Abstract
Background
Orthodontic treatment involves manipulation of tooth position that can temporarily lead to occlusal interferences capable of inducing bruxism. The objectives of this study were to determine the self-reported incidence of bruxism and its association with factors such as facial type, divergence, skeletal and dental malocclusions in orthodontic patients.
Materials and methods
80 patients who underwent a minimum of six months of orthodontic treatment were surveyed using a validated self-reported bruxism questionnaire for the presence or absence of bruxism. Data regarding patients’ facial type, divergence, skeletal and dental malocclusions were measured and collected from the patients’ orthodontic records. Binomial logistic regression analysis was used to assess the association of these factors with bruxism.
Results
About 45% of the orthodontic patients reported bruxism after the commencement of orthodontic treatment. The median age of the sample was 19.8 (17.7, 24.3) years and 60% of them were women. Binomial logistic regression analysis showed an insignificant association of gender and age with bruxism. When analyzing the association with facial type, divergence, skeletal and dental malocclusion no statistically significant association was found. However, patients with hypodivergent face [odds ratio (OR) = 2.4; 95% confidence interval (CI) = 0.7–8.5] and dental class III [OR = 4.0; 95% CI = 0.3–51.0] were more likely to report bruxism after the initiation of orthodontic treatment. A statistically significant association was found with jaw fatigue or soreness upon awakening (28.7%), clenching (27.5%) and grinding (25%) in the bruxism group (p-value ≤ 0.001). Teeth and gum soreness were also significantly associated with bruxism, affecting 25% of the orthodontic patients (p-value ≤ 0.001). On the contrary, nocturnal grinding (10%) and temporal headaches (21.3%) were negatively correlated with bruxism.
Conclusions
There is a risk of bruxism among orthodontic patients, with 45% of them reporting bruxism following the initiation of treatment. Patients with bruxism commonly reported jaw fatigue or soreness upon awakening, clenching, grinding, teeth and gum soreness. Factors such as facial type, facial divergence, skeletal and dental malocclusions have no impact on the onset of bruxism during orthodontic treatment.
Keywords: Bruxism, Orthodontics, Fixed appliance, Malocclusion, Oral habit
Introduction
Bruxism is the repetitive masticatory muscle activity characterized by clenching/grinding of the teeth. It may also be associated with bracing or thrusting of the mandible when awake or asleep [1]. Bruxism leads to hypertrophy of masticatory muscles, tooth surface loss due to attrition and hypersensitive or painful teeth [2]. It may also cause fracture of teeth, loss of restorations and periodontal support of teeth. Previously considered a pathological phenomenon, bruxism is now thought to be a physiological or protective mechanism [3]. It has been established that bruxism is multifactorial in nature and can be caused not only by morphological factors, i.e., occlusal discrepancies and jaw anatomy but also due to pathophysiological and psychosocial factors [4].
An established relationship exists between musculoskeletal disorders, bruxism and tooth wear. Tay et al. [5] found a high prevalence of teeth grinding (38.11%) and possible sleep bruxism (4.72%) in adult Asian population, negatively affecting the quality of life. Wetselaar et al. [6] reported sleep bruxism (16.5%) to be a common condition in Dutch adult population while awake bruxism (5%) was comparatively rarer. Toyama et al. [7] found in their study that bruxism can be a causal factor in the development of malocclusion, particularly crowding. In contrast, orthodontic interventions such as fixed appliances and expanders have been reported to help in the reduction of self-reported bruxism [8–10]. Therefore, a multidisciplinary approach to its diagnosis and treatment is necessary [8].
Orthodontic treatment entails the arrangement of tooth position, alignment and leveling. The process of occlusal adjustments can temporarily lead to occlusal interferences. These interferences can trigger bruxism in orthodontic patients and lead to temporomandibular joint disorders [11, 12]. Moreover, the experience of undergoing orthodontic treatment can be emotionally challenging to some patients as they may feel self-conscious about their appearance, experience discomfort during adjustments, or worry about the success of the treatment [13]. These psychological factors may contribute to the development of bruxism in orthodontic patients [14].
Orthodontic patients often have a variety of malocclusions, which might increase the chances of developing bruxism [15–17]. Patients undergoing orthodontic treatment present with different skeletal and dental malocclusions, facial types and divergence [17]. Understanding the reason behind the occurrence of bruxism and identifying the associated risk factors is essential for orthodontists to effectively manage and mitigate the potential negative effects. Furthermore, it is essential to educate the patients beforehand to prevent the development of any side effects due to bruxism. Pereira et al. [9] reported an increased frequency of bruxism in patients undergoing fixed mechanotherapy. Whereas, Hirsch [15]. reported a decrease in bruxism activity in such patients. Souza et al. [18] in their study found that bruxism and its clinical features differed among different facial types. However, there remains a gap in the literature regarding the incidence of bruxism in patients undergoing orthodontic treatment. Assessing the role of orthodontic intervention in the onset of bruxism among patients who previously exhibited no signs of bruxism, TMJ disorders or functional occlusal shifts is crucial. This is particularly important given the widely accepted belief that orthodontic treatment plays a role in alleviating rather than contributing to the development of bruxism. Similarly, its association with facial type, divergence, skeletal and dental malocclusion in patients undergoing orthodontic treatment warrants further discussion and exploration. Therefore, the primary objective of our study was to determine the incidence of self-reported bruxism six months after the initiation of orthodontic treatment and the secondary objective was to assess the association of different skeletal and dental malocclusions, facial types and divergences with increased tendency towards bruxism during orthodontic treatment.
Materials & methods
After obtaining approval from the Ethical Review Committee (2023–9103-26467), a cross-sectional study was conducted at a tertiary care hospital. Sample size calculation was carried out with Open-epi software by using the findings of Hirsch [15]. who reported the frequency of self-reported bruxism in orthodontic patients as 8.4%. Keeping α as 0.05, the power of the study as 80% and the confidence level at 95%, a sample of 80 subjects was required to conduct this study.
We included orthodontic patients aged between 13 to 45 years who underwent at least six months of orthodontic treatment and those who signed the consent form. Subjects with a previous history of any orthopedic or orthodontic treatment, presence of any craniofacial syndromes or dental anomaly, any temporomandibular joint disorder, history of bruxism, anxiety or stress disorder, history of trauma, patients taking medication that may cause bruxism and patients with uncontrolled periodontal disease were excluded from the study.
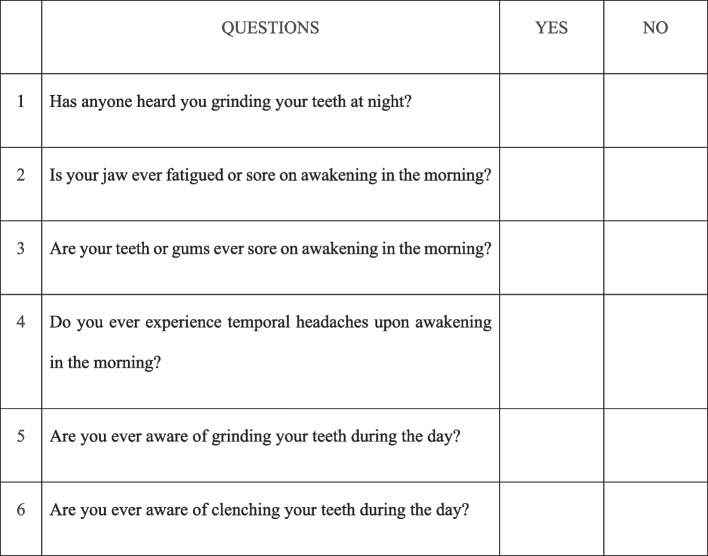
After obtaining written informed consent, from all the patients participating in the study and in case of patients younger than 18 years assent from the child and parental consent from the parents, patients visiting the orthodontic clinics at Aga Khan University Hospital were recruited in the study. They were asked to fill out a validated questionnaire from the study of Pintado et al. [19]. consisting of six questions assessing the presence or absence of bruxism. The questionnaire was explained to each participant by the investigator to ensure consistent understanding across all participants. The concept of bruxism and differences between clenching and grinding were thoroughly explained to each participant. Those patients who responded affirmatively to two out of six questions were categorized as bruxers (Fig. 1) [19]. In addition to determining the self-reported bruxism, this questionnaire was also used to conduct a secondary analysis on the relationship between specific questionnaire responses and bruxism status. Participants’ age and gender were recorded along with facial type judged by the facial index (FI) which was determined using a digital vernier caliper [20]. The facial index was calculated using the following formula:
Fig. 1.
Questionnaire
Where N = Nasion, Gn = Gnathion and ZA = Zygomatic arch.
The FI classified the face of the patient as, dolichofacial (FI = 90–94.9%), brachyfacial (FI = 80–84.9%), mesofacial (FI = 85–89.9%). [21] The facial divergence and skeletal malocclusion were assessed using cephalometric analysis using values of Frankfort horizontal to mandibular plane angle (FMA) and ANB angle, respectively. The FMA determined whether the face was hypodivergent (FMA < 21˚), hyperdivergent (FMA > 29˚) or normodivergent (FMA 25˚ ± 4˚). ANB angle was calculated by the difference between the Sella-Nasion-A angle (SNA) and Sella-Nasion-B angle (SNB). It classified the face into skeletal class I (ANB 2˚ ± 2˚), class II (ANB > 4˚) and class III (ANB < 0˚) malocclusions. Dental malocclusions were determined based on the position of mesiobuccal cusp (MB) of maxillary first molar (Mx1) with respect to buccal groove of mandibular first molar (Mn1) using dental casts and were classified into dental class I (if MB cusp of Mx1 lies in the buccal groove of Mn1), class II (if MB cusp of Mx1 lies mesial to the buccal groove of Mn1) and class III (if MB cusp of Mx1 lies distal to the buccal groove of Mn1) malocclusions. Data was collected on an organized study proforma by a single investigator. To calibrate the scoring of the single investigator, the facial type, divergence, skeletal and dental malocclusion of 10 random patients were selected to be evaluated at an initial time point. The same readings were retaken three weeks later to establish the consistency of the examiner [0.85].
We did not include the assessment of occlusal wear facets or crazing since the patients were undergoing orthodontic treatment and may present with surface deficits due to reason other than bruxism such as bracket breakages. According to a study by Abe et al. [22] tooth wear scores have only a modest diagnostic value in distinguishing bruxers from non-bruxers. This is further supported by Pergamalian et al. [23] who did not find bruxism to have destructive effects on the masticatory system such as noticeable tooth wear or muscle pain. There also remains a concern that tooth wear, crazing and cracks take time to appear in patients with bruxism and in our study only six months after the initiation of orthodontic treatment was evaluated.
Data analysis
Data was analyzed using SPSS version 23.0. The normality of the data was assessed using the Shapiro-Wilk test which showed a non-normal distribution. An intra-class correlation was applied to determine the intra-examiner reliability. Median and interquartile range (IQR) were reported for the age of patients. Frequencies were reported for all the categorical variables. Chi-square test was used to determine the relationship between questionnaire responses and presence or absence of bruxism. Binomial logistic regression analysis was used to assess the association of different factors with bruxism. A p-value of ≤ 0.05 was considered statistically significant.
Results
The total sample size was 80, with a gender distribution of 48 females and 32 males. The median age of the sample was 19.8 (17.7, 24.3) years. An intra-examiner reliability of 0.85 was determined.
Out of 80 (N) participants, 36 (n) reported bruxism after the initiation of orthodontic treatment. Among these 36 patients, 22 were mesofacial, nine were dolichofacial and five were brachyfacial. Regarding the facial divergence, 18 were normodivergent, 10 were hyperdivergent and eight were hypodivergent (Table 1).
Table 1.
Frequency of bruxism in orthodontic patients
| Variables | Frequency (Percentage%) | |
|---|---|---|
| Facial Type | Mesofacial | 22 (61) |
| Dolichofacial | 09 (25) | |
| Brachyfacial | 05 (14) | |
| Facial Divergence | Normodivergent | 18 (50) |
| Hyperdivergent | 10 (28) | |
| Hypodivergent | 08 (22) | |
| Skeletal Malocclusion | Class I | 17 (47) |
| Class II | 17 (47) | |
| Class III | 02 (6) | |
| Dental Malocclusion | Class I | 08 (22) |
| Class II | 26 (72) | |
| Class III | 02 (6) | |
N (Total no. of subject) = 80,
n (Total no. of subjects with bruxism) = 36
Binomial logistic regression analysis showed no association of bruxism with age and gender. When analyzing the association with different factors such as facial type and divergence, no statistically significant association was found. However, the odds of bruxism in hypodivergent patients were 2.4 times higher than normodivergent patients (Table 2). There was no statistically significant association of bruxism with skeletal and dental malocclusions. However, the odds of bruxism in dental class III patients were four times higher than class I patients (Table 2).
Table 2.
Influence of different factors on bruxism
| Variables | Odds Ratio | 95% CI | p-value | |
|---|---|---|---|---|
| Facial Type | Mesofacial | 0.8 | 0.4, 1.4 | 0.397 |
| Dolichofacial | 1.0 | 0.4, 3.0 | 0.939 | |
| Brachyfacial | 1.3 | 0.3, 4.9 | 0.728 | |
| Facial Divergence | Normodivergent | 0.7 | 0.4, 1.2 | 0.183 |
| Hyperdivergent | 1.3 | 0.5, 3.5 | 0.671 | |
| Hypodivergent | 2.4 | 0.7, 8.5 | 0.175 | |
| Skeletal Malocclusion | Class I | 0.8 | 0.4, 1.5 | 0.425 |
| Class II | 1.2 | 0.5, 2.9 | 0.752 | |
| Class III | 0.9 | 0.1, 5.8 | 0.879 | |
| Dental Malocclusion | Class I | 0.5 | 0.2, 1.2 | 0.109 |
| Class II | 1.9 | 0.7, 5.3 | 0.201 | |
| Class III | 4.0 | 0.3, 51.0 | 0.286 | |
N (Total no. of subject) = 80
n (Total no. of subjects with bruxism) = 36
Binomial Logistic regression, p ≤ 0.05
In the assessment of self-reported bruxism among patients undergoing orthodontic treatment, a statistically significant association was found with jaw fatigue or soreness upon awakening, with 28.7% of patients reporting these symptoms (p-value < 0.001) in the bruxism group. Furthermore, clenching (27.5%) and grinding (25%) during the daytime were significantly more prevalent among orthodontic patients with bruxism (p-value < 0.001). Teeth and gum soreness were also significantly associated with bruxism, affecting 25% of the orthodontic patients (p-value < 0.001). On the contrary, nocturnal grinding (10%) and temporal headaches (21.3%) were negatively correlated with bruxism in orthodontic patients (Table 3).
Table 3.
Association of Questionnaire responses with Bruxisms
| Bruxism | Has anyone heard you grinding your teeth at night? | Is your jaw ever fatigued or sore on awakening in the morning? | Are your teeth or gums ever sore on awakening in the morning? | Do you ever experience temporal headaches upon awakening in the morning? | Are you ever aware of grinding your teeth during the day? | Are you ever aware of clenching your teeth during the day? | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Yes | 8 (10%) | 28 (35%) | 23 (28.7%) | 13 (16.3%) | 20 (25%) | 16 (20%) | 17 (21.3%) | 19 (23.8%) | 20 (25%) | 16 (20%) | 22 (27.5%) | 14 (17.5%) |
| No | 1 (1.3%) | 43 (53.8%) | 5 (6.3%) | 39 (48.8%) | 6 (7.5%) | 38 (47.5%) | 4 (5%) | 40 (50%) | 1 (1.3%) | 43 (53.8%) | 7 (8.8%) | 37 (46.3%) |
| p-value | 0.006* | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** | ||||||
N (Total no. of subject) = 80,
n (Total no. of subjects with bruxism) = 36
Chi-square, p ≤ 0.05*, p ≤ 0.001**
Discussion
There is considerable literature in orthodontics regarding the relation of bruxism with orthodontic treatment and whether orthodontic therapy helps alleviate or rather provokes orofacial functional disorders in patients with bruxism/TMJ disorders. The question arises as to whether fixed mechanotherapy, which involves active tooth movement and may result in temporary occlusal interferences, could be a contributing factor to bruxism in a patient undergoing orthodontic treatment. In our study, 45% of orthodontic patients reported bruxism after commencement of the treatment. No significant association of bruxism with facial type, divergence, skeletal and dental malocclusions was observed. Though the results were not statistically significant, an elevated risk of bruxism in dental class III and hypodivergent patients was detected.
In a systematic review, Mohlin et al. [24] concluded that orthodontic therapy does not lead to the development of TMJ disorder/bruxism. Similarly, in a study by Hirsch [15]. , he evaluated the prevalence of bruxism in children and adolescents during orthodontic treatment and did not find any increased risk of bruxism or TMJ disorders, rather he observed a decrease in bruxism activities during treatment. The results are in contradiction with our study, as the adolescent and adult patients stated an increased risk of bruxism, suggesting a potential of fixed mechanotherapy for creating interferences capable of causing bruxism during orthodontic treatment.
Pereira et al. [9] compared awake bruxism in patients undergoing orthodontic treatment with fixed mechanotherapy (FA) and clear aligners (OA). They found frequency of bruxism to be 51.3% in patients undergoing orthodontic treatment with fixed mechanotherapy and 53.5% in patients with orthodontic aligners. The habits that comprised the diagnosis of awake bruxism in group FA included clenching of the teeth (7.6%) and grinding of the teeth (0.4%). Our study appraised both sleep and awake bruxism in patients undergoing fixed mechanotherapy and the results were reminiscent of their study revealing an increased risk of bruxism in orthodontic patients after the initiation of the treatment. Increased jaw fatigue or soreness upon awakening (28.7%), clenching (27.5%) and grinding (25%) during the daytime were reported as the most prevalent habits. Teeth and gum soreness also affected 25% of the orthodontic patients that reported bruxism.
Literature has revealed different oral habits and morphological factors that can lead to the development of bruxism [24, 25]. Safari et al. [26] reported a favorable relationship between bruxism and premature occlusal contacts suggesting the process of occlusal adjustments during orthodontic treatment could play a role in the development of bruxism. Our findings agree with these conclusions, as 45% orthodontic patients reported bruxism after the initiation of the treatment. Bellerive et al. [27] in their study investigated the effect of upper arch expansion on sleep bruxism in children and reported maxillary arch expansion to help reduce the occurrence of bruxism. Studies have reported intense and frequent bruxers to benefit from mandibular advancement devices and maxillary occlusal splints [28]. A study by Fujita et al. [29], which evaluated female orthodontic patients with a history of TMJ disorder and bruxism, reported that the bruxism habit remains unchanged or intensified throughout the treatment period, reinforcing these findings. In our study, we assessed the effect of fixed mechanotherapy in orthodontic patients with no previous history of bruxism or TMJ disorders and found an elevated risk of bruxism. This suggests that tooth manipulation during the treatment can be a risk factor for temporary bruxism.
According to Souza et al. [18] brachyfacial adolescents are less likely to present with awake bruxism compared to mesofacial. Whereas we found brachyfacial patients were at a higher risk of reporting bruxism as compared to mesofacial patients. Similarly, patients with hypodivergent facial type have increased odds of reporting bruxism during orthodontic treatment as compared to normodivergent facial types. Hazar Bodrumlu et al. [30] compared the length and width of the maxilla in bruxers and non-bruxers and found no difference between the two groups. Nahás-Scocate et al. [31] evaluated the association between bruxism and transverse malocclusions, such as posterior crossbite in children, and found no significant association between the two. However, our study, found that hypodivergent and dental class III patients had an elevated likelihood of reporting bruxism, although no significant association was found.
Ispir et al. [32] conducted a study to assess the effects of masseter muscle thickness on facial morphology and parafunctional habits. Though they found variation in masseter muscle thickness with facial morphology, they did not report any association with bruxism. A systematic review by Ribeiro-Lages et al. [33] further supports this interpretation and stated no association between bruxism with dental or skeletal malocclusions. Our study results are comparable to these findings, however, an increased odds of self-reported bruxism in hypodivergent and dental class III patients were demonstrated. This is suggestive of the fact that facial morphology alone may not be a determining factor, however, with the initiation of orthodontic tooth movement it may contribute to the development of bruxism in patients.
Patients with hypodivergent faces have a more compact bite that can lead to increased occlusal forces or stress and muscles activity during orthodontic treatment. Similarly, patients with class III malocclusion undergo changes in occlusion as well as bite forces, potentially resulting in altered muscle patterns. These shifts may contribute to occlusal discomfort, which could be a factor in the development of bruxism during orthodontic treatment [34].
During orthodontic treatment, teeth are often in a sensitive state and the treatment itself can lead to complications such as root resorption. When bruxism is introduced, which is known to cause hypersensitivity, root resorption and painful teeth, the overall impact can be significantly detrimental [2]. This highlights the importance of monitoring occlusal changes throughout the treatment process. Based on the increased reports of bruxism with hypodivergence and dental class III, orthodontists should monitor these patients more closely for any signs of bruxism throughout the treatment. Early detection of symptoms like jaw soreness or developing clenching or grinding habits is critical. Identification of occlusal discomfort or muscle tension early on can allow for timely intervention including the use of occlusal splints or occlusal adjustments. Proactive management strategies can ensure better outcomes and minimize complications associated with increased bruxism in these high-risk groups.
Most orthodontic interventions with fixed mechanotherapy take place during adolescence when all permanent teeth have erupted but there is an increasing trend of the adult population seeking orthodontic treatment for their esthetic and psychosocial benefits. Therefore, we evaluated the influence of orthodontics on bruxism in adolescents as well as adult patients. Our study was limited to being a cross-sectional study with a self-reported bruxism questionnaire and to the assessment of only four variables in association with bruxism in adolescent and adult age groups. Though the results did not reveal any statistical significance, a potential association is suggested by the odds ratio and warrants a further investigation in the area. While concerted efforts were made to exclude patients with a known history of bruxism, temporomandibular joint disorder (TMD), or anxiety, it remains possible that some cases of undiagnosed anxiety or TMD were not identified at baseline. To minimize this risk patients were asked specific questions regarding stress, and anxiety to rule out these cases before asking the patient to fill out the questionnaire.
Recommendations
The presence and absence of self-reported bruxism was evaluated but we recommend evaluation of factors such as a specific tooth movement, banding of molars or cementation of certain appliances that may be involved in development of bruxism. Furthermore, incorporating psychosocial factors, such as stress and anxiety in the analysis of this condition can help in devising specific preventive and treatment strategies. This holistic perspective acknowledges bruxism resulting not solely from physical factors but also phycological stresses. Variations in treatment plans, modalities and appliances may influence the development of such habits as well as TMJ disorders. Future studies could benefit from a larger sample size and an investigation of other factors that may have a relation with bruxism such as evaluation of occlusal scheme, canine guided occlusion versus group function occlusion; and presence of any occlusal interferences (working or non-working interferences, contacts on non-functional cusps). Conducting studies on a multicenter level in all age groups is crucial, given the public health relevance and its clinical implications of promoting root resorption and tooth surface damage.
Conclusions
The incidence of self-reported bruxism in orthodontic patients after the commencement of treatment was found to be 45%.
Factors such as facial type, divergence, skeletal and dental malocclusion have no statistically significant association with bruxism during orthodontic treatment.
There were increased odds of self-reported bruxism in dental class III and hypodivergent patients after the initiation of the treatment.
There is an increased frequency of jaw fatigue or soreness upon awakening, teeth and gum soreness, clenching and grinding during the daytime in orthodontic patients reporting with bruxism.
Acknowledgements
Not applicable.
Authors’ contributions
M.G: Conceptualization, study design, literature review, data collection, initial drafting of manuscript M.F: Conceptualization, critical review of the manuscript and supervision R.H.S: Conceptualization, statistical analysis and final review of the manuscript.
Funding
Not applicable.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study has been conducted in accordance with the guidelines of the Declaration of Helsinki. Additionally, approval (2023-9103-26467) was obtained from the Ethical Review Committee at the Aga Khan University before initiating the study. Written informed consent was obtained from all the patients participating in the study. In case of patients younger than 18 years assent from the child and parental consent from the parents were taken.
Consent for publication
Consent was obtained.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018;45:837–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beddis H, Pemberton M, Davies S. Sleep bruxism: an overview for clinicians. Br Dent J. 2018;225:497–501. [DOI] [PubMed] [Google Scholar]
- 3.Manfredini D, Ahlberg J, Lobbezoo F. Bruxism definition: past, present, and future - what should a prosthodontist know? J Prosthet Dent. 2022;128:905–12. [DOI] [PubMed] [Google Scholar]
- 4.Deo SS, Singh DP, Dogra N. Bruxism: its multiple causes and its effects on dental implants: a review. J Oral Health Craniofac Sci. 2017;2:57–63. [Google Scholar]
- 5.Tay KJ, Ujin YA, Allen PF. Impact of sleep bruxism on oral health-related quality of life. Int J Prosthodont. 2020;33:285–91. [DOI] [PubMed] [Google Scholar]
- 6.Wetselaar P, Vermaire EJH, Lobbezoo F, Schuller AA. The prevalence of awake bruxism and sleep bruxism in the Dutch adult population. J Oral Rehabil. 2019;46:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toyama N, Ekuni D, Taniguchi-Tabata A, Kataoka K, Yamane-Takeuchi M, Fujimori K, et al. Awareness of clenching and underweight are risk factors for onset of crowding in young adults: a prospective 3-year cohort study. Int J Environ Res Public Health. 2019;16:690–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chisini LA, San Martin AS, Cademartori MG, Boscato N, Correa MB, Goettems ML. Interventions to reduce bruxism in children and adolescents: a systematic scoping review and critical reflection. Eur J Pediatr. 2020;179:177–89. [DOI] [PubMed] [Google Scholar]
- 9.Pereira NC, Oltramari PV, Conti PC, Bonjardim LR, de Almeida-Pedrin RR, Fernandes TM, et al. Frequency of awake bruxism behaviour in orthodontic patients: randomized clinical trial: awake bruxism behaviour in orthodontic patients. J Oral Rehabil. 2021;48:422–9. [DOI] [PubMed] [Google Scholar]
- 10.Mainjot AK, Oudkerk J, Bekaert S, Dardenne N, Streel S, Koenig V, et al. Bruxism as a new risk factor of musculo-skeletal disorders? J Dent. 2023;135:1–8. [DOI] [PubMed] [Google Scholar]
- 11.Al-Groosh DH, Abid M, Saleh AK. The relationship between orthodontic treatment and temporomandibular disorders: a dental specialists’ perspective. Dent Press J Orthod. 2022;27:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giray B, Sadry S. Modifications in class I and class II division 1 malocclusion during orthodontic treatment and their association with TMD problems. Cranio. 2021;39:65–73. [DOI] [PubMed] [Google Scholar]
- 13.Deng X, Wang YJ, Deng F, Liu PL, Wu Y. Psychological well-being, dental esthetics, and psychosocial impacts in adolescent orthodontic patients: a prospective longitudinal study. Am J Orthod Dentofac Orthop. 2018;153:87–96. [DOI] [PubMed] [Google Scholar]
- 14.Machado NA, Costa YM, Quevedo HM, Stuginski-Barbosa J, Valle CM, Bonjardim LR, et al. The association of self-reported awake bruxism with anxiety, depression, pain threshold at pressure, pain vigilance, and quality of life in patients undergoing orthodontic treatment. J Appl Oral Sci. 2020;28:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirsch C. No increased risk of temporomandibular disorders and bruxism in children and adolescents during orthodontic therapy. J Orofac Orthop. 2009;70:39–50. [DOI] [PubMed] [Google Scholar]
- 16.Serafim I, Rode S, Lopes S, Oliveira W, Pinho S, Silva E, et al. Impact of bruxism on craniomandibular morphology: a cone-beam computed tomographic study. Cranio. 2022;23:1–11. [DOI] [PubMed] [Google Scholar]
- 17.Lamenha Lins RM, Cavalcanti Campêlo MC, Mello Figueiredo L, Vilela Heimer M, Dos Santos-Junior VE. Probable sleep bruxism in children and its relationship with harmful oral habits, type of crossbite and oral breathing. J Clin Pediatr Dent. 2020;44:66–9. [DOI] [PubMed] [Google Scholar]
- 18.Souza GL, Serra-Negra JM, Prado IM, Aguiar SO, Pordeus IA, Auad SM, et al. Association of facial type with possible bruxism and its related clinical features in adolescents: a cross-sectional study. Int Orthod. 2020;18:758–69. [DOI] [PubMed] [Google Scholar]
- 19.Pintado MR, Anderson GC, DeLong R, Douglas WH. Variation in tooth wear in young adults over a two-year period. J Prosthet Dent. 1997;77:313–20. [DOI] [PubMed] [Google Scholar]
- 20.Wetselaar P, Vermaire EJ, Lobbezoo F, Schuller AA. The prevalence of awake bruxism and sleep bruxism in the Dutch adolescent population. J Oral Rehabil. 2021;48:143–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muralidhar NV, Ranjan A, Jayashankar Rao JS, Sreeshyla HS, Nitin P. Cephalic index, facial index and dental parameters: a correlative study to evaluate their significance in facial reconstruction. J Oral Maxillofac Pathol. 2021;25:537–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abe S, Yamaguchi T, Rompré PH, De Grandmont P, Chen YJ, Lavigne GJ. Tooth wear in young subjects: a discriminator between sleep bruxers and controls? Int J Prosthodont. 2009;22:342–50. [PubMed] [Google Scholar]
- 23.Pergamalian A, Rudy TE, Zaki HS, Greco CM. The association between wear facets, bruxism, and severity of facial pain in patients with temporomandibular disorders. J Prosthet Dent. 2003;90:194–200. [DOI] [PubMed] [Google Scholar]
- 24.Mohlin B, Axelsson S, Paulin G, Pietilä T, Bondemark L, Brattström V, et al. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod. 2007;77:542–8. [DOI] [PubMed] [Google Scholar]
- 25.Gonçalves LP, Toledo OA, Otero SA. The relationship between bruxism, occlusal factors and oral habits. Dent Press J Orthod. 2010;15:97–104. [Google Scholar]
- 26.Safari A, Jowkar Z, Farzin M. Evaluation of the relationship between bruxism and premature occlusal contacts. J Contemp Dent Pract. 2013;14:616–21. [DOI] [PubMed] [Google Scholar]
- 27.Bellerive A, Montpetit A, El-Khatib H, Carra MC, Remise C, Desplats E, et al. The effect of rapid palatal expansion on sleep bruxism in children. Sleep Breath. 2015;19:1265–71. [DOI] [PubMed] [Google Scholar]
- 28.Landry ML, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont. 2006;19:549–56. [PubMed] [Google Scholar]
- 29.Fujita Y, Motegi E, Nomura M, Kawamura S, Yamaguchi D, Yamaguchi H. Oral habits of temporomandibular disorder patients with malocclusion. Bull Tokyo Dent Coll. 2003;44:201–7. [DOI] [PubMed] [Google Scholar]
- 30.Hazar Bodrumlu E, Çakmak Özlü F, Yılmaz H, Demiriz L. Investigating the effect of bruxism on maxillary arch length and width in children using three-dimensional digital model analysis. Prog Orthod. 2022;23:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nahás-Scocate AC, Coelho FV, De Almeida VC. Bruxism in children and transverse plane of occlusion: is there a relationship or not? Dent Press J Orthod. 2014;19:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ispir NG, Toraman M. The relationship of masseter muscle thickness with face morphology and parafunctional habits: an ultrasound study. Dentomaxillofac Radiol. 2022;51:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ribeiro-Lages MB, Martins ML, Magno MB, Masterson Ferreira D, Tavares-Silva CM, Fonseca-Gonçalves A, et al. Is there association between dental malocclusion and bruxism? A systematic review and meta-analysis. J Oral Rehabil. 2020;47:1304–18. [DOI] [PubMed] [Google Scholar]
- 34.Alhammadi MS, Almashraqi AA, Khadhi AH, Arishi KA, Alamir AA, Beleges EM, Halboub E. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in borderline class III malocclusion: a systematic review. Clin Oral Investig. 2022;26:6443–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.