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kyinn, M. et al. Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy. Int J. Obes.45, 2562–2569 (2021). [DOI] [PubMed] [Google Scholar]
- 45.Patterson, C., Sepúlveda, M.-J. & White, J. Understanding the Well-being of LGBTQI+ Populations (The National Academies Press, 2020). [PubMed]
- 46.McGregor, K. et al. Disordered eating and considerations for the transgender community: a review of the literature and clinical guidance for assessment and treatment. J. Eat. Disord.11, 1–12 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reisner, S. L. et al. Global health burden and needs of transgender populations: a review. Lancet388, 412–436 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
All data from this manuscript comes from de-identified data from the TriNetX platform. The data used in Fig. 1 is included within Tables 2 and 3. The data that support the findings of this study are available from TriNetX but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Due to data privacy restrictions in the User Data Agreement between University Hospitals and TriNetX, individual patient-level data will not be shared publicly, but aggregated and de-identified data may be available upon request for qualified researchers, with proper citation of the TriNetX network in all publications. Those interested in accessing the data should contact the corresponding author of this manuscript.


