Abstract
Introduction:
Competency-based Medical Education (CBME) was introduced in the year 2019 in India. It has brought about major changes in medical education. The curriculum is learner centric, outcome based, focuses on the development of core competencies and professionalism. However, many institutions have faced challenges during the implementation of the CBME curriculum. This study was aimed at assessing the challenges faced by all the stakeholders (students, faculty, and administrators) of various medical institutions and gather their insights on proposed solutions.
Methodology:
This cross-sectional study was conducted over a period of 3 months, from October 1, 2023, to December 31, 2023. The study was conducted in 32 medical colleges across India. A total of 60 faculty of various disciplines, 32 administrators of the institutes, and 580 undergraduate medical students were included in the study. Perception of students and faculty was collected using a validated survey form. One-on-one interview was done for all the 32 administrators using a facilitator guide. A mixed-methods approach was used for quantitative and qualitative data collection and analysis.
Results:
Around 40 (66.6%) faculty opined that that deficiency of trained faculty was a significant challenge in implanting CBME curriculum. Twenty (33.3%) of the faculty felt that there is a lack of adequate infrastructure required for the implementation of CBME curriculum. Among the administrators surveyed, 12 (37.5%) felt that dwindling student attendance was a major challenge, whereas 10 (31.5%) felt that there was the lack of collaboration between universities, colleges, and regulatory authorities. Four hundred and twenty-five (73.2%) of students opined that simulation-based training and 435 (75%) students opined that electives were very good initiatives by CBME curriculum. The students found the inclusion of integrated teaching, Attitude, Ethics, and Communication Module, early clinical exposure, and Family Adoption Programme in the CBME curriculum helpful.
Conclusion:
CBME curriculum was largely accepted across all the medical colleges. The training of faculty and administrators was considered an important challenge which needs to be considered. Students opined that the newer curricular reforms enhanced their learning.
Keywords: Competency-based medical education curriculum, challenges in competency-based medical education, foundation course, integrated teaching, student centric
Introduction
Indian medical education has undergone a remarkable transformation, spanning five centuries. From the 16th century, Portuguese introduction to the dawn of vernacular training in 1822, Indian medical education has undergone a remarkable revolution.[1] This journey, starting with establishing the historic Calcutta Medical College in 1835 and reaching its latest milestone with the Competency-Based Medical Education (CBME) framework in 2019, is a testament to the constant evolution and adaptation of medical training in India.[1,2]
CBME drives medical graduates beyond knowledge acquisition. Aligned with global standards, it cultivates core competencies such as clinical skills, communication skills, empathy, and professionalism. The curriculum reforms include subject-specific sub-competencies, integrated learning and skill development, innovative teacher training, and multifaceted assessment methods.[3]
CBME faces a multitude of challenges, ranging from the content itself to the inertia surrounding its implementation and the practical implementation.[4] COVID-19 pandemic and subsequent lockdowns posed a major challenge in implementing CBME curriculum.[5] One of the important challenges is assessment, as it demands multiple assessors, varied assessment tools, and robust rating systems, each requiring meticulous training for evaluators.[6,7] Regulatory and accreditation hurdles further complicate matters, while logistical issues, insufficient medical education, and research funding add to the burden.[8,9]
CBME is a much-discussed topic in medical education, with passionate proponents and equally vocal critics. A multicentric study showed that the faculty overwhelmingly preferred an evolutionary approach to curriculum reform, with incremental changes to the existing curriculum favored by over 75% of the faculty.[10] This underscores the importance of prioritizing faculty input, equipping them with adequate training in the new curriculum, and providing ongoing support for successful implementation.[10] The past 4 years have provided valuable insights into both the successes and challenges of CBME implementation.
This study aims to understand the perceptions of various stakeholders such as students, faculty members, and administrators regarding implementing CBME across 32 medical colleges in India focusing on challenges and their possible solutions. This collective effort intends to unlock valuable knowledge and actionable blueprints, empowering stakeholders to build a roadmap for success to optimize the implementation of CBME.
Methodology
This multi-centric cross-sectional study was conducted across 32 medical colleges in India over a period of 3 months, from October 1st, 2023 to December 31st, 2023. Undergraduate medical students, faculty members, and administrators were included in the study.
The sample and sampling method
Faculty, administrators, and students were included from 32 medical colleges from all over the country. A total of 60 faculties, 32 administrators, and 580 medical undergraduate students were involved in the study. The faculties were involved in teaching undergraduate medical students for at least 5 years and the administrators were involved in the implementation of CBME curriculum in their respective institutions. Convenient sampling was done. A mixed-methods approach was used for quantitative and qualitative data collection and analysis as described:
Data collection
The study was conducted after obtained approval from the institutional ethical committee vide letter number AMCH/IEC-BHR/2023/08/03 dated August 10, 2023. Informed consent was obtained, and confidentiality was assured. Two self-administered questionnaires were prepared by the authors to assess the feedback of CBME curriculum from faculty members and students. The questionnaire was validated by two external members who were senior members of medical education unit. They conducted the face-validity of the questionnaire. The pilot study was done on 25 students and 10 faculty members. The questionnaires for faculty members included sociodemographic profile, department, designation of faculty, and number of years of teaching experience. The questions included were:
The CBME curriculum has been implemented in your institute: Yes/No
List the most important challenges faced or perceived by faculty during implementing CBME curriculum?
Describe any modifications/suggestions for the better implementation of CBME curriculum.
The survey form for students included demographic details, phase of MBBS, and following questions.
Enlist the best initiatives in the CBME which helped you learn better?
What aspects of the CBME curriculum need to be revised for a better learning experience?
-
Describe your experiences, challenges faced, and modifications required in the following curricular reforms in CBME curriculum
Foundation course
Early clinical exposure (ECE)
Attitude, Ethics and Communication (AETCOM) module
Self-directed learning
Family Adoption Program (FAP).
The questionnaires were disseminated through Google forms to the faculty members and students.
A total of 32 in-depth interviews were conducted for the administrators of various interviews by the investigators. The administrators were Principals/Vice-principals/Head of the departments/Senior members of Medical Education Units/Curriculum Committee (CC) members who were involved in implementing CBME curriculum in their institutes. The interviews were conducted either in the online or physical mode. The interviews were recorded and transcribed by an expert who was not involved in the study. The interview guide was prepared by the investigators and was validated by two external experts. The interview started with introduction of the interviewee and interviewer, purpose of the study, and following questions.
Describe the challenges faced by administrators in implementing CBME curriculum in your institute
What are the suggestions and modifications required for better implementation of CBME curriculum.
Data analysis
Qualitative
Inductive thematic analysis was performed for the qualitative data obtained from the responses of faculty and students to the open-ended questions in the feedback questionnaire. The steps of familiarization, coding, and generating themes were followed in the sequence. Inductive coding of the data was done. Coding was done by two investigators and consensus was achieved in more than 90%. Initial codes were generated, themes were identified, defined and the conclusion was written.[11]
Quantitative
The collected data were entered into Microsoft Excel, and analysis was done using Microsoft Excel 2019 and SPSS. Descriptive statistics of the student feedback were analyzed in terms of mean and standard deviation. The analysis was carried out using SPSS version 23 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY, USA: IBM Corp.).
Results
The questionnaire was sent to 80 faculty members, total of 60 faculty responded. The questionnaire was sent to 750 students, out of them 580 responded. The response rate was 75% for faculty members and 77% for students. Out of 32 medical colleges, 17 were private medical colleges and 15 were government medical college.
Totally, the data from 60 faculty members were included in the study. All these faculties were involved in imparting CBME curriculum in their institutions. The mean teaching experience of the faculty was 12.5 (SD ± 4.2) years. All the faculties were associate professors and professors. Thirty (50.0%) were from phase 1 MBBS, 19 (31.6%) were involved in teaching phase 2 MBBS, and 11 (18.3%) were from phase 3 MBBS part II. Figure 1 depicts the challenges faced by faculty members during the implementation of CBME curriculum.
Figure 1.
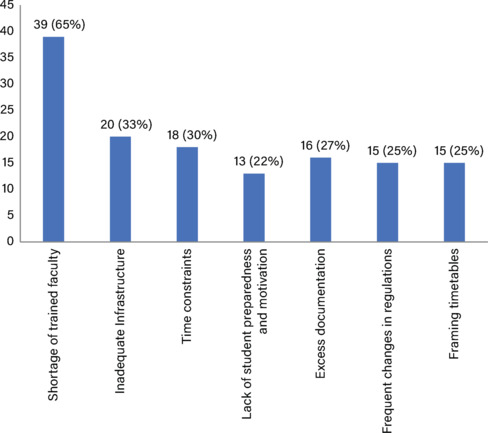
Bar Diagram showing the frequency of the challenges faced by faculty during implementation of competency-based medical education curriculum (n = 60)
The verbatims of faculty which were recorded regarding challenges in the implementation of CBME curriculum were as follows:
“Many faculty members are not trained in BCME and CISP. There is a lot of work related to documentation and many faculty are required to conduct small group discussions.”
“Many sessions are conducted by senior residents and assistant professors. Most of them are not trained in Medical Education technologies.”
“Senior stakeholders are not aware of CBME reforms. They feel the traditional curriculum was sufficient”.
“Many faculty are not willing to adopt the newer changes as they feel it will increase their workload. Faculty members do not coordinate with each other. Often the topics which need to be aligned are not happening.”
“Adequate resources and infrastructure are required for implementing CBME reforms like SDL, Simulation based teaching, small group discussions. Many colleges do not have adequate infrastructure.”
“Students are not aware of the curricular reforms brought about in CBME. They do not understand the importance of the changes in curriculum.”
The abbreviations referred to in verbatims such as BCME stands for Basic Course in Medical Education; CISP - Curriculum Implementation Support Program; PG - Postgraduate; SDL - Self-directed learning.
Thematic analysis was conducted on the responses. The inductive codes which were generated, themes are depicted in Tables 1 and 2.
Table 1.
Thematic analysis of the faculty perspective on challenges faced during implementing competency-based medical education curriculum (n=60)
| Themes | Codes |
|---|---|
| Deficiency of trained faculty in basic course in medical education | Lack of trained faculty |
| Excessive workload for faculty | |
| Untrained senior residents and assistant professors | |
| Lack of teamwork among faculty | Lack of interdepartmental collaboration |
| Not able to align the topics | |
| Resistant to adopt new changes | |
| Lack of adequate infrastructure | Lack of space for conducting small group discussions |
| Skills lab not upgraded | |
| Need adequate support from IT teams | |
| Senior administrators need training in CBME | Many senior administrators are not aware of the CBME reforms |
| Senior administrators should cooperate for full implementation of CBME | |
| Lack of sensitization among students regarding CBME | Some students not interested in the newer curricular changes |
| Lack of motivation among students | |
| Poor attendance | |
| Students attending PG entrance trainings | |
| Faculty training in assessments | Faculty lack training in OSCE/OSPE/newer assessments |
| Difficult to give adequate feedback |
CBME: Competency-based medical education; OSCE/OSPE: Objective structured clinical examination/Objective structured practical examination
Table 2.
Thematic analysis of the suggestions by faculty for better faced implementing competency-based medical education curriculum (n=60)
| Themes | Codes |
|---|---|
| Improve faculty training | Regular training of the faculty in BCME and CISP |
| Conduct of workshops regarding teaching-learning and assessment methods | |
| Train senior residents | |
| Faculty recognition and appreciation | Faculty incentivization |
| Faculty awards | |
| Improve student involvement and sensitization | Better student engagement |
| Involvement of parents in need | |
| Adequate student sensitization regarding student-centric curricular reforms | |
| Adopt 360° feedback for students | |
| Robust mentorship programme | |
| Improvement of infrastructures | Upgradation of infrastructure |
| Better lecture halls, skills labs, IT support, adequate internet connections |
BCME: Basic course in medical education; CISP: Curriculum Implementation Support Program
A total of 580 MBBS students were included in the survey. The distribution of students as per the phase of M.B.B.S. was 112 (19.3%) from Phase 1; 129 (22.2%) from Phase 2; 80 (13.8%) from Phase 3 Part I, and 259 (44.7%) from Phase 3 Part II. Among the students, males were 320 (55.1%), whereas females were 260 (44.9%). Figure 2 depicts the frequency of the students who listed the most useful initiatives in the CBME curriculum. Students felt that various reforms such as AETCOM, simulation-based learning, skill training, and training using scenarios were impactful. However, students opined that there is excessive logbook documentation which needs to be reduced. Furthermore, they felt that SDL needs to be conducted in a systemic manner and the curriculum can be more aligned with national level exit examinations. The themes identified based on the student response to the question “What aspects of the CBME curriculum need to be revised for a better learning experience?” are summarized in Figure 3 and Table 3.
Figure 2.
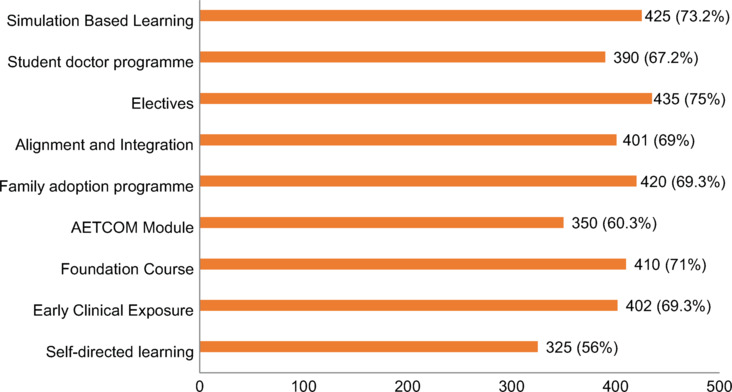
Bar graph showing the frequency of the students who listed the most useful initiatives in the competency-based medical education curriculum (n = 580)
Figure 3.
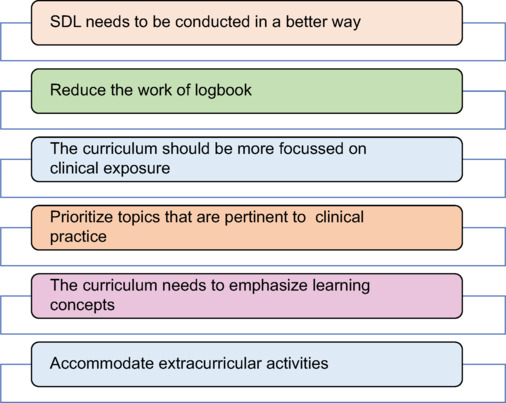
Themes generated out of the student responses to the question- “What aspects of the competency-based medical education curriculum need to be revised for a better learning experience?” (n = 580)
Table 3.
Thematic analysis of the student reforms to curricular changes like foundation course, attitude ethics, communication module, early clinical exposure, self-directed learning and family adoption programme (n=580)
| Themes on the challenges faced by students | Themes on the suggestions for improvement | Verbatims |
|---|---|---|
|
FC | ||
| FC was too lengthy | The duration of FC may be shortene | “FC sensitized us regarding the subjects, improved our interaction, we made friends, also had sports and extracurricular activities” |
| Missed some classes of FC due to late admissions | Language and computer skills can be optional | |
|
Aetcom module | ||
| AETCOM is more theoretical | AETCOM sessions can be in real-life scenarios like wards/OPD | “Interesting to learn concepts like empathy, ethics, communication which are not taught routinely” |
| Role-plays become monotonous after a few sessions | Sharing real-life experiences by faculty helpful | |
|
Early clinical exposure | ||
| Time constraints in the wards | Smaller batches for visits to wards | “Made students feel like doctors and it helped in application of knowledge and relevance of basic sciences” |
| Shortage of clinical faculty | Virtual tours, and live-streamed procedures in classroom settings | |
|
Self directed learning | ||
| The process of SDL is not clear | Better faculty training and student sensitization | “Students learn more and the learning is in-depth. SDL promoted student research” |
| SDL may not be suitable for all students | Uniform and standard protocols about SDL | |
|
Family adoption programme | ||
| Going to the village multiple times is difficult | Faculty can accompany students | “We understood the life of people in the village. Improved community engagement. Learnt health practices in the families and awareness of myths and perception about the health conditions” |
| People are hesitant to share their personal information | Reduce the number of visits | |
| Migratory population | Telecommunication may be helpful | |
FC: Foundation course; SDL: Self-directed learning; ECE: Early clinical exposure; AETCOM: Attitude ethics, communication module; OPD: Out-patient department
One-to-one interviews were conducted for 32 senior stakeholders who actively participated in implementing CBME in their institutions. Out of total, 10 (31.2%) were Deans or Associate Deans, 20 (62.5%) were senior MEU members, and 2 (6.3%) were senior members of the CC. Many senior stakeholders felt that frequent changes in curriculum lead to confusion. Furthermore, they were concerned about dwindling student attendance and faculty motivation. The other challenges faced by them are represented in Figures 4 and 5.
Figure 4.
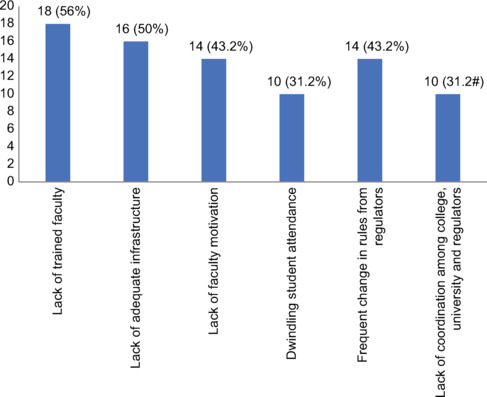
Bar diagram showing the frequency of codes captured out the responses from senior administrators regarding challenges faced in the implementation of competency-based medical education curriculum (n = 32)
Figure 5.
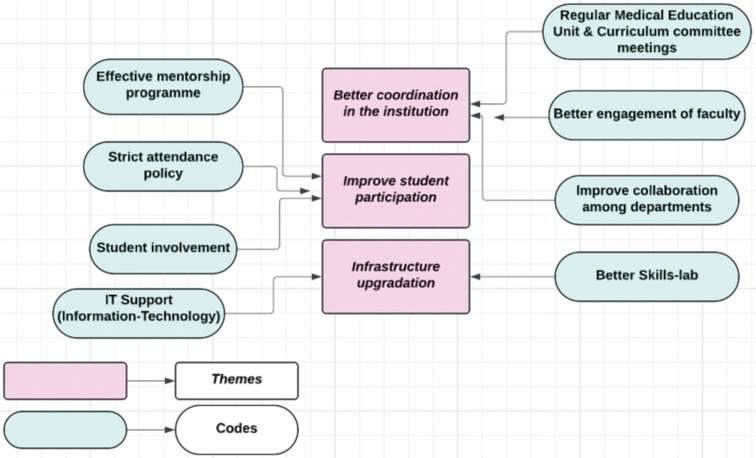
Thematic map representing the themes and codes generated out the responses from senior administrators regarding suggestions for the better implementation of competency-based medical education curriculum (n = 32)
Discussion
Competency-based medical education introduced in India in 2019 has brought about a revolutionary change in medical education. CBME focused on acquiring the defined competencies for a comprehensive acquisition of knowledge and skills. However, the journey from its introduction till now had many challenges. Also, the future ahead needs to be planned for making medical education more applicable and efficient.
The current study has elaborately described the challenges faced by faculty, students, and senior administrators during implementing CBME curriculum. In addition, several suggestions have been provided for the better implementation of CBME.
Around 60% of the faculty opined that there is a shortage of trained faculty for smooth implementation of CBME. Furthermore, they mentioned that junior faculty who are also involved in teaching-learning and assessments are still not trained. Hence, their training will be helpful in the better implementation of CBME. These findings were concordant with the study conducted by Ramanathan et al. who also mentioned that lack of trained faculty was the major challenge. This study also noted that 75% them believed that the faculty members are not adequate for preparatory work for CBME implementation.[10] Faculty training has to be well planned and should address the needs of the faculty. The faculty training should focus on understanding the intricacies of CBME curriculum, teaching-learning methodologies, assessments and feedback.[12,13,14]
The findings of our study indicate that many new faculty members are not adequately trained in conduct of Objective structured clinical examination/Objective structured practical examination (OSCE/OSPE). Furthermore, faculty find difficulty in providing adequate feedback for the students. As per the study done by Dongre and Chacko, the assessment should have good educational impact.[15] Effective environment should be created to make assessments valid, reliable, and uniform. There needs to be alignment between learning objectives and assessment tools.[15]
The findings of the current study indicate that foundation course was well appreciated by students. However, a few of them mentioned that the duration can be trimmed and many sessions such as language and computer operations can be individualized. A study by Velusami et al. showed that foundation course was found useful and interesting by students. However, students opined that the sessions should be more interactive.[16]
The current study shows that students such as AETCOM as they felt that it improved their soft skills and awareness about the importance of good communication. The students opined that they would like the faculty to share their own experiences regarding good communication skills and ethics. This will help them to understand the attributes of AETCOM module in a better manner. The findings were like the study by Jain et al. who opined that AETCOM module will improve the soft skills of students and will also prevent professional malpractices and litigations in medical practice.[17,18]
ECE was perceived by students are a very useful initiative which helped them to integrate the concepts of basic sciences and apply them. They felt that there should be more involvement of clinical faculty and there has to better preparedness during ECE sessions. As per the literature, the major challenge in medical education is improvization of clinical education.[17] The students must understand the clinical correlation of basic sciences. ECE will help the students to apply the knowledge learnt in basic sciences and understand the concepts in depth.[19]
The findings of our study show that FAP was well accepted by students. They felt that more faculty must be involved during the trips as they found that few families were not cooperative. Furthermore, some of them felt that the number of families per student can be reduced. A study by Yalamanchili et al. showed that FAP was found useful for students to understand and comprehend the community aspects of diseases. However, there can be multiple challenges for colleges such as transports and identifying the families.[20]
Implementing CBME is no quick sprint; it is a long-distance race demanding unwavering commitment and strategic adaptation.[21] Institutions should foster a culture of continuous improvement by encouraging stakeholder feedback, conducting regular reviews, and adjusting based on data and evidence.
To our best knowledge, this is the first study conducted in India which thoroughly assessed the challenges perceived by students, faculty, and administrators regarding implementing CBME. They have provided their suggestions for the improvement of the same.
The limitation of the study is its small sample size. Furthermore, the demographic and social factors of the study participants were not considered in the study. The number of questions in the survey questionnaire was less to ensure that the participants could describe their experiences of implementing CBME curriculum in detail. This study is descriptive with more focus on the qualitative data, which was aimed to capture some sensitive perceptions and suggestions which may not have been captured through quantitative questions.
Conclusion
CBME curriculum has a long way to go through. It has been implemented and adopted across India. There are many challenges encountered mostly about shortage of trained faculty, sensitization, and implementing reforms amidst tight curricular schedules. Improved faculty training with focus on teaching-learning and assessments methods, student involvement with robust mentorship program, and strong support from senior administrators can help in the better implementation of CBME curriculum.
Ethical statement
The study was approved by the “Institutional Ethics Committee for Biomedical and Health Research (IEC-BHR), Adesh Medical College and Hospital, Vill. Mohri, Shahabad (M), Haryana. Reference No.- AMCH/IEC-BHR/2023/08/03. Dated 10/08/2023.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge the contributions and participation of all the FAIMER faculty and fellows (Fellowship of Advanced International Medical Education and Research) from Christian Medical College, Ludhiana.
Funding Statement
Nil.
References
- 1.Anshu, Supe A. Evolution of medical education in India: The impact of colonialism. J Postgrad Med. 2016;62:255–9. doi: 10.4103/0022-3859.191011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manchanda C, Patil A. Competency based medical education in India, a new beginning: A perspective. IOSR J Dent Med Sci. 2019;18:57–60. [Google Scholar]
- 3.Supe A, Sheshadri GK, Singh P, Sajith KR, Chalam PV, Maulik KS, et al. Medical Council of India. Vol. 1. New Delhi: Medical Council of India; 2018. Competency-Based Undergraduate Curriculum for the Indian Medical Graduate. [Google Scholar]
- 4.Agarwal S, Dhingra C, Nayyar R. Perception on Competency-Based Medical Curriculum at Indian Medical Schools: Post-Implementation Position. 3rd World Conference on Research on Social Sciences, Vienna. 2021:23–4. [Google Scholar]
- 5.Jain P, Ramanathan R, Jayapal M, Gopalakrishna SM, Shanmugam J, Moorthy R. Impact of COVID-19 pandemic on medical education. Natl J Physiol Pharm Pharmacol. 2023;13:462–6. [Google Scholar]
- 6.Lockyer J, Carraccio C, Chan MK, Hart D, Smee S, Touchie C, et al. Core principles of assessment in competency-based medical education. Med Teach. 2017;39:609–16. doi: 10.1080/0142159X.2017.1315082. [DOI] [PubMed] [Google Scholar]
- 7.Badyal DK, Sharma M. Internal assessment in new MBBS curriculum: Methods and logistics. Int J Appl Basic Med Res. 2020;10:68–75. doi: 10.4103/ijabmr.IJABMR_70_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Melle E, Frank JR, Holmboe ES, Dagnone D, Stockley D, Sherbino J, et al. A core components framework for evaluating implementation of competency-based medical education programs. Acad Med. 2019;94:1002–9. doi: 10.1097/ACM.0000000000002743. [DOI] [PubMed] [Google Scholar]
- 9.Ryan MS, Holmboe ES, Chandra S. Competency-based medical education: Considering its past, present, and a post-COVID-19 era. Acad Med. 2022;97:S90–7. doi: 10.1097/ACM.0000000000004535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramanathan R, Shanmugam J, Gopalakrishnan SM, Palanisamy KT, Narayanan S. Challenges in the implementation of competency-based medical curriculum: Perspectives of prospective academicians. Cureus. 2022;14:e32838. doi: 10.7759/cureus.32838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Javadi M, Zarea M. Understanding thematic analysis and its pitfalls. J Client Care. 2016;1:33–9. [Google Scholar]
- 12.Shrivastava SR, Shrivastava PS. Qualitative study to identify the perception and challenges faced by the faculty of community medicine in the implementation of competency-based medical education for postgraduate students. Fam Med Community Health. 2019;7:e000043. doi: 10.1136/fmch-2018-000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramanathan R, Shanmugam J, Gopalakrishnan SM, Palanisamy KT, Narayanan S. Challenges in the implementation of competency-based medical curriculum: Perspectives of prospective academicians. Cureus. 2022;14:e32838. doi: 10.7759/cureus.32838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Payal B, Avinash S, Soumendra S, Rashmi V. Faculty development for competency based medical education. Natl J Integr Res Med. 2017;8:89–95. [Google Scholar]
- 15.Dongre AR, Chacko TV. A critical review of new competency-based curriculum for community medicine using various curricular review frameworks. Indian J Public Health. 2019;63:362–6. doi: 10.4103/ijph.IJPH_141_19. [DOI] [PubMed] [Google Scholar]
- 16.Velusami D, Dongre RA, Kagne NR. Evaluation of one-month foundation course for the first year undergraduate students at a Medical College in Puducherry, India. J Adv Med Educ Prof. 2020;8:165–71. doi: 10.30476/jamp.2020.86857.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jain T, Mohan Y, Maiya GR, Nesan GS, Boominathan C, Eashwar AV. Evaluating the effectiveness of ‘AETCOM module’ on the medical interns posted in peripheral health centres of a tertiary care medical college in Kanchipuram, Tamil Nadu. J Family Med Prim Care. 2022;11:2828–33. doi: 10.4103/jfmpc.jfmpc_1647_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shrivastava SR, Shrivastava PS. Ensuring smooth implementation of attitude, ethics, and communication module in medical colleges: SWOT analysis. Ibnosina J Med Biomed Sci. 2021;13:222–6. [Google Scholar]
- 19.Tayade MC, Latti RG. Effectiveness of early clinical exposure in medical education: Settings and scientific theories – Review. J Educ Health Promot. 2021;10:117. doi: 10.4103/jehp.jehp_988_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yalamanchili VK, Uthakalla VK, Naidana SP, Kalapala A, Venkata PK, Yendapu R. Family adoption programme for medical undergraduates in India – The way ahead: A qualitative exploration of stakeholders’ perceptions. Indian J Community Med. 2023;48:142–6. doi: 10.4103/ijcm.ijcm_831_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall AK, Rich J, Dagnone JD, Weersink K, Caudle J, Sherbino J, et al. It’s a marathon, not a sprint: Rapid evaluation of competency-based medical education program implementation. Acad Med. 2020;95:786–93. doi: 10.1097/ACM.0000000000003040. [DOI] [PubMed] [Google Scholar]


