Abstract
We report a nonfatal case of streptococcal toxic shock syndrome (STSS) caused by a Streptococcus pyogenes emm118 strain encoding a novel variant of streptococcal mitogenic exotoxin Z (SMEZ-34). This variant was responsible for the major mitogenic activity in the cell culture supernatant. Patient sera showed seroconversion toward SMEZ, implying a role for this toxin in STSS.
CASE REPORT
A 36-year-old woman who was in Fiji competing in an adventure tourism event complained of severe headache and widespread myalgia and arthralgia over the preceding 3 days. There was no history of respiratory, gastrointestinal, or urinary symptoms. She was seen at a local hospital and found to be cold (temperature = 35.5°C), tachycardic (heart rate = 100/min) and hypotensive (blood pressure = 60/40 mm Hg). She was given 5 liters of intravenous fluids and transferred to Auckland City Hospital, Auckland, New Zealand, with a provisional diagnosis of dengue fever. On arrival, she was found to have several minor noninfected coral cuts on her feet and a reddened ecchymosis over the extensor surface of her left elbow. Her vital signs (temperature = 38°C, heart rate = 100/min, blood pressure = 90/60 mm Hg, and respiratory rate = 20/min) were largely unchanged, and there was evidence of a right pleural effusion but no other examination findings of note. In particular, there was no rash or conjunctival injection. Initial investigations showed a hemoglobin count of 107 g/liter (normal range [N] = 115 to 155), a white blood cell count of 4.80 × 109/liter (N = 4.0 to 10.0), band neutrophils of 1.92 × 109/liter with toxic granulation and Doehle bodies present, a platelet count of 54 × 109/liter (N = 150 to 400), activated partial thromboplastin time of 46 s (N = 25 to 37), international normalized ratio of 1.4, albumin at 20 g/liter (N = 35 to 48), bilirubin at 41 μmol/liter (N = 1 to 18), alanine transaminase at 63 units/liter (N = 0 to 40), and aspartate transaminase at 69 IU/liter (N = 0 to 45). Her creatine kinase was elevated (461 U/liter; N = 30 to 180), as was her serum myoglobin (138 μg/liter; N = 25 to 60). Blood cultures were performed on arrival at Auckland Hospital on blood collected from a peripheral vein and were found to be sterile.
She rapidly deteriorated with worsening hypotension, and when a chest X ray showed features of acute respiratory distress syndrome, she was transferred to the Department of Critical Care Medicine. She was treated with cefuroxime (1 g every 8 h) and erythromycin (500 mg every 6 h) intravenously for the first 2 days after her admission but received no further antibiotic therapy until day 12 after her admission. Her hospital stay was complicated by an acute cardiomyopathy with widespread electrocardiogram changes, prolonged episodes of supraventricular tachycardia, echocardiographic evidence of global ventricular impairment, and a rise in her troponin T levels to 1.42 μg/liter (N = <0.03) during the first 2 days after her admission; the development of large pleural effusions on day 6 after her admission; and the onset of severe bilateral, radicular, neuropathic pain in her legs on day 12 after her admission. A magnetic resonance imaging scan showed soft tissue inflammatory changes from T12 to L2 but no abnormalities in the vertebrae, spinal cord, or nerve roots. Testing of acute- and convalescent-phase sera showed no evidence of recent infection with dengue virus, Leptospira spp., Rickettsia, Legionella spp., Ross River virus, or other arboviruses.
On day 12 after her admission, she developed bilateral olecranon bursitis and several discrete soft tissue collections around her left thigh. Gram-positive cocci were seen in pus swabs from her right olecranon bursa and from superficial collections over both elbows and her left hip. Streptococcus pyogenes was isolated from all samples. Subsequent PCR amplification and sequencing of the emm gene demonstrated that all isolates were emm type 118. She was treated with benzylpenicillin (2 mU every 6 h) for 14 days, and these collections resolved with no subsequent relapse. She was discharged home after a hospital admission of 31 days. Follow-up assessment 3 months after admission found no significant long-term complications.
Written consent for using serum samples and for publishing the data has been obtained from the patient. Incidences of infection by Streptococcus pyogenes, or group A streptococcus (GAS), and subsequent invasive diseases have been increasing since the 1980s (6, 14). One of the most severe forms of invasive streptococcal disease is streptococcal toxic shock syndrome (STSS), which often occurs in conjunction with other invasive diseases, such as cellulitis, bacteremia, and necrotizing fasciitis. The characteristics of STSS are hypotension, shock, multiple organ failure, and sometimes death. STSS is associated with a mortality rate of 30 to 80% (7, 14).
GAS produce a number of highly mitogenic toxins that belong to the family of bacterial superantigens (SAgs). Currently, 11 immunogenically different GAS superantigens have been described in the literature (reviewed in reference 10). These include the streptococcal pyrogenic exotoxins A, C, and G to M; the streptococcal superantigen; and the streptococcal mitogenic exotoxin Z (SMEZ), which has 33 known allelic variants.
Several lines of evidence suggest that SAgs play a pivotal role in the pathogenesis of STSS. (i) Epidemiological studies have established a link between GAS strains that produce SAgs and the development of STSS (16). (ii) Animal infection models and in vitro analyses have shown that SAgs are strong inducers of proinflammatory cytokines, in particular interleukin-1β and tumor necrosis factor alpha, and that they can cause STSS-like symptoms in rabbits, rodents, and baboons (2, 5, 8, 15). (iii) Clinical studies have shown circulating SAgs in the acute-phase sera of patients with STSS and seroconversion during convalescence (12, 13). Furthermore, the lack of neutralizing anti-SAg (α-SAg) antibodies appears to be a risk factor for the development of STSS (3, 1).
In this study, we provide further evidence for the involvement of SAgs, in particular SMEZ, in a severe case of STSS. Patient sera (PS) from 2, 6, and 16 days after hospital admission were assayed for the presence of circulating SAgs, using methods published previously (12). Each of the serum samples, and fetal calf serum (FCS) as a control, was tested for the ability to stimulate human peripheral blood lymphocytes (PBLs) in a [3H]thymidine uptake assay. All experiments were carried out in duplicate. No significant PBL stimulation was detected with any of the three PS (results not shown), indicating that the sera did not contain significant amounts of SAgs. This was not surprising, as the first sample (day 2 postadmission) was taken 5 days after infection. In a previous study, circulating SAgs could be detected only early during the acute phase and were subsequently cleared (12).
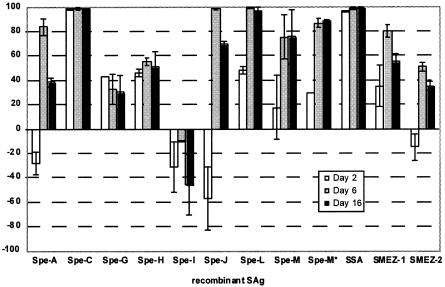
To investigate SAg-induced seroconversion, the three PS were tested for SAg-neutralizing antibodies. Serum samples (5%) were incubated with PBLs in the presence of recombinant SAgs at subsaturation concentrations. FCS was used as a negative control. The relative inhibition of SAg activity was calculated as 1 − (cpmPS/cpmFCS) × 100. The results in Fig. 1 show that between day 2 and day 16 postadmission, the patient developed neutralizing antibodies toward SPE-A, -J, -L, -M, and -M*, SMEZ-1, and SMEZ-2. In particular, the patient completely lacked neutralization capacity against SPE-A, SPE-J, and SMEZ-2 at day 2 postadmission but developed significant neutralization responses at day 6 (84%, 48%, and 51%, respectively), indicating the production of these SAgs during infection. We also observed an increase in titer for neutralizing antibodies against SPE-L (from 48% to 94%), SPE-M (17% to 75%), SPE-M* (29% to 88%), and SMEZ-1 (35% to 55%). SMEZ-1 and SMEZ-2 are allelic variants, and some degree of antibody cross-reactivity has been shown previously (11).
FIG. 1.
Titers of α-SAg neutralizing antibodies in acute- and convalescent-phase sera. The PS, collected on days 2, 6, and 16 after hospital admission, were tested for SAg neutralization against all currently known streptococcal SAgs. All experiments were carried out in duplicate. The error bars indicate standard deviations.
The serotype of the isolated GAS strain was determined to be emm118, a recent addition to the Lancefield classification, which is most closely related to serotype M49 (4). The clinical isolate was genotyped for the complete set of currently known GAS sag genes by PCR, using previously described methods (12). The genotype of this isolate was determined for all known sag genes and found to be positive for spe-g, spe-h, spe-j, and smez. The smez gene was sequenced, and when compared to the 33 known alleles, was found to be a novel allele most closely related to smez-2. The toxin differs from SMEZ-2 (the most potent SMEZ variant discovered so far) in only three amino acids (N11D, I23T, and V177T) but is only 92% identical (by amino acid sequence) to SMEZ-1, which might explain the difference in the neutralization potencies of the PS (Fig. 1). The novel allele was designated smez-34.
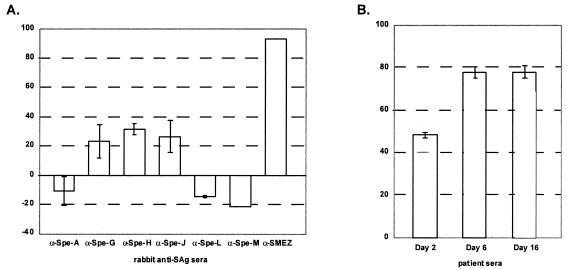
The clinical GAS isolate was cultured as previously described (12), and the culture supernatant was collected for analysis of in vitro SAg expression. A standard PBL proliferation assay with various dilutions of GAS cell supernatant showed mitogenic activity starting at 1:8,000 dilution and reaching saturation at 1:5. In an attempt to identify the SAg(s) responsible for the detected activity, a subsaturating dilution of supernatant (1:10) was incubated with individual 5% rabbit sera raised against SPE-A, -G, -H, -J, -L, and -M and SMEZ in a standard PBL stimulation assay (Fig. 2A). The α-SMEZ serum was raised against a combination of SMEZ-1 and SMEZ-2. The addition of rabbit α-SMEZ serum alone inhibited 92.9% of the supernatant activity, while only minor inhibition was observed with α-SPE-H serum (31.5%), α-SPE-J serum (26.5%), and α-SPE-G serum (20.4%). No inhibition was obtained with α-SPE-A, α-SPE-L, and α-SPE-M antibodies. This indicates that SMEZ is the major immunoactive SAg in the GAS supernatant. The three PS were also tested in this assay (Fig. 2B) and progressively inhibited the supernatant activity, ranging from 48.5% on day 2 and 77.8% on day 6 to 78.0% on day 16, which is consistent with the observed seroconversion against individual toxins (Fig. 2A).
FIG. 2.
(A) The clinical isolate preferentially produces SMEZ in vitro. The isolated emm118 strain was grown in vitro, and culture supernatant was used to stimulate human PBL proliferation. Rabbit antisera raised against individual SAgs were used to specifically neutralize SAg activity. Anti-SMEZ antiserum (raised against a 1:1 mixture of recombinant SMEZ-1 and recombinant SMEZ-2) neutralized the majority (92.9%) of the supernatant activity, while antisera against other toxins had no or only minor effects. (B) Patient sera increase in neutralization capacity over time. Patient sera were used to neutralize SAg activity in culture supernatant of the emm118 strain. Significant increase in the neutralizing antibody titer was observed during convalescence. All experiments were carried out in duplicate. The error bars indicate standard deviations.
Our results are in line with a previous study that showed that SMEZ was the major immmunoactive agent in a clinical GAS isolate (17). Moreover, SMEZ was shown to induce a cytokine response approximately 10-fold higher than that with SPE-A (9). Our results also strongly support the observations in other studies that suggested lack of neutralizing α-SAg antibody as a risk factor for STSS (1, 3).
Using site-directed mutational analysis, we have created several SMEZ mutants that are deficient in binding to the T-cell receptors but not to major histocompatibility complex class II (unpublished data). These mutants show strongly decreased proliferation responses and could potentially be used as toxoids in the development of a vaccine against STSS.
Nucleotide sequence accession number.
The novel allele smez-34 was submitted to GenBank under accession number AY803782.
Acknowledgments
This work was supported by the Health Research Council New Zealand (Sir Charles Hercus Research Fellowship).
REFERENCES
- 1.Basma, H., A. Norrby-Teglund, Y. Guedez, A. McGreer, D. E. Low, O. El-Ahmedy, B. Schwartz, and M. Kotb. 1999. Risk factors in the pathogenesis of invasive group A streptococcal infections: role of protective humoral immunity. Infect. Immun. 67:1871-1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonventre, P. F., H. Heeg, C. Cullen, and C. J. Lian. 1993. Toxicity of recombinant toxic shock syndrome toxin 1 and mutant toxins produced by Staphylococcus aureus in a rabbit infection model of toxic shock syndrome. Infect. Immun. 61:793-799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eriksson, B. K. G., J. Andersson, S. E. Holm, and M. Norgen. 1999. Invasive group A streptococcal infections: T1M1 isolates expressing pyrogenic exotoxins A and B in combination with selective lack of toxin-neutralizing antibodies are associated with increased risk of streptococcal toxic shock syndrome. J. Infect. Dis. 180:410-418. [DOI] [PubMed] [Google Scholar]
- 4.Facklam, R. F., D. R. Martin, M. Lovgren, D. R. Johnson, A. Efstratiou, T. A. Thompson, S. Gowan, P. Kriz, G. J. Tyrell, E. Kaplan, and B. Beall. 2002. Extension of the Lancefield classification for group A streptococci by addition of 22 new M protein gene sequence types from clinical isolates: emm103 to emm124. Clin. Infect. Dis. 34:28-38. [DOI] [PubMed] [Google Scholar]
- 5.Herman, A., J. W. Kappler, P. Marrack, and A. M. Pullen. 1991. Superantigens: mechanism of T-cell stimulation and role in immune responses. Annu. Rev. Immunol. 9:745-772. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan, E. L. 1991. The resurgence of group A streptococcal infections and their sequelae. Eur. J. Clin. Microbiol. Infect. Dis. 10:55-57. [DOI] [PubMed] [Google Scholar]
- 7.McCormick, J. K., J. M. Yarwood, and P. M. Schlievert. 2001. Toxic shock syndrome and bacterial superantigens: an update. Annu. Rev. Microbiol. 55:77-104. [DOI] [PubMed] [Google Scholar]
- 8.Miethke, T., C. Wahl, K. Heeg, B. Echtenacher, P. H. Krammer, and H. Wagner. 1992. T cell-mediated lethal shock triggered in mice by the superantigen staphylococcal enterotoxin B: critical role of tumor necrosis factor. J. Exp. Med. 175:91-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muller-Alouf, H., T. Proft, T. M. Zollner, D. Gerlach, E. Champagne, P. Desreumaux, C. Fitting, C. Geoffroy-Fauvet, J. E. Alouf, and J. M. Cavaillon. 2001. Pyrogenicity and cytokine-inducing properties of Streptococcus pyogenes superantigens: comparative study of streptococcal mitogenic exotoxin Z and pyrogenic exotoxin A. Infect. Immun. 69:4141-4145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Proft, T., and J. D. Fraser. 2003. Bacterial superantigens. Clin. Exp. Immunol. 133:299-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Proft, T., S. L. Moffatt, K. D. Weller, A. Paterson, D. Martin, and J. D. Fraser. 2000. The streptococcal superantigen SMEZ exhibits wide allelic variation, mosaic structure, and significant antigenic variation. J. Exp. Med. 191:1765-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Proft, T., S. Sriskandan, L. Yang, and J. D. Fraser. 2003. Superantigens and streptococcal toxic shock syndrome. Emerg. Infect. Dis. 9:1211-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sriskandan, S., D. Moyes, and J. Cohen. 1996. Detection of circulating bacterial superantigen and lymphotoxin-α in patients with streptococcal toxic-shock syndrome. Lancet 348:1315-1316. [DOI] [PubMed] [Google Scholar]
- 14.Stevens, D. L. 2000. Streptococcal toxic shock syndrome associated with necrotizing fasciitis. Annu. Rev. Med. 51:271-288. [DOI] [PubMed] [Google Scholar]
- 15.Stevens, D. L., A. E. Bryant, S. P. Hackett, A. Chang, G. Peer, S. Kosanke, T. Emerson, and L. Hinshaw. 1996. Group A streptococcal bacteremia: the role of tumor necrosis factor in shock and organ failure. J. Infect. Dis. 173:619-626. [DOI] [PubMed] [Google Scholar]
- 16.Talkington, D. F., B. Schwartz, C. M. Black, J. K. Todd, J. Elliott, R. F. Breiman, and R. R. Facklam. 1993. Association of phenotypic and genotypic characteristics of invasive Streptococcus pyogenes isolates with clinical components of streptococcal toxic shock syndrome. Infect. Immun. 61:3369-3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Unnikrishnan, M., D. M. Altmann, T. Proft, F. Wahid, J. Cohen, J. D. Fraser, and S. Sriskandan. 2002. The bacterial superantigen streptococcal mitogenic exotoxin Z is the major immunoactive agent of Streptococcus pyogenes. J. Immunol. 169:2561-2569. [DOI] [PubMed] [Google Scholar]