Abstract
Since the late 1980s several studies have described the increased incidence and severity of invasive group A streptococcal (GAS) infections. However, most studies on GAS pathogenesis have focused on information obtained during outbreaks. We analyzed isolate distribution and host susceptibility as part of a nationwide prospective surveillance study performed between January 2001 and August 2002. GAS isolates collected from 201 patients with invasive infections, 335 patients with noninvasive infections, and 17 asymptomatic carriers were characterized with respect to their emm types and superantigen genotypes. The superantigen-neutralizing capacity and levels of antibodies against streptolysin O and DNAse B were determined for isolates from the sera from 36 invasive cases and 91 noninvasive cases. emm type 1 (emm-1) isolates were significantly more common among invasive cases, whereas emm-4, emm-6, and emm-12 dominated among the noninvasive cases. The distributions of the phage-associated superantigen genes (speA, speC, speH, speI, ssa) differed among invasive and noninvasive isolates, mainly due to their linkage to certain emm types. No significant differences in serum superantigen-neutralizing capacities were observed. The levels of anti-streptolysin O and anti-DNAse B antibodies were highest in the sera from invasive cases. Our study emphasizes the importance of obtaining data during years with stable incidences, which will enable evaluation of future outbreak data.
Group A streptococcus (GAS) is one of the most common human pathogens and causes both invasive and noninvasive infections. Invasive GAS infections include bacteremia, pneumonia, puerperal sepsis, cellulitis, necrotizing fasciitis (NF), and streptococcal toxic shock syndrome (STSS) (7, 40). Noninvasive infections, which predominantly manifest as tonsillitis and impetigo, cause a significant number of consultations in general practice (18).
In the late 1980s severe invasive GAS infections reemerged, and since then, attention has particularly been focused on the increasing incidence and severity of these infections (7, 8, 19, 40). Only a few reports have recently described the incidence of noninvasive GAS infections and of the throat carriage of GAS (23, 24).
The M protein is an important virulence determinant in the pathogenesis of GAS infections. Since approximately 150 different M-protein gene sequence types (emm types) have been documented, the emm type is an important surveillance tool in investigations of the dynamics in GAS infections (26, 39). Furthermore, GAS produces a range of streptococcal pyrogenic exotoxins (SPEs), which are important in the pathogenesis of severe GAS infections, where they act as superantigenic toxins (SAgs) (14, 28, 32). The prevalence and severity of the invasive disease that any particular GAS isolate (of a given emm type and SAg profile) may cause depend on the invasiveness of the strain, the prevalence of the strain circulating within a community, and the level of strain-specific immunity (33). Without coincident data on the prevalences of emm types and SAg profiles that circulate in a given community and that cause noninvasive disease, no conclusions can be drawn about the relative invasiveness of a strain. Most studies so far have been based on clinical specimens collected during outbreaks of invasive GAS infections. In this paper, we present nationwide data on the epidemiology of isolates causing invasive and noninvasive GAS disease prospectively collected during a prolonged period of stable incidence rates. Additionally, we present comparable data for isolates that were identified from either invasive or noninvasive GAS infections as well as from asymptomatic carriers in order to monitor possible trends in the emm distributions; SAg profiles, i.e., the genes encoding pyrogenic exotoxins A to C and F to J, SSA, and SMEZ (speA to speC, speF to speJ, ssa, and smeZ, respectively) (19, 27, 29, 34-37); and the hosts' susceptibilities to their own infecting strains.
MATERIALS AND METHODS
Surveillance, including specimens and sera.
Included in this study were 201 invasive GAS isolates obtained from normally sterile sites (blood, cerebrospinal fluid [CSF], synovial fluid, pleural fluid, sterile aspirates, or tissue obtained during surgery or autopsy). The invasive GAS isolates were obtained between 1 January 2001 and 1 August 2002 and were collected from all of the 15 clinical microbiological departments in Denmark through a nationwide surveillance study conducted by the Streptococcus Unit, Statens Serum Institut, Copenhagen, Denmark. Ninety-five percent of the invasive isolates were obtained from blood; 1% of the isolate were obtained from CSF; and the remaining 4% of the isolates were obtained from lung, tissue, or pleural fluid. Ten of the 15 clinical microbiological departments were able to provide additional information regarding the number of blood cultures for invasive GAS performed. This enabled us to estimate that we received in average 80% of the GAS blood isolates identified by the clinical microbiological departments.
A detailed questionnaire (relating to patient characteristics, the infection, and the outcome) was obtained from the physicians responsible for the treatment of each patient. The questionnaire response rate was 98%. In the present study the following definitions were used: bacteremia was defined as a clinical entity associated with identification of GAS in the blood culture without any septic focus or complications. NF was defined as clinically diagnosed necrosis of the fascia or tissue (excluding muscle). A soft tissue infection was defined as either NF or myositis. A patient with septic shock was defined as one who had an invasive GAS infection and a systolic blood pressure below 90 mm Hg. Finally, the definition of STSS was based on the consensus definition from the Working Group on Severe Streptococcal Infections (43).
The overall case fatality rate was assessed 30 days after sampling of specimens with positive culture results, based on the dates of death obtained from the Danish Central Office of Civil Registration.
In addition to the invasive isolates, a total of 2,089 throat and wound swab specimens were received from general practitioners (GPs) between 1 January 2001 and 1 August 2002 (Table 1). The GPs were not restricted in terms of the selection of patients based upon age, sex, or underlying conditions. In total, GAS were identified in 352 swab specimens. GAS were identified in 273 (28%) throat swab specimens from patients with tonsillitis (synonymous with pharyngitis in this study) included among the 975 throat swab specimens from patients with sore throat. GAS were identified in 62 (13%) of the 467 wound swab specimens from patients with impetigo. Finally, 17 (3%) of 647 asymptomatic individuals investigated carried GAS in the throat. An asymptomatic carrier was defined as an individual harboring GAS in the throat without having a sore throat or impetigo and without having received treatment with antibiotics within the last 2 weeks but who still consulted a GP. Asymptomatic carriage was not considered an infection, but since the GP swabbed these individuals, we still designate them as patients.
TABLE 1.
Clinical manifestations of the invasive and noninvasive group A streptococcal cases
| Clinical manifestation | No. (%) of cases
|
||
|---|---|---|---|
| Total casesa | Fatal casesb | Cases with seraa | |
| Invasive cases | |||
| Bacteremia only | 50 | 19 (38) | 6 (12) |
| Erysipelas | 49 | 4 (8) | 11 (22) |
| Pneumonia | 23 | 5 (22) | 2 (9) |
| STSS | 20 | 11 (55) | 2 (10) |
| NF | 13 | 4 (31) | 3 (23) |
| Arthritis | 10 | 1 (10) | 2 (20) |
| Puerperal sepsis | 8 | 1 (13) | 2 (25) |
| Meningitis | 6 | 2 (33) | 0 (0) |
| Otherc | 36 | 5 (14) | 8 (22) |
| Total for invasive cases | 201 | 50 (25) | 33 (16) |
| Noninvasive cases | |||
| Tonsillitis | 273 | NId | 82 (30) |
| Impetigo | 62 | NI | 6 (10) |
| Total for noninvasive cases | 335 | NI | 91 (27) |
| Carriers | 17 | NI | 4 (24) |
| Controls | 0 | NI | 148 |
Among the invasive cases, some cases are registered with more than one diagnosis.
Fatal cases, death ≤30 days after culture was obtained. The date of death was obtained from Central Office of Civil Registration.
Including gynecological, urological, or orthopedic infections or unknown.
NI, not investigated.
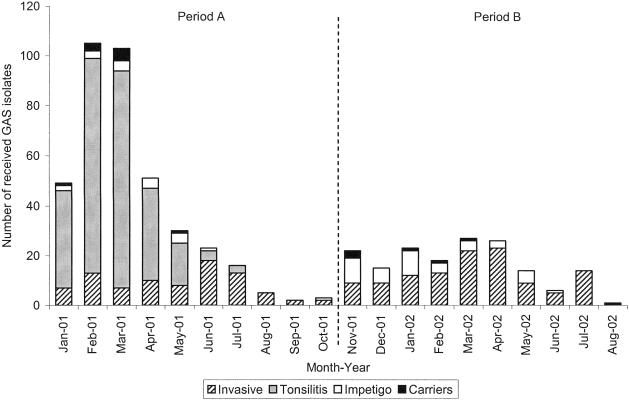
Based on the collection dates of the isolates received (Fig. 1), we divided the study period into two periods: period A was from 1 January 2001 to 31 October 2001, and period B was from 1 November 2001 to 1 August 2002. Moreover, noninvasive GAS isolates (from patients with tonsillitis and impetigo and from healthy carriers) collected during period A were from five counties (in the region of Zealand) only. Noninvasive GAS isolates (from patients with impetigo and healthy carriers) collected during period B were from 10 counties (in the regions of Funen and Jutland) only. In the present study, differences in the distributions of the emm types or the SAg profiles between invasive and noninvasive isolates were investigated by comparing isolates obtained from the same period of time to avoid any potential bias due to differences in the times of collection.
FIG. 1.
Distributions by month of the invasive and noninvasive group A streptococcal isolates received in the Streptococcus Unit during the study period and the presentations of the patients during period A (1 January to 31 October 2001) and period B (1 November 2001 to 1 August 2002).
We received blood samples from 36 patients with invasive GAS infections from whom we had already received invasive GAS isolates (defined as paired sera and GAS isolates). The delay between the onset of the initial symptoms and the time of blood sampling ranged from 3 to 63 days. We intended to include sera collected ≤6 days after the onset of the initial symptoms, as described previously (31). However, sera from only 12 patients (33%) were collected ≤6 days (median, 4.5 days) after the onset of the initial symptoms; and therefore, sera from the remaining 24 patients, which were collected >6 days after the onset of symtoms, were also included as a comparison group in the present study. The GPs did not provide any information regarding the duration of symptoms prior to the time of blood sampling.
In total, 809 blood samples were received from the GPs, and in 92 cases we received both a noninvasive GAS isolate culture and a blood sample (paired sera and GAS isolates). Of the remaining 717 blood samples, 148 were chosen at random. The throat or wound swabs from these patients were GAS negative and served as GAS-negative controls.
Characterization of the isolates. (i) DNA preparation and emm sequencing.
Genomic DNA was prepared as described previously (15) and was used for emm sequencing and identification of the spe genes. In addition to the 352 GAS noninvasive isolates, 200 of the 201 invasive isolates were available for determination of the emm types and the SAg profiles.
The emm gene types of the GAS were determined by amplification and sequencing of the emm genes essentially as described elsewhere (4). The emm sequences were obtained according to recommendations (12) and aligned with sequences available at the emm type database of the Centers for Disease Control and Prevention (http://www.cdc.gov/ncidod/biotech/strep/strepindex.html).
(ii) Identification of spe genes (speA to speC, speF to speJ, ssa, and smeZ).
The primers used for identification of the spe genes were found in the literature (6, 20, 27, 34, 35, 42).
Detection of speF to speJ, ssa, and smeZ was performed by using the following protocol in the thermocycler: preheating for 2 min at 95°C, followed by 40 cycles of 94°C for 1 min, 50°C for 30s, and 72°C for 1 min 30s. The detection of speA to speC was carried out by the same protocol; however, annealing was at 58°C for 35 cycles (20). Amplification of each of the genes located on a mobile DNA element (i.e., speA, apeC, speH, speI, and ssa) was carried out in combination with amplification of a chromosomal gene (i.e., speB, speF, speG, speJ, smeZ, or 16S rRNA), which functioned as a positive control.
Preparation of bacterial culture supernatants.
After incubation overnight in 6 ml Todd-Hewitt broth (Statens Serum Institut, Denmark), the bacteria were removed from the culture supernatants by centrifugation. Proteins were precipitated overnight at −20°C by adding 10.5 ml 99.9% ethanol to 3.5 ml of the culture supernatant. After centrifugation, the sediments were solubilized in 350 μl distilled H2O; transfused through a 0.2 μl sterile filter (Minisart, Sartorius, Goettingen, Germany); and placed in Eppendorf tubes, which were kept on ice. This corresponds to a 10-fold concentration of the culture filtrate (30).
Thirty-five of the culture supernatants were initially tested at 1:100 dilutions for their ability to induce T-cell proliferation. All gave good proliferative responses (mean, 19,942 CPM; range, 11,002 to 30,396 CPM); hence, this concentration was used in further experiments.
Superantigen neutralization assay.
Peripheral blood mononuclear cells were isolated from a healthy blood donor, stimulated with the cell-free bacterial culture supernatants (diluted 1:100) in the presence of 2.5% heat-inactivated patient serum (PS) supplemented with 2.5% fetal calf serum (FCS), or in the presence of 5% FCS, and incubated at 37°C in 5% CO2 with 95% humidity. The patients' serum samples were tested for neutralizing activity against their own bacterial isolates. After 72 h the cells were pulsed for 6 h with 1 μCi/well [3H]thymidine (specific activity = 6.7 Ci/mmol; MP Biomedicals, Irvine, CA), harvested onto glass-fiber filters, and counted in liquid scintillation counter (Packard, Downers Grove, IL).
All samples were assayed in triplicate, and the data are presented as the mean counts per minute of [3H]thymidine uptake ± standard deviation, calculated by the equation (30): [1 − (cpmPS + stimulus − cpmPS)/(cpmFCS + stimulus − cpmFCS)] × 100.
As a control to exclude any cytoxic effect, the proliferative responses of all culture supernatants supplemented with FCS (Sup, FCS) were tested without PS: mean(Sup,FCS), 21,357 cpm (range, 2,354 to 52,588 cpm). In comparison, the mean of the unstimulated peripheral blood mononuclear cells was 181 cpm (range, 10 to 1,364 cpm).
Four blood samples were subsequently excluded from the neutralizing assay due to procedural errors. Therefore, the neutralizing activity in the sera was investigated with the paired sera and GAS isolates from 91 patients with noninvasive GAS infections and 33 patients with invasive GAS infections.
ASOT and ASDB antibodies.
Determination of the anti-streptolysin O (ASOT) and anti-DNase B (ASDB) titers in sera was performed as described by Johnson et al. (21, 22). Results were obtained for 33 and 88 patients with invasive and noninvasive GAS infections, respectively. Likewise, sera from the 148 GAS-negative controls were analyzed.
Statistical analysis.
Data were analyzed with the SAS system, release 8.02 (SAS Institute Inc. Cary, NC) and GraphPad Prism version 3.00 for Windows (GraphPad Software, San Diego, CA). The chi-square test or Fisher's exact probability test, together with the Mann-Whitney test, was used where appropriate for comparisons between the groups. The Spearman rank correlation test was performed to assess the correlation between serum antibody titers and age. A P value of <0.05 was considered significant.
The annual number of inhabitants in the period from 2000 to 2001 was reported from Statistics Denmark. Incidence rates are presented as the number of cases per 100,000 inhabitants per year.
Ethical considerations.
Informed consent was obtained from all patients. The invasive isolates were received as part of the national surveillance program. The study was approved by the Scientific Ethical Committees for Copenhagen and Frederiksberg [no. (KF) 11-156/00] and by the Danish Data Protection Agency (no. 2001-41-0807).
RESULTS
The 201 invasive GAS isolates were received as part of the national program of surveillance for invasive beta-hemolytic streptococcal infections. A total of 107 (53.0%) of the patients were females. Table 1 presents the clinical manifestations and outcomes of the infections for patients with invasive and noninvasive cases. Among the invasive cases, bacteremia was registered as the only diagnosis in 25% of the cases, followed by erysipelas, which occurred in 24% of the cases (all erysipelas GAS isolates were obtained from blood cultures). Twenty patients (10%) had STSS, and 13 (6%) had NF. Other diagnoses included pneumonia, puerperal sepsis, and meningitis. The overall case fatality rate was 25% and varied substantially with age and clinical manifestations. Of the 50 patients with fatal outcomes, 56% died on the same day or the day after the sample for culture was obtained, and 80% died within the first 6 days.
The distributions of the collection dates of the invasive and noninvasive group A streptococcal isolates received during the study period and their relation to periods A and B are shown in Fig. 1.
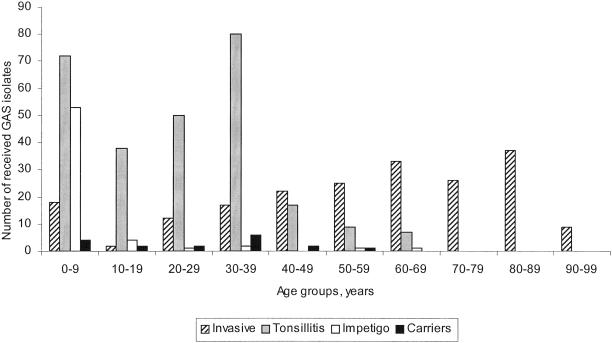
There were significant differences in the age distributions between the categories of patients (P < 0.01): the median age of the patients with invasive infections was 61.7 years (range, 0.4 to 97.4 years), whereas the median age of the patients with tonsillitis was 27.2 years (range, 0.9 to 69.7 years); and the patients with impetigo were younger, with a median age of 4.7 years (range, 0.4 to 61.2 years). The median age of the carriers was 32.2 years (range, 0.4 to 69.7 years) (Fig. 2).
FIG. 2.
Age distributions of the invasive and noninvasive group A streptococcal isolates from patients with invasive infections, tonsillitis, and impetigo and asymptomatic carriers.
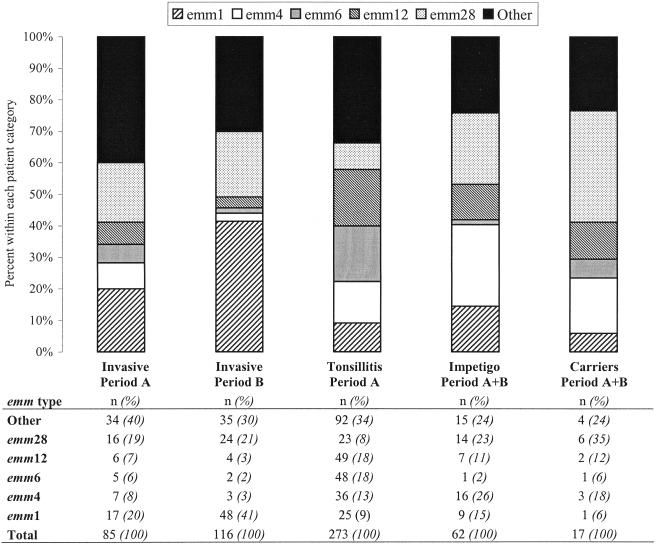
Various distributions of emm types among invasive and noninvasive isolates.
In total, 27 different emm types were found among the invasive isolates, of which emm type 1 (emm-1), emm-28, emm-12, emm-6, and emm-4 constituted 69% of the emm types. emm-1 and emm-28 alone constituted 32 and 20% of the emm types, respectively (Table 2). A significant increase in emm-1 isolates (P = 0.047) was identified when the distributions of the emm types between invasive GAS isolates collected during periods A and B were compared (Fig. 3). emm-12 and emm-4 were the most frequent emm types (both 16%) among the noninvasive GAS isolates, followed by emm-6 (14%), emm-28 (12%), and emm-1 (10%). Twenty different emm types were found among the remaining isolates (Table 2). The emm type distributions differed significantly (P < 0.001) among the three categories of patients with noninvasive GAS infections (Fig. 3). In addition, the emm type distribution among the invasive and noninvasive isolates differed significantly (P < 0.001). The significant difference remained (P = 0.001) when the emm types of the isolates from tonsillitis patients and invasive isolates from the same period (1 January 2001 to 30 June 2001) were compared (data not shown). There were no significant age differences between patients from whom the most prevalent emm types were collected and the patients with pharyngitis or invasive disease. Patients with impetigo and healthy carriers were omitted from these analyses due to the sparse number of patients registered.
TABLE 2.
Distribution of emm types among invasive and noninvasive isolates
| emm type | No. (%) of isolates
|
|
|---|---|---|
| Invasive | Noninvasive | |
| 1 | 65 (32.3) | 35 (9.9) |
| 2 | 1 (0.5) | 20 (5.7) |
| 3 | 8 (4.0) | 13 (3.7) |
| 4 | 10 (5.0) | 56 (15.9) |
| 5 | 0 (0.0) | 5 (1.4) |
| 6 | 7 (3.5) | 50 (14.2) |
| 9 | 2 (1.0) | 8 (2.3) |
| 11 | 4 (2.0) | 3 (0.9) |
| 12 | 11 (5.5) | 58 (16.5) |
| 22 | 2 (1.0) | 12 (3.4) |
| 28 | 40 (19.9) | 43 (12.2) |
| 29 | 0 (0.0) | 1 (0.3) |
| 43 | 3 (1.5) | 0 (0.0) |
| 49 | 0 (0.0) | 1 (0.3) |
| 58 | 1 (0.5) | 2 (0.6) |
| 70 | 0 (0.0) | 1 (0.3) |
| 73 | 0 (0.0) | 3 (0.9) |
| 75 | 3 (1.5) | 10 (2.8) |
| 76 | 1 (0.5) | 0 (0.0) |
| 77 | 5 (2.5) | 11 (3.1) |
| 78 | 4 (2.0) | 1 (0.3) |
| 87 | 2 (1.0) | 4 (1.1) |
| 88 | 1 (0.5) | 0 (0.0) |
| 89 | 20 (10.0) | 10 (2.8) |
| 94 | 4 (2.0) | 2 (0.6) |
| 102 | 1 (0.5) | 1 (0.3) |
| 105 | 0 (0.0) | 1 (0.3) |
| 109 | 1 (0.5) | 1 (0.3) |
| 110 | 1 (0.5) | 0 (0.0) |
| 27G | 1 (0.5) | 0 (0.0) |
| st1389 | 1 (0.5) | 0 (0.0) |
| st3757 | 1 (0.5) | 0 (0.0) |
| No emma | 1 (0.5) | 0 (0.0) |
| Total | 201 (100) | 352 (100) |
One isolate was not available for emm typing.
FIG. 3.
Distribution of emm types among invasive and noninvasive group A streptococcal isolates. The distribution of isolates is divided into two groups based on the sampling date: period A (1 January to 31 October 2001) and period B (1 November 2001 to 1 August 2002). See text for details of the statistical analyses.
Differential distribution of SAg genes in GAS isolates from invasive and noninvasive infections.
The chromosomally located genes encoding SpeB, SpeF, SpeG, SpeJ, and SMEZ were identified in all isolates investigated. The presence of the phage-associated SAg genes varied among the isolates, as shown in Table 3, with significant differences in speA, speC, and speH between isolates from invasive and noninvasive cases. In addition, there were also significant differences between the SAg profiles identified among the invasive isolates from periods A and B, with speA being more prevalent during period B, whereas the reverse was seen for speC and speH. No significant differences in SAg prevalence were observed between the noninvasive isolates (Table 3).
TABLE 3.
Distribution of SAg genes among invasive and noninvasive group A streptococcal isolatesa
| SAg gene | No (%) of isolatesb
|
||||||
|---|---|---|---|---|---|---|---|
| Invasive
|
Noninvasive
|
||||||
| Period A | Period B | Total | Tonsillitis, period A | Impetigo, periods A + B | Carriers, periods A + B | Total | |
| speA | 20 (24)c | 54 (47)c | 74 (37)d | 50 (18) | 12 (19) | 1 (6) | 63 (18)d |
| speC | 58 (68)c | 59 (51)c | 117 (59)d | 196 (72) | 43 (69) | 12 (71) | 251 (71)d |
| speH | 23 (27)c | 10 (9)c | 33 (17)d | 80 (29) | 11 (18) | 4 (24) | 94 (27)d |
| speI | 2 (2) | 3 (3) | 5 (2) | 15 (6) | 0 (0) | 1 (6) | 15 (5) |
| ssa | 36 (42)c | 26 (23)c | 62 (31) | 81 (30) | 23 (37) | 5 (29) | 108 (31) |
| speA + speC | 4 (5) | 14 (12) | 17 (9) | 19 (7) | 2 (3) | 0 (0) | 21 (6) |
| speA + ssa | 7 (8) | 8 (7) | 15 (8) | 10 (4) | 2 (3) | 0 (0) | 12 (3) |
| speC + ssa | 24 (28)c | 15 (13)c | 39 (19) | 60 (22) | 20 (32) | 4 (24) | 84 (24) |
The invasive isolates are divided into two groups based on sampling date (periods A and B): period A, 1 January to 31 October 2001; period B, 1 November 2001 to 1 August 2002.
The GAS isolate may carry multiple SAg genes.
P < 0.05 by comparison of invasive isolates between periods A and B, as determined by the chi-square test.
P < 0.05 by comparison of invasive and noninvasive isolates, as determined by the chi-square test.
Comparison of SAg profiles among invasive and noninvasive isolates with the same emm type revealed significant differences among emm-1, emm-4, emm-12, and emm-28 isolates (Table 4). Among the emm-1 and emm-28 isolates, most of the differences became nonsignificant when invasive and noninvasive isolates from the same collection period were compared (Table 5). A significant decrease in the prevalence of the speA (P = 0.029) and the ssa (P = 0.016) genes among invasive emm-1 isolates was seen in isolates from period B compared to that in isolates from period A. The decrease in the prevalence of speA among invasive and noninvasive emm-1 isolates was due to this shift in speA-harboring emm-1 isolates, and this significant difference disappeared when invasive and noninvasive isolates from period A only were compared. In contrast, the differences regarding ssa among emm-1 isolates remained significant (P = 0.002). The significant differences reported for the emm-28 isolates (Table 4) were also associated with a change in the prevalence of these particular SAgs among emm-28 isolates from periods A and B, and the differences disappeared when invasive and noninvasive isolates from period A were compared. There were not enough isolates of other emm types to identify similar trends.
TABLE 4.
Prevalence of SAg genes among the five most frequent emm types of invasive and noninvasive group A streptococcal isolates
| SAgs gene | Prevalence (%)a
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
emm-1
|
emm-4
|
emm-6
|
emm-12
|
emm-28
|
||||||
| Inv (n = 65) | Non (n = 35) | Inv (n = 10) | Non (n = 56) | Inv (n = 7) | Non (n = 50) | Inv (n = 11) | Non (n = 58) | Inv (n = 40) | Non (n = 43) | |
| speA | 74b | 97b | 0 | 2 | 14 | 4 | 9 | 12 | 23b | 7b |
| speC | 37b | 11b | 100 | 95 | 86 | 96 | 82 | 84 | 75 | 86 |
| speH | 3 | 6 | 80b | 29b | 0 | 12 | 64 | 81 | 18 | 9 |
| speI | 2 | 3 | 0 | 0 | 0 | 0 | 27 | 19 | 0 | 2 |
| ssa | 15b | 3b | 100 | 86 | 14 | 18 | 45b | 14b | 25b | 5b |
The GAS isolate may carry multiple SAg genes. Inv, invasive group A streptococcal isolates (total n = 200); Non, noninvasive group A streptococcal isolates (from patients with tonsillitis and impetigo and from asymptomatic carriers) (total n = 352).
P < 0.05 by comparison of invasive and noninvasive isolates, as determined by the chi-square test.
TABLE 5.
Prevalence of SAg genes among emm-1 and emm-28 noninvasive and invasive isolates during study periods A and B
| SAg gene | Prevalence (%)a
|
|||||
|---|---|---|---|---|---|---|
|
emm-1
|
emm-28
|
|||||
| Noninvasive, period A (n = 27) | Invasive
|
Noninvasive, period A (n = 31) | Invasive
|
|||
| Period A (n = 17) | Period B (n = 48) | Period A (n = 16) | Period B (n = 24) | |||
| speA | 96 | 94b | 67b | 10 | 0b | 38b |
| speC | 11 | 24 | 42 | 81 | 100b | 58b |
| speH | 7 | 6 | 2 | 13 | 38b | 4b |
| ssa | 0c | 35b,c | 8b | 6 | 19 | 29 |
The GAS isolate may carry multiple SAg genes. Period A, 1 January to 31 October 2001; period B, 1 November 2001 to 1 August 2002.
P < 0.05 by comparison of invasive isolates between period A and B, as determined by the chi-square test.
P < 0.05 by comparison of invasive and noninvasive isolates in period A, as determined by the chi-square test.
Host susceptibility to GAS infection as assessed by serum antibody responses.
Paired sera and GAS isolates collected from 33 patients with invasive infection and 91 patients from general practice were investigated (Table 1). The 12 patients from whom the sera were obtained within 6 days after the onset of symptoms presented with different clinical manifestations; 1 patient had NF and myositis, and the remaining 11 patients had less severe infections. However, one of these patients, an 85-year-old woman, died. The 91 patients from general practice included 89% who had tonsillitis, 7% who had impetigo, and 4% who were carriers.
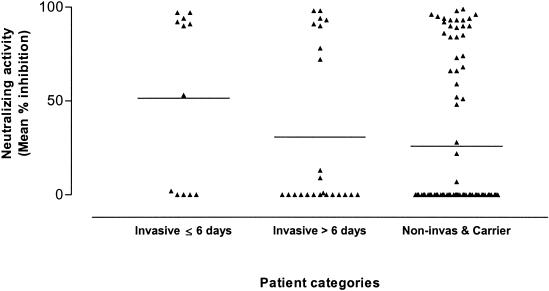
The serum neutralizing activity against superantigens produced by the patients' own isolates was tested (Fig. 4), and 58% of the serum specimens from invasive GAS cases (7 of 12) and 30% of the serum specimens noninvasive GAS cases (27 of 91) induced significant inhibition (≥50%) of mitogenicity in the culture supernatant (P = 0.058). We did not find any difference in the inhibitory activities of sera obtained within the first 6 days of illness and those of the sera obtained after day 6. There was no correlation between the age of the patients with invasive GAS isolates and the neutralizing activities of their sera; however, in patients with noninvasive isolates there was a negative correlation between age and the neutralizing activity (data not shown).
FIG. 4.
Supernatant inhibition of sera from patients with invasive and noninvasive group A streptococcal infections and asymptomatic carriers. The results are for patients with invasive GAS infections from whom a blood sample was taken within the first 6 days after the onset of symptoms (invasive ≤ 6 days [n = 12]), for patients with invasive GAS infections from whom a blood sample was taken more than 6 days after the onset of symptoms (invasive > 6 days [n = 24]), and for the group of patients with noninvasive GAS infections or asymptomatic carriers (Noninvas & Carrier [n = 91]). Serum from each patient was tested for neutralizing activity against the GAS isolate from that patient. Proliferation was assessed after 3 days of culture, and the mean counts per minute ± standard error of the mean for triplicate samples were calculated. The neutralizing activity of each patient's plasma is expressed as the percent inhibition of the mitogenic activity of the supernatant (see the equation in Materials and Methods). Horizontal lines indicate the mean antibody level within each patient category. See text for statistical analyses.
The sera were also assessed for the levels of ASOT and ASDB antibodies (data not shown). The level of ASOT antibodies was significantly lower in sera obtained from the GAS-negative controls than in the sera obtained within the first 6 days (P = 0.032) and in the sera from patients with noninvasive isolates (P < 0.001). There were no significant differences in the levels of ASOT antibodies (P = 0.063) between the sera from patients with invasive GAS isolates and the sera from patients with noninvasive isolates. In contrast, the level of ASDB antibodies was lower in the sera from patients with noninvasive isolates than in the sera from patients with invasive isolates (P = 0.049), and the level of ASDB antibodies was also significantly lower in the sera from controls than in the sera from patients with invasive (P = 0.006) or noninvasive (P = 0.029) isolates. There were no differences in either the ASOT or the ASDB antibody levels when the results for sera obtained within or after the first 6 days after the onset of symptoms were compared.
DISCUSSION
In this study, we present data for patients with invasive and noninvasive GAS infections and from asymptomatic carriers received from all over Denmark for a total of 19 months. In order to minimize possible differences of the GAS culture due to differences in the collection period, we divided it into two periods (periods A and B). The 201 invasive GAS isolates which we received during the study period were received as part of an enhanced nationwide program of surveillance for invasive streptococcal infections. The overall case fatality rate of 25% for invasive GAS infections as well as the occurrences and case fatality rates of 55% and 31% of STSS and NF, respectively, were comparable to those described previously (8). The study design did not allow evaluation of whether the cause of the fatal outcome was related to the GAS infection, since the information concerning death was obtained only from the Central Office of Civil Registration. However, it has previously been estimated that approximately 90% of deaths within 30 days after a positive culture result are directly related to the GAS infection (17).
Inclusion of appropriate noninvasive GAS isolates in studies of invasive GAS infections is important in order to be able to distinguish between the virulence properties and the prevalence of a particular GAS isolate in the general population (23, 24, 33). Furthermore, tonsillitis in childhood has been proposed as the major reservoir for circulating strains with the potential of causing invasive infection (13). The mean age of the patients with tonsillitis in our study was considerably higher than that of patients in conventional pharyngitis surveillance studies established in pediatric clinics (13, 39). However, this is probably of minor importance, since we did not find any significant correlation between age and the emm type distribution in the groups of patients with tonsillitis and invasive infection, respectively.
In agreement with previous studies, we found that the emm type distribution differed significantly between the different patient categories, which demonstrates a potential association between emm types and the kinds of infections (2, 5, 23). However, it should be recognized that although the differences may be explained by relative oversampling of some regions for invasive isolates or noninvasive isolates relative to the other, it seems unlikely that it could be the only explanation. In recently published studies, isolates from invasive and noninvasive infections were of similar emm types and prevalence (10, 13, 26, 39). Others have investigated isolates from invasive and noninvasive infections without identifying any clones that were statistically associated with invasive infections (2, 6), although M1 (emm-1) streptococci have been described as disproportionately associated with severe infections (23). Shulman et al. (39) recently described an emm-specific invasive index, based on analyses of more than 3,000 GAS isolates from patients with pharyngitis or invasive infections in the United States, and hypothesized that the observed variations in the invasiveness could probably be caused by differences in virulence factors, including exotoxins, although this hypothesis is still speculative.
We assessed the SAg genotype rather than relying on direct assays of SAg because it is likely that the toxin expression may be down regulated in vitro (14).
In the present study, the SAg profiles in the two most prevalent emm types (emm-1 and emm-28, respectively) were almost identical, regardless of the origin of the specimen. However, among the emm-28 strains, the prevalence of the ssa was significantly higher among invasive isolates than noninvasive isolates. We also noted fluctuations in the serotype distribution over time, as the prevalence of emm-1 increased almost twofold among invasive cases during period B compared to that during period A. Interestingly, not only did the emm types shift over time, but the SAg profiles both between and within certain emm types also shifted. The strong association found between certain emm types and the SAg genes detected among invasive isolates was in concordance with the previously reported SAg linkage to certain emm types (especially emm-1) (38, 41). However, the phage-associated SAg genes differed among isolates with the same emm type when invasive and noninvasive isolates were compared and also when invasive isolates obtained during period A and those obtained during period B were compared. Fewer differences were noted within the same period of time when the origins of the isolates were disregarded. This probably reflects a time issue and a reflection of the normal fluctuation in types.
The dissemination of a particular serotype, i.e., emm type, in the community likely depends on the prevalence of that strain circulating within a community, the invasiveness of that strain, and the degrees of both individual and population-level immunity to that strain (11, 24). The present proportional increase in emm-1 could therefore be explained by a general increased susceptibility in the population, as described previously (9, 16).
Host susceptibility has been recognized as a major factor in determining the severity of GAS infections. Several studies have shown that the host's humoral immunity is important in pathogenesis, as a lack of protective antibodies against superantigens (3, 31) and against cell wall-attached GAS antigens (1, 3, 19) has been reported to be associated with a more severe disease manifestation. We assessed humoral immunity among invasive cases, noninvasive cases, and negative controls through analyses of serum SAg-neutralizing activity and determination of ASOT and ASDB antibody levels. Surprisingly, the highest antibody responses were found in the sera from the invasive cases, whose ASDB antibody titers were significantly higher than those in noninvasive cases and controls. Likewise, the ASOT antibody titers were significantly higher in invasive case than in controls, although they were not significantly different compared to those in the noninvasive cases. There were no significant differences when the results for sera obtained within or after the first 6 days after the onset of symptoms were compared.
Another finding that is in contrast to those from previous reports (3) was the lack of a positive correlation between protective antibody titers and age among the invasive and noninvasive cases. These data imply that we are not looking at preexisting antibodies but, rather, at the response of each individual to his or her own invasive infection. The sera demonstrated either no or total inhibition of the supernatant mitogenicity, suggesting the presence of individual host factors that divide the patients into groups of responders and nonresponders without regard to the category of the infection or the origin of the isolate. Kotb et al. (25) reported a strong association with the HLA class II allotype of infected patients and disease progression and identified high and low immune responders to streptococcal SAgs. However, it remains to be elucidated whether the current findings for low and high responders with respect to neutralizing activity can be linked to the HLA class II allotype. Further studies on humoral immunity, preferably, studies that include acute-phase and consecutive sera and not only sera obtained during outbreaks but also sera obtained during periods of stable incidences are required to fully understand the role of protective antibodies in relation to susceptibility to invasive infection.
In conclusion, we were not able to identify any significant differences in the neutralizing capacities of sera from the two patient groups. However, we found that the levels of ASOT and ASDB antibodies were correlated to the patient category, indicating that the host probably plays a pivotal but not well-defined role in contributing to the severity and the outcome of the infection. Our study demonstrates that there were different emm type distributions among isolates causing either severe or nonsevere infections during the time frame of the study, which was restricted to Denmark. Furthermore, our data suggest that the emm type-SAg correlation, like immunity, seems to be both strain and M-type specific (25).
Acknowledgments
This study was supported by grants from StrepEuro (QLK2.CT.2002.01398), the Swedish Medical Research Council (12610, ANT), and the Swedish Foundation for Strategic Research (A3 02:098, ANT).
We thank Kimette Nielsen, Kirsten Burmeister, and Kirsten Linboe for skillful technical assistance. Annemarie Jørgensen and Jesper Madsen are also gratefully acknowledged for secretarial and statistical assistance, respectively; and likewise, Lotte Hougs and Jørgen S. Jensen are thanked for their superior assistance with the PCR. Moreover, we thank all GPs and patients for their participation in the study, all the Danish clinical microbiological departments for submitting the invasive isolates, and the physicians for filling in the questionnaires and returning them to the Statens Serum Institut.
REFERENCES
- 1.Akesson, P., M. Rasmussen, E. Mascini, U. Pawel-Rammingen, R. Janulczyk, M. Collin, A. Olsen, E. Mattsson, M. L. Olsson, L. Bjorck, and B. Christensson. 2004. Low antibody levels against cell wall-attached proteins of Streptococcus pyogenes predispose for severe invasive disease. J. Infect. Dis. 189:797-804. [DOI] [PubMed] [Google Scholar]
- 2.Anthony, B. F., E. L. Kaplan, L. W. Wannamaker, and S. S. Chapman. 1976. The dynamics of streptococcal infections in a defined population of children: serotypes associated with skin and respiratory infections. Am. J. Epidemiol. 104:652-666. [DOI] [PubMed] [Google Scholar]
- 3.Basma, H., A. Norrby-Teglund, Y. Guedez, A. McGeer, D. E. Low, O. El Ahmedy, B. Schwartz, and M. Kotb. 1999. Risk factors in the pathogenesis of invasive group A streptococcal infections: role of protective humoral immunity. Infect. Immun. 67:1871-1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beall, B., R. Facklam, and T. Thompson. 1996. Sequencing emm-specific PCR products for routine and accurate typing of group A streptococci. J. Clin. Microbiol. 34:953-958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bessen, D. E., J. Carapetis, B. Beall, R. Katz, M. Hibble, B. J. Currie, T. Collingridge, M. W. Izzo, D. A. Scaramuzzino, and K. S. Sriprakash. 2000. Contrasting molecular epidemiology of group A streptococci causing tropical and nontropical infections of the skin and throat. J. Infect. Dis. 182:1109-1116. [DOI] [PubMed] [Google Scholar]
- 6.Chatellier, S., N. Ihendyane, R. G. Kansal, F. Khambaty, H. Basma, A. Norrby-Teglund, D. E. Low, A. McGeer, and M. Kotb. 2000. Genetic relatedness and superantigen expression in group A streptococcus serotype M1 isolates from patients with severe and nonsevere invasive diseases. Infect. Immun. 68:3523-3534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies, H. D., A. McGeer, B. Schwartz, K. Green, D. Cann, A. E. Simor, D. E. Low, et al. 1996. Invasive group A streptococcal infections in Ontario, Canada. N. Engl. J. Med. 335:547-554. [DOI] [PubMed] [Google Scholar]
- 8.Efstratiou, A. 2000. Group A streptococci in the 1990s. J. Antimicrob. Chemother. 45:3-12. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson, B. K., J. Andersson, S. E. Holm, and M. Norgren. 1998. Epidemiological and clinical aspects of invasive group A streptococcal infections and the streptococcal toxic shock syndrome. Clin. Infect. Dis. 27:1428-1436. [DOI] [PubMed] [Google Scholar]
- 10.Eriksson, B. K., M. Norgren, K. McGregor, B. G. Spratt, and B. H. Normark. 2003. Group A streptococcal infections in Sweden: a comparative study of invasive and non-invasive infections and analysis of dominant T28 emm28 isolates. Clin. Infect. Dis. 37:1189-1193. [DOI] [PubMed] [Google Scholar]
- 11.Eriksson, B. K., A. Villasenor-Sierra, M. Norgren, and D. L. Stevens. 2001. Opsonization of T1M1 group A streptococcus: dynamics of antibody production and strain specificity. Clin Infect. Dis. 32:E24-E30. [DOI] [PubMed] [Google Scholar]
- 12.Facklam, R., B. Beall, A. Efstratiou, V. Fischetti, D. Johnson, E. Kaplan, P. Kriz, M. Lovgren, D. Martin, B. Schwartz, A. Totolian, D. Bessen, S. Hollingshead, F. Rubin, J. Scott, and G. Tyrrell. 1999. emm typing and validation of provisional M types for group A streptococci. Emerg. Infect. Dis. 5:247-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haukness, H. A., R. R. Tanz, R. B. Thomson, Jr., D. K. Pierry, E. L. Kaplan, B. Beall, D. Johnson, N. P. Hoe, J. M. Musser, and S. T. Shulman. 2002. The heterogeneity of endemic community pediatric group A streptococcal pharyngeal isolates and their relationship to invasive isolates. J. Infect. Dis. 185:915-920. [DOI] [PubMed] [Google Scholar]
- 14.Hauser, A. R., D. L. Stevens, E. L. Kaplan, and P. M. Schlievert. 1991. Molecular analysis of pyrogenic exotoxins from Streptococcus pyogenes isolates associated with toxic shock-like syndrome. J. Clin. Microbiol. 29:1562-1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helweg-Larsen, J., J. S. Jensen, T. Benfield, U. G. Svendsen, J. D. Lundgren, and B. Lundgren. 1998. Diagnostic use of PCR for detection of Pneumocystis carinii in oral wash samples. J. Clin. Microbiol. 36:2068-2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henrichsen, J., and T. Rønne. 1992. Reemergence of servere group A streptococcal infections in Denmark 1988-89. Zentbl. Bakteriol. Parasitenkd. Infektkrankh. Hyg. Abt. 1 Orig. 22:8-10. [Google Scholar]
- 17.Hindsholm, M., and H. C. Schonheyder. 2002. Clinical presentation and outcome of bacteraemia caused by beta-haemolytic streptococci serogroup G. APMIS 110:554-558. [DOI] [PubMed] [Google Scholar]
- 18.Hoffmann, S. 1986. Frequency of consultations because of sore throat. Ugeskr. Laeger. 148:2041-2044. (In Danish, with a summary in English.) [PubMed] [Google Scholar]
- 19.Holm, S. E., A. Norrby, A. M. Bergholm, and M. Norgren. 1992. Aspects of pathogenesis of serious group A streptococcal infections in Sweden 1988-89. J. Infect. Dis. 166:31-37. [DOI] [PubMed] [Google Scholar]
- 20.Jasir, A., A. Tanna, A. Efstratiou, and C. Schalen. 2001. Unusual occurrence of M type 77, antibiotic-resistant group A streptococci in southern Sweden. J. Clin. Microbiol. 39:586-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson, D. R., E. Kaplan, J. Sramek, P. Kriz, J. Motlova, R. Bicova, J. Havlicek, and H. Havlickova. 1996. Determination of anti-deoxyribonuclease B, p. 69-76. In D. R. Johnson (ed.), Laboratory diagnosis of group A streptococcal infections. World Health Organization, Geneva, Switzerland.
- 22.Johnson, D. R., E. Kaplan, J. Sramek, P. Kriz, J. Motlova, R. Bicova, J. Havlicek, and H. Havlickova. 1996. Determination of anti-streptolysin O, p. 57-68. In D. R. Johnson (ed.), Laboratory diagnosis of group A streptococcal infections. World Health Organization, Geneva, Switzerland.
- 23.Johnson, D. R., D. L. Stevens, and E. L. Kaplan. 1992. Epidemiologic analysis of group A streptococcal serotypes associated with severe systemic infections, rheumatic fever, or uncomplicated pharyngitis. J. Infect. Dis. 166:374-382. [DOI] [PubMed] [Google Scholar]
- 24.Johnson, D. R., J. T. Wotton, A. Shet, and E. L. Kaplan. 2002. A comparison of group A streptococci from invasive and uncomplicated infections: are virulent clones responsible for serious streptococcal infections? J. Infect. Dis. 185:1586-1595. [DOI] [PubMed] [Google Scholar]
- 25.Kotb, M., A. Norrby-Teglund, A. McGeer, H. El Sherbini, M. T. Dorak, A. Khurshid, K. Green, J. Peeples, J. Wade, G. Thomson, B. Schwartz, and D. E. Low. 2002. An immunogenetic and molecular basis for differences in outcomes of invasive group A streptococcal infections. Nat. Med. 8:1398-1404. [DOI] [PubMed] [Google Scholar]
- 26.Li, Z., V. Sakota, D. Jackson, A. R. Franklin, and B. Beall. 2003. Array of M protein gene subtypes in 1064 recent invasive group A streptococcus isolates recovered from the active bacterial core surveillance. J. Infect. Dis. 188:1587-1592. [DOI] [PubMed] [Google Scholar]
- 27.McCormick, J. K., A. A. Pragman, J. C. Stolpa, D. Y. Leung, and P. M. Schlievert. 2001. Functional characterization of streptococcal pyrogenic exotoxin J, a novel superantigen. Infect. Immun. 69:1381-1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michie, C., A. Scott, J. Cheesebrough, P. Beverly, and G. Pasvol. 1994. Streptococcal toxic shock-like syndrome: evidence of superantigen activity and its effects on T lymphocyte in vivo. Clin. Exp. Immunol. 98:140-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Musser, J. M., A. R. Hauser, M. H. Kim, P. M. Schlievert, K. Nelson, and R. K. Selander. 1991. Streptococcus pyogenes causing toxic-shock-like syndrome and other invasive diseases: clonal diversity and pyrogenic exotoxin expression. Proc. Natl. Acad. Sci. USA 88:2668-2672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norrby-Teglund, A., R. Kaul, D. E. Low, A. McGeer, D. W. Newton, J. Andersson, U. Andersson, and M. Kotb. 1996. Plasma from patients with severe invasive group A streptococcal infections treated with normal polyspecific IgG inhibits streptococcal superantigen-induced T cell proliferation and cytokine production. J. Immunol. 156:3057-3064. [PubMed] [Google Scholar]
- 31.Norrby-Teglund, A., K. Pauksens, S. E. Holm, and M. Norgren. 1994. Relation between low capacity of human sera to inhibit streptococcal mitogens and serious manifestation of disease. J. Infect. Dis. 170:585-591. [DOI] [PubMed] [Google Scholar]
- 32.Norrby-Teglund, A., P. Thulin, B. S. Gan, M. Kotb, A. McGeer, J. Andersson, and D. E. Low. 2001. Evidence for superantigen involvement in severe group A streptococcal tissue infections. J. Infect. Dis. 184:853-860. [DOI] [PubMed] [Google Scholar]
- 33.O'Brien, K. L., B. Beall, N. L. Barrett, P. R. Cieslak, A. Reingold, M. M. Farley, R. Danila, E. R. Zell, R. Facklam, B. Schwartz, and A. Schuchat. 2002. Epidemiology of invasive group A streptococcus disease in the United States, 1995-1999. Clin Infect. Dis. 35:268-276. [DOI] [PubMed] [Google Scholar]
- 34.Proft, T., V. L. Arcus, V. Handley, E. N. Baker, and J. D. Fraser. 2001. Immunological and biochemical characterization of streptococcal pyrogenic exotoxins I and J (SPE-I and SPE-J) from Streptococcus pyogenes. J. Immunol. 166:6711-6719. [DOI] [PubMed] [Google Scholar]
- 35.Proft, T., S. L. Moffatt, C. J. Berkahn, and J. D. Fraser. 1999. Identification and characterization of novel superantigens from Streptococcus pyogenes. J. Exp. Med. 189:89-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Proft, T., S. L. Moffatt, K. D. Weller, A. Paterson, D. Martin, and J. D. Fraser. 2000. The streptococcal superantigen SMEZ exhibits wide allelic variation, mosaic structure, and significant antigenic variation. J. Exp. Med. 191:1765-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reda, K. B., V. Kapur, D. Goela, J. G. Lamphear, J. M. Musser, and R. R. Rich. 1996. Phylogenetic distribution of streptococcal superantigen SSA allelic variants provides evidence for horizontal transfer of ssa within Streptococcus pyogenes. Infect. Immun. 64:1161-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmitz, F. J., A. Beyer, E. Charpentier, B. H. Normark, M. Schade, A. C. Fluit, D. Hafner, and R. Novak. 2003. Toxin-gene profile heterogeneity among endemic invasive European group A streptococcal isolates. J. Infect. Dis. 188:1578-1586. [DOI] [PubMed] [Google Scholar]
- 39.Shulman, S. T., R. R. Tanz, W. Kabat, K. Kabat, E. Cederlund, D. Patel, Z. Li, V. Sakota, J. B. Dale, and B. Beall. 2004. Group A streptococcal pharyngitis serotype surveillance in North America, 2000-2002. Clin. Infect. Dis. 39:325-332. [DOI] [PubMed] [Google Scholar]
- 40.Stevens, D. L., M. H. Tanner, J. Winship, R. Swarts, K. M. Ries, P. M. Schlievert, and E. Kaplan. 1989. Severe group A streptococcal infections associated with a toxic shock-like syndrome and scarlet fever toxin A. N. Engl. J. Med. 321:1-7. [DOI] [PubMed] [Google Scholar]
- 41.Talkington, D. F., B. Schwartz, C. M. Black, J. K. Todd, J. Elliott, R. F. Breiman, and R. R. Facklam. 1993. Association of phenotypic and genotypic characteristics of invasive Streptococcus pyogenes isolates with clinical components of streptococcal toxic shock syndrome. Infect. Immun. 61:3369-3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Unnikrishnan, M., D. M. Altmann, T. Proft, F. Wahid, J. Cohen, J. D. Fraser, and S. Sriskandan. 2002. The bacterial superantigen streptococcal mitogenic exotoxin Z is the major immunoactive agent of Streptococcus pyogenes. J. Immunol. 169:2561-2569. [DOI] [PubMed] [Google Scholar]
- 43.Working Group on Severe Streptococcal Infections. 1993. Defining the group A streptococcal toxic shock syndrome. Rationale and consensus definition. JAMA 269:390-391. [PubMed] [Google Scholar]