Ehlers–Danlos syndrome type IV can escape diagnosis until the development of catastrophic complications in adult life.
CASE HISTORY
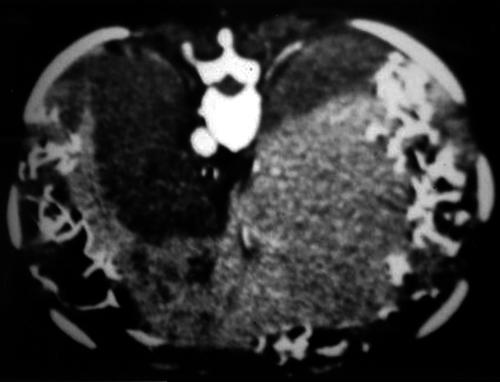
A Pakistani woman aged 23 years experienced sudden chest pain and dyspnoea five days after caesarean section. Physical examination, chest radiography and arterial blood gas measurements showed nothing abnormal. She was anti-coagulated for risk of thromboembolic disease. Six hours later she reported right subscapular pain; her abdomen was now tense. Haemoglobin was 6.2 g/dL, platelets 119 × 109/L, bilirubin 45 μmol/L, alanine aminotransferase 102 iu/L, alkaline phosphatase 657 iu/L; prothrombin time was normal. An abdominal tap yielded frank blood and emergency laparotomy revealed a large subcapsular liver haematoma (no known antecedent trauma). Initial packing of the liver did not control the bleeding and she required a second laparotomy by a liver surgeon. On day two she was stable enough to allow transfer to our liver intensive care unit. Biphasic liver CT (Figure 1) showed tightly packed liver with abnormal perfusion of the parenchyma and intrahepatic haematomas. Bilateral spontaneous pneumothoraces then developed, requiring chest drains. During further laparotomy there was uncontrolled bleeding from the liver, because of complete decapsulation. Abnormal fragility of the bowel and mesentery was noted. Thought was given to total hepatectomy with portocaval shunt and listing for transplantation, but the tissues were considered unsuitable for successful transplantation and further efforts were concentrated on achieving haemostasis. She became profoundly hypotensive and had an asystolic cardiac arrest. After cardiac massage, the suprahepatic inferior vena cava was found to have completely avulsed from her liver. Further resuscitation efforts were unsuccessful.
Figure 1.
Biphasic CT scan indicating bilobar liver haematoma
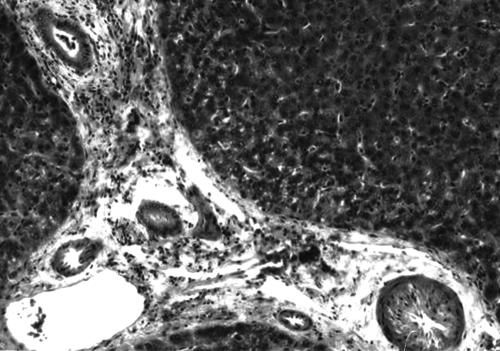
A liver specimen taken at operation (Figure 2) showed patchy fibrointimal hyperplasia of hepatic arterioles with smooth muscle and elastic-tissue hypertrophy, consistent with a connective tissue disorder. The patient's medical history was likewise suggestive. She had been born with bilateral club foot and contractures of her hand and had been registered handicapped with retarded motor delay at a young age. She had had several operations for hearing loss and had been seen by an ophthalmologist on account of her prominent globes and poor closure of her eyelids. There was no family history of note except for a brother with transposition of the great vessels who had undergone heart transplantation at age 18; there was no evidence of collagen disorder in his case and he is currently well. The patient was a primigravida and her pregnancy had been unremarkable. During her caesarean section the fat was noted to be friable and the tissues exceptionally soft. The findings and the medical history led us to diagnose Ehlers–Danlos syndrome (EDS) type IV. Confirmation will require culture of fibroblasts, to detect abnormal collagen production, and mutation analysis.
Figure 2.
Liver biopsy showing fibrointimal hyperplasia and smooth muscle hypertrophy
COMMENT
Spontaneous hepatic rupture, which is most often associated with a liver tumour together with coagulopathy,1 is not a common feature of EDS.2 The abnormality in EDS type IV is a defect of the collagen most abundant in the skin, blood vessels and gastrointestinal tract—namely, type III.3 Affected patients who undergo surgery are at risk of postoperative arterial rupture, perhaps because surgical trauma increases collagenase activity.4 In childhood, complications are rare but a quarter of patients have their first complication by age 20 and more than three-quarters by age 40. The risk of lethal complications in EDS type IV seems to be augmented by pregnancy, and is especially high during labour and early postpartum. In the largest survey of 'classic' EDS type IV, fatal pregnancy-related complications developed in 9–15% of women who became pregnant;5 therefore, the desirability of conception must be considered. Because the syndrome is inherited in autosomal dominant fashion genetic screening is important, and in the family discussed here all five of the patient's siblings are being tested. In the mother and sister, both of whom have a history of easy bruising, tests have already shown fibroblasts to be free from a collagen III defect. The child will need to be tested.
This case illustrates the difficulties in early diagnosis of EDS type IV. Surgeons who encounter extreme tissue fragility at operation should think of connective tissue disorder. Although no specific therapies delay the onset of complications in these patients, awareness of the clinical signs and knowledge of the diagnosis may influence reproductive counselling, the management of pregnancy and surgical interventions.
References
- 1.Chen ZY, Qi QH, Dong ZL. Etiology and management of haemorrhage in spontaneous liver rupture: a report of 70 cases. World J Gastroenterol 2002;8: 1063-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mistry BM, Solomon H, Garvin P, et al. Spontaneous rupture of the liver upon revascularization during transplantation. Transplantation 2000;69: 2214-18 [DOI] [PubMed] [Google Scholar]
- 3.Tucker L. Heritable disorders of connective tissue and disability and chronic disease in childhood. Curr Opin Rheumatol 1992;4: 731-40 [PubMed] [Google Scholar]
- 4.Barabas AP. Ehlers–Danlos syndrome type IV. N Engl J Med 2000;343: 366. [DOI] [PubMed] [Google Scholar]
- 5.Pepin M, Schwarze U, Superti-Furga A, et al. Clinical and genetic features of Ehlers–Danlos type IV, the vascular type. N Engl J Med 2000;342: 673-80 [DOI] [PubMed] [Google Scholar]